Abstract
We estimated the prevalence of ASD in a population-based sample comprising children aged 3–12 years (N = 74,252) in Shanghai. This included a high-risk group sampled from special education schools and a low-risk group randomly sampled from general schools. First, we asked parents and then teachers to complete the Social Communication Questionnaire for participating children. Children who screened positive based on both parental and teachers’ reports were comprehensively assessed. ASD was identified based on DSM-5 criteria. We identified 711 children as being at-risk for ASD, of which 203 were identified as ASD cases. The prevalence of ASD was 8.3 per 10,000, which is likely an underestimate, given that 81.6% of the children diagnosed with ASD had IQs below 40. This is the first report on the prevalence of ASD according to DSM-5 in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, the prevalence of ASD has been reported to be increasing, especially in the past two decades (Keyes et al. 2012; Hertz-Picciotto and Delwiche 2009; Elsabbagh et al. 2012). The median worldwide prevalence of autism is currently about 1.0% (Elsabbagh et al. 2012; Lai et al. 2014). This rapid increase has provoked scientific scrutiny and public anxiety. The increase might be attributable to several factors, including the use of different screening tools (Hedley et al. 2015; Rice et al. 2012), changes in epidemiological screening methods and diagnostic criteria (Hansen et al. 2015; Wheeler et al. 2015), and increased public awareness. It is also possible that the number of individuals afflicted with ASD is actually increasing. According to several Chinese epidemiological studies (Sun et al. 2013), the pooled prevalence of childhood autism in mainland China was 11.8 per 10,000 children (95% confidence interval [CI] 8.2/10,000, 15.3/10,000). Few studies have addressed the prevalence of childhood autism in Hong Kong and Taiwan. A systematic review of the prevalence of ASD in mainland China, Hong Kong, and Taiwan revealed the prevalence of childhood autism in these areas was 26.6 per 10,000 children (Sun et al. 2013). The increase in ASD prevalence is commonly attributed to changing diagnostic criteria for ASD (Hansen et al. 2015). The latest manual for clinical diagnostic criteria (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; DSM-5) was published in May, 2013.
ASD is a disorder that can restrict a range of social activities and interests. Urbanicity is associated with ASD; Lauritsen et al. (2014) found a dose–response association with greater level of urbanicity and increased risk of ASD in children who moved to a higher level of urbanicity after birth. While the global burden of autism is currently unknown, in the US and UK, the annual social burden of ASD exceeds several billion US dollars (Knapp et al. 2009; Ganz 2007). Individuals with ASD place a heavy demand on educational, social, and medical services. Accurate prevalence estimates are essential for planning such services. Shanghai is a metropolitan city that differs from the rest of China. Therefore, a program to prevent and control ASD was supported by the Shanghai Municipal Enhancing Public Health 3-year Action Program of Shanghai Municipal Health and Family Planning Commission. This cross-sectional study aimed to estimate the prevalence of ASD among children aged 3–12 years in kindergartens and primary schools in Shanghai, China.
Methods
This study was approved by the Institutional Review Board of Shanghai Municipal Commission of Health and Family Planning.
Study Population and Sampling
We used multi-stage stratified cluster sampling to assess children aged 3–12 years in kindergartens and primary schools from the general population of Shanghai. There are eight urban districts in the central area, and nine suburban districts in suburban areas according to the geographical and social population distribution in Shanghai. Children living in urban and suburban districts were defined as urban and suburban residents, respectively. The sampling method has been described in our previous publication (Chen et al. 2016). Briefly, according to the sixth Chinese national census conducted in 2010, there were about 1.05 million children aged 3–12 years in Shanghai. First, we randomly sampled three of the eight urban districts (Jing’an, Xuhui, and Yangpu) and four of the nine suburban districts (Minghang, Pudong, Fenxian, and Chongming) in Shanghai. We investigated all children aged 3–12 years attending special education schools in the selected districts, as this population is generally considered to be at high-risk for ASD. Chinese special educational schools include children with language, hearing, limb, or cognitive disabilities. There is at least one special school in each district in Shanghai, all of which are public. we proportionally sampled children attending general education schools, (excluding those in special education or schools for hearing impaired-mute children) according to the number of children aged 3–12 years in each selected district. This means we randomly sampled a specific number of kindergartens and primary schools from the complete school list, regarding each school as a sampling unit.
