Abstract
Sensory reactivity is a new DSM-5 criterion for autism spectrum disorder (ASD). The current study aims to validate a clinician-administered sensory observation in ASD, the Sensory Processing Scale Assessment (SPS). The SPS and the Short Sensory Profile (SSP) parent-report were used to measure sensory reactivity in children with ASD (n = 35) and typically developing children (n = 27). Sixty-five percent of children with ASD displayed sensory reactivity symptoms on the SPS and 81.1 % on the SSP. SPS scores significantly predicted SSP scores. We next identified the five SPS tasks that best differentiated groups. Our results indicate that a combination of parent-report and at least the five most differentiating observational tasks may be most sensitive in identifying the presence of sensory reactivity issues.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the major changes to the criteria for autism spectrum disorder (ASD) in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is the addition of sensory reactivity symptoms to the restricted and repetitive behavior domain. Specifically, “hyper- or hypo-reactivity to sensory input or unusual interest in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movements)”(American Psychiatric Association 2013). Hyper-reactivity in the DSM-5 is characterized as an “adverse responses to stimuli”, hypo-reactivity as an “indifference” to sensory stimuli, and unusual interest as “fascination with stimuli” or sensation seeking. The definition and nomenclature for sensory reactivity varies greatly across professional disciplines and includes terms such as sensory over-responsivity (Schoen et al. 2008), enhanced perceptual functioning (Mottron et al. 2006), tactile defensiveness (Baranek et al. 1997; Goldsmith et al. 2006), sensory integration disorder and hyper-responsivity (Ayres and Tickle 1980). To be consistent with the DSM-5, we will use the term sensory reactivity to refer to responses to sensory stimuli in the environment.
Methodology for measuring sensory reactivity also varies across clinical and research fields. There are a wide range of sensory reactivity measures including questionnaires and observational assessments. Results from autism studies indicate that 60–90 % of individuals with ASD show sensory reactivity issues on parent- or self-reports (Lane et al. 2011; Tomchek and Dunn 2007). The Short Sensory Profile (SSP) (Dunn 1999; Lane et al. 2011; Tomchek and Dunn 2007) is a validated and standardized parent-report questionnaire that measures sensory reactivity by assessing the frequency of behaviors and responses towards sensory stimuli (Eeles et al. 2013; Lane et al. 2011; Tomchek and Dunn 2007). Differences in the SSP between individuals with and without ASD have been confirmed cross-culturally (Cheung and Siu 2009) and are evident across the lifespan (Kern et al. 2007a). There are several other sensory questionnaires, such as the Sensory Processing Inventory, which examines independent sensory domains (vision, hearing, and touch) (Schoen et al. 2008, 2014) and was originally developed for children with sensory processing disorders. The Sensory Experiences Questionnaire is another parent rating scale, which investigates sensory patterns such as hyper- and hypo-reactivity in children with and without ASD (Baranek et al. 2006). Other validated questionnaires include the Sensory Processing Measure (SPM), which is a parent-or-teacher rating scale that measures sensory functioning in school-aged children (Boyd et al. 2009). In general, sensory questionnaires are considered valuable screening tools for sensory issues and have the advantage of being low cost and easy to administer (Hoyle et al. 2001). However, retrospective parent- or caregiver- reports are subject to recollection bias and inaccurate responses (Hoyle et al. 2001). Direct clinician-administered observational assessments of sensory reactivity may provide greater objectivity and improved sensitivity and specificity.
The Sensory Processing Scale Assessment (SPS; previously called “SenSOR”) (Schoen et al. 2008, 2014) is a clinician-administered observation tool, which examines several senses, including vision, hearing and touch. The SPS identifies sensory hyper-reactivity, hypo-reactivity or seeking behaviors in children and adults (Schoen et al. 2008). Other sensory observation tools also exist, including the Sensory Integration and Praxis Tests (SIPT) (Ayres and Tickle 1980; Ayres 1989) the Sensory Processing Assessment for Young Children (SPA) (Patten et al. 2013), the Tactile Defensiveness and Discrimination Test—Revised (TDDT-R) (Baranek and Berkson 1994) and the Infant Test of Sensory Functioning (Boyd et al. 2010; Eeles et al. 2013). The SPA for example measures sensory hyper- and hypo-reactivity to novel and unexpected sensory stimuli in children as young as 9 months up to 6 years (Baranek et al. 2007). While other observations focus on just one sense, the SPS is unique in that it allows for clinician observation of symptoms included in the DSM-5 criteria for ASD of hyper-reactivity, hyporeactivity and seeking behaviors in multiple sensory domains.
