Abstract
This study compared bone mineral density (BMD) of the spine obtained by dual-energy X-ray absorptiometry (DEXA), nutritional status, biochemical markers, and gastrointestinal (GI) symptoms in 4–8 year old boys with Autism Spectrum Disorder (ASD) with a group of age-matched, healthy boys without ASD. Boys with ASD had significantly lower spine BMD compared to controls but this was not correlated with any biochemical markers, dietary intake of calcium and vitamin D, elimination diet status, or GI symptomology. Reduced BMD in 4–8 year old boys with ASD appears to involve factors other than nutrient intake and GI status, and requires further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication and social interaction, and restricted, repetitive patterns of behavior, interests or activities (American Psychiatric Association. 2013). Children with ASD are at greater risk of gastrointestinal (GI) disorders and associated symptoms (abdominal pain, constipation, diarrhea and gastroesophageal reflux), than are their typically developing peers (Buie et al. 2010a, 2010b; Valicenti-McDermott et al. 2006; Black et al. 2002; Schieve et al. 2012). While there is limited data on the impact of GI symptoms on bone health in children with ASD (Hediger et al. 2008; Neumeyer et al. 2013; Roke et al. 2012; Ekhlaspour et al. 2016), decreased bone mineral density (BMD) in children with inflammatory bowel disease, but no developmental concerns, is well established (reviewed by (Thangarajah et al. 2015)).
Severe GI symptoms in children compromise dietary intake and cause nutritional depletion (Hartman et al. 2009). Inadequate intake due to dietary preference, anorexia or dysphagia, dietary restrictions, nutrient malabsorption, increased intestinal losses, and an increase in nutritional demand that accompanies many catabolic states can all contribute to this loss of nutrients (Mahan and Escott-Stump 2008; Porter and Kaplan 2011). A compromised nutritional status may negatively impact growth velocity and increases the risk of developing medical conditions secondary to the primary diagnosis of ASD. Children with ASD may therefore be at risk for suboptimal bone development (Roke et al. 2012). This may arise from low dietary calcium and vitamin D intake due to a restrictive diet (Schreck et al. 2004; Williams et al. 2000), the use of medications that may interfere with bone metabolism (Goodman et al. 2007), decreased or limited physical activity and exposure to sunlight (Macdonald et al. 2011), and activity restriction and/or motor disorders (Hediger et al. 2008).
In reviewing the literature, we found only one paper reporting on bone health in younger children (ages 4–8 years) with ASD. In this study, while bone cortical thickness (BCT) was found to increase with age, there was a progressive widening of the gap between the medians of BCT for boys with ASD and the reference (Hediger et al. 2008). The authors also reported that 12% of the boys on a casein-free diet had an overall larger deviation in BCT, to nearly twice that of boys on minimally restricted or unrestricted diets (Hediger et al. 2008). However, this study did not take into consideration nutrient intake for each child. For example, a child on a nutrient-dense, casein-free diet may receive more than adequate levels of calcium and vitamin D compared to a child receiving the standard American diet (Herndon et al. 2009). Hediger and colleagues also did not take into consideration GI problems in the children with ASD, which could cause nutrient malabsorption, regardless of nutritional intake.
More recently, Neumeyer and colleagues examined bone density in pre-pubertal boys. In this study, boys with ASD aged 8–14 years had lower BMD Z-scores at the spine, hip, and femoral neck, lower vitamin D intake from food and in serum, and lower levels of physical activity suggesting that, at least in this study population, BMD may be associated with impaired vitamin D status and lower exercise activity (Neumeyer et al. 2013). A study in adolescents and young adults with ASD also reported lower hip and femoral neck BMD Z-scores and lower spine, hip and femoral neck height adjusted BMD Z-scores in ASD participants compared to controls, but diet and physical activity were not examined (Ekhlaspour et al. 2016).
The objective of this study was to assess bone mineral density, nutritional status and GI symptomology in boys diagnosed with ASD in comparison to a control group of age-matched, healthy boys without ASD.
Method
Participants
A total of 84 boys (n = 42/group), primarily non-Hispanic (75%) ages 4–8 years with and without ASD were enrolled in the study. Three participants (one ASD and two controls) were removed from the study as they were not able to complete the DEXA scan. One additional ASD subject was removed following their diagnostic assessment (see section below). This analysis therefore represents 80 participants. For the ASD group, there were 40 participants with a mean age of 6.36 (95% CI: 5.96, 6.76) years. For the control group, there were 40 age-matched participants with a median age of 6.55 (95% CI: 6.05, 7.04) years. Participants were recruited by the use of informational flyers placed locally and/or social media. Some ASD participants were also recruited through an outpatient ASD clinic. The majority of subjects lived in Texas and below 37° latitude. Seven control participants had a sibling with ASD that also participated in the study. Parents or the legal guardians of each participant were given a brief verbal overview of the study prior to their study visit and the option to meet with a research assistant for more information. Exclusion criteria were as follows: a BMI < 3rd or >97th percentiles, diagnoses or procedures that may affect bone health, as well as certain genetic conditions, physical and/or psychiatric disorders that precluded participation in study procedures. These included: genetic disorders of metabolism; genetic disorders of bone formation; genetic disorders of the endocrine system causing or contributing to osteoporosis, osteofibrosis or hypermineralization; episodic (more than two rounds) or continual use of medications known to decrease bone mineral density (e.g. oral glucocorticoids, anti-seizure medications and prolactin-raising antipsychotics); children undergoing chelation therapy or having undergone chelation therapy within the previous 6 months; and children who were unable to remain still for the duration of the bone density scanning procedure. If the parent/guardian expressed interest in the study, the informed consent form was reviewed with them and consent obtained. Median (IQR) days for completing study procedures was 15 (7, 31) and 5 (4, 14) for ASD and control subjects, respectively.