Case Identification
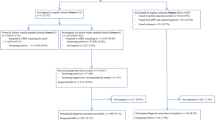
In this study, ASD cases were identified using a three-stage investigation (Fig. 1). Non-response was defined as distributed questionnaires that were not returned and questionnaires with more than 30% missing questions. We did not impute missing data as the sample size was sufficient. In stage 1 (June 2014), we systematically screened the entire sample. All of the children’s parents were asked to complete the Social and Communication Questionnaire (SCQ). This instrument has been standardized in Chinese (Gau et al. 2011; Berument et al. 1999). We entered data in July and August, 2014. The SCQ was developed by Rutter and Lord (Mulligan et al. 2009), and has 40 yes/no questions. It was derived from the Autism Diagnostic Interview-Revised, and developed as a screening tool for children with a high risk for developmental problems. The SCQ is an operational screening tool that is based on behavioral item scores in three functional categories: reciprocal social interaction, language and communication, and repetitive and stereotyped patterns of behavior. A study by Berument and Rutter (Berument et al. 1999) identified the optimum cut-off score for the SCQ as 15. We asked all parents of the sampled children to complete the SCQ.
ASD case identification process and adjusted prevalence process. ASD cases were identified using a three-stage investigation. In stage 1, we systematically screened the entire sample using the Social and Communication Questionnaire (SCQ) completed by parents; In stage 2, filled with the SCQ then completed by teachers for screen-positive children. In stage 3, screen-positive children were further evaluated and identified as having ASD if they met the relevant DSM-5 criteria
In stage 2 (September 2014), the teachers of children who screened positive by their parents were asked to complete the SCQ (current version) (Schanding et al. 2012). We considered children to be at high-risk of ASD if screening by both parents and teachers was positive. From the children with parents-screen positive and teacher-screen negative, we randomly selected 3196 from two of seven districts (one urban and one suburban district). These children were interviewed by a professional developmental and behavioral pediatrician, and we determined the false negative rate.
In stage 3 (October 2014), children who screened positive were referred to the Department of Development and Behavior of Shanghai Children’s Medical Center. All referred children underwent further evaluation and cognitive tests including developmental evaluation: the GESELL test for those aged 3–4 years, the Wechsler Preschool and Primary Scale of Intelligence (WPPSI) test for those aged 4–6 years, and the Wechsler Intelligence Scale for Children-Revised (WISC-R) for children aged 6–12 years. Children and their parents were simultaneously interviewed using the DSM-5 checklist by at least two experienced developmental and behavioral pediatricians independently. The children’s history with regard to pregnancy, birth, growth, and development was obtained. Next, we checked the consistency between the two pediatricians; if disagreement occurred, a third experienced pediatrician was involved and all pediatricians discussed the case until consensus was reached. Extensive efforts were made to contact the parents of children who screened positive and obtain consent for diagnostic evaluations. Children whose parents did not provide consent were classified as nonparticipants. Children were identified as having ASD if they met the appropriate DSM-5 criteria. The final diagnosis was made based on comprehensive clinical judgments; the clinician observed and evaluated children using the test of development and behavior. ASD cases had to meet DSM-5 criteria.
Quality Assurance
In the first stage, all schools followed the same quality assurance standards. For example, data for each child were encoded using the same rules, and all children were screened anonymously. A random selection of 10.0% questionnaire data was re-entered, with 96.1% agreement. In the second stage, which included a review of all screen-positive children, the agreement between two developmental and behavioral pediatricians was 97.8% based on a blinded independent assessment of the same information. Participants were asked to reply “Yes” or “No” to each question. Questionnaires with fewer missing answers (< 30%) were entered and total scores were calculated. In these cases, a total score of more than 15 was considered positive.
Statistical Analysis
All analyses were conducted using SPSS version 22.0 (SPSS Corporation, Chicago, USA). All statistics, such as proportions, percentages, and means were target population estimates calculated by two-steps of inverse probability weighting to take into account selective attrition in multistage sampling and SCQ screening strata, as well as differential responses to the SCQ associated with district, local residence, and sex (Baird et al. 2006). The inverse probability weighting was implemented by Stata 13.0 (Stata Corporation, College Station, TX, USA). We used Chi square tests to assess the association between categorical variables. A p value < 0.05 was considered statistically significant. In this study, all children from special education schools were surveyed, whereas those from general schools were randomly sampled from the entire population. Therefore, we estimated the prevalence of ASD among children aged 3–12 years in kindergartens and primary schools using several procedures.
First, we counted ASD cases (N) among all general schools in seven districts according to the ratio of the number of ASD children who attended general schools (N1) and the total number of children selected from general schools (N2). The calculation formula was:
N′ is the total number of children in general schools in seven districts.
