Abstract
Purpose
Sperm that bypass natural apoptosis and the ubiquitin-proteasome system may find their way into semen. In order to avoid the insemination of such sperm during an intracytoplasmic sperm injection (ICSI) treatment, novel sperm selection procedures such as the Zeta procedure have been implemented. Therefore, the aim of this study was to evaluate extent of ubiquitination and external phosphatidylserine (EPS) in sperm populations selected by combines density gradient centrifugation (DGC) and Zeta electric potential in comparison to DGC and neat semen samples.
Methods
Semen samples were collected from 51 infertile men and divided into control, DGC and DGC-Zeta groups. Semen analysis was carried out according to World Health Organization criteria. The percentages of protamine deficiency, DNA fragmentation, EPS and ubiquitinated sperm were assessed by chromomycin A3 (CMA3), TUNEL, Annexin V, and immunostaining, respectively.
Results
Sperm selected by the DGC-Zeta procedure presented a lower percentage of sperm with protamine deficiency, abnormal morphology and DNA fragmentation while the percentage of annexin V and ubiquitin-positive sperm increased.
Conclusion
The results of this study reveal that, DGC-Zeta improves the quality of the selected spermatozoa for ICSI and increases ubiquitination and EPS rates. We propose these alterations are part of the normal physiological process of capacitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Upon fertilization, sperm triggers oocyte activation and contributes to approximately half the genetic content of future progeny [1]. Therefore, delivery of normal chromatin content by sperm has important consequences on fertilization, development and future health of the conceived individual. Three main mechanisms have been suggested for the development of abnormal sperm chromatin are: 1) improper DNA packaging due to defects in replacement of histones with protamine [2] (2) production of reactive oxygen species due to endogenous and exogenous factors [3] (3) abortive apoptosis [4]. Externalization of phosphatidylserine to the outer membrane of sperm and DNA damage are considered as early and lately signs of apoptosis. In fertile individuals, abnormal or defective sperm are removed by apoptosis or the ubiquitin-proteasome system during sperm maturation in the testis and epididymis, respectively. Ubiquitin-proteasome system recognized dysfunctional proteins or un-properly fold proteins. Therefore, defective sperm identified in ejaculate may have bypassed these self-protective systems. This phenomenon is believed to occur at much higher rates in infertile individuals [5–7]. In spontaneous conception, natural barriers to fertilization ensure that defective sperm are excluded from the insemination population and they have lower chances of participating in the fertilization process [8]. However, during intra cytoplasmic sperm insemination or ICSI procedure, although sperm is selected based on viability and morphology, but such defective sperm have significantly higher chances of participating in the fertilization process and thereby account for fertilization failure, failed pregnancy and abortion. Indeed, Avendaño et al. shows that in infertile individuals up to 50% sperm with normal morphology may present DNA fragmentation [9]. Therefore, to overcome these in vitro shortcomings, novel sperm selection has been established based on ability to bind hyaluronic acid [10, 11], surface charge [12, 13], surface apoptotic markers [14] and nuclear normalcy [15].
Considering presence of an electric charge of −16 to −20 mV on sperm surface, called Zeta potential, has made selection of sperm based on this property, a convenient methods. The Zeta potential is due presence of negative charges in sialoglyoproteins on the sperm membrane. Previous studies suggest that sperm selected based on this properties, present better morphology and higher percentage of sperm with intact chromatin (11–13).
Clinical trials are necessary to evaluate the possible efficiencies of these techniques with respect to one another. Such trials are time consuming and may not always be possible. Another alternative to evaluate the possible efficiency of these techniques is to assess the functional characteristics of the selected sperm population for comparison of this method with each other or routine procedure for sperm processing, such as density gradient centrifugation (DGC).
Therefore, we aimed to evaluate whether this combined procedure (DGC-Zeta) could influence the percentage of apoptotic or aberrant sperm in the selected population assessed for EPS and ubiquitination, respectively.
Materials and methods
Semen sample collection and preparation
This study received approval from the Institutional Review Board of Isfahan Fertility and Infertility Center and Royan Institute. Informed consent forms were signed by all patients. All chemicals were obtained from Merck (Darmstadt, Germany), unless otherwise stated. Experimental design is shown in the Fig. 1. The percentage of abnormal morphology, DNA fragmentation and protamine deficiency were assessed by Papanicoulau staining, TUNEL and CMA3 accordingly Nasr-Esfahani et al. [16–18]. Ubiquitination and external phosphatidyl serine (EPS) were assessed by flow cytometry as described by Sutovsky et al. 2001 [19] and [20], respectively. In this study, EPS was not assessed in the control fraction due to the presence of M540 or apoptotic bodies, which are known to be EPS positive with similar size to sperm [21].
