Abstract
The primary purposes of this study were to compare (a) physical activity participation, screen-time habits, obesity, and (b) reported reasons for lack of participation in sport, between a nationally representative sample of Irish children with and without autism spectrum disorder (ASD). Participation in moderate to vigorous activity, light activity, and sports was significantly lower among the group with ASD. On examination of screen time variables, no significant differences were seen between groups. However, time spent watching TV was higher among children with ASD. Overweight or obese status was more prevalent among the group with ASD (34.4 vs. 24.7 %). The findings are discussed in relation to international statistics on youth physical activity, screen-time, and weight status, and recommendations are provided for future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity among youth is a public health issue of global importance (Han et al. 2010). Lifestyle factors such as physical inactivity and excessive screen time usage have been identified as modifiable causal factors (Jimenez-Pavon et al. 2010; Smith et al. 2010). Regular engagement in physical activity (PA) has been demonstrated to help youth control their weight while decreasing the chances of developing additional health-related issues, such as cardiovascular disease, diabetes, hypertension, anxiety, and depression (Centers for Disease Control and Prevention [CDC], 2014). Independent of physical activity participation, sedentary behaviors (e.g., screen time) can have potentially deleterious health consequences and have been identified as a risk factor for several health-related issues including cardiovascular disease and type 2 diabetes (Starkoff et al. 2014). Recent research, utilizing a representative sample of youth aged 12–15 years in the United States (U.S.) suggests that about one quarter engaged in the recommended daily 60 min of moderate to vigorous physical activity (Fakhouri et al. 2014). Similarly, in Europe, research shows that only one-in-five children, aged 11–15, report that they undertake moderate-to-vigorous exercise regularly, according to results from the 2009–2010 HBSC survey (Curie et al. 2012). Ireland consistently stands out as a strong performer; with 31 % of girls and 43 % of boys at age 11 meeting the guidelines (Curie et al. 2012).
For all youth, physical activity and screen time habits are important elements to promote and maintain health, fitness, and well-being (Laurson et al. 2014). For children with autism spectrum disorder (ASD), research has identified a number of additional benefits to being physically active, such as improvements in social skills, sleep quality, and feelings of enjoyment (Ayvazoglu et al. 2015; Wachob and Lorenzi 2015). Unfortunately, however, research suggests that youth with ASD may be at especially high risk of not engaging in PA during leisure time (Tyler et al. 2014) and the school day compared to their TD peers (Memari et al. 2013; Pan et al. 2015). Research findings point to several reasons for why youth with ASD refrain from PA, such as limitations in social-communication, lack of motor domain skills, and social exclusion from activities. (Srinivasan et al. 2014) (Must et al. 2015).
Rather than engaging in physical activities, youth with ASD tend to spend more time engaging in screen time activities (e.g., watching television, playing video games) than their typically developing (TD) peers (Mazurek and Wenstrup 2013; Memari et al. 2013; Must et al. 2014; Sandt and Frey 2005). This may be partially attributed to parents, who use screen time activities to occupy youth with ASD during household chores (Sandt and Frey 2005). Because children with ASD tend to be less physically active and engage in more screen time activities than peers without disabilities, they are at greater risk for experiencing health-related issues. As such, research suggests that youth with ASD may have higher rates of obesity and lower fitness levels than their TD peers (Curtin et al. 2010; Srinivasan et al. 2014; Tyler et al. 2014). According to Curtin et al. (2010), the prevalence of obesity in children with ASD in the U.S. is approximately 30.4 %, in comparison to 23.6 % among their TD peers. There is somewhat conflicting evidence regarding the obesity of youth with ASD in the United States, though, as more recent nationally representative data suggest ASD status is not independently related to obesity once secondary conditions (e.g., learning disabilities) and medication use are taken into account (Corvey et al. 2016).
Currently, research examining physical activity participation, screen time habits, and obesity in youth with ASD is limited by geographic location and small samples (Corvey et al. 2016). Although a few population-based studies have been conducted in North America pertaining to ASD (Corvey et al. 2016; Curtin et al. 2010) and other disabilities (Kim et al. 2013; Wilson et al. 2016), research of this magnitude is currently absent in a number of European countries, including Ireland. It is reasonable to suggest that barriers to physical activity participation are contextually influenced, and those experienced by youth with ASD in Ireland will likely vary from those experienced by children in other countries. Therefore, the primary purposes of this investigation were to compare (a) physical activity participation, screen-time habits, and obesity, and (b) reported reasons for lack of participation in sport, between a nationally representative sample of Irish children with and without ASD. Furthermore, a secondary purpose was to examine physical activity, screen-time habits and obesity among the children with ASD, based on gender, age of diagnosis, and comorbidities.