Next, we calculated the prevalence of ASD among children aged 3–12 years in kindergartens and primary schools in the seven studied districts: we used the total number of ASD cases in general schools plus the number of cases in special educational schools as the numerator, and the total number of children in general schools plus those in special education schools as the denominator. We estimated the 95% CI using the formula:
We considered the putative effects of imprecise estimates in that the SCQ did not have a 100% response rate, sensitivity, and specificity in this multistage survey. We adjusted the prevalence with reference to the study by Pantelis and Kennedy (Pantelis and Kennedy 2016). The prevalence of ASD in boys and girls, urban and suburban areas, and in different age groups was calculated using the same method.
Results
In total, 81,282 (of 84,934) parents responded to our study, giving a response rate of 95.7%. We excluded invalid questionnaires, such as those with an age outside the target 3–12 range (n = 234) and those with more than 30% of information missing (n = 1750). There were 212 (0.28%) participants with more than 30% missing data and 5046 participants (6.2%) whose answers were inconsistent. Inconsistent responders responded “No” to the first question: “Is she/he now able to talk using short phrases or sentences?, but did not follow the skip pattern to go to question 8. Despite answering “No” to the first item they answered “Yes” to items 2–7, questions about talking in phrases or sentences. These participants may not have read carefully or fully understood the questions on the SCQ. Alternatively, they may not have understood the time frame for these questions, which would have impacted parents of older children. Therefore, 74,252 children aged 3–12 years were included in our analysis; 734 children (85.4% response rate) from special education schools and 73,487 children (87.4% response rate) from general kindergartens and primary schools. The flow of participants through the study is described in Fig. 1.
The sex, age group, registration, and district distribution of the sampled children are summarized in Table 1. Among the 734 children from special educational schools, 472 (64.7%) were boys and 258 (35.3%) were girls. Additionally, 540 (78.4%) of these children were local residents, 149 (21.6%) were migrants; 173 (23.6%) attended school in an urban area and 561 (76.4%) attended school in a suburban area. Among the 73,487 children from general education kindergartens and primary schools, 38,560 were boys (53.1%) and 33,989 were girls (46.9%). Additionally, 44,566 children (63.4%) were local residents and 25,734 (36.5%) were migrants.
The sex, age group, registration, school, and district distribution of the children whoscreened positive by both parents and teachers are summarized in Table 2. For the 74,252 children whose parents completed the SCQ, 4121 children (309 from special education schools and 3811 from general schools) scored ≥ 15 in the parent-rated screen, which was considered positive. Analysis of the teacher-completed SCQ for these 4121 children showed that 711 scored ≥ 15, and were considered to have a high risk of ASD (SCQ screen positive by both parents and teachers); the mean SCQ score from parents was 18.62 and from teachers was 20.13. For 3196 children with parents-screen positive and teacher-screen negative in 7 sampled districts, we randomly selected 677 children from two of seven districts (58 in Jin’an urban district and 619 in Minghang suburban district). These children were interviewed by two professional developmental and behavioral pediatricians, who identified two ASD cases, the false negative rate was 1.2/10,000.
Of the 84,075 participants from general schools, 3811 children were screened positive by their parents (positive rate 5.2%), whereas 309 of the 734 participants from special education schools were screened positive by parents (positive rate 42.1%). Teachers screened 506 of 3613 children from general schools (positive rate 14%), and 205 of 294 children in special education schools (positive rate 69.7%) as positive (Fig. 1). Of these, 663 (93.2%) children underwent diagnostic evaluation, and 203 were confirmed to have ASD: 163 children (80.3%) from special education schools, 29 (14.3%) from general kindergartens, and 11 (5.4%) from general primary schools. Among these 203 children, 20 were evaluated with the WPPSI and 127 were evaluated by WISC-R. The results showed that 120 (81.6%) children had an intelligence quotient (IQ) below 40, 16 (10.9%) from 40 to 70, and 11 (7.5%) equal to or greater than 70. Another 56 children could not perform the IQ evaluation because of language impairment or uncontrollable behaviors.
