Abstract
Funding for early intensive behavioral intervention (EIBI) for children with autism spectrum disorder is rapidly expanding. Yet we know little about children’s utilization, and research on inequities in utilization is lacking. We examined the relationship between utilization during the first year of EIBI and (a) child race-ethnicity and (b) neighborhood characteristics. Using a sample of children eligible for a Medicaid waiver through a novel policy of presumptive eligibility (N = 108), we estimated a series of two-level growth curve models. Children’s average utilization ranged between 24 and 48% of weekly hours, and utilization did not differ by race-ethnicity or neighborhood during the first year. Findings underscore the need to monitor utilization of EIBI and warrant research on the feasibility of EIBI provision in the general population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An increasing number of children meet diagnostic criteria for autism spectrum disorder (ASD), a neurodevelopmental disorder characterized by social communication challenges and restricted or repetitive behaviors or interests (American Psychiatric Association 2013; Centers for Disease Control and Prevention 2016, 2018). In response, Medicaid coverage of the most effective approach for treating ASD, or early intensive behavioral intervention (EIBI) (Peters-Scheffer et al. 2011; Virués-Ortega 2010), is expanding. In fact, in 2014 the Centers for Medicare and Medicaid services directed states to include applied behavior analysis (ABA), on which EIBI is based, as one service available to children with ASD through Early Periodic Screening, Diagnosis and Treatment (Centers for Medicare and Medicaid Services 2014). Current recommendations include 20 to 40 h of EIBI per week for 1–4 years (Reichow et al. 2014). Evidence suggests that children with greater utilization (i.e., children who use more weekly hours) achieve better outcomes, and that children make the most gains early in treatment (Granpeesheh et al. 2009; Howlin et al. 2009; Linstead et al. 2017; Makrygianni and Reed 2010; Reed and Osborne 2012; Reichow and Wolery 2008; Virués-Ortega 2010).
With the goal of enrolling children in EIBI as early as possible, states are transforming policy to promote early identification of ASD. Recently, researchers detailed a successful and unique policy of presumptive eligibility for an EIBI Medicaid waiver, which received federal approval in October 2012 (Rotholz et al. 2017). Specifically, children who received EIBI through BabyNet (South Carolina’s Early Intervention Program) at least 30 days prior to their third birthday and screened positive for ASD bypassed a wait list for a Medicaid waiver that provided EIBI to children between the ages of three and ten who were diagnosed by age eight. On their third birthday, if children had received an ASD diagnosis, the state allotted up to 40 h per week of EIBI for 3 years.
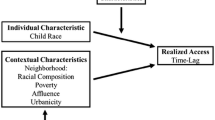
Despite this policy’s promise, unknown is children’s utilization post-enrollment and the role of social characteristics in utilization. Indeed, the Interagency Autism Coordinating Committee encourages the use of state Medicaid and administrative data to better understand inequities in access and utilization of ASD treatment (Interagency Autism Coordinating Committee (IACC) 2017), as existing literature suggests that children with ASD experience racial-ethnic (Magaña et al. 2013; Parish et al. 2012; Shattuck et al. 2009; Zuckerman et al. 2017b), socioeconomic (Irvin et al. 2012; Shattuck et al. 2009), and geographic inequities (Murphy and Ruble 2012; Thomas et al. 2011) in treatment utilization. With potential to inform state practices in the delivery of Medicaid-funded ASD treatment, the purpose of this study is to seize the time-sensitive opportunity to expand on recent work on this unique cohort of children (i.e., BabyNet users) by examining (1) treatment utilization during their first year in the waiver and (2) the relationship between utilization and child race-ethnicity, and utilization and neighborhood poverty, affluence, racial composition, and urbanicity.