Diagnostic Assessments
A diagnostic assessment was performed for each ASD participant, which included the Autism Diagnostic Observation Schedule (ADOS; Gotham et al. 2007) and Autism Diagnostic Interview—Revised (ADI-R; Rutter et al. 2003). Subsequent clinical diagnosis of each child was based on all the available data and determined by a licensed clinical psychologist with established research reliability on the ADOS and ADI-R, using DSM-IV criteria. Out of the remaining 41 participants in the ASD group, 29 were given a diagnosis of Autistic Disorder, 4 Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS), and 5 Asperger’s Disorder. Due to scheduling issues, we were unable to complete an ADI-R for two participants but their ADOS assessments indicated one classification of Autism Spectrum and one of Autism. These two participants were included in the analyses. One additional participant was unable to finish the ADOS assessment due to behavioral concerns. His ADI-R assessment indicated an Autism classification, although the diagnostician also noted that additional testing would be required in order to rule out bipolar disorder and oppositional defiant disorder as additional diagnoses. This subject was removed from the analysis resulting in 40 ASD participants.
A health history questionnaire was performed for all control participants to confirm that they were relatively healthy and there were no developmental concerns. In addition, all control participants underwent a developmental screening using the Adaptive Behavior System (ABAS-II), which was evaluated by a clinical diagnostician. Controls participants were excluded if their ABAS-II screening indicated any developmental concerns.
Biochemical Indices
Biomarkers for nutritional status such as albumin and hematocrit were collected for all participants during their office visit through a comprehensive metabolic panel and complete blood count. Serum vitamin D, ionized calcium, phosphorus, magnesium, intact parathyroid hormone and C-reactive protein (CRP) were also measured, as well as an erythrocyte sedimentation rate (ESR). Fasting blood samples for all participants were collected in office and sent to Clinical Pathology Laboratories, Inc. (CPL) to be analyzed using standard methods. If we were unable to obtain a blood sample in office, participants had the option of scheduling a blood draw at any CPL Patient Service Center. Magnesium and boron, important in the formation of osseous tissue (Schaafsma et al. 2001), were assessed by use of a red blood cell (RBC) Elements test (Doctor’s Data, Inc, St. Charles, IL). This test required each participant to withhold any supplemental minerals for 3 days prior to the fasting blood draw.
Nutritional Intake
All participants completed a three-day food diary. Standardized written instructions were provided to caregivers who recorded all food and beverage intake for two weekdays and one weekend day that they consider typical for their child just prior to their initial study visit. Measurement guidelines were provided to the caregivers to improve the accuracy of reported portion sizes. Caregivers were asked to provide homemade recipes, brand names of packaged products and restaurant information in the food diary. Any incomplete dietary record was verified via phone by a trained nutrition research assistant before proceeding further. Food records were analyzed using Food Processor SQL (version 10.3.0, 2008, ESHA, Salem, OR). Data for the 3 days were combined using the Multiple Source Method (Haubrock et al. 2011). Supplement data was not included in the nutrient analysis for an accurate assessment of dietary nutriture, but was used to ascertain total calcium and vitamin D intake from all sources. Estimated energy requirement for each participant was derived from height, weight, and a moderate physical activity level using the formulas developed by the Institute of Medicine (Institute of Medicine 2005). Activity level was assessed for all participants through several questions taken from a self-reported physical activity questionnaire (although the entire questionnaire was not administered). All study participants met our clinical assessment for moderate activity level, which by Dietary Reference Intakes definition is activities of daily living plus 30–60 min of additional movement/exercise three times/week.
Dietary Status
Out of the 40 ASD participants, 19 were on a gluten and casein free (GFCF) diet. Of these, 15 were under the care of a dietitian or nutritionist who monitored nutrient intake at the time of study participation, whereas 4 were reportedly on a GFCF diet but were not under the care of a professional at the time of study participation so compliance could not be substantiated. The remaining 21 boys with ASD did not report any dietary intervention. Out of the 40 control participants, 2 boys were following a GFCF diet; 1 was under the care of a professional and 1 was not. The remaining 38 controls did not report any dietary intervention.
Anthropometric Measurements
All participants underwent a physical exam conducted by a nurse practitioner or registered dietician during a scheduled office visit using a single scale and stadiometer. BMI was calculated as kg/m2. Height and weight were compared with the standards for linear growth derived from the Centers for Disease Control National Center for Health Statistics Growth Charts (Institute of Medicine 2005). Other anthropometrics collected included triceps skinfold (TSF) and mid-arm circumference (MAC), from which, a mid-arm muscle circumference (MAMC) was calculated as an indicator of protein and fat reserves.
Gastrointestinal Symptoms
Gastrointestinal (GI) symptoms were assessed using the Gastrointestinal Symptoms Rating Scale (GSRS; Svedlund et al. 1988), which consists of 15 items, each rated on a four point Likert scale, regarding five major GI domains: abdominal pain (abdominal pain, hunger pains and nausea); reflux syndrome (heartburn and acid regurgitation), indigestion syndrome (borborygmus, abdominal distension, eructation and increased flatus), diarrhea syndrome (diarrhea, loose stools and urgent need for defecation), and constipation syndrome (constipation, hard stools and feeling of incomplete evacuation). Scores are calculated by taking the mean of the items within an individual scale, with higher scores indicating greater severity of symptoms. The questionnaire is used in clinical trials with children (Lionetti et al. 2006; Thomson et al. 2004; Bausserman and Michail 2005) and has been tested for validity and reliability (Dimenas et al. 1996). For the GSRS, there were 40 completed questionnaires for the ASD group but only 20 for the control group due to missing data.