Twenty-nine of the 29,986 children who were randomly selected from 234,413 children in general kindergartens in the seven studied districts were identified as having ASD. Therefore, we estimated there were 227 children with ASD in all general kindergartens in the seven districts. Similarly, we estimated there were 87 children with ASD from all general primary schools in the seven districts, meaning the total estimated number of children with ASD in general and special education schools in the seven districts was 477. This gave a prevalence of ASD among children aged 3–12 years in kindergartens and primary schools in Shanghai of 8.3 per 10,000 children (95% CI 6.2/10,000, 10.4/10,000). Given a false negative rate of 1.2/10,000, the integrated prevalence was 9.5/10,000 and the adjusted prevalence was 7.58/10,000 (95% CI 6.87/10,000, 8.29/10,000). The process of detailed adjusted prevalence calculation is shown in Fig. 1; 5.4 per 10,000 children (95% CI 4.8/10,000, 6.0/10,000) in the general-population and 2.23% (95% CI 19.3/10,000, 25.3/10,000) in the high-probability population. The prevalence in boys (12.7 per 10,000, 95% CI 11.4/10,000, 14.0/10,000) was significantly higher than in girls (3.5 per 10,000, 95% CI 2.8/10,000, 4.2/10,000), with a male to female ratio of 3.6:1. The prevalence in urban and suburban areas was 9.4/10,000 (95% CI 4.6/10,000, 14.2/10,000) and 7.9/10,000 (95% CI 5.6/10,000, 10.2/10,000), respectively. Table 3 shows the prevalence of ASD in special education and general schools, urban and suburban areas, and in different age groups. According to the inverse probability weighting method, delivering a boy increased the average prevalence of ASD by a statistically significant 0.124%, a Shanghai local birth increased the average prevalence of ASD by a statistically significant 0.12%, and urbanity increased the average prevalence of ASD by 0.12%.
Discussion
Prevalence Difference and Possible Reasons
Among Chinese children aged 3–12 years in kindergartens and primary schools in Shanghai, the prevalence of ASD was 8.3/10,000 (95% CI 6.2/10,000, 10.4/10,000), the adjusted prevalence was 7.58/10,000 (95% CI 6.87/10,000, 8.29/10,000), and the male-to-female ratio was 3.6:1. Kindergarten and primary school attendance age correspond to 3–12 years in the Chinese education system, making it practical and relatively easy to organize the survey in this age range. Lord et al. reported that atypical autism is less stable until around age 3 years (Lord et al. 2006). Under Chinese education law, school attendance is free and compulsory for children aged 6–15 years. Almost all children go to kindergarten because primary school requires kindergarten experience; otherwise, new students cannot follow up the competing study in primary school in Shanghai. In our study, the prevalence of ASD in urban districts was higher than in suburban districts, which may indicate more awareness of or attention to the disorder, or that better/more readily accessible diagnostic and medical services are available in urban areas.
Our prevalence estimate was close to the pooled prevalence for childhood autism in mainland China (11.8 per 10,000, 95% CI 8.2/10,000, 15.3/10,000) (Sun et al. 2013), but lower than that reported in a recent study in Beijing (119 per 10,00, 95% CI 53/10,000, 265/10,000) (Sun et al. 2015). We structured our study with parents being the primary responders. Based on parents-screen positive results, the corresponding teachers completed the SCQ for those children and professional developmental and behavioral pediatricians identified ASD cases according to DSM-5 criteria. We screened children using parent-completed SCQ first because the SCQ has been well-validated as a parents-report screen in several studies among children aged 2–16 years (Allen et al. 2007; Corsello et al. 2007; Lee et al. 2007; Wiggins; et al. 2007; Chen et al. 2009; Eaves et al. 2006; Johnson et al. 2011). The sensitivity of the SCQ completed by parents (75.3%) was reported to be higher than that of the SCQ completed by teachers (60.0%) (Schanding et al. 2012). Teachers completed the SCQ for 4121 children with a parent-rated SCQ ≥ 15. Of these 4121 children, only 711 had a teacher reported SCQ ≥ 15; parents and teachers’ screen-positive rate was 5.2 and 14.0% for general schools, and 42.1 and 69.7% for special schools (Fig. 1). The screen-positive rate in special schools in present study was higher than in other studies (Barnard-Brak et al. 2016; Schanding et al. 2012). The reason for low agreement between parents and teachers may be diverse parental education levels that were lower than that of teachers, and some parents might not have fully understood the questionnaire. Most Chinese families only have one child, meaning they cannot compare children in the family; however, teachers have opportunity to observe and compare students in the same class. However, care must be taken in interpreting findings across studies because there are considerable differences in the methods used, sampling procures, and diagnostic criteria among studies from South Thames, UK (Baird et al. 2006); Cambridge, UK (Baron-Cohen et al. 2009); Goyang, South Korea (Kim et al. 2011); and Bergen, Norway (Posserud et al. 2010). These studies screened for ASD among a variety of populations including: children with special educational needs, children who were on a disability registry, children in elementary schools, and/or children who were receiving treatment from local clinicians. The prevalence of ASD of 1.81% reported in a study from Japan (Kawamura et al. 2008) was based on screening and advising parents to consult a doctor, with diagnosis based on clinical interviews with the parents and observation of the child. The prevalence of ASD estimated by the US Autism Developmental Disabilities Monitoring Network (Developmental Disabilities Monitoring Network Surveillance Year Principal Investigators Centers for Disease Control