Methods
In 2007, South Carolina became one of the first states to offer a 1915(c) Home and Community Based Services (HCBS) Medicaid waiver specifically for EIBI. For a decade, the waiver provided up to 3 years of EIBI to children between the ages of 3 and 10. We created a comprehensive dataset of all children with ASD who enrolled in the waiver between the date that the first child enrolled (February 6, 2007) and the end of the first quarter of calendar year 2015 (March 31, 2015). Detailed information about the waiver and data integration are provided elsewhere (Yingling et al. 2017a). Briefly, we integrated data from the South Carolina Department of Disabilities and Special Needs (DDSN) and the Office of Revenue and Fiscal Affairs (RFA). The current sample (N = 108) is a subset of children who enrolled in the waiver after a policy change implemented in October 2012 made them presumptively eligible to enroll on their third birthday (Fig. 1 illustrates the timing of data collection and policy implementation). They were included because they received at least one therapy session in a minimum of 26 weeks during the first year (52 weeks) of treatment. We applied the latter inclusion criterion because of the focus on typical utilization during the first year of enrollment. If children did not receive between 26 and 52 weeks of treatment, they arguably did not have a trajectory to analyze and could have significantly biased the models. Also, children’s initial therapy session must have taken place on or prior to March 30, 2014 to ensure they had the opportunity to participate in 52 weeks of therapy before data collection concluded. We received approval from an institutional review board.
Measures
Dependent Variable
We measured treatment utilization, the outcome of interest, as the percent of allotted weekly hours used. EIBI providers conduct a thorough assessment using tools such as the Assessment of Basic Language and Learning Skills Revised, Peabody Picture Vocabulary Test IV, Expressive Vocabulary Test II, and Vineland Adaptive Behavioral Skills II. Based on results, providers recommend how many weekly hours children need. Then, administrators budget for the recommended number of hours and record them in the agency’s central database. We first divided the total year budget by 52 weeks to determine the number of allotted weekly hours. For example, the quotient of a budget of 1560 h divided by 52 weeks is 30 h per week. Next, we calculated the quotient of the number of hours a child used each week divided by the number of allotted weekly hours. For instance, if a child used 15 of 30 allotted hours in the first week, a child’s utilization in the first week is 50%. We calculated this quotient for all 52 weeks.
Level-1 Independent Variable
The unit of time in the model is weeks, coded as Week 0–Week 51. The intercept (Week 0) is the first week a child received services, and Week 51 is the final week a child received services during the first year of treatment.
Level-2 Independent Variables
We combined data from DDSN and RFA to create the primary variable child race-ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic other, and unknown). Both sources provided the category unknown. Hispanic includes children identified as Hispanic white and Hispanic black; the latter category included too few children to analyze separately, and ethnicity was prioritized. We derived non-Hispanic other from a range of categories in the original data too small to analyze (i.e., Asian, Hawaiian/Pacific Islander and American Indian). No children were categorized as non-Hispanic other. RFA assigned a census tract ID to children based on the residential address recorded by DDSN. Racial composition is the percent of white residents in the census tract (grand-mean centered). Neighborhood poverty is a composite variable calculated as a z-score computed from the sample’s census tract grand-mean of the following variables commonly used to measure neighborhood poverty (Leventhal and Brooks-Gunn 2003): (a) single parent female-headed households, (b) percent of people below the federal poverty level, (c) residents who receive cash assistance, (d) residents enrolled in SNAP, (e) residents who receive SSI, and (f) people who are unemployed. Also a composite measure, neighborhood affluence, commonly used to measure neighborhood quality, is a z-score computed from the sample’s census tract grand mean of variables often used to measure neighborhood affluence (Leventhal and Brooks-Gunn 2003): (a) median household income, (b) percent of residents with professional/managerial employment, and (c) percent of residents with a Bachelor’s degree or higher. We calculated poverty and affluence by taking the average of the z-scores for each of the indicators listed above for each composite variable. To measure urbanicity, we used Rural–Urban Commuting Areas (RUCA) to create dummy variables for urban, suburban, and rural census tracts. RUCA codes are at the level of census tracts and are described by the United States Department of Agriculture as codes that use “measures of population density, urbanization, and daily commuting” (United States Department of Agriculture 2016). The most recent RUCA codes are used in this study and are based on the 2010 decennial census and the 2006–2010 American Community Survey.
Time-Invariant Covariates
Covariates included sex (1 = female, 0 = male) and family socioeconomic status (SES), measured by the payment category billed by waiver providers, which is most often determined by family income. Sources included payment under the Tax Equity and Fiscal Responsibility Act (TEFRA), which assists families with incomes too high to qualify for Medicaid, Supplemental Security Income (SSI), which assists low-income families, or “other” source.