DEXA Scan (Dual-Energy X-ray Absorptiometry)
After completion of the above questionnaires and procedures, all participants underwent a DEXA scan of the lumbar (L1–L4) areas of the spine to determine bone mineral content (BMC). A projected areal density, referred to as bone mineral density (BMD g/cm2), was then calculated to assess regional bone density and strength. Instrument-generated BMD Z-scores were then determined and used for all analyses. Scanning was performed on a Hologic Discovery C Bone Densitometer (same instrument for all participants) at a regional imaging center. BMD measurements were determined from normative age- and gender-based databases of DEXA in children. Since DEXA measures area and not volumetric BMD, values may be overestimated in taller children and underestimated in smaller children (Carter et al. 1992). To help validate BMD findings, bone mineral content (BMC) was also reported as BMD can be misleading when used to compare bones of different sizes due to inherent biases caused by bone thickness differences (Carter et al. 1992). All DEXA reports were interpreted by radiologists specializing in bone densitometry.
Metacarpal X-ray
To examine bone age all participants underwent a metacarpal X-ray per standard protocol.
Statistical Analyses
All data analysis was conducted using R version 3.3.2 (Core-Team 2016). To account for non-independence of errors when data contained sibling pairs, all comparisons between ASD and control cases were analyzed using partially clustered models. Partially clustered models were fit with mixed models with a random effect for the sibling pairs, which accounts for non-independence of observations when only some observations are non-independent (Baldwin et al. 2011). This was the case for the present study in which only some participants were members of clusters (i.e. sibling pairs). All mixed models were fit using the R lme4 function (Bates et al. 2015). In all models the outcome was regressed on a variable coded 1 for ASD and 0 otherwise. For models that only included ASD participants (e.g. professionally monitored ASD GFCF participants versus ASD non-GFCF participants), ordinary least squares regression models were fit as there were no sibling pairs in these models. Pearson correlations were used for all reported correlations. To determine whether BMD increased with age, and if age-related changes in BMD differed across ASD and control participants, a regression model with age, condition, and the interaction of these two variables was used. Data were log-transformed by taking the natural log of the raw data plus one. Adding one has the benefit of allowing values of zero to be transformed and the log of 1 = 0. The one exception to this was the BMD Z-score, which was analyzed in the Z-score format. A dummy variable coded 1 if data were collected in the summer and zero otherwise was included in any models in which vitamin D was the outcome.
Results
Clinical, Biochemical and Anthropometric Data
Boys with ASD did not differ from controls for age, height, weight, BMI, and MAMC (Table 1). Biochemical data was similar for ASD and control participants, however, there were two notable exceptions: the level of serum 25 (OH) vitamin D, adjusted for season, (ASD mean [95% CI]: 41.87 [33.80, 49.94] versus control mean [CI]: 31.35 [28.02, 34.68] ng/ml; t(72) = 2.69, p = 0.009) and magnesium (ASD mean [95% CI]: 2.04 [2.00, 2.09] versus control mean [95% CI]: 1.97 [1.92, 2.01] ng/ml; t(77) = 2.47, p = 0.016) were significantly higher in ASD participants compared to controls. For the sake of brevity, only calcium, magnesium, phosphorus, vitamin D, boron, and parathyroid hormone are reported (Table 1).
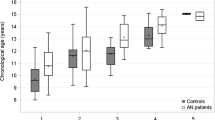
Bone Mineral Density and Bone Age
Boys with ASD had significantly lower BMD of the spine compared to controls: (Mean [95% CI] = 0.49 [0.47, 0.51] g/cm2 versus 0.55 [0.52, 0.59] g/cm2, respectively, p = 0.001; Table 1). This was also true for instrument-generated BMD Z-scores (t[71] = −3.23, p = 0.002). There was no interaction between ASD and participant age on BMD Z-scores (t[76] = −0.76, p = 0.450). A follow-up model using only age indicated that there was an increase in BMD as age increased for all participants (t[78] = 4.60, p < 0.001). BMD and BMC measures were highly correlated (r = 0.85; p < 0.001). Due to the age-dependence of BMD, BMD Z-scores were used in all subsequent analyses. Bone age, based on a metacarpal X-ray, was reported as within normal range for the majority of participants (data not shown). Bone age that was determined to be at least two SDs from the normal range were as follows: for ASD participants, three had advanced and one had delayed bone age; for control participants, four had advanced and two had delayed bone age.