Prevention, Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2010, 2014; Christensen et al. 2016a, b), was calculated based on a systematic retrospective review of 8-year-old children, in which records from regions in 11 states were examined. Therefore, the potential effect of differing methodologies on prevalence estimations should not be overlooked when comparing the results of different studies. Most studies on ASD have been conducted in Western countries, and the prevalence of ASD in China is uncertain. Although all children were screened anonymously during our study, it is possible that some parents, fearing a diagnosis, chose not to objectively report ASD symptoms or not to participate in diagnostic evaluations. This might have resulted in an underestimation of the prevalence of ASD, because further investigation was based on parent-rated screening. Parental lack of awareness about ASD and failure to recognize symptoms is also likely to be a factor, especially in cases of children who suffered from a mild form of the disorder. Since we didn’t adjust for missing values in computer, the total score for questionnaires with fewer missing answers (< 30%), it may have contributed to missing some true positive cases. According to the results of IQ tests, more than 80% of the children had an IQ below 40 (low functioning). This differs from recent prevalence studies in Western countries, and was considered as a reason for the difference in prevalence between our study and other prevalence research. A reason for this may be that the SCQ is not sufficiently sensitive to detect high functioning (cognitively-able) cases; although a few questions in the scale may capture these cases, they would not be sufficient to achieve a cut-off score of 15. However, we are not clear about how strong the impact of this was on data in our research.
Preliminary studies have reported significant differences in diagnostic yield using the DSM-IV and new DSM-5 criteria. Frazier and colleagues (Frazier et al. 2012) evaluated the validity of DSM-5 criteria with respect to ASD by analyzing the symptoms of 14,744 siblings (8911 ASD and 5863 controls) enrolled in a national registry. They concluded that the increased specificity of the DSM-5 relative to the DSM IV may reduce the rate of false positive ASD diagnoses. Another study (Yang and Pan 2013) also reported that the DSM-5 diagnostic criteria are stricter than those in the DSM-IV, and stated that patients with autism diagnosed using DMS-5 criteria tend to be more severely affected. According to a systematic review and meta-analysis (Kulage et al. 2014), the DSM-5 will likely decrease the number of individuals diagnosed with ASD by 31%, particularly those in the PDD-NOS subgroup. Based on these previous studies, it is possible that high-functioning cases identified as having ASD according to the DSM-IV may not be diagnosed with ASD according to DSM-5 criteria. The prevalence of ASD in the Chinese population and Han race differed from Western countries, and the reasons detailed above might have contributed to the lower prevalence of ASD in the present study.
Strengths and Limitations
To our knowledge, this is the first population-based prevalence study of ASD under the DSM-5 diagnostic criteria in China. We designed several characteristics of the present study with the intention of overcoming the limitations of previous research, and aimed to provide the most accurate prevalence estimate for ASD in China. First, the sample size was sufficient to provide high precision; ours was the largest epidemiological study of ASD using an active case ascertainment design. Second, the children in our sample were older than 3 years, which is the age at which ASD symptoms usually become obvious or have caused significant functional impairment. Third, prospective identification, rather than use of retrospective case-review procedures, has been shown to contribute to prevalence estimation. Additionally, we screened all children in special educational schools, thus ensuring a low percentage of possible missed cases of ASD. Fourth, we used a careful diagnostic procedure. Ascertainment by screening was followed by a diagnostic assessment, with the goal of reaching a best-estimate clinical consensus regarding the diagnosis based on combined parent report information, information from school teachers, and direct observation of the child.
A limitation of this study was that we only obtained information from teachers about children who were screened positive by their parents. For practical reasons, no random selection was added from children for whom the SCQ had been completed first by teachers, or completed by both parents and teachers simultaneously. What’s more, a cut-off score of SCQ less than 15 may be preferable. In addition, follow-up of the ASD cohort is essential. We will consider these points in our future study. Therefore, it is possible that we missed cases among parental screen-negative children, which might have resulted in an underestimation of the prevalence; however, we randomly selected two districts for 3196 parents-screen positive and teacher-screen negative children, and found the false negative rate was 1.2/10,000. Additionally, to clinically confirm the diagnosis of ASD, all participating developmental and behavioral pediatricians used the DSM-5; however, the detection of ASD may vary in different areas in terms of behavioral functioning during social interactions, communication, and activities, which may not be fully captured by the DSM-5. Specific scales such as the Autism Diagnostic Observation Schedule (ADOS) and the Autism Diagnostic Interview-Revised (ADI-R) may provide key information to confirm the presence of ASD. However, these scales are not widely available in mainland China and are time consuming. Therefore, we did not use the ADOS or ADI-R in the present large-scale cross-sectional study. We will use the ADOS to confirm some ASD cases for future research.