Method
Participants
Data were obtained from wave two of the nationally representative data set; Growing Up in Ireland (GUI) which included a range of physical, behavioral, psychological, environmental, and cognitive outcomes for 13 year olds living in Ireland. A systematic stratified sampling procedure was utilized to recruit participants (n = 8570) from 910 schools (of the national total of 3200 Primary schools) across Ireland. Parents and children completed questionnaires on a range of outcomes related to the child’s characteristics, experiences, and development. In addition, the child’s teacher and school principal provided information relating to the child’s social, emotional, and cognitive development, as well as school characteristics. The data were collected between September 2007 and June 2008, under ethical approval from the Health Research Boards’ Research Ethics Committee. Response rates were 82 and 57 % at the school and family levels, respectively. For more detailed information on the data set, including the conceptual framework and methodology, see Murray et al. (2011).
The present study included 141 children; 67 children with ASD, and a randomly extracted sample of 74 TD children for comparison. Adolescents were included in the ‘ASD group’ if their primary caregiver reported that the child had ASD diagnosed by a medical professional. In Ireland, professionals who may provide a diagnosis include psychologists, psychiatrists and/or community paediatricians, in conjunction with other disciplines such as speech and language therapist, clinical nurse specialist, and social workers (Health Service Executive 2012).
Measures
Physical Activity and Sport Participation
Multiple self-report measures of physical activity and sport participation were included in the analysis. First, the adolescents’ physical activity was measured though self-report, using questions adapted from the Leisure Time Exercise Questionnaire (Godin and Shepard 1985). To assess participation in moderate to vigorous physical activity (MVPA), the respondents answered the question “How many times, in the past 14 days, have you done at least 20 min of hard exercise to make you breathe fast and make your heart beat faster?”; examples of activities were provided including playing soccer, jogging and fast cycling. To assess participation in light physical activity, the participants were asked “How many times in the past 14 days have you done at least 20 min of light exercise that was not hard enough for you to breathe heavily and make your heart beat fast?” Examples provided included walking or slow cycling. For both questions participants were instructed to include time spent in physical education. Participants responded using a five-point scale, ranging from 1 (none) to 5 (9 or more days). These measures were used in previous research (Cadogen et al. 2014), have demonstrated concurrent validity with measures of maximum oxygen intake (VO2 max) and muscular endurance (Godin et al. 1986), and acceptable test–retest reliability (Sallis et al. 1993).
A series of questions were also asked regarding the child’s participation in sport. The number of team or individual sports in which the child participates was assessed with the question “Outside of your physical education classes, how many team or individual sports or activities did you participate in during the past 12 months?” Examples provided included a school or local soccer/netball team, athletics, or tennis club. Respondents choose from none, one, two, three, or four or more activities. Respondents were also asked if they “play sports or undertake physical activities without a coach or instructors (e.g. biking, skate-boarding, etc.)?” and if they “play sports with a coach or instructor, or as part of an organized team, other than in Physical Education class (swimming, soccer, hockey, etc.)?”. Answer options for both questions included: (1) never; (2) less than once a week; (3) 1–3 times a week; or, (4) 4 or more times a week.
Screen Time Variables
Children answered three questions that measured screen time behavior of the sample with and without ASD. Questions included: (1) “on a normal weekday during term-time, about how many hours do you spend watching television, videos or DVDs? Please remember to include time before school as well as time after school?” (2) “On a normal weekday, during term-time, about how much time do you spend using the computer? Please include time before school as well as time after school. Do not include time spent using computers in school”; and (3), “On a normal weekday, during term-time, about how much time do you spend playing video games such as Playstation, X-box, Nintendo, etc.?” In response to these questions respondents selected one of 13 categories, representing 30 min increments (e.g., 1–30 min). A total screen time scale variable was also created which combined the three screen time variables (television, computer, and video games), thus resulting in a 39 point scale. A higher score on all variables reflects higher levels of screen time.
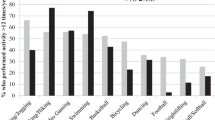
Reasons for Lack of Team Sport Participation
In addition to exploring numerical values for duration of physical activity, the GUI also sought to explain reasons why participants did not participate Participants were asked the question,. “Outside of your physical education classes, how many team or individual sports or activities did you participate in during the past 12 months?,”If respondents selected “none”, they were prompted to select reasons as to why they “choose not to participation in sporting activities?.” Possible reasons that the respondent could choose from included: (1) I do not like team games; (2) I prefer to watch sports on TV; (3) I am no good at games; (4) I do not fit in with the sporty crowd; (5) I have no opportunities to play; (6) I do not like to get dirty or sweaty; (7) I feel people laugh at me because of my size; (8) I am not competitive; (9) I have a disability or health problem which prevents me from playing; (10) I prefer to play computer games; and finally, (11) respondents could select ‘other’ and to specify their reason.