Nutrient Intake, Supplementation, and Dietary Status
The intake of protein, fats and carbohydrates was similar for ASD and control participants (Table 2). There were a number of significant differences between groups in nutrient intake derived from food. Specifically, the intake of biotin, calcium, iodine, iron, phosphorus, selenium, vitamin A, vitamins B2, B6, B12, and D, folate, and zinc was significantly lower in ASD versus control participants (Table 2). Nutrients derived from supplements were not included in nutrient intake calculations but were separately calculated for calcium and vitamin D. Supplemental calcium and vitamin D intake was reported by 29/40 (72.5%) and 27/40 (67.5%) ASD subjects, respectively (data not shown). When examining both food and supplemental nutrient intake, vitamin D intake was significantly higher in the ASD group compared to controls, whereas for calcium it approached significance. For vitamin D, mean [95% CI] intake (mcg) was 39.48 [20.58, 58.38] versus 2.00 [0.93, 3.06], (t(64) = 6.03, p < 0.001) for ASD and control groups, respectively. For calcium, mean [95% CI] intake (mg) was 929.21 [798.84, 1059.57] versus 718.99 [628.71, 809.27] (t(70) = 1.79, p = 0.077) for ASD and control groups, respectively. Since only 2/40 (5.0%) control subjects reported supplementation with calcium and/or vitamin D, a comparison of intake derived from supplements only between the two groups could not be accurately determined.
ASD participants on a supported GFCF diet received nutritional counseling for between 3 and 48 months (median [IQR] = 19 [10.5, 36] months). Nutrient intake within the ASD group was similar for subjects on either a supported GFCF diet or with no dietary intervention except for the intake of iodine, which was significantly lower in ASD participants on a supported GFCF diet (p = 0.043; Table 3). While the intake of vitamin D in ASD participants was similar regardless of dietary status, the total intake of vitamin D from both dietary and supplemental sources was significantly higher in ASD participants on a supported GFCF diet compared to ASD participants with no dietary intervention: mean [95% CI] intake (mcg): 75.74 [38.13, 113.35] versus 10.45 [5.78, 15.13], t(31) = 3.65, p < 0.001, respectively. When examining total intake of calcium from both dietary and supplemental sources, intake was similar for ASD participants on a supported GFCF diet versus ASD participants with no dietary intervention: mean [95% CI] intake (mg): 1027.27 [808.25, 1246.30] versus 863.03 [696.82, 1029.24], t(33) = 1.00, p = 0.323 respectively.
Gastrointestinal Symptoms
ASD participants reported significantly higher scores on the GSRS in all five GI domains compared to control participants (p < 0.05; Table 4).
Correlation of BMD Z-Scores with Biochemical Indices
BMD Z-scores were not correlated with select biochemical measures including serum calcium, magnesium, phosphorus, vitamin D, and intact PTH in either ASD and control participants (Table 5). The only exception was for RBC boron in ASD participants, which was negatively correlated with BMD Z-scores (p = 0.027).
Correlation of BMD Z-Scores and Nutrient Intake
BMD Z-scores were not correlated with nutrient intake in ASD participants except for biotin (p = 0.047). In control participants, BMD Z-scores were correlated with the intake of calcium, vitamin B3, and folate (p < 0.05; Table 6).
Correlation of BMD Z-Scores with Dietary Status in Participants with ASD
BMD Z-scores were not correlated with dietary status within the ASD group: Mean (95% CI) BMD Z-score in ASD participants on a supported GFCF diet was −0.37 (−0.85, 0.11) compared with −0.64 (−1.13, −0.14) in ASD participants not reporting any dietary intervention (t[34] = 0.74; p = 0.463). Furthermore, there was no correlation between BMD Z-scores and length participants were on a GFCF diet (r = 0.28, p = 0.31).
Correlation of BMD Z-Scores with Symptomatic GI Presentation
BMD Z-scores were not correlated with any of the five GI domain derived from the GSRS in both ASD and control participants (Table 7).
Discussion
In this study, we examined BMD of the lumbar spine by DEXA in 4–8 year old boys with and without ASD. BMD was significantly lower in boys with ASD compared to the controls and was independent of age. There are a handful of other studies that have examined bone health in children with ASD. For example, the only previous study investigating bone density in young boys (ages 4–8 years) with ASD found that while overall bone cortical thickness (BCT) increased with age there was a progressive widening of the gap between the medians of BCT for boys with ASD and the reference group (Hediger et al. 2008). Specifically, BCT in the ASD group did not differ significantly from the reference group until age 5–6 years. However, that study relied on the Fels reference ranges for comparison, data that was derived from children studied in the 1930s–1960s (Roche and Malina 1983), which may not necessarily represent BCT of children in the twenty-first century. The study also did not include a DEXA scan, which is considered a more precise measure of bone health (Davies et al. 2005). In pre-pubertal boys, BMD at the spine, femoral neck and total hip were found to be lower in boys with ASD compared to controls (Neumeyer et al. 2013), while pubertal bone accrual was similar to controls (Neumeyer et al. 2017a). Finally, in a small study of young adults ages 14–21 years, lower BMD Z-scores were reported in the ASD group compared to healthy controls, although 7 of the 9 ASD subjects studied were on medications known to influence BMD (Ekhlaspour et al. 2016). Taken together, these data are concerning as they suggest that reduced BMD can be identified in 4–8 year old boys with ASD, and continues throughout child development and into young adulthood.
There are a number of risk factors that can affect BMD in children with ASD including nutritional status, particularly calcium and vitamin D intake (Golden et al. 2014; Palacios 2006), food selectivity due to restrictive feeding behaviors (Hyman et al. 2012), gastrointestinal (GI) disorders (Thangarajah et al. 2015), decreased physical activity (Neumeyer et al. 2017b), and medications that interfere with bone production and resorption, such as anti-epileptics and anti-psychotics (Calarge et al. 2015). In our study, laboratory testing revealed that the levels of select nutrients and elements involved in bone accrual (calcium, phosphorus, boron and parathyroid hormone) were similar between groups whereas serum vitamin D and magnesium levels were significantly lower in control participants. Height, weight, and BMI were similar in the ASD and control groups. Data examining BMI in children with ASD is conflicting with some studies reporting increased BMI and increased risk for obesity (Mari-Bauset et al. 2015; Meguid et al. 2014; Hediger et al. 2008), some reporting no difference in BMI (Neumeyer et al. 2013; Evans et al. 2012), and others reporting lower BMI in children with ASD (Barnhill et al. 2017; Mari-Bauset et al. 2012).