Conclusions and Implications
ASD is a lifelong developmental disability that has become an important public issue in China. A sufficient number of qualified pediatricians and child psychiatrists, efficacious screening tools, and diagnostic scales consistent with international measurements are urgently needed to identify patients with ASD. As individuals with ASD place a heavy demand on educational, social, and medical services, our estimation of the health burden is essential and will help inform decisions on public health policy. Specific rehabilitation facilities should be established as soon as possible to provide services for children with ASD.
References
Allen, C. W., Silove, N., Williams, K., & Hutchins, P. (2007). Validity of the social communication questionnaire in assessing risk of autism in preschool children with developmental problems. Journal of Autism and Developmental Disorders, 37(7), 1272–1278. https://doi.org/10.1007/s10803-006-0279-7.
Baird, G., Simonoff, E., Pickles, A., Chandler, S., Loucas, T., Meldrum, D., et al. (2006). Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: The special needs and autism project (SNAP). The Lancet, 368(9531), 210–215. https://doi.org/10.1016/S0140-6736(06)69041-7.
Barnard-Brak, L., Brewer, A., Chesnut, S., Richman, D., & Schaeffer, A. M. (2016). The sensitivity and specificity of the social communication questionnaire for autism spectrum with respect to age. Autism Research, 9(8), 838–845. https://doi.org/10.1002/aur.1584.
Baron-Cohen, S., Scott, F. J., Allison, C., Williams, J., Bolton, P., Matthews, F. E., et al. (2009). Prevalence of autism-spectrum conditions: UK school-based population study. British Journal of Psychiatry the Journal of Mental Science, 194(6), 500–509.
Berument, S. K., Rutter, M., Lord, C., Pickles, A., & Bailey, A. (1999). Autism screening questionnaire: Diagnostic validity. British Journal of Psychiatry, 175, 444–451.
Chen, C., Jin, Z., Yang, Y., Jiang, F., Jin, X., Huang, H., et al. (2016). Prevalence of grade 1, 2, 3 thinness is associated with lower socioeconomic status in children in Shanghai, China. Public Health Nutrition, 19(11), 2002–2010. https://doi.org/10.1017/S1368980016000045
Chen, Y. H., Rodgers, J., & McConachie, H. (2009). Restricted and repetitive behaviours, sensory processing and cognitive style in children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(4), 635–642. https://doi.org/10.1007/s10803-008-0663-6.
Christensen, D. L., Baio, J., Braun, K. V., Bilder, D., Charles, J., Constantino, J. N., et al. (2016a). Prevalence and characteristics of autism spectrum disorder among children aged 8 years: Autism and developmental disabilities monitoring network, 11 Sites, United States, 2012. MMWR Surveillance Summaries, 65(3), 1–23. https://doi.org/10.15585/mmwr.ss6503a1.
Christensen, D. L., Bilder, D. A., Zahorodny, W., Pettygrove, S., Durkin, M. S., Fitzgerald, R. T., et al. (2016b). Prevalence and characteristics of autism spectrum disorder among 4-year-old children in the autism and developmental disabilities monitoring network. Journal of Developmental and Behavioral Pediatrics, 37(1), 1–8. https://doi.org/10.1097/DBP.0000000000000235.
Corsello, C., Hus, V., Pickles, A., Risi, S., Cook, E. H. Jr., Leventhal, B. L., et al. (2007). Between a ROC and a hard place: Decision making and making decisions about using the SCQ. Journal of Child Psychology and Psychiatry, 48(9), 932–940. https://doi.org/10.1111/j.1469-7610.2007.01762.x.
Developmental Disabilities Monitoring Network Surveillance Year Principal Investigators Centers for Disease Control Prevention, Prevalence of autism spectrum disorder among children aged 8 years: Autism and developmental disabilities monitoring network, 11 sites, United States, 2010. (2014). MMWR Surveillance Summaries, 63(2), 1–21.
Eaves, L. C., Wingert, H., & Ho, H. H. (2006). Screening for autism: Agreement with diagnosis. Autism, 10(3), 229–242. https://doi.org/10.1177/1362361306063288.