Body Mass Index
Body mass index is the most widely used method for measuring the degree of body fat in children and has shown to correlate strongly with measures of body fat derived from direct physiological assessment (Lindsay et al. 2001). To derive a body mass index score for each child, in each household the interviewer took the weight and height of each study child. A Leicester portable height measure was used to record height to the nearest millimeter. For weight, a Class IV, medically approved scales (SECA 761) were used to record the child’s weight to the nearest kilogram. Body mass index was then calculated by dividing weight in kilograms by height in meters squared. Body mass index cut-offs, standardized by age and sex, as provided by the International Obesity Task Force (IOTF) (Cole et al. 2000), were used to classify children as non-overweight, overweight, or obese.
Statistical Analyses
Descriptive statistics for participants’ demographic data were reported. Pearson correlations were conducted to examine the relationship between the physical activity, screen time variables, comorbidities, and age of diagnosis (before 6, 6–10, and 10+). Mann–Whitney tests and Fisher exact tests were used to compare continuous and categorical physical activity, screen time, and BMI variables between children with ASD and TD children. When ordinal or continuous dependent variables were not normally distributed, Kruskal–Wallis tests were used to determine if there were significant differences between two or more groups. Moreover, exploratory analyses were completed, with data stratified by gender, age of diagnosis, presence of comorbidities, and weight status (IOTF BMI categories). All analysis were conducted using SPSS 23, with an alpha level set at 0.05.
Results
A comparison of the TD children with the members of the full dataset, showed there to be no significant differences on physical activity, screen time behaviors, or BMI (p < .05). Descriptive characteristics of the children are provided in Table 1, presented as TD children and children with ASD. Chi square tests were used to compare groups on gender and mothers’ education level (college or not); Mann Whitney was used for comparison of the continuous variable, equivalized-household income (weighted to account for differences in size and composition of households in terms of the number of adults and children in the home). Fifty-three members of the group who had ASD (57.6 %) were male, in comparison to 39 males in the TD group (42.4 %) (p = .002). Additional information on characteristics of the group with ASD are presented in Table 2, including the number of comorbidities experienced by the child, comorbidity type, medication use, and age of ASD diagnosis.
Physical Activity and Sport Participation
The most commonly reported number of days that children with ASD reported at least 20 min of MVPA over the past 14 days was “1–2 days”, with 32.85 % (n = 22) of the sample selecting this response (Table 3). In contrast, only 10.8 % of TD children selected the “1–2 days” response, with the most commonly reported response for TD children (36.5 %) being “9 or more days” during the 2 week period. Comparing MVPA participation on 5 or fewer days versus 6 or more days per 2 week period, Fishers Exact test demonstrated the children with ASD participated in significantly less MVPA (p < .001). Results showed that 70.1 % (n = 47) of the children with ASD participated in less than 5 days of MVPA compared to only 23.9 % (n = 16) of the TD children. Regarding number of days with at least 20 min of participation in light physical activity, there were no significant differences between the children with ASD and the TD children (Table 3).
On the measure of participation in team or individual sports outside of physical education, the children with ASD reported to participate in a mean of 2.2 sports, in comparison to the mean of 3.07 sports participated in by the TD group (U = 1513, p < .001) (Table 3). More specifically, the group with ASD undertook significantly fewer activities that involved a coach or instructor per week (U = 1516, p < .001). Results showed that 24 children with ASD (37.5 %) reported never playing sports with a coach in comparison to 18 TD children (25 %). Conversely, 25 TD children (34.7 %) reported to participate in sports with a coach four or more times a week, in comparison to only three children with ASD (4.7 %). Regarding participation in sports or physical activity without a coach, no significant differences were revealed between TD children and children with ASD (U = 1980, p = .106). However, 18 TD children (25 %) participated in sports without a coach four or more times a week in comparison to 9 children with ASD (14.1 %). For children with ASD, Pearson correlations revealed a positive significant correlation between levels of MVPA and participation in team or individual sports outside of physical education (r = .471, n = 63, p < .001), participation in sports with a coach or instructor (r = .597, n = 63, p < .001), and participation in sports without a coach or instructor (r = .696, n = 63, p < .001).