Dietary intake of fats, protein and carbohydrates were also similar between groups. However, the intake of several key nutrients including calcium, iron, phosphorus, folate, and vitamins A, D, B1, B2, B6, and B12 were all significantly lower in boys with ASD, similar to previous studies (Bener et al. 2014; Molloy et al. 2010; Clark et al. 1993; Neumeyer et al. 2013). Children with ASD frequently have food selectivity and feeding issues that may affect nutritional status and growth (Evans et al. 2012; Herndon et al. 2009). For example, lower calcium and vitamin D intake has been shown to affect bone accrual in children (Davies et al. 2005). Since participants with ASD in our study had lower dietary calcium and vitamin D intake, we also examined total calcium and vitamin D intake through food and supplementation. In this analysis vitamin D nutrient intake was significantly higher in participants with ASD compared to controls, which may explain why serum vitamin D levels in ASD participants were significantly higher than in controls, and why neither vitamin D nor calcium were correlated with BMD in ASD participants.
Children with ASD may also be at risk for suboptimal bone development because of restrictive dietary intakes (Williams et al. 2000; Schreck et al. 2004) or the use of a GFCF diet, which might limit calcium or vitamin D intake (Millward et al. 2004; Knivsberg et al. 2002). However, it is worth noting that children on a supported GFCF diet are more likely to be taking a vitamin D supplement (Srinivasan et al. 2016) and meet their vitamin D intake requirements (Stewart et al. 2015). This was evidenced in our study where a large proportion of ASD subjects had been prescribed a vitamin D supplement due to previous low serum 25 (OH) vitamin D testing, which significantly increased their overall vitamin D intake to levels above those of controls. When comparing total nutrient intake of calcium and vitamin D derived from both food and supplements in ASD children on a GFCF diet with clinical support versus those that reported no dietary restrictions, calcium levels and vitamin D levels were significantly higher in the GFCF group. This is an important finding since it provides evidence that dietary intervention in ASD, such as a GFCF diet, which is frequently implemented to address feeding issues, food allergies, and GI concerns, does not result in deficiencies in calcium and vitamin D when implemented and supported by a clinician. The only difference in dietary intake for ASD participants on a supported versus unsupported diet was for iodine, which was significantly lower in ASD participants on a supported diet. This may arise from the increased intake of processed foods for children on unsupported diets.
In the current study, ASD boys on a supported GFCF diet had similar BMD to ASD boys on unrestricted diets. Conversely, Hediger et al. (2008) reported that 12% of the boys on a casein-free diet had an overall larger deviation in bone cortical thickness (BCT), to almost twice that of boys on minimally restricted or unrestricted diets. In pre-pubertal boys, four boys with ASD on GFCF diets had lower BMD (Neumeyer et al. 2013). However, neither of these studies identified which subjects were on a clinician-supported GFCF diet versus those that were not. This is a necessary distinction since many families implement dietary intervention and the use of supplements for their child with ASD without clinical support (Wong and Smith 2006), which may negatively impact the levels of micronutrients and supplements consumed (Stewart et al. 2015). For example, a child on a nutrient-dense, casein-free diet may receive more than adequate levels of calcium and vitamin D compared to a child receiving the standard American diet (Herndon et al. 2009). The data from our study suggests that the intake of calcium and vitamin D in children on a GFCF diet is not a contributing factor to the observed decrease in BMD in ASD participants.
GI disorders and associated symptoms including chronic abdominal pain, constipation, chronic diarrhea and gastroesophageal reflux (GERD), are commonly reported in children with an ASD (Buie et al. 2010a, b; Valicenti-McDermott et al. 2006; Black et al. 2002). Children without ASD or developmental delays, but diagnosed with Crohn’s disease or ulcerative colitis, have been found to have decreased BMD (Lopes et al. 2008). While participants with Crohn’s disease, celiac disease, and inflammatory bowel disease were excluded from the study, a questionnaire was included to capture undiagnosed GI concerns. In this study we found that boys with ASD reported significantly greater GI symptoms than boys without ASD across all five GI symptom domains assessed. Furthermore, some of the dietary micronutrient deficiencies reported for the ASD participants (including iron, vitamin B1, B6 and B12) are also commonly reported as serum deficiencies in IBD (Weisshof and Chermesh 2015). This reinforces potential concern for nutrient intake and absorption in children with ASD, especially when there are GI symptoms present.
There are a number of limitations to this study. Firstly, the cross-sectional study design does not prove causation, and thus limits the findings. Secondly, the sample size did not allow for stratification of the data by ASD severity or diagnosis, nor could we stratify by ethnicity. ASD severity may play a role in a child’s motor planning/mobility, access to daylight and/or exercise/activity level, which were not addressed in this study, and overall health. Ethnicity could impact lifestyle including dietary intake and/or dietary restrictions. Additionally, a number of ASD participants were from families actively pursuing nutritional care with clinicians with nutritional expertise. Their awareness of the importance of nutritional strategies should be taken into consideration when viewing these results. Finally, gastrointestinal symptoms were reported by parents and were not confirmed clinically. Despite there being a high frequency of GI symptoms reported in children with ASD (Buie et al. 2010a), they are more difficult to recognize in a child with ASD and may go undiagnosed (Kushak et al. 2016).