Elsabbagh, M., Divan, G., Koh, Y. J., Kim, Y. S., Kauchali, S., Marcin, C., et al. (2012). Global prevalence of autism and other pervasive developmental disorders. Autism Research, 5(3), 160–179. https://doi.org/10.1002/aur.239.
Frazier, T. W., Youngstrom, E. A., Speer, L., Embacher, R., Law, P., Constantino, J., et al. (2012). Validation of proposed DSM-5 criteria for autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 51(1), 28–40.e23. https://doi.org/10.1016/j.jaac.2011.09.021.
Ganz, M. L. (2007). The lifetime distribution of the incremental societal costs of autism. Archives of Pediatrics and Adolescent Medicine, 161(4), 343–349.
Gau, S. S.-F., Lee, C.-M., Lai, M.-C., Chiu, Y.-N., Huang, Y.-F., Kao, J.-D., et al. (2011). Psychometric properties of the Chinese version of the Social Communication Questionnaire. Research in Autism Spectrum Disorders, 5(2), 809–818. https://doi.org/10.1016/j.rasd.2010.09.010.
Hansen, S. N., Schendel, D. E., & Parner, E. T. (2015). Explaining the increase in the prevalence of autism spectrum disorders: The proportion attributable to changes in reporting practices. JAMA Pediatrics, 169(1), 56–62. https://doi.org/10.1001/jamapediatrics.2014.1893.
Hedley, D., Nevill, R. E., Monroy-Moreno, Y., Fields, N., Wilkins, J., Butter, E., et al. (2015). Efficacy of the ADEC in identifying autism spectrum disorder in clinically referred Toddlers in the US. Journal of Autism and Developmental Disorders, 45(8), 2337–2348. https://doi.org/10.1007/s10803-015-2398-5.
Hertz-Picciotto, I., & Delwiche, L. (2009). The rise in autism and the role of age at diagnosis. Epidemiology, 20(1), 84–90. https://doi.org/10.1097/EDE.0b013e3181902d15.
Johnson, S., Hollis, C., Hennessy, E., Kochhar, P., Wolke, D., & Marlow, N. (2011). Screening for autism in preterm children: Diagnostic utility of the Social Communication Questionnaire. Archives of Disease in Childhood, 96(1), 73–77. https://doi.org/10.1136/adc.2010.194795.
Kawamura, Y., Takahashi, O., & Ishii, T. (2008). Reevaluating the incidence of pervasive developmental disorders: Impact of elevated rates of detection through implementation of an integrated system of screening in Toyota, Japan. Psychiatry and Clinical Neurosciences, 62(2), 152–159. https://doi.org/10.1111/j.1440-1819.2008.01748.x.
Keyes, K. M., Susser, E., Cheslack-Postava, K., Fountain, C., Liu, K., & Bearman, P. S. (2012). Cohort effects explain the increase in autism diagnosis among children born from 1992 to 2003 in California. International Journal of Epidemiology, 41(2), 495–503. https://doi.org/10.1093/ije/dyr193.
Kim, Y. S., Leventhal, B. L., Koh, Y. J., Fombonne, E., Laska, E., Lim, E. C., et al. (2011). Prevalence of autism spectrum disorders in a total population sample. American Journal of Psychiatry, 168(9), 904–912.
Knapp, M., Romeo, R., & Beecham, J. (2009). Economic cost of autism in the UK. Autism, 13(3), 317–336. https://doi.org/10.1177/1362361309104246.
Kulage, K. M., Smaldone, A. M., & Cohn, E. G. (2014). How will DSM-5 affect autism diagnosis? A systematic literature review and meta-analysis. Journal of Autism and Developmental Disorders, 44(8), 1918–1932.
Lai, M. C., Lombardo, M. V., & Baron-Cohen, S. (2014). Autism. Lancet, 383(9920), 896–910. https://doi.org/10.1016/s0140-6736(13)61539-1.
Lauritsen, M. B., Astrup, A., Pedersen, C. B., Obel, C., Schendel, D. E., Schieve, L., et al. (2014). Urbanicity and autism spectrum disorders. Journal of Autism and Developmental Disorders, 44(2), 394–404. https://doi.org/10.1007/s10803-013-1875-y.
Lee, L.-C., David, A. B., Rusyniak, J., Landa, R., & Newschaffer, C. J. (2007). Performance of the social communication questionnaire in children receiving preschool special education services. Research in Autism Spectrum Disorders, 1(2), 126–138. https://doi.org/10.1016/j.rasd.2006.08.004.