Physical Activity and Gender
For TD children, males participated in more MVPA, with the majority (51.3 %, n = 20) participating in 9 or more days that included at least 20 min of MVPA, than females. Only 30 % (n = 7) of the females participated in this amount of MVPA. When comparing reported MVPA participation as being 5 or fewer days versus 6 or more days per 2 week period, significant difference between males and females was revealed (p = .001). Males also participated in significantly more sports without a coach (M = 2.87 vs. M = 2.18, U = 422, p = .009), and with a coach (M = 3.08 vs. 2.5, U = 478.5, p = .46). No significant differences were revealed between males and females in the sample of children with ASD on MVPA, LPA, or sports participation variables.
Physical Activity, Comorbidities and Age of Diagnosis
Pearson correlation did not indicate the number of comorbidities or age of diagnosis to be significantly correlated with the physical activity variables of interest, for the children with ASD. Kruskal–Wallis Tests determined mean levels of participation in MVPA, among the children with ASD, did not differ depending upon age of diagnosis, number of comorbidities, or comorbidity type (p > .05).
Screen Time
For time spent watching television, children with ASD reported spending, on average, between 121 and 150 min per day in comparison to TD children who spent a mean of 91–120 min a day. Time spent using the computer per day was less, with both groups reporting spending a mean of 61–90 min per day. Time spent playing video games was also similar for both groups, with a mean of 31–60 min a day spent in this activity. Finally, although not quite statistically significant, comparing groups on the total screen time scale variable, children with ASD engaged in more screen time (m = 11.8) than TD children (m = 10.02),(U = 1901, p = .105). For the group with ASD, Pearson’s correlation showed total screen time score to be negatively correlated with both participation in light physical activity (r = −.33, n = 62, p = .009), and number of sports participated in outside of physical education (r =− .34, n = 62, p = .−026).
Screen Time, Comorbidities and Age of Diagnosis
No significant correlations existed between number of comorbidities and screen time variables, however, the age of diagnosis was correlated with time spent watching television (r = −.26). Children diagnosed with ASD before the age of five (n = 18), or between 5 and 10 years (n = 27), spent, on average, 121–151 min watching television. Conversely, the children who were diagnosed after age 10 spent an average of 61–91 min watching television. Kruskal–Wallis Tests determined mean levels of total screen time, among the children with ASD, did not significantly differ depending upon age of diagnosis, number of comorbidities, or comorbidity type (p > .05).
Reasons for Lack of Team Sport Participation
Twenty-three children with ASD and 11 TD children answered the question relating to reasons not to participate in sport. The most prevalent response provided by both groups for lack of participation in sports outside of physical education, was “I prefer to play computer games” including 13 children with ASD (56.5 %) and four TD children (36.4 %). The reasons “I do not like team games” and "I am not competitive” were each chosen twice by children with ASD. The other reasons for lack of participation were each chosen once. Two children from each group provided reasons identified as ‘other’ which were not available for viewing in the data set available to the researchers.
Body Mass Index (BMI)
Height and weight measures were missing for three children with ASD, and one TD child. The mean BMI for the children with ASD was 21.21, in comparison to 20.42 for the TD children. Distributions were not significantly different (U = 2122, p = .438). On comparing groups by weight status, overweight/obese status was more prevalent among the group with ASD, with 22 children being overweight/obese (34.9 %), in comparison to 18 children (24.7 %) in the TD group. A Chi Square test demonstrated this difference to not be significant (p = .190). See Table 4 for an overview of weight status among children with ASD and TD children. Kruskal–Wallis Tests determined mean BMI among the children with ASD did not differ depending upon age of diagnosis, number of comorbidities, or comorbidity type (p > .05).