In summary, this study suggests that reduced BMD can be identified in 4–8 year old children with ASD, and that nutrient intake and dietary status were not driving this effect, at least in participants under the care of a clinician monitoring nutrient/supplement intake. Additional research studies should include girls with ASD, as well as children of younger ages to determine how early BMD may be affected in ASD. Furthermore, research on additional risk factors for reduced BMD in children with ASD, such as GI symptoms and/or limited physical activity, should be undertaken.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. (5th edn.). Arlington, VA: American Psychiatric Association.
Baldwin, S. A., Bauer, D. J., Stice, E., & Rohde, P. (2011). Evaluating models for partially clustered designs. Psychological Methods, 16(2), 149–165. doi:10.1037/a0023464.
Barnhill, K., Gutierrez, A., Ghossainy, M., Marediya, Z., Marti, C. N., & Hewitson, L. (2017). Growth status of children with autism spectrum disorder: A case-control study. Journal of Human Nutrition and Dietetics, 30(1), 59–65. doi:10.1111/jhn.12396.
Bates, D., Mächler, M., Bolker, B., & Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software. doi:10.18637/jss.v067.i01.
Bausserman, M., & Michail, S. (2005). The use of Lactobacillus GG in irritable bowel syndrome in children: a double-blind randomized control trial. Journal of Pediatrics, 147(2), 197–201.
Bener, A., Khattab, A. O., & Al-Dabbagh, M. M. (2014). Is high prevalence of vitamin D deficiency evidence for autism disorder?: In a highly endogamous population. Journal of Pediatric Neuroscience, 9(3), 227–233. doi:10.4103/1817-1745.147574.
Black, C., Kaye, J. A., & Jick, H. (2002). Relation of childhood gastrointestinal disorders to autism: Nested case-control study using data from the UK general practice research database. British Medical Journal, 325(7361), 419–421.
Buie, T., Campbell, D. B., Fuchs, G. J., Furuta, G. T., Levy, J., Vandewater, J., et al. (2010a). Evaluation, diagnosis, and treatment of gastrointestinal disorders in individuals with ASDs: A consensus report. Pediatrics, 125(Suppl 1), S1–S18.
Buie, T., Fuchs, G. J., Furuta, G. T., Kooros, K., Levy, J., Lewis, J. D., et al. (2010b). Recommendations for evaluation and treatment of common gastrointestinal problems in children with ASDs. Pediatrics, 125(Suppl 1), S19–S29. doi:10.1542/peds.2009-1878D.
Calarge, C. A., Burns, T. L., Schlechte, J. A., & Zemel, B. S. (2015). Longitudinal examination of the skeletal effects of selective serotonin reuptake inhibitors and risperidone in boys. Journal of Clinical Psychiatry, 76(5), 607–613. doi:10.4088/JCP.14m09195.
Carter, D. R., Bouxsein, M. L., & Marcus, R. (1992). New approaches for interpreting projected bone densitometry data. Journal of Bone Mineral Research, 7(2), 137–145. doi:10.1002/jbmr.5650070204.
Clark, J. H., Rhoden, D. K., & Turner, D. S. (1993). Symptomatic vitamin A and D deficiencies in an eight-year-old with autism. Journal of Parenteral and Enteral Nutrition, 17(3), 284–286. doi:10.1177/0148607193017003284.
Core-Team, R. (2016). R: A language a nd environment for statistical computing. https://www.R-project.org/. Accessed 14 July 2017.
Davies, J. H., Evans, B. A., & Gregory, J. W. (2005). Bone mass acquisition in healthy children. Archives of Disease in Childhood, 90(4), 373–378. doi:10.1136/adc.2004.053553.
Dimenas, E., Carlsson, G., Glise, H., Israelsson, B., & Wiklund, I. (1996). Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scandinavian Journal of Gastroenterology, 31(Suppl 221), 8–13.
Ekhlaspour, L., Baskaran, C., Campoverde, K. J., Sokoloff, N. C., Neumeyer, A. M., & Misra, M. (2016). Bone density in adolescents and young adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. doi:10.1007/s10803-016-2871-9.
Evans, E. W., Must, A., Anderson, S. E., Curtin, C., Scampini, R., Maslin, M., et al. (2012). Dietary patterns and body mass index in children with autism and typically developing children. Research in Autism Spectrum Disorders, 6(1), 399–405. doi:10.1016/j.rasd.2011.06.014.
Golden, N. H., & Abrams, S. A.,& Committee on Nutrition. (2014). Optimizing bone health in children and adolescents. Pediatrics, 134(4), e1229–e1243. doi:10.1542/peds.2014-2173.
Goodman, S. B., Jiranek, W., Petrow, E., & Yasko, A. W. (2007). The effects of medications on bone. Journal of the American Academy of Orthopedic Surgery, 15(8), 450–460.
Gotham, K., Risi, S., Pickles, A., & Lord, C. (2007). The autism diagnostic observation schedule: Revised algorithms for improved diagnostic validity. Journal of Autism and Developmental Disorders, 37(4), 613–627. doi:10.1007/s10803-006-0280-1.
Hartman, C., Eliakim, R., & Shamir, R. (2009). Nutritional status and nutritional therapy in inflammatory bowel diseases. World Journal of Gastroenterology, 15(21), 2570–2578.