Missing Data
Of the 115 children who met inclusion criteria, 5 had no census tract ID. Missing data across all children and all variables was less than 1%. There was no evidence that data were systematically missing. Because sample size was small and the number of explanatory variables were limited, missing data procedures were not possible. Although three children in the sample had siblings also enrolled in the waiver, none of the siblings met inclusion criteria and therefore, random selection of one sibling was unnecessary.
Of the 177 children who began treatment 52 weeks prior to the end of data collection, 62 children used less than 26 weeks of treatment. Of these, 7 were missing demographic data. For informational purposes only, Table 1 includes demographic characteristics of the 55 children excluded from the study.
Statistical Analyses
Although we intended to employ three-level growth curve models (i.e., time at level-1, children at level-2, and neighborhoods at level-3), due to the high number of singletons among census tracts (i.e., one child per census tract), we estimated contextual two-level growth curve models. This is appropriate when the interest is in the context of the neighborhood rather than differences between neighborhoods (Diez 2002). This approach allowed the estimation of mean utilization from a child’s initial therapy session (Week 0) to the end of the first year of treatment (Week 51) as well as child differences in change in utilization over time.
To determine the best fitting model, we used PROC MIXED in SAS® 9.4 with maximum likelihood (ML) estimation and Satterthwaite degrees of freedom. We estimated four models. First, we estimated an unconditional model with no predictors (Model 1). The intraclass correlation coefficient (ICC) revealed that 16% of the variability in utilization was between children. After estimating the unconditional model, we plotted average utilization for all 52 weeks. Because this plot did not reveal a linear average utilization trajectory (Fig. 1), we assessed the form of change in utilization by estimating one level-1 model with time as the only level-1 predictor and random slope and a second level-1 model with both time and time2 (i.e., quadratic term) as level-1 predictors and random slopes. Because the latter did not converge, we concluded that there was no curvature and did not include the quadratic in subsequent models. We then estimated a main effect model (Model 3) with time and level-2 variables, including child race-ethnicity, neighborhood characteristics, and covariates. Given the small sample, we only ran interaction models with predictors that demonstrated differences at baseline. Therefore, we ran one cross-level interaction model (Model 4) to determine if the relationship between the significant level-2 predictor (i.e., child race-ethnicity) varied over time. To examine model fit, we compared differences in -2 Log likelihood. This process revealed Model 3 as best fitting. To test model assumptions, we ran the MIXED_DX macro to examine residuals for violations of distributional assumptions at both level-1 and level-2 and to examine the data for influential outliers. No violations were detected.
Results
Table 1 presents descriptive statistics. The sample included mostly males (83%), and most children identified as white (42%), lived in an urban neighborhood (75%), and had higher family SES (42%). Three variables not included in analyses—number of hours allotted to children, number of weeks used during the year, and the number of hours children used—are included in Table 1 for informational purposes only. As depicted in Fig. 2, unadjusted weekly percent of utilization during the first year of treatment ranged from 24 to 48%.
Table 2 presents parameter estimates and fit statistics for all models. Model 1 indicates that on average children used 37% of allotted hours during their first week of EIBI treatment (b = 37.07, p < .0001) and that there was significant variability between children in their utilization during Week 1 (b = 913.14, p < .0001). Sixteen percent of the variation in utilization occurred between children meaning that 84% of utilization variation occurred within children. Model 2 shows that on average children had a very small increase in their utilization over time (b = 0.18, p < .0001) and that children varied in their changes in utilization (b = 878.56 p < .0001). Model 3 contains the level-2 predictors and covariates. Compared to non-Hispanic white children, Hispanic children used an average of 9% less treatment hours during Week 1 (b = -8.96, p < .05). Although Model 3 suggests a statistically significant difference in utilization at Week 1 between Hispanic children and non-Hispanic white children, the non-significant cross-level interaction shown in Model 4 indicates that the initial racial difference did not persist over time. Pseudo R2 calculations demonstrate that the growth model explained 46% of the ICC, leaving 54% of the observed variability between children unexplained.
Discussion
During their first year in the EIBI waiver, children used an average of 37% of allotted hours per week, or 14.5 h. Average utilization was highest during Week 1, perhaps a function of commencing treatment. In subsequent weeks, average utilization primarily ranged between 30 and 44%, although in Week 2 dropped to as low as 24%. Results provide evidence of a relationship between child race-ethnicity and utilization during Week 1. Specifically, compared to non-Hispanic white children, Hispanic children used an average of 9% less treatment hours. However, we detected no relationship between child race-ethnicity and utilization over time. There was neither a significant relationship between neighborhood characteristics and utilization during Week 1 nor utilization over time.