Density Gradient Centrifugation (DGC) and Zeta procedures
The DGC and Zeta procedures were carried out according to Chan et al. (2006) and Kheirollahi-Kouhestani et al. (2009) [12, 22]. Following DGC, the processed samples were divided into two fractions, one for evaluation of the aforementioned tests and the remaining portion was used for the Zeta procedure. For the DGC-Zeta procedure, 5 × 106 sperm were diluted in Ham’s F10 buffer. To induce a positive charge, the tube was placed inside a latex glove up to the cap and by grasping the cap, the tube was rotated two or three times and rapidly removed. Each tube was kept at room temperature for 1 min to allow adherence of the charged sperm to the wall of the tube. Then, the medium was discarded to remove non-adhering sperm. The surface of the tube was washed by 1 ml of Ham’s F10 + albumin 10% to neutralize the charge on the wall of the tube and detach adhering sperm. Then, the aforementioned tests were carried out on this fraction. To minimize variation, a single trained individual performed all procedures.
Evaluation of capacitation and the acrosome reaction CTC procedure
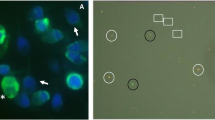
Sperm capacitation was assessed by CTC fluorescence according to DasGupta et al. (1994) [23]. This method is based on alterations in staining patterns of the sperm head during the process of capacitation and acrosome reaction. The ‘F’ pattern characteristic of non-capacitated or acrosome-intact spermatozoa; the ‘B’ pattern characteristic of capacitated but acrosome-intact spermatozoa and the ‘AR’ pattern characteristic of acrosome-reacted spermatozoa are shown in Fig. 4a.
Statistical analysis
Results are expressed as means ± SEM. For statistical analysis, the two-paired student’s t-test was used. Levene’s test for equality of variances and Shapiro-Wilk were carried out to assess normal distribution. P values of <0.05 were considered significant. For three or more groups, data were analyzed by one-way ANOVA. Differences between all groups were compared by the Tukey multiple comparison post hoc test. Flow cytometry data was analyzed with WinMDI 2.9 software.
Results
A descriptive of semen parameters, including sperm concentration, percentage of abnormal morphology and motility are shown in Table 1. Out of 51 infertile men, 10 asthenozospermia and 12 teratozospermia and the remaining were normozospermic. Table 2 shows the comparison of abnormal morphology, protamine deficiency and DNA fragmentation in the three groups. The mean percentage of abnormal sperm morphology in the control, DGC and DGC-Zeta groups were 94.14 ± 1.10, 90.38 ± 1.16 and 79.34 ± 2.76, respectively. The percentage of abnormal morphology reduced significantly in the DGC and DGC-Zeta groups when compared with the control group (p < 0.05). In addition, the percentage of abnormal morphology was also compared between the DGC and DGC-Zeta groups. There was a significant difference between the two groups (p < 0.05).
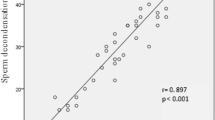
The percentage of ubiquitin sperm was assessed by flow cytometry in the control, DGC and DGC-Zeta groups. The results are presented in Fig. 2a and b. The mean percentage of ubiquinated sperm was 4.64 ± 1.02 in the control group which increased insignificantly to 5.35 ± 1.06 following DGC. A significant increase (8.85 ± 1.80) was seen after DGC-Zeta compared to the control and DGC groups (Fig. 2b), respectively. Assessment of ubiquitin was also performed in 14 semen samples during capacitation and the results of (Fig. 2c) shows that the percentage of ubiquitin increases during capacitation.