Haubrock, J., Nothlings, U., Volatier, J. L., Dekkers, A., Ocke, M., Harttig, U., et al. (2011). Estimating usual food intake distributions by using the multiple source method in the EPIC-potsdam calibration study. Journal of Nutrition, 141(5), 914–920. doi:10.3945/jn.109.120394.
Hediger, M. L., England, L. J., Molloy, C. A., Yu, K. F., Manning-Courtney, P., & Mills, J. L. (2008). Reduced bone cortical thickness in boys with autism or autism spectrum disorder. Journal of Autism and Developmental Disorders, 38(5), 848–856. doi:10.1007/s10803-007-0453-6.
Herndon, A. C., DiGuiseppi, C., Johnson, S. L., Leiferman, J., & Reynolds, A. (2009). Does nutritional intake differ between children with autism spectrum disorders and children with typical development? Journal of Autism and Developmental Disorders, 39(2), 212–222. doi:10.1007/s10803-008-0606-2.
Hyman, S. L., Stewart, P. A., Schmidt, B., Cain, U., Lemcke, N., Foley, J. T., et al. (2012). Nutrient intake from food in children with autism. Pediatrics, 130(Suppl 2), S145–S153. doi:10.1542/peds.2012-0900L.
Institute of Medicine (2005). Panel on macronutrients standing committee on the scientific evaluation of dietary reference intakes. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, D.C.: National Academies Press.
Knivsberg, A. M., Reichelt, K. L., Hoien, T., & Nodland, M. (2002). A randomised, controlled study of dietary intervention in autistic syndromes. Nutritional Neuroscience, 5(4), 251–261. doi:10.1080/10284150290028945.
Kushak, R. I., Buie, T. M., Murray, K. F., Newburg, D. S., Chen, C., Nestoridi, E., et al. (2016). Evaluation of intestinal function in children with autism and gastrointestinal symptoms. Journal of Pediatric Gastroenterology and Nutrition, 62(5), 687–691. doi:10.1097/MPG.0000000000001174.
Lionetti, E., Miniello, V. L., Castellaneta, S. P., Magista, A. M., de Canio, A., Maurogiovanni, G., et al. (2006). Lactobacillus reuteri therapy to reduce side-effects during anti-Helicobacter pylori treatment in children: A randomized placebo controlled trial. Alimentary Pharmacology & Therapeutics, 24(10), 1461–1468. doi:10.1111/j.1365-2036.2006.03145.x.[pii].
Lopes, L. H., Sdepanian, V. L., Szejnfeld, V. L., de Morais, M. B., & Fagundes-Neto, U. (2008). Risk factors for low bone mineral density in children and adolescents with inflammatory bowel disease. Digestive Diseases and Sciences, 53(10), 2746–2753. doi:10.1007/s10620-008-0223-0.
Macdonald, M., Esposito, P., & Ulrich, D. (2011). The physical activity patterns of children with autism. BMC Research Notes, 4, 422. doi:10.1186/1756-0500-4-422.
Mahan, K. L., & Escott-Stump, S. (2008). Krause’s Food and Nutrition Therapy. (12th edn.). St Louis, MO: Saunders.
Mari-Bauset, S., Llopis-González, A., Zazpe, I., Mari-Sanchís, A., & Suárez-Varela, M. M. (2015). Anthropometric measures of Spanish children with autism spectrum disorder. Research in Autism Spectrum Disorders, 9, 26–33.
Mari-Bauset, S., Zazpe, I., Mari-Sanchis, A., Llopis-González, A., & Suárez-Varela, M. M. (2012). Are there anthropometric differences between autistic and healthy children? Journal of Child Neurology, 28, 1226–1232.
Meguid, N. A., Kandeel, W. A., Wakeel, K. E., & El-Nofely, A. A. (2014). Anthropometric assessment of a middle eastern group of autistic children. World Journal of Pediatrics, 10(4), 318–323. doi:10.1007/s12519-014-0510-0.
Millward, C., Ferriter, M., Calver, S., & Connell-Jones, G. (2004). Gluten- and casein-free diets for autistic spectrum disorder. The Cochrane Database of Systematic Reviews, 2:CD003498. doi:10.1002/14651858.CD003498.pub2.
Molloy, C. A., Kalkwarf, H. J., Manning-Courtney, P., Mills, J. L., & Hediger, M. L. (2010). Plasma 25(OH) D concentration in children with autism spectrum disorder. Developmental Medicine & Child Neurology, 52(10), 969–971. doi:10.1111/j.1469-8749.2010.03704.x.
Neumeyer, A. M., Gates, A., Ferrone, C., Lee, H., & Misra, M. (2013). Bone density in peripubertal boys with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(7), 1623–1629. doi:10.1007/s10803-012-1709-3.
Neumeyer, A. M., Sokoloff, N. C., McDonnell, E., Macklin, E. A., McDougle, C. J., & Misra, M. (2017a). Bone accrual in males with autism spectrum disorder. Journal of Pediatrics, 181, 195–201. doi:10.1016/j.jpeds.2016.10.080.
Neumeyer, A. M., Sokoloff, N. C., McDonnell, E., Macklin, E. A., McDougle, C. J., & Misra, M. (2017b). Bone microarchitecture in adolescent boys with autism spectrum disorder. Bone, 97, 139–146. doi:10.1016/j.bone.2017.01.009.