The finding that Hispanic children received less hours during Week 1 aligns with evidence that parents of Latino children with ASD are less likely to enroll in an EIBI waiver, despite reporting more unmet needs (Magaña et al. 2013). However, the finding that this difference does not persist over time is perplexing, as children’s transition into the waiver is administrative in nature; on the child’s third birthday the funding source for EIBI (not providers) changes from BabyNet to the waiver. One potential explanation is that language barriers, which research indicates are influential in access to ASD services (Zuckerman et al. 2017b), are resolved soon after enrollment. Because of the small sample size, and because low utilization translates to a difference of only 1–2 h per week, further investigation is necessary.
Results complicate existing research that records racial-ethnic and neighborhood inequities in utilization among children with ASD. In one study, compared to black and Hispanic children, white and Asian children increased their intensity in weekly utilization of individual services outside of school (Siller et al. 2014). Similarly, in a study on enrollment in Wisconsin’s EIBI waiver, researchers documented that census tracts that had a higher percentage of people who were white and a higher percentage of families with incomes ≥ 200% of the federal poverty level were more likely to enroll (Shattuck et al. 2009). In the same program, white children were more likely to enroll than Latino children (Magaña et al. 2013). It is possible that current findings are explained by the measurement of weekly utilization. In any given week, children in the current sample used zero treatment hours. There are countless reasons for this, such as holidays or special events, family illnesses, emergencies or vacations, or provider cancellations. In this study, these factors are unknown. Additionally, there may not be racial and neighborhood differences in utilization due to the nature of the sample. That is, children who never enrolled in the waiver may be qualitatively different from those who enrolled, and the lack of statistically significant findings could be a function of sample size. Future research should continue to investigate these relationships, especially given recent evidence that child race-ethnicity and neighborhood affluence are associated with utilization of EIBI in older children (Yingling et al. 2019).
Perhaps most significant, despite benefiting from presumptive eligibility for EIBI at the prime age of three, children’s average utilization, which never reached 50%, is surprisingly low. Evidence suggests that earlier and greater utilization yields better outcomes (Granpeesheh et al. 2009; Howlin et al. 2009; Makrygianni and Reed 2010; Reed and Osborne 2012; Reichow and Wolery 2008; Virués-Ortega 2010). Yet in the current sample, earlier receipt does not appear to yield greater utilization. To explore this issue, we conducted a separate analysis of utilization among older children who enrolled traditionally in the waiver. Interestingly, these children used slightly more allotted hours (average of 41%) than children with presumptive eligibility.
At minimum, the current study serves as a red flag to Medicaid administrators across the country that large scale implementation of EIBI may require an investment of time and resources in areas other than EIBI provision, such as parent education, provider recruitment strategies, and intersystem collaboration. Specifically, these findings raise at least two questions for health care providers. First, is the intensity of EIBI currently recommended feasible in the general population? This question is fundamental to future inquiry and is especially critical given the potential of EIBI to improve outcomes and increase societal savings (Chasson et al. 2007; Jacobson et al. 1998), the recent, sizeable investment made in private and public health coverage (Centers for Medicare and Medicaid Services 2014; Douglas et al. 2017; Maglione et al. 2016), and the need to maximize limited resources. Second, if feasible, what is required to increase utilization?