Discussion
A primary purpose of this article was to compare PA participation between a nationally representative sample of Irish children with ASD and TD peers. In this study, over 70 % of the children with ASD participated in <5 days of MVPA over a two-week period, in comparison to only 23.9 % of the TD children. Children with ASD most frequently reported to participate in at least 20 min of MVPA on 1–2 days over a two-week period. Conversely, TD children most frequently reported to participate in MVPA on 9 or more days. Overall, the findings of our study reflect the inactivity of youth with ASD in other research. For example, Memari et al. (2015) utilized parent-reported data on children with ASD, aged 6–15, (n = 83) finding that only 12 % (n = 10) of children with ASD were active and 88 % (n = 73) were inactive based upon activity guidelines and activity score measured by the Godin-Shephard Leisure Time Questionnaire (GLTEQ). This result is in contrast to research by Corvey et al. (2016) who found no significant differences in physical activity rates between the sample with ASD and the TD control. In addition, Bandini et al. (2013) demonstrated children with and without ASD, with a mean age of 6.6, participated in similar amounts of light, moderate, and vigorous physical activity as measured by accelerometry, when adjusted for age and sex. However, parent reports did reveal the children with ASD to participated in significantly fewer types of activities than the TD children. (6.9 vs. 9.9 per year, respectively). The tendency for youth with ASD to participate in fewer activities and sports is reflected in the 2003 National Survey of Children’s Health finding that children with ASD were less likely to participate in sports (41 vs. 27 %, p < .005) or extracurricular activities (45 vs. 34 %, p < .05) than children with other developmental disabilities. The finding in our study support this trend, whereby the children with ASD reported to engage in fewer sports outside of physical education compared to their TD counterparts (2.2 vs. 3.07). More specifically, the majority (n = 24, 35.7 %) of the group with ASD reported to never participate in sports or physical activities involving a coach, in comparison the majority (n = 22, 29.7 %) of the TD children who participated one to three times per week. This may be due to the tendency for sport with a coach to typically be of a more competitive nature, which may make it less appealing to children with ASD whom have been reported to have movement impairments (Blanchard et al. 2006). In addition, in Ireland sports that involve a coach would most commonly be team sports such as football (soccer), and Gaelic games (Gaelic football and Hurling). The social nature of these sports may be demanding for a child with difficulties in the social domain, such as those with ASD.
Research on barriers to physical activity for children with ASD is sparse and predominantly focuses on parental report. Common barriers cited by parents include time and financial constraints, and lack of opportunities (Memari et al. 2015; Lee et al. 2008). Albeit infrequent, the perspective of children with ASD has been elicited also. Obrusnikova and Cavalier (2011), utilized Photovoice to enable 14 children with ASD to recall barriers to physical activity. Among their responses, intrapersonal barriers and a preference for screen-based activities were the most commonly noted. These finding reflect the results of our study. The preference for screen-based activities as a barrier to physical activity participation was the most commonly reported barrier in our study as well (reported by 56.5 % of the sample). However, depending on the view that is elicited, research on barriers to physical activity for children with disabilities differ. For example, a systematic review on the topic demonstrates children to commonly cite personal reasons, while parents tend to focus on familial, social, and policy factors (Shields et al. 2012). Future research may want to utilize a qualitative approach in order to better understand the barriers children with ASD face that prevent them from engaging in PA. This may provide in depth information for researchers then to develop more effective strategies for families and schools that may help children with ASD to become more active.
In regards to screen time, this study revealed no significant difference between the children with ASD and the TD children on computer, video, and television use. Children in both groups reported spending the most time watching television, with children with ASD reporting to spend a mean of 121 and 150 min per day in comparison to the TD children who spent a mean of 91–120 min. Previous research has revealed screen-time behavior to be significantly higher for children with ASD in comparison to TD children. For example, Must et al. (2014), utilizing parental report, showed mean daily screen-time to be 2.5 hours for children with ASD, in comparison to 1.6 hours for TD children. Similarly, Mazurek and Wenstrup (2013) compared screen-time between siblings with and without ASD revealing that children with ASD spent more time in screen-based activities per day than TD children.
Several factors are proposed as contributors to the increased likelihood of children with ASD to engage in screen time activities. Nally et al. (2000) found that television and video games served as a means to calm the child with ASD, as reported by parents. In addition, children with ASD are visually orientated. This characteristic might make screen viewing particularly appealing. Finally, the social deficits experienced by children with ASD may result in a reluctance to engage in play and sports that are often socially demanding. This aversion to group games, may lead to a preference for individual activities such as television viewing and video games, and in particular, non-social screen-based activities of which children with ASD choose to participate in (Mazurek et al. 2012). It has been showed (Graf et al. 2009) that TD children can increase energy expenditure using exergames. Exergaming has also shown to provide fitness games for children with intellectual and developmental disabilities (Lotan et al. 2009). Future research must continue to assess how parents can use screen-based media to motivate their children with ASD to engage in increased amounts of MVPA. The behavioral, cognitive, and social benefits of exergaming must also be explored for this population.