Dot plot of sperm ubiquitination status in control, DGC and DGC-Zeta in a semen sample (a). Comparison of percentage ubiquinated sperm was assessed by flow cytometry in the control, DGC and DGC-Zeta groups in 30 semen samples (b). Assessment of the percentage of ubiquinated sperm during incubation in control, DGC and DGC-Zeta groups in 14 semen samples (c). Common letters are significantly different at p < 0.05
Figure 3a and b show the image of annexin positive sperm and the related histogram of a semen sample before and after DGC- Zeta. The mean values of the percentage of An-PI-/PI- and An+PI-/PI- sperm are presented in Fig. 3c. The percentage of annexin positive viable sperm increased from 12.55 ± 2.80 to 31.14 ± 3.98 upon implementation of Zeta, and consequently the percentage of annexin negative viable sperm decreased from 87.44 ± 2.80 to 68.84 ± 3.98. The percentage of annexin positive viable sperm was also increased by incubation of sperm in capacitation medium (T0 = 7.10 ± 1.56, T30 = 11.42 ± 3.62, T60 = 8.97 ± 2.03, T90 = 6.41 ± 1.54 and T DGC-Zeta = 13.18 ± 2.35).
Comparison of the percentage of non-capacitated, capacitated and acrosome reacted in these groups is shown in Fig. 4. The mean percentages of the F pattern in these groups were 38.00 ± 3.48 (control), 24.94 ± 2.75 (DGC-0 min), 17.45 ± 2.56 (DGC-30 min), 11.22 ± 1.73 (DGC-60 min), 8.26 ± 1.67 (DGC-90 min) and 16.92 ± 3.10 (DGC-Zeta). The percentage of F pattern reduced gradually over time while the percentage of the B and AR patterns increased over the same period with slight alteration. Although the maximum time taken to carry out the DGC-Zeta procedure ranged from 10 to 20 min, the pattern capacitation of the DGC-Zeta was similar to when the sperm remained in the capacitation medium for 60 min.
Comparison of the percentage of sperm non-capacitated, capacitated and acrosome reacted sperm during capacitation in control, DGC and DGC-Zeta groups (a). The percentage of CTC pattern sperm during capacitation in aformation groups from 21 samples (b). Common letters are significantly different at p < 0.05
The mean percentage of protamine deficiency assessed by CMA3 staining in the control, DGC and DGC-Zeta groups were 41.56 ± 3.43, 29.64 ± 2.74 and 20.57 ± 3.07, respectively. Comparison of the mean values of protamine deficiency between the two procedures with the control group showed significant reduction in the percentage of protamine deficiency following the DGC and DGC-Zeta procedures when compared with the control group (p < 0.05). The difference between the mean values of protamine deficiency in the DGC and DGC-Zeta groups were also significant (Table 2).
The percentage of DNA-damaged sperm gradually reduced following DGC (17.47 ± 3.52) and DGC-Zeta (6.98 ± 1.45) compared to the control (21.97 ± 3.84). Comparison between the three groups only revealed a significant difference between the control and DGC-Zeta and between DGC and DGC-Zeta. Unlike the aforementioned parameters, a significant difference between the DGC and control was not observed (Table 2).
Discussion
Spermatogonia stem cells clonally expand and differentiate to produce sperm. During this process 75% of potential sperm are disposed via physiological apoptosis to assure intact and healthy spermatozoa are available to guarantee the health of future progeny. Although disputable, it is believed some sperm bypass these natural selection procedures and are identified in ejaculate, a process called abortive apoptosis [4]. To ensure that such a sperm are made redundant, the reproductive system has implemented another natural defense system, known as the ubiquitin-proteasome system in the epididymis. This system removes defective sperm and prevents them from reaching the ejaculate [24]. However despite these safety mechanisms, for unknown reasons, annexin V, FAS or ubiquitin positive sperm are found at higher frequencies in the ejaculate of infertile compared to fertile individuals, which suggest that these sperm have bypassed these mechanisms [7, 25]. Therefore, to avoid insemination of these sperm during ICSI, novel sperm selection procedures based on these properties or other functional properties of sperm have been suggested. Therefore, this study aimed to evaluate changes in EPS as assessed by annexin V and ubiquitin during the DGC-Zeta procedure and whether these were suitable bio-markers for the assessment quality of selected sperm.