To answer these questions, a mixed-methods research agenda is required. Future research must include measurement of weekly utilization using large, representative samples, clearly define high utilization, and identify modifiable factors associated with utilization. Regarding the latter, several studies offer direction. Parents report that the inability to provide EIBI in the school setting negatively impacts utilization (Yingling et al. 2017b). This challenge should be less prominent among three-year-old children. However, although utilization of EIBI in BabyNet may not change simply by transitioning into the waiver, it is possible that after their third birthday, children’s eligibility for school-related services provided through Part B of the Individuals with Disabilities and Education Act (The Individuals with Disabilities Education Act, Reauthorization 2004 2004) introduce scheduling challenges (Yingling et al. 2017b). Is high EIBI utilization possible, therefore, when it cannot be delivered in the educational setting (South Carolina Department of Disabilities and Special Needs 2012)? Another consideration is that parents are presented with and select myriad treatments, and less effective interventions (Cohen et al. 2006) might consume limited hours otherwise available for EIBI (Bilaver et al. 2016; Green et al. 2006; Thomas et al. 2006; Yingling et al. 2017b). Also, parents’ perceptions of ASD and treatment may influence utilization (Al Anbar et al. 2010; Zuckerman et al. 2015). If parents in EIBI feel that their children are overburdened by school and treatment demands (Yingling et al. 2017b) and rank intuition as more important than empirical evidence when choosing treatments (Carlon et al. 2015), what are effective means for increasing utilization? Moreover, parents describe negative aspects of EIBI, such as reduced family privacy and challenges retaining high quality providers (Grindle et al. 2008; Yingling et al. 2017b). Do all parents understand the challenges of EIBI implementation prior to enrollment? Conversely, do they understand the positive elements (Grindle et al. 2008)? Answering these questions in the context of Medicaid-funded EIBI using qualitative methods (e.g., focus groups, interviews, case studies) is paramount to understanding treatment utilization and to determining whether and how utilization in state plans can be increased. For instance, prior to enrollment, parents may benefit from education on the positive association between weekly dosage and child outcomes. Furthermore, factors at the provider level likely contribute to utilization. In South Carolina, the presumptive eligibility policy introduced new children into the waiver system. Thus, it is likely that provider shortages, which were a challenge early in the waiver (South Carolina Department of Disabilities and Special Needs 2014) and certainly contribute to long wait lists (L & M Policy Research, LLC 2014; Yingling et al. 2017a), played a role in utilization. This issue and others, such as provider reliability and quality (Grindle et al. 2008), deserve national attention.
Limitations
Despite this study’s significant contribution, because the sample only includes children enrolled in South Carolina, generalizability to waivers in other states is limited. In addition, since data collection for this study, the state dissolved the waiver to prevent service duplication (Centers for Medicare and Medicaid Services 2014). Presently, the state provides ASD treatment, including EIBI, via its Medicaid state plan. This change in funding restricts generalizability. Yet for 10 years, South Carolina was among the most generous states for EIBI provision, and DDSN maintained records that, to our knowledge, do not exist in other states. To disregard the knowledge gained due to this limitation—which is always a risk when researching public services—would be misguided.
Although the racial-ethnic data available in the current sample is a substantial improvement reportedly available in other waivers (Shattuck et al. 2009), it remains a primary limitation. Compared to the racial distribution of South Carolina, although Hispanic children are slightly overrepresented in the sample, non-Hispanic black and non-Hispanic white children are underrepresented. It is possible that the sizeable proportion of unknown race-ethnicity influenced findings. Also important to consider is the persistence of inequities in age of diagnosis (Daniels and Mandell 2014). Because the current sample only included children diagnosed before their third birthday, their utilization may be qualitatively different than children diagnosed after their third birthday. Also, children’s utilization of EIBI in BabyNet was unavailable. Thus, it was not possible to compare utilization before and after enrollment. What percent of hours received were home- versus center-based is also unclear. Although waiver policy required a minimum of 50% of hours to be at home, the remaining 50% could be either, and this could impact utilization. Additionally, standardized measures of children’s abilities, which may be associated with utilization, (e.g., IQ, Adaptive Behavior) (Zuckerman et al. 2017a), and factors related to providers that likely influence utilization, were unavailable in the current study. However, children’s severity is captured in the calculation of treatment utilization. Based on the child’s assessed need, or “severity,” providers prescribed the number of hours a child should receive. Thus, we used each child’s utilization of their individual recommended dosage to examine utilization. Finally, we used conventional growth modeling, a variable-centered approach that assumes that individuals come from a single population and that a single (i.e., the average) growth trajectory can effectively estimate an entire population. Although inappropriate due to the small sample size, a person-centered approach would allow the assignment of children to unique utilization trajectories (Jung and Wickrama 2008).
Conclusion
This study provides important insight into treatment utilization among a unique cohort of young children with ASD who benefited from an innovative policy of presumptive eligibility for an EIBI waiver. In addition to warranting future research into the role of child race-ethnicity in utilization, results suggest a need to investigate barriers to EIBI utilization among pre-school children in Medicaid state plans. Given the importance of high utilization to promote optimal outcomes for children and families, efforts to increase utilization are worthy of examination and require discussion.