In the US, the rates of overweight and obesity among children with ASD is higher than those of TD children (Curtin et al. 2010). For example, among a large clinical sample, Broder-Fingert et al. (2014) found higher rates of obesity among children with ASD (23.2 %) and Aspergers syndrome (25.3 %) compared to a TD control (6.3 %). To date, research outside of the US is limited to data representing a few countries: rates range from 31.5 % in China (Xia et al. 2010) to 52 % in the United Kingdom (Whiteley et al. 2004). To the knowledge of the authors, the current study is the first to examine overweight and obesity rates for children with ASD in Ireland. Our Chi square analyses showed there was no relationship between being overweight and having an ASD diagnosis, however rates of overweight and obesity among the sample with ASD were higher than the TD control, with 22 children being overweight or obese (34.9 %), compared to 18 children (24.7 %) in the TD group. This difference did not reach statistical significance. Various factors are proposed for the difference in overweight prevalence among individuals with ASD, including restricted food preferences (Schreck et al. 2004), lower physical activity levels (Pan 2008; Rimmer et al. 2010), and medication use associated with weight gain (Esbensen et al. 2009). Research by Corvey et al. (2016), using data from the 2011–2012 National Survey of Children’s Health indicate that ASD was not independently related to obesity when medication use and the presence of secondary conditions were taken into account. In the current study, overweight and obesity rates did not significantly differ between the sample with and without comorbidities. Future research should examine the factors associated with weight status among children with ASD in Ireland, examining individual (including ASD severity levels), social and environmental factors.
Limitations and Recommendations
This study overcomes a number of limitations of past research (Corvey et al. 2016) on this topic including a relatively large sample size, use of a comparison group, and involvement of children from an unresearched geographical area. However, several limitations should be stated. First, this study utilized a variety of self-report measures. Self-report may be prone to recall error and bias, and research has demonstrated social desirability to compromise the validity of self-report use in measuring physical activity (Dishman et al. 2005). However, due to the large number of questionnaires used in the data collection, the effect of social-desirability for the questions of interest for this study will be minimized. The use of self-report measures presents another challenge for the measurement of physical activity for children with ASD. Past research (Bandini et al. 2013), has demonstrated that physical activity participation as measured by accelerometery was not associated with parental reports of the child’s activity. The authors proposed that this may be due to the failure for the parent to report activities such as pacing, spinning, or other motor movements commonly observed in children with ASD. It is possible that the children with ASD in this study engaged in similar movements that went unidentified due to the self-report nature of the data. Future research should seek to extend this research by using objective data collection methods. In addition, because of the nature of the nationally representative data collection procedure, it was not possible to confirm the ASD diagnosis, or establish severity levels of the children in this study. Future research should seek to examine PA and screen time levels by the severity of ASD, which will help to better tailor future interventions for this population.
Conclusion
There is a growing body of research on physical activity, screen-time and overweight status of individuals with ASD; results remain ambiguous, and are limited by a lack of comparison groups, constrained geographical areas, small samples sizes, and reliance on self or parent report data. The current study contributes to the literature on this topic, revealing lower levels of physical activity among children with ASD, and higher levels of TV watching, compared to a TD control. Future interventions to increase PA and decrease screen time in children with ASD should be tailored to this population, as results demonstrated differences in activity behaviors among children with ASD and TD children.
References
Ayvazoglu, N. R., Kozub, F. M., Butera, G., & Murray, M. J. (2015). Determinants and challenges in physical activity participation in families with children with high functioning autism spectrum disorders from a family systems perspective. Research in Developmental Disabilities, 47, 93–105. doi:10.1019/j.ridd.2015.08.015.
Bandini, L. G., Gleason, J., Curtin, C., Lividini, K., Anderson, S. E., Cermak, S. A., ... & Must, A. (2013). Comparison of physical activity between children with autism spectrum disorders and typically developing children. Autism, 17(1), 44–54.
Blanchard L. T., Gurka M. J., & Blackman J. A. (2006). Emotional, developmental, and behavioral health of American children and their families: A report from the 2003 National Survey of Children’s Health. Pediatrics, 117(6), e1202–e1212.
Cadogan, S., Keane, S., & Kearney, P. (2014). The effects of individual, family and environmental factors on physical activity levels in children: A cross-sectional study. BMC Pediatrics, 14, 107. doi:10.1186/1471-2431-14-107.
Centers for Disease Control and Prevention (2014). State indicator report on physical activity, 2014 (p. 2014). Atlanta, GA: U.S. Department of Health and Human Services.
Cole, T. J., Bellizzi, M. C., Flegal, K. M., & Dietz, W. H. (2000). Establishing a standard definition for child overweight and obesity worldwide: International survey. British Medical Journal, 320(7244), 1240–1243.
Corvey, K., Menear, K. S., Preskitt, J., Goldfarb, S., & Menachemi, N. (2016). Obesity, physical activity and sedentary behaviors in children with an autism spectrum disorder. Maternal & Child Health Journal, 20, 466–476. doi:10.1007/s10995-015-1844-5.
Currie C. et al. (2012). Social determinants of health and well-being among young people. Health behavior in school-aged children (HBSC) study: International report from the 2009/2010 survey. Copenhagen: WHO Regional Office for Europe.
Curtin, C., Anderson, S. E., Must, A., & Bandini, L. (2010). The prevalence of obesity in children with autism: A secondary data analysis using nationally representative data from the National Survey of Children’s Health. BMC Pediatrics, 10(11).