Analysis of EPS revealed that the selected sperm population post DGC-Zeta showed a higher percentage of ubiquitin positive sperm compared to the control and DGC groups (Fig. 2b). This observation was contrary to our expectation since ubiquitination has been considered as a sign for the removal of defective sperm in the epididymis. Study of the literature reveal that ubiquitination in the epididymis is process by which defective sperm are removed while reorganization of ubiquitined protein onto sperm surface post capacitation is part of sperm oocyte interaction with zona pellucida. These proteins might become redundant and therefore eliminated by the protease system of the oocyte post-fertilization [26–28]. Therefore, we expect that the increase in rate of ubiquitination post DGC-Zeta may be part of the natural process of fertilization and these proteins may become exposed during the process of capacitation. Therefore, we assessed the percentage of ubiquitination in the DGC sample which was allowed to undergo capacitation. The results revealed that the percentage of ubiquitinated sperm increased gradually by 60 min in the capacitation medium and then subsequently decreased (Fig. 2c). Additionally our results showed that during the Zeta procedure, even in the absence of serum, a process similar to capacitation is induced, which was confirmed by CTC. Therefore, this revealed a possible association between capacitation and the percentage of positive ubiquitinated sperm. These results are in agreement with a previous report which has stated that capacitated mouse sperm can interact with the anti-ubiquitin protein while no interaction occurs between such antibodies with incapacitated sperm [27, 28].
In contrast to our expectation, results of EPS revealed that a percentage of viable sperm presenting EPS increase while the percentage of viable sperm without EPS decreases post DGC-Zeta (Fig. 3). Grunewald stated that “the knowledge gained from studies of somatic cells cannot be transferred without experimental proof to sperm which is transcriptionally inactive” and this author contributed to the controversies in apoptotic signaling in sperm [29, 30].
However, before hypothesizing the reasons for increased EPS in the DGC-Zeta group, an extensive literature review regarding EPS in sperm revealed that: 1) EPS mediates phagocytosis of apoptotic spermatogenetic cells by Sertoli cells [31] (2) EPS in ejaculated sperm before capacitation may represent apoptotic sperm which have escaped phagocytosis [32] (3) indirect evidence suggests that sperm presenting EPS in the ejaculate have a lower ability to undergo capacitation. In contrast, it has been reported that EPS increase upon introduction into capacitation medium and induction of an acrosome reaction in human spermatozoa. In addition, EPS at the sperm membrane may play a role during sperm oocyte interaction, such as the interaction of apoptotic cells with phagocytes [33]. Furthermore, apoptosis and capacitation have an inverse relation, which suggests that sperm undergoing capacitation are non-apoptotic, consequently apoptotic sperm have a lower ability to undergo capacitation [30]. Therefore, not all the external apoptotic factors, like H2O2, can induce PE externalization while they activate the capases which suggests that PS externalization in sperm post-ejaculation is not directly associated with apoptosis [34]. With these in mind, it can be concluded that EPS in ejaculate before capacitation may be an indicator of abortive apoptosis, however, increase in EPS following exposure of sperm to capacitation medium and induction of an acrosome reaction are part of the physiological process to achieve fertilization [32]. Therefore, increases in the rate of capacitation and EPS in DGC-Zeta selected spermatozoa may indicate that the Zeta procedure is inducing capacitation. Since there is an inverse relation between capacitation and apoptosis, it is very unlikely that Zeta selected sperm which present with an increased rate of PE externalization are apoptotic.
Since our result proposes that the increased ubiquitination and EPS are part of physiological process of capacitation, that may be induced by Zeta produce, therefore, we assessed the semen sample post DGC-Zeta for DNA fragmentation and also for protamination status and morphology assessment and showed that this procedure can select sperm with better morphology, normal protamination and lower DNA fragmentation rate.
Indeed, a recent study which selected acrosome-reacted sperm based on birefringence properties of sperm have concluded that the chance of obtaining a high quality embryo and pregnancy increase through this selection [35]. Therefore, the improvement in ICSI results as a consequence of the Zeta selection procedure, in addition to selection of sperm with reduced DNA fragmentation, and normal protamine content can be attributed to the increased chance of insemination of sperm which might have undergone capacitation and possibly an acrosome reaction.
Recently Varum et al. have reported that even though ubiquitination and apoptosis are independent phenomena, however all annexin positive sperm are also ubiquitinated. Therefore, our results are also consistent with this report which shows a concomitant increase in ubiquitination and annexin staining [36].
In conclusion, our results suggest that following DGC-Zeta the percentage of ubiquitination and annexin increases. These increases appear to be normal consequences of capacitation and may be considered as physiological processes which further confirm the ability of the Zeta procedure to select normal sperm in terms of these biomarkers and other chromatin markers, such as TUNEL and CMA3. In addition, the use of annexin and ubiquitin as biomarkers for the assessment of sperm should be considered along with the sperm’s capacitation status.
References
Agarwal A, Allamaneni SS. The effect of sperm DNA damage on assisted reproduction outcomes. Minerva Ginecol. 2004;56:235–45.