References
Al Anbar, N. N., Dardennes, R. M., Prado-Netto, A., Kaye, K., & Contejean, Y. (2010). Treatment choices in autism spectrum disorder: The role of parental illness perceptions. Research in Developmental Disabilities, 31(3), 817–828. https://doi.org/10.1016/j.ridd.2010.02.007.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Arlington, VA: American Psychiatric Association.
Bilaver, L. A., Cushing, L. S., & Cutler, A. T. (2016). Prevalence and correlates of educational intervention utilization among children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(2), 561–571. https://doi.org/10.1007/s10803-015-2598-z.
Carlon, S., Carter, M., & Stephenson, J. (2015). Decision-making regarding early intervention by parents of children with autism spectrum disorder. Journal of Developmental and Physical Disabilities, 27(3), 285–305. https://doi.org/10.1007/s10882-014-9415-z.
Centers for Disease Control and Prevention. (2016). Prevalence of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2012. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, DC: 2002), 65(3), 1–23.
Centers for Disease Control and Prevention. (2018). Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2014. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, DC: 2002), 67(6), 23.
Centers for Medicare and Medicaid Services. (2014). Medicaid and CHIP FAQs: Services to address autism. Department of Health and Human Services. Retrieved from http://www.medicaid.gov/federal-policy-guidance/downloads/faq-09-24-2014.pdf
Chasson, G. S., Harris, G. E., & Neely, W. J. (2007). Cost comparison of early intensive behavioral intervention and special education for children with autism. Journal of Child and Family Studies, 16(3), 401–413. https://doi.org/10.1007/s10826-006-9094-1.
Cohen, H., Amerine-Dickens, M., & Smith, T. (2006). Early intensive behavioral treatment: Replication of the UCLA model in a community setting. Journal of Developmental and Behavioral Pediatrics, 27(2), S145–S155.
Daniels, A. M., & Mandell, D. S. (2014). Explaining differences in age at autism spectrum disorder diagnosis: A critical review. Autism, 18(5), 583–597. https://doi.org/10.1177/1362361313480277.
Diez, R. (2002). A glossary for multilevel analysis. Journal of Epidemiology and Community Health, 56(8), 588.
Douglas, M. D., Benevides, T. W., & Carretta, H. (2017). Analyzing state autism private insurance mandates for allied health services: A pilot study. OTJR Occupation, Participation and Health, 37(4), 218–226.
Granpeesheh, D., Dixon, D. R., Tarbox, J., Kaplan, A. M., & Wilke, A. E. (2009). The effects of age and treatment intensity on behavioral intervention outcomes for children with autism spectrum disorders. Research in Autism Spectrum Disorders, 3(4), 1014–1022. https://doi.org/10.1016/j.rasd.2009.06.007.
Green, V. A., Pituch, K. A., Itchon, J., Choi, A., O’Reilly, M., & Sigafoos, J. (2006). Internet survey of treatments used by parents of children with autism. Research in Developmental Disabilities, 27(1), 70–84. https://doi.org/10.1016/j.ridd.2004.12.002.
Grindle, C. F., Kovshoff, H., Hastings, R. P., & Remington, B. (2008). Parents’ experiences of home-based applied behavior analysis programs for young children with autism. Journal of Autism and Developmental Disorders, 39(1), 42–56. https://doi.org/10.1007/s10803-008-0597-z.
Howlin, P., Magiati, I., & Charman, T. (2009). Systematic review of early intensive behavioral interventions for children with autism. American Journal on Intellectual and Developmental Disabilities, 114(1), 23–41. https://doi.org/10.1352/2009.114:23-41.
Interagency Autism Coordinating Committee (IACC). (2017). 2016–2017 Interagency Autism Coordinating Committee Strategic Plan For Autism Spectrum Disorder. U.S. Department of Health and Human Services Interagency Autism Coordinating Committee. Retrieved from https://iacc.hhs.gov/publications/strategic-plan/2017/
Irvin, D. W., McBee, M., Boyd, B. A., Hume, K., & Odom, S. L. (2012). Child and family factors associated with the use of services for preschoolers with autism spectrum disorder. Research in Autism Spectrum Disorders, 6(1), 565–572. https://doi.org/10.1016/j.rasd.2011.07.018.