Dishman, R. K., Motl, R. W., Sallis, J. F., et al. (2005). Self-management strategies mediate self-efficacy and physical activity. American Journal of Preventive Medicine, 29, 10–18. doi:10.1016/j.amepre.2005.03.012.
Esbensen, A. J., Greenberg, J. S., Seltzer, M. M., & Aman, M. G. (2009). A longitudinal investigation of psychotropic and non-psychotropic medication use among adolescents and adults with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39, 1339–1349.
Fakhouri THI, Hughes, J. P., Burt, V. L., et al. (2014). Physical activity in U.S. youth aged 12–15 years, 2012. NCHS data brief, no. 141. Hyattsville, MD: National Center for Health Statistics.
Godin, G., Jobin, J., & Bouillon, J. (1986). Assessment of leisure time exercise behavior by self-report: A concurrent validity study. Canadian Journal of Public Health, 77, 359–361.
Graf, D. L., Pratt, L. V., Hester, C. N., & Short, K. R. (2009). Playing active video games increases energy expenditure in children. Pediatrics, 124(2), 534–540.
Han, J. C., Lawlor, D. A., & Kimm, S. Y. (2010). Childhood obesity. Lancet, 375, 1737–1748. doi:10.1016/S0140-6736(10)60171-7.
Health Service Executive (2012). National review of autism services: Past, present and way forward. Retrieved from http://www.fedvol.ie/_fileupload/Next%20Steps/autismreview2012.pdf.
Jimenez-Pavon, D., Kelly, J., & Reilly, J. J. (2010). Associations between objectively measured habitual physical activity and adiposity in children and adolescents: Systematic review. International Journal of Pediatric Obesity, 5(1), 3–8. doi:10.3109/17477160903067601.
Kim, Y., Conners, R. T., Hart, P. D., Kang, Y. S., & Kang, M. (2013). Association of physical activity and body mass index with metabolic syndrome among US adolescents with disabilities. Disability and Health Journal, 6, 253–259.
Laurson, K. R., Lee, J. A., Gentile, D. A., Walsh, D. A., & Eisenmann, J. C. (2014). Concurrent associations between physical activity, screen time, and sleep duration with childhood obesity. ISRN Obesity, 2014, 1–6. doi:10.1155/2014/204540.
Lee, L. C., Harrington, R. A., Louie, B. B., & Newschaffer, C. J. (2008). Children with autism: Quality of life and parental concerns. Journal of Autism and Developmental Disorders, 38(6), 1147–1160.
Lindsay, R. S., Hanson, R. L., Roumain, J., Ravussin, E., Knowler, W. C., & Tataranni, P. A. (2001). Body mass index as a measure of adiposity in children and adolescents: Relationship to adiposity by dual energy X-ray absorptiometry and to cardiovascular risk factors. Journal of Clinical Endocrinology and Metabolism, 86, 4061–4067.
Lotan, M, Yalon-Chamovitz, S., & Weiss, P. L. T. (2009). Improving physical fitness of individuals with intellectual and developmental disability through a virtual reality intervention program. Research in Developmental Disabilities, 30(2), 229–239.
Mazurek, M. O., & Wenstrup, C. (2013). Television, video game and social media use among children with ASD and typically developing siblings. Journal of Autism and Developmental Disorders, 43, 1258–1271. doi:10.1007/s1083-012-1659-9.
Mazurek M. O., Shattuck P. T., Wagner M. & Cooper B. P. (2012). Prevalence and correlates of screen-based media use among youths with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(8), 1757–1767.
Memari, A. H., Ghaheri, B., Ziaee, V., Kordi, R., Hafizi, S., & Moshayedi, P. (2013). Physical activity in children and adolescents with autism assessed by triaxial accelerometry. Pediatric Obesity, 8, 150–158. doi:10.1111/j.2047-6310.2012.00101.x.
Murray, A., McCrory, C., Thorton, M., Williams, J., & Quail, A. (2011). Growing up in Ireland: Design, instrumentation and procedures for the child cohort. Department of Children and Youth Affairs. Dublin: Government Publications.
Must, A., Phillips, S., Curtin, C., Anderson, S., Maslin, M., Lividini, K., & Bandini, L. (2014). Comparison of sedentary behaviors between children with autism spectrum disorders and typically developing children. Autism, 18(4), 376–384. doi:10.1177/1362361313479039.
Must, A., Phillips, S., Curtin, C., & Bandini, L. G. (2015). Barriers to physical activity in children with autism spectrum disorders: Relationship to physical activity and screen time. Journal of Physical Activity & Health, 12, 529–534. doi:10.1123/jpah.2013-0271.