Carrell DT, Liu L. Altered protamine 2 expression is uncommon in donors of known fertility, but common among men with poor fertilizing capacity, and may reflect other abnormalities of spermiogenesis. J Androl. 2001;22:604–10.
Venkatesh S, Shamsi MB, Dudeja S, Kumar R, Dada R. Reactive oxygen species measurement in neat and washed semen: comparative analysis and its significance in male infertility assessment. Arch Gynecol Obstet. 2010.
Sakkas D, Seli E, Bizzaro D, Tarozzi N, Manicardi GC. Abnormal spermatozoa in the ejaculate: abortive apoptosis and faulty nuclear remodelling during spermatogenesis. Reprod Biomed Online. 2003;7:428–32.
Anzar M, He L, Buhr MM, Kroetsch TG, Pauls KP. Sperm apoptosis in fresh and cryopreserved bull semen detected by flow cytometry and its relationship with fertility. Biol Reprod. 2002;66:354–60.
Sutovsky P, Moreno R, Ramalho-Santos J, Dominko T, Thompson WE, Schatten G. A putative, ubiquitin-dependent mechanism for the recognition and elimination of defective spermatozoa in the mammalian epididymis. J Cell Sci. 2001;114:1665–75.
Almeida C, Sousa M, Barros A. Phosphatidylserine translocation in human spermatozoa from impaired spermatogenesis. Reprod Biomed Online. 2009;19:770–7.
Berkovitz A, Eltes F, Soffer Y, Zabludovsky N, Beyth Y, Farhi J, et al. ART success and in vivo sperm cell selection depend on the ultramorphological status of spermatozoa. Andrologia. 1999;31:1–8.
Avendaño C, Franchi A, Taylor S, Morshedi M, Bocca S, Oehninger S. Fragmentation of DNA in morphologically normal human spermatozoa. Fertil Steril. 2009;91:1077–84.
Nasr-Esfahani MH, Razavi S, Vahdati AA, Fathi F, Tavalaee M. Evaluation of sperm selection procedure based on hyaluronic acid binding ability on ICSI outcome. J Assist Reprod Genet. 2008;25:197–203.
Razavi SH, Nasr-Esfahani MH, Deemeh MR, Shayesteh M, Tavalaee M. Evaluation of Zeta and HA-binding methods for selection of spermatozoa with normal morphology, protamine content and DNA integrity. Andrologia. 2010;42:13–9.
Kheirollahi-Kouhestani M, Razavi S, Tavalaee M, Deemeh MR, Mardani M, Moshtaghian J, et al. Selection of sperm based on combined density gradient and Zeta method may improve ICSI outcome. Hum Reprod. 2009;24:2409–16.
Khajavi NA, Razavi S, Mardani M, Tavalaee M, Deemeh MR, Nasr-Esfahani MH. Can Zeta sperm selection method, recover sperm with higher DNA integrity compare to density gradient centrifugation? IJRM. 2009;7:73–7.
Dirican EK, Ozgün OD, Akarsu S, Akin KO, Ercan O, Uğurlu M, et al. Clinical outcome of magnetic activated cell sorting of non-apoptotic spermatozoa before density gradient centrifugation for assisted reproduction. J Assist Reprod Genet. 2008;25:375–81.
Monqaut AL, Zavaleta C, López G, Lafuente R, Brassesco M. Use of high-magnification microscopy for the assessment of sperm recovered after two different sperm processing methods. Fertil Steril. 2010.
World Health Organization. Examination and processing human semen. 5th ed. New York: Cambridge University Press; 2010.
Nasr Esfahani MH, Razavi S, Mardani M, Khajavi NA, Deemeh MR, Tavalaee M. The comparison of efficiency of density gradient centrifugation and zeta methods in separation of mature sperm with normal chromatin structure. J Yakhteh. 2009;11:168–75.
Nasr-Esfahani MH, Tavalaee M, Deemeh MR, Arbabian M, Parrington J. Can assessment of total acrosin activity help predict failed or low fertilization rate ICSI for implementation of artificial oocyte activation? Open Androl J. 2010.
Sutovsky P, Terada Y, Schatten G. Ubiquitin-based sperm assay for the diagnosis of male factor infertility. Hum Reprod. 2001;16:250–8.
Hoogendijk CF, Kruger TF, Bouic PJ, Henkel RR. A novel approach for the selection of human sperm using annexin V-binding and flow cytometry. Fertil Steril. 2009;91:1285–92.