Jacobson, J. W., Mulick, J. A., & Green, G. (1998). Cost–benefit estimates for early intensive behavioral intervention for young children with autism—general model and single state case. Behavioral Interventions, 13(4), 201–226.
Jung, T., & Wickrama, K. A. S. (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317. https://doi.org/10.1111/j.1751-9004.2007.00054.x.
L & M Policy Research, LLC. (2014). Autism spectrum disorders: State of the states of services and supports for people with ASD (No. HHSM-500-2006-00009I/HHSM-500-T0002). Washington, DC: Centers for Medicare and Medicaid Services. Retrieved from http://www.medicaid.gov/medicaid-chip-program-information/by-topics/long-term-services-and-supports/downloads/asd-state-of-the-states-report.pdf
Leventhal, T., & Brooks-Gunn, J. (2003). Children and youth in neighborhood contexts. Current Directions in Psychological Service, 12(1), 27–31.
Linstead, E., Dixon, D. R., French, R., Granpeesheh, D., Adams, H., German, R., et al. (2017). Intensity and learning outcomes in the treatment of children with autism spectrum disorder. Behavior Modification, 41(2), 229–252. https://doi.org/10.1177/0145445516667059.
Magaña, S., Lopez, K., Aguinaga, A., & Morton, H. (2013). Access to diagnosis and treatment services among Latino children with autism spectrum disorders. Intellectual and Developmental Disabilities, 51(3), 141–153. https://doi.org/10.1352/1934-9556-51.3.141.
Maglione, M. A., Kadiyala, S., Kress, A. M., Hastings, J. L., & O’Hanlon, C. E. (2016). TRICARE Applied Behavior Analysis (ABA) Benefit: Comparison with Medicaid and Commercial Benefits. Santa Monica, CA: RAND Corporation. Retrieved from https://www.rand.org/pubs/research_reports/RR1334.html
Makrygianni, M. K., & Reed, P. (2010). A meta-analytic review of the effectiveness of behavioural early intervention programs for children with Autistic Spectrum Disorders. Research in Autism Spectrum Disorders, 4(4), 577–593. https://doi.org/10.1016/j.rasd.2010.01.014.
Murphy, M. A., & Ruble, L. A. (2012). A comparative study of rurality and urbanicity on access to and satisfaction with services for children with autism spectrum disorders. Rural Special Education Quarterly, 31(3), 3–11.
Parish, S., Magaña, S., Rose, R., Timberlake, M., & Swaine, J. G. (2012). Health care of Latino children with autism and other developmental disabilities: Quality of provider interaction mediates utilization. American Journal on Intellectual and Developmental Disabilities, 117(4), 304–315. https://doi.org/10.1352/1944-7558-117.4.304.
Peters-Scheffer, N., Didden, R., Korzilius, H., & Sturmey, P. (2011). A meta-analytic study on the effectiveness of comprehensive ABA-based early intervention programs for children with autism spectrum disorders. Research in Autism Spectrum Disorders, 5(1), 60–69. https://doi.org/10.1016/j.rasd.2010.03.011.
Reed, P., & Osborne, L. (2012). Impact of severity of autism and intervention time-input on child outcomes: Comparison across several early interventions. British Journal of Special Education, 39(3), 130–136. https://doi.org/10.1111/j.1467-8578.2012.00549.x.
Reichow, B., Barton, E., Boyd, B., & Hume, K. (2014). Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD): A systematic review. Campbell Systematic Reviews. Retrieved from http://www.campbellcollaboration.org/lib/project/338/
Reichow, B., & Wolery, M. (2008). Comprehensive synthesis of early intensive behavioral interventions for young children with Autism based on the UCLA Young Autism Project Model. Journal of Autism and Developmental Disorders, 39(1), 23–41. https://doi.org/10.1007/s10803-008-0596-0.
Rotholz, D. A., Kinsman, A. K., Lacy, K. K., & Charles, J. (2017). Improving early identification and intervention for children at risk for autism spectrum disorder. Pediatrics, 139(2), e20161061.
Shattuck, P., Grosse, S., Parish, S., & Bier, D. (2009). Utilization of a Medicaid-funded intervention for children with autism. Psychiatric Services, 60(4), 549–552. https://doi.org/10.1176/appi.ps.60.4.549.