In summary, despite the fact that sensory reactivity is widespread in ASD and causes substantial impairment in social functioning and adaptive behavior (Boyd et al. 2009; Hilton et al. 2010; Pfeiffer et al. 2005), there is no consensus on how to best measure sensory reactivity. While parent-report questionnaires have been widely used, there is a need for more objective direct clinical assessment as well. The goal of the current study is to use the SPS to capture hyper- and hypo-reactivity to sensory stimuli and sensation seeking behaviors across multiple sensory modalities for children with ASD and to (1) examine the reliability of the SPS in an ASD sample, (2) examine convergent validity of the SPS relative to the SSP, and (3) determine which SPS items were most informative in order to simplify the SPS and optimize its use within this population.
Methods
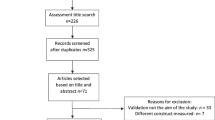
Participants were recruited as part of ongoing studies at the Seaver Autism Center for Research and Treatment at the Icahn School of Medicine at Mount Sinai. The Mount Sinai Institutional Review Board approved the current study. Informed consent was obtained from all parents/guardians and assent was obtained from participants over the age of seven when appropriate.
Participant Characteristics
Thirty-five children with ASD and 27 typically developing (TD) controls participated in this study. The ASD group (28 males; mean age 8.7, SD 2.8, range 4–14; mean IQ 103.1, SD 16.6, IQ range 80–132) and the TD group (12 males; mean age 9.5 years, SD 3.2, range 5–16; mean IQ 109.2, SD 13.6, IQ range 90–128) did not differ by age (p = .61) or IQ (p = .21). Cognitive functioning was measured using the Wechsler Abbreviated Scale of Intelligence (Wechsler 1999). ASD diagnoses were determined based on the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) (Lord et al. 2012), the Autism Diagnostic Interview- Revised (ADI-R) (Lord et al. 1994), psychiatric evaluation, and DSM-5 criteria. One participant out of original 36 participants with ASD was excluded because of failure to meet on ADOS-2 and ADI-R. All remaining 35 children with ASD included in the analysis met ADOS-2, ADI-R, and DSM-5 criteria. In addition, the Autism Spectrum Quotient (AQ) was used to screen for ASD traits in the TD group (Auyeung et al. 2008; Baron-Cohen et al. 2006; Bastiaansen et al. 2011). The AQ is a 50-item questionnaire with five subscales measuring autistic traits; social skills, attention switching, attention to detail, imagination, and communication (Auyeung et al. 2008; Baron-Cohen et al. 2006; Bastiaansen et al. 2011). Results from the AQ have been replicated cross-culturally (Hoekstra et al. 2008) and across different age groups (Auyeung et al. 2008; Baron-Cohen et al. 2006) with good test–retest reliability. A cut-off of above 26 on a scale of 0–50 is indicative of clinically significant ASD traits. All participants in the TD group scored below the cut-off for ASD.
Sensory Questionnaires
Short Sensory Profile (SSP)
The Short Sensory Profile (SSP) was used to measure parent-reported sensory reactivity. The SSP is derived from the longer Sensory Profile, a 125-item questionnaire, which was standardized on a sample of over 1000 typically developing children (Dunn 1999). The SSP consists of 38-items in which parents rate how often their child shows a particular behavior (e.g., “prefers to be in the dark”), using a five-point Likert scale that ranges from always (1) to never (5). Higher scores reflect more typical behavior. The SSP has high internal reliability (.90–.95) (Dunn 1999) and shows sensory differences in up to 90 % of children and adults with ASD compared to controls (Crane et al. 2009; Dunn et al. 2002; Kern et al. 2007b; Kientz and Dunn 1997; Leekam et al. 2007; Tomchek and Dunn 2007; Watling et al. 2001; Wiggins et al. 2009). Since the SSP is one of the most widely used sensory measures in children with ASD, convergent validity with the SSP and item reduction analysis was conducted to examine the psychometric properties of the SPS in children with ASD.
Sensory Processing Scale Assessment (SPS)
The Sensory Processing Scale (SPS) was developed for children with sensory reactivity difficulties and shows strong reliability (scale reliability >.90) (Schoen et al. 2014).
Fifteen structured games are played during the SPS to establish whether a participant displays sensory hyper-reactivity, hypo-reactivity or craving/seeking behaviors. Examples of tactile tasks include the “Paint your arm” game in which participants paint their arm with a feather, a brush and a rough sponge, and the “Goo” game in which participants remove 2 plastic animals from goo. Visual tasks include tasks such as the “Sparkle” game, which requires participants to observe a spinning sparkle wheel for 20 s, and the “Round and Round” game in which participants observe a black and white spinning wheel move for 20 s. One example of an auditory task is the “Orchestra” game in which participants are asked to play along to music and make noise with certain instruments. A trained administrator (T.T.) conducted and scored the SPS (Schoen et al. 2008, 2014).