Muratori M, Porazzi I, Luconi M, Marchiani S, Forti G, Baldi E. AnnexinV binding and merocyanine staining fail to detect human sperm capacitation. J Androl. 2004;25:797–810.
Chan PJ, Jacobson JD, Corselli JU, Patton WC. A simple Zeta method for sperm selection based on membrane charge. Fertil Steril. 2006;85:481–6.
DasGupta S, Mills CL, Fraser LR. A possible role for Ca(2+)-ATPase in human sperm capacitation. J Reprod Fertil. 1994;102:107–16.
Muratori M, Marchiani S, Criscuoli L, Fuzzi B, Tamburino L, Dabizzi S, et al. Biological meaning of ubiquitination and DNA fragmentation in human spermatozoa. Soc Reprod Fertil Suppl. 2007;63:153–8.
Hodjat M, Akhondi MA, Al-Hasani S, Mobaraki M, Sadeghi MR. Increased sperm ubiquitination correlates with abnormal chromatin integrity. Reprod Biomed Online. 2008;17:324–30.
Nuell MJ, Stewart DA, Walker L, Friedman V, Wood CM, Owens GA, et al. Prohibitin, an evolutionarily conserved intracellular protein that blocks DNA synthesis in normal fibroblasts and HeLa cells. Mol Cell Biol. 1991;11:1372–81.
Sutovsky P. Ubiquitin-dependent proteolysis in mammalian spermatogenesis, fertilization, and sperm quality control: killing three birds with one stone. Microsc Res Tech. 2003;61:88–102.
Hongmei W, Changcheng S, Chongwen D, Weixian Shi, Cunxi Li, Dayuan C, Yongchao W. Effects of ubiquitin-proteasome pathway on mouse sperm capacitation, acrosome reaction and in vitro fertilization. Chin Sci Bull. 2002;47:127–32.
Grunewald S, Paasch U, Glander HJ, Anderegg U. Mature human spermatozoa do not transcribe novel RNA. Andrologia. 2005;37:69–71.
Grunewald S, Kriegel C, Baumann T, Glander HJ, Paasch U. Interactions between apoptotic signal transduction and capacitation in human spermatozoa. Hum Reprod. 2009;24:2071–8.
Kawasaki Y, Nakagawa A, Nagaosa K, Shiratsuchi A, Nakanishi Y. Phosphatidylserine binding of class B scavenger receptor type I, a phagocytosis receptor of testicular sertoli cells. J Biol Chem. 2002;277:27559–66.
Martin G, Sabido O, Durand P, Levy R. Phosphatidylserine externalization in human sperm induced by calcium ionophore A23187: relationship with apoptosis, membrane scrambling and the acrosome reaction. Hum Reprod. 2005;20:3459–68.
Grunewald S, Baumann T, Paasch U, Glander HJ. Capacitation and acrosome reaction in nonapoptotic human spermatozoa. Ann N Y Acad Sci. 2006;1090:138–46.
Taylor SL, Weng SL, Fox P, Duran EH, Morshedi MS, Oehninger S, et al. Somatic cell apoptosis markers and pathways in human ejaculated sperm: potential utility as indicators of sperm quality. Mol Hum Reprod. 2004;10:825–34.
Collodel G, Federico MG, Pascarelli NA, Geminiani M, Moretti E. Natural sperm birefringence can be used to estimate sperm viability and morphology. Syst Biol Reprod Med. 2010.
Varum S, Bento C, Sousa AP, Gomes-Santos CS, Henriques P, Almeida-Santos T, et al. Characterization of human sperm populations using conventional parameters, surface ubiquitination, and apoptotic markers. Fertil Steril. 2007;87:572–83.
Acknowledgment
The authors express their gratitude to Royan Institute for its financial support and the staff of Isfahan Fertility and Infertility Center for their kind collaboration.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Zeta induces capacitation which in turn increases rate of ubiquitination and external phosphatidyl serine.
Rights and permissions
About this article
Cite this article
Zarei-Kheirabadi, M., Shayegan nia, E., Tavalaee, M. et al. Evaluation of ubiquitin and annexin V in sperm population selected based on density gradient centrifugation and zeta potential (DGC-Zeta). J Assist Reprod Genet 29, 365–371 (2012). https://doi.org/10.1007/s10815-011-9689-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-011-9689-3