Siller, M., Reyes, N., Hotez, E., Hutman, T., & Sigman, M. (2014). Longitudinal change in the use of services in autism spectrum disorder: Understanding the role of child characteristics, family demographics, and parent cognitions. Autism, 18(4), 433–446.
South Carolina Department of Disabilities and Special Needs. (2012). PDD Parent Handbook. Retrieved from http://www.ddsn.sc.gov/consumers/Documents/PDD%20Parent%20Handbook%20CS6.pdf
South Carolina Department of Disabilities and Special Needs. (2014). Pervasive Developmental Disorder Program. Retrieved from http://www.ddsn.sc.gov/about/recentnews/Documents/PDD%20Program%20Report.pdf
The Individuals with Disabilities Education Act, Reauthorization 2004, Pub. L. No. PL 108–446 (2004). Retrieved from http://www.copyright.gov/legislation/pl108-446.pdf
Thomas, K. C., Morrissey, J. P., & McLaurin, C. (2006). Use of autism-related services by families and children. Journal of Autism and Developmental Disorders, 37(5), 818–829.
Thomas, K. C., Parish, S. L., Rose, R. A., & Kilany, M. (2011). Access to care for children with autism in the context of state Medicaid reimbursement. Maternal and Child Health Journal, 16(8), 1636–1644. https://doi.org/10.1007/s10995-011-0862-1.
United States Department of Agriculture. (2016). Rural-Urban Commuting Area Codes. Retrieved from https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
Virués-Ortega, J. (2010). Applied behavior analytic intervention for autism in early childhood: Meta-analysis, meta-regression and dose–response meta-analysis of multiple outcomes. Clinical Psychology Review, 30(4), 387–399. https://doi.org/10.1016/j.cpr.2010.01.008.
Yingling, M. E., Bell, B. A., & Hock, R. M. (2019). Treatment utilization trajectories among children with autism spectrum disorder: Differences by race-ethnicity and neighborhood. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-019-03896-3.
Yingling, M. E., Hock, R. M., & Bell, B. A. (2017a). Time-lag between diagnosis of autism spectrum disorder and onset of publicly-funded early intensive behavioral intervention: Do race-ethnicity and neighborhood matter? Journal of Autism and Developmental Disorders, 48, 561.
Yingling, M. E., Hock, R. M., Cohen, A., & McCaslin, E. (2017b). Parent perceived challenges to treatment utilization in a publicly funded early intensive behavioral intervention program for children with Autism Spectrum Disorder. International Journal of Developmental Disabilities, 25, 525. https://doi.org/10.1080/20473869.2017.1324352.
Zuckerman, K., Friedman, N. D., Chavez, A. E., Shui, A. M., & Kuhlthau, K. A. (2017a). Parent-reported severity and health/educational services use among US children with autism: Results from a national survey. Journal of Developmental and Behavioral Pediatrics, 38(4), 260–268.
Zuckerman, K. E., Lindly, O. J., Reyes, N. M., Chavez, A. E., Macias, K., Smith, K. N., et al. (2017b). Disparities in diagnosis and treatment of autism in Latino and non-Latino white families. Pediatrics, 139(5), e20163010. https://doi.org/10.1542/peds.2016-3010.
Zuckerman, K. E., Lindly, O. J., Sinche, B. K., & Nicolaidis, C. (2015). Parent health beliefs, social determinants of health, and child health services utilization among US school-age children with autism. Journal of Developmental and Behavioral Pediatrics, 36(3), 146–157. https://doi.org/10.1097/DBP.0000000000000136.
Acknowledgments
We acknowledge the South Carolina Department of Disabilities and Special Needs for its support of this work. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the South Carolina Department of Disabilities and Special Needs.
Author Contributions
MY conceived of the study, led its design and coordination, conducted analyses, and drafted the manuscript; BB contributed to conceptualization and interpretation of analyses and provided feedback on manuscript drafts. Both authors read and approved the final manuscript.
Funding
This study was funded in part by a Clemson University Project Completion Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declared that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yingling, M.E., Bell, B.A. Underutilization of Early Intensive Behavioral Intervention Among 3-Year-Old Children with Autism Spectrum Disorder. J Autism Dev Disord 49, 2956–2964 (2019). https://doi.org/10.1007/s10803-019-04005-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-019-04005-0