Nally, B., Houlton, B., & Ralph, S. (2000) Researches in brief: The management of television and video by parents of children with autism. Autism, 4(3), 331–338.
Obrusnikova, I., & Cavalier, A. R. (2011). Perceived barriers and facilitators of participation in after-school physical activity by children with autism spectrum disorders. Journal of Developmental and Physical Disabilities, 23(3), 195–211.
Pan, C. Y. (2008). Objectively measured physical activity between children with autism spectrum disorders and children without disabilities during inclusive recess settings in Taiwan. Journal of Autism and Developmemtal Disorders, 38, 1292–1301.
Pan, C. Y., Hus, P. J., Chung, I. C., Hung, C. S., Liu, Y. J., & Lo, S. Y. (2015). Physical activity during the segmented school day in adolescents with and without autism spectrum disorders. Research in Autism Spectrum Disorders, 15–16, 21–28. doi:10.1016/j.rasd.2015.04.003.
Rimmer, J. H., Yamaki, K., Lowry, B. M., et al. (2010). Obesity and obesity-related secondary conditions in adolescent with intellectual/developmental disabilities. Journal of Intellectual Disability Research, 54, 787–794.
Sallis, J. F., Buono, M. J., Roby, J. J., Micale, F. G., & Nelson, J. A. (1993). Seven-day recall and other physical activity self-reports in children and adolescents. Medicine and Science in Sports and Exercise, 25, 99–108.
Sandt, D. D. R., & Frey, G. C. (2005). Comparison of physical activity levels between children with and without autistic spectrum disorders. Adapted Physical Activity Quarterly, 22, 146–159.
Schreck, K. A., Williams, K., & Smith, A. F. (2004). A comparison of eating behaviors between children with and without autism. Journal of autism and developmental disorders, 34(1), 433–438.
Shields, N., Synnot, A. J., & Barr, M. (2012). Perceived barriers and facilitators to physical activity for children with disability: A systematic review. British Journal of Sports Medicine, 46(14), 989–997.
Smith, B. J., Grunseit, A., Hardy, L. L., King, L., Wolfenden, L., & Milat, A. (2010). Parental influences on child physical activity and screen viewing time: A population based study. BMC Public Health, 10(593), 1–11. doi:10.1186/1471-2458-10-593.
Srinivasan, S. M., Pescatello, L. S., & Bhat, A. N. (2014). Current perspectives on physical activity and exercise recommendations for children and adolescents with autism spectrum disorders. Physical Therapy, 94(6), 875–889.
Starkoff, B. E., Petosa, R. L., Balk, E. K., Eneli, I. U., Bonny, A. E., Hoffman, R. P., & Devor, S. T. (2014). Sedentary and physical activity habits of obese adolescents. American Journal of Health Education, 45(6), 335–341. doi:1080/19325037.2014.945669.
Tyler, K., MacDonald, M., & Menear, K. (2014). Physical activity and physical fitness of school-aged children and youth with autism spectrum disorder. Autism Research and Treatment, 2014, 1–6.
Wachob, D., & Lorenzi, D. G. (2015). Brief report: Influence of physical activity on sleep quality in children with autism. Journal of Autism & Developmental Disorders, 45, 2641–2646. doi:10.1007/s10803-015-2424-7.
Whiteley, P., Dodou, K., Todd, L., & Shattock, P. (2004). Body mass index of children from the United Kingdom diagnosed with pervasive developmental disorders. Pediatrics International, 46(5), 531–533.
Wilson, P., Haegele, J. A., & Zhu, X. (2016). Mobility status as a predictor of obesity, physical activity, and screen time use among children aged 5 to 11 years in the United States. Journal of Pediatrics, 176, 23.e1–29.e1.
Xia W, Zhou Y, Sun C, et al. (2010). A preliminary study on nutritional status and intake in Chinese children with autism. European Journal of Pediatrics, 169, 1201–1206.
Acknowledgments
No grants or financial support were involved in the completion of this study. The authors would like to acknowledge the Irish Department of Children and Youth Affairs (DCYA) and Ireland’s Central Statistics Office (CSO) for the collection of the data.
Author Contributions
All authors contributed to the writing of the manuscript, and Sean Healy completed the analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Healy, S., Haegele, J.A., Grenier, M. et al. Physical Activity, Screen-Time Behavior, and Obesity Among 13-Year Olds in Ireland with and without Autism Spectrum Disorder. J Autism Dev Disord 47, 49–57 (2017). https://doi.org/10.1007/s10803-016-2920-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-016-2920-4