Within each sensory domain (vision, hearing and touch), a Global Clinical Impression (GCI) of sensory symptoms or typical behavior was obtained based on a behavioral scoring system (Schoen et al. 2014). Sensory hyper-reactivity was identified when the following behaviors were observed: adverse response, discomfort, worries and/or avoidance. Such participants displayed worry during the “Paint your arm” game by asking whether a stimulus would hurt. Discomfort, such as grimacing or flinching, was also observed during the “Goo” game. Sensory hypo-reactivity was identified when participants did not respond to sensory stimuli or were slow to respond; for example, not noticing the roughness of the sponge during the “Paint your arm” game. Sensory seeking behavior was identified when a child continued to use test items after tasks were completed and/or was unable to disengage from sensory material, such as continuing to spin the sparkle wheel in the “Sparkle” game for an inappropriate length of time. Typical behavior was noted when the participant appeared comfortable, appropriately handled, and was aware of sensory material as requested while completing each task within a reasonable time frame.
Data Analysis
SPSS 22 was used to analyze the data. To investigate group differences ANOVA and Chi-square tests were conducted. Regression analysis and inter-rater reliability (IRR) was used to compare measures and to quantify overlap between them. Item distribution was used to identify the five most informative SPS tasks in participants with ASD (Rust and Golomok 1999).
Results
All participants’ parents were able to complete the parent-report questionnaires. All TD participants and 97 % of participants with ASD were able to complete the SPS.
Sensory Questionnaire: Short Sensory Profile (SSP)
Using ANOVA with group as a fixed factor and SSP total scores as the dependent variable, children with ASD had lower SSP total scores [F(1) = 26.2, p = .0001] than TD children. Levene’s test showed that the variances were equal for both groups [F(1) = 1.57, p = .21]. For the SSP, the manual classifies children as having “definite differences” in sensory reactivity, if the scores fall two standard deviations away from the mean (see Table 1). Eighty-one percent (81.1 %) of children with ASD were identified as having “definite” sensory reactivity symptoms according to the SSP.
Sensory Processing Observation (SPS)
Chi-square analysis showed a significant difference in the distribution of SPS scores across groups, with children in the ASD group exhibiting greater sensory reactivity symptoms on the SPS (χ 2 = 23.5, p = .0001) (Table 1). The SPS allowed investigation of sensory subtypes in accordance with the DSM-5. In the visual domain, the most common sensory symptom for children with ASD was sensory seeking (33 %). In both the auditory (15 %) and tactile (33 %) domains, the most common sensory symptom for children with ASD was hyper-reactivity (see Table 2).
Inter-Rater Reliability
To calculate inter-rater reliability, both assessments were treated as independent ratings and the absolute agreement was calculated by dividing the number of agreements by the total number of possible agreements. The SPS and SSP had an IRR of .74, meaning they agreed 74 % of the time. Results from the SSP combined with the SPS indicated that 65 % of children with ASD were classified as having definite sensory reactivity symptoms on both measures. No participants in the typically developing group fell into this category when both questionnaire and observation data were included in the analysis.
Correlations and Regression Analysis
Correlation analysis showed that age, gender, and IQ were not significantly correlated with any dependent variables across groups (p > .05) and within each group (p > .05). A linear regression analysis with SSP as the dependent variable and SPS as the independent variable was conducted to examine the relationship between the two measures. Scores on the SPS significantly predicted scores on the SSP across groups [R = .43, R 2 = .19, F(1) = 13.50, p = .001].
Item Distribution Analysis and Item Reduction
An item distribution analysis was conducted for the SPS. Items for which over 75 % of participants scored the same were excluded as they were not informative (Rust and Golomok 1999). The analysis identified five critical items: Sparkles (vision), Round-and-Round (vision), Goo game (touch), Paint your Arm (touch) and Orchestra (hearing). The IRR between the full SPS and the five-item version is .91.
Discussion
Since sensory reactivity symptoms are now part of the DSM-5, it is crucial to establish consensus on how to measure sensory reactivity for both clinical and research purposes. We set out to test the use of a clinician-administered sensory observation tool, the SPS, compared to a validated parent-report questionnaire, the SSP. Nearly all (97 %) participants with ASD were able to complete the SPS, suggesting that this seems to be a feasible measure of sensory reactivity in verbal children with ASD. Further studies are underway to test feasibility of clinician-administered sensory observations for minimally verbal children. The current study also showed that a significant number of children with ASD (60–80 %) have sensory reactivity issues across measures. This is consistent with previous research showing that 60–90 % of individuals with ASD show sensory reactivity issues on parent- and self-report questionnaires (Ben-Sasson et al. 2007; Brown et al. 2001; Crane et al. 2009; Dunn et al. 2002; Kern et al. 2006).
Our current study confirmed differences for children with ASD on the SSP (Dunn 1999; Lane et al. 2011; Tomchek and Dunn 2007) as compared to TD children. On the SSP, 81 % of children with ASD fell into the category of definite differences, with scores two standard deviations away from the normed average. An advantage of integrating sensory questionnaires, such as the SSP, into clinical practice is to screen for sensory symptoms described in the DSM-5 criteria for ASD. Nonetheless, because questionnaires are subjective, the current study also set out to evaluate more objective clinician-administered measures of sensory reactivity.
This was the first study to use the SPS on a sample