Palacios, C. (2006). The role of nutrients in bone health, from A to Z. Critical Reviews in Food Science and Nutrition, 46, 621–628.
Porter, R. S., & Kaplan, J. L. (2011). The Merck Manual of Diagnosis and Therapy. (19th edn.). Whitehouse Station: Merck Research Laboratories.
Roche, A. F., & Malina, R. M. (Eds.). (1983). Manual of Physical Status and Performance in Childhood: Physical Status (Vol. 1B). New York: Plenum Press.
Roke, Y., van Harten, P. N., Buitelaar, J. K., Tenback, D. E., Quekel, L. G., de Rijke, Y. B., et al. (2012). Bone mineral density in male adolescents with autism spectrum disorders and disruptive behavior disorder with or without antipsychotic treatment. European Journal of Endocrinology, 167(6), 855–863. doi:10.1530/EJE-12-0521.
Rutter, M., Le Couteur, A., & Lord, C. (2003). Autism diagnostic interview–revised (ADI–R) manual. Los Angeles: Western Psychological Services.
Schaafsma, A., de Vries, P. J., & Saris, W. H. (2001). Delay of natural bone loss by higher intakes of specific minerals and vitamins. Critical Reviews in Food Science and Nutrition, 41(4), 225–249.
Schieve, L. A., Gonzalez, V., Boulet, S. L., Visser, S. N., Rice, C. E., Van Naarden Braun, K., et al. (2012). Concurrent medical conditions and health care use and needs among children with learning and behavioral developmental disabilities, National Health Interview Survey, 2006–2010. Research in Developmental Disabilities, 33(2), 467–476. doi:10.1016/j.ridd.2011.10.008.
Schreck, K. A., Williams, K., & Smith, A. F. (2004). A comparison of eating behaviors between children with and without autism. Journal of Autism and Developmental Disorders, 34(4), 433–438.
Srinivasan, S., O’Rourke, J., Bersche Golas S., Neumeyer, A., & Misra, M. (2016). Calcium and vitamin D supplement prescribing practices among providers caring for children with autism spectrum disorders: Are we addressing bone health?. Autism Research and Treatment, 2016, 6763205. doi:10.1155/2016/6763205.
Stewart, P. A., Hyman, S. L., Schmidt, B. L., Macklin, E. A., Reynolds, A., Johnson, C. R., et al. (2015). Dietary supplementation in children with autism spectrum disorders: Common, insufficient, and excessive. Journal of the Academy of Nutrition and Dietetics, 115(8), 1237–1248. doi:10.1016/j.jand.2015.03.026.
Svedlund, J., Sjodin, I., & Dotevall, G. (1988). GSRS—a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Digests in Disability Science, 33(2), 129–134.
Thangarajah, D., Hyde, M. J., Konteti, V. K., Santhakumaran, S., Frost, G., & Fell, J. M. (2015). Systematic review: Body composition in children with inflammatory bowel disease. Alimentary Pharmacology & Therapeutics, 42(2), 142–157. doi:10.1111/apt.13218.
Thomson, M., Fritscher-Ravens, A., Hall, S., Afzal, N., Ashwood, P., & Swain, C. P. (2004). Endoluminal gastroplication in children with significant gastro-oesophageal reflux disease. Gut, 53(12), 1745–1750, doi:10.1136/gut.2004.041921.
Valicenti-McDermott, M., McVicar, K., Rapin, I., Wershil, B. K., Cohen, H., & Shinnar, S. (2006). Frequency of gastrointestinal symptoms in children with autistic spectrum disorders and association with family history of autoimmune disease. Journal of Developmental and Behavioral Pediatrics, 27(2 Suppl), S128–S136.
Weisshof, R., & Chermesh, I. (2015). Micronutrient deficiencies in inflammatory bowel disease. Current Opinion in Clinical Nutrition & Metabolic Care, 18(6), 576–581. doi:10.1097/MCO.0000000000000226.
Williams, P. G., Dalrymple, N., & Neal, J. (2000). Eating habits of children with autism. Pediatric Nursing, 26(3), 259–264.
Wong, H. H., & Smith, R. G. (2006). Patterns of complementary and alternative medical therapy use in children diagnosed with autism spectrum disorders. Journal of Autism and Developmental Disorders, 36(7), 901–909. doi:10.1007/s10803-006-0131-0.
Acknowledgments
We are very grateful to all the families that participated in this research study. We would particularly like to thank Anissa Ryland, Morgan Devlin, Nichole Roatch, Tiffany Maudlin, Tony Phelan, Michael Rotko, Hannah Somerville, Meg Glausser, Sean Goetz, and all the support staff and clinicians at The Johnson Center for Child Health and Development, for assistance with implementing this study. Funding was provided by The Johnson Center for Child Health and Development.
Author contribution
KB and LH conceived the study, participated in its design and coordination, interpreted the data, and drafted the manuscript; LR, AG, RS and CS participated in the design of the study and performed the measurements; WR and AP participated in the design and coordination of the study and collected data; and CNM performed the statistical analysis, assisted in the interpretation of the data, and helped draft the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All of the authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants, or participant’s representative (parent), included in the study and according to the above-mentioned principles.
Rights and permissions
About this article
Cite this article
Barnhill, K., Ramirez, L., Gutierrez, A. et al. Bone Mineral Density in Boys Diagnosed with Autism Spectrum Disorder: A Case-Control Study. J Autism Dev Disord 47, 3608–3619 (2017). https://doi.org/10.1007/s10803-017-3277-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-017-3277-z