Lord, C., Risi, S., DiLavore, P. S., Shulman, C., Thurm, A., & Pickles, A. (2006). Autism from 2 to 9 years of age. Archives of General Psychiatry, 63(6), 694–701. https://doi.org/10.1001/archpsyc.63.6.694.
Mulligan, A., Richardson, T., Anney, R. J., & Gill, M. (2009). The Social Communication Questionnaire in a sample of the general population of school-going children. Irish Journal of Medical Science, 178(2), 193–199. https://doi.org/10.1007/s11845-008-0184-5.
Pantelis, P. C., & Kennedy, D. P. (2016). Estimation of the prevalence of autism spectrum disorder in South Korea, revisited. Autism, 20(5), 517–527. https://doi.org/10.1177/1362361315592378.
Posserud, M., Lundervold, A. J., Lie, S. A., & Gillberg, C. (2010). The prevalence of autism spectrum disorders: Impact of diagnostic instrument and non-response bias. Social Psychiatry and Psychiatric Epidemiology, 45(3), 319–327.
Rice, C. E., Rosanoff, M., Dawson, G., Durkin, M. S., Croen, L. A., Singer, A., et al. (2012). Evaluating Changes in the Prevalence of the Autism Spectrum Disorders (ASDs). Public Health Reviews, 34(2), 1–22.
Schanding, G. T. Jr., Nowell, K. P., & Goin-Kochel, R. P. (2012). Utility of the social communication questionnaire-current and social responsiveness scale as teacher-report screening tools for autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(8), 1705–1716. https://doi.org/10.1007/s10803-011-1412-9.
Sun, X., Allison, C., Matthews, F. E., Sharp, S. J., Auyeung, B., Baron-Cohen, S., et al. (2013). Prevalence of autism in mainland China, Hong Kong and Taiwan: A systematic review and meta-analysis. Molecular Autism, 4(1), 7. https://doi.org/10.1186/2040-2392-4-7.
Sun, X., Allison, C., Matthews, F. E., Zhang, Z., Auyeung, B., Baron-Cohen, S., et al. (2015). Exploring the underdiagnosis and prevalence of autism spectrum conditions in beijing. Autism Research, 8(3), 250–260. https://doi.org/10.1002/aur.1441.
Wheeler, A. C., Mussey, J., Villagomez, A., Bishop, E., Raspa, M., Edwards, A., et al. (2015). DSM-5 changes and the prevalence of parent-reported autism spectrum symptoms in Fragile X syndrome. Journal of Autism and Developmental Disorders, 45(3), 816–829. https://doi.org/10.1007/s10803-014-2246-z.
Wiggins;, L. D., Bakeman;, R., Adamson;, L. B., & Robins, D. L. (2007). The Utility of the Social Communication Questionnaire in Screening for Autism in Children Referred for Early Intervention. Focus on Autism and Other Developmental Disabilities, 22, 33–38.
Yang, Y., & Pan, C. (2013). Role of metabotropic glutamate receptor 7 in autism spectrum disorders: A pilot study. Life Sciences, 92(2), 149–153. https://doi.org/10.1016/j.lfs.2012.11.010.
Acknowledgments
We are grateful to all parents and teachers of the children for their assistance and cooperation in this study. We thank Liwen Bianji, Edanz Group China (http://www.liwenbianji.cn/ac), for editing the English text of this manuscript. This work was supported by the Shanghai Municipal Commission of Health and Family Planning: Shanghai Municipal Enhancing Public Health 3-Year Prevention and Control of ASD Program, 2011–2013 [Grant No. 11PH1951202], National Human Genetic Resources Sharing Service Platform [2005DKA21300], National Science and Technology Commission [2016YFC1305203], Project of Shanghai Children’s Health Service Capacity Construction[GDEK201708].
Author information
Authors and Affiliations
Contributions
JX, JZ and LS designed the study; JZ, HH, and YY performed the study; JZ and LS drafted the manuscript and performed statistical analyses; LS, JZ, HH and JX contributed to interpretation of the results and critically reviewed the manuscript; LS had primary responsibility for final content. All authors have read and approved the final manuscript.
Corresponding authors
Rights and permissions
About this article
Cite this article
Jin, Z., Yang, Y., Liu, S. et al. Prevalence of DSM-5 Autism Spectrum Disorder Among School-Based Children Aged 3–12 Years in Shanghai, China. J Autism Dev Disord 48, 2434–2443 (2018). https://doi.org/10.1007/s10803-018-3507-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-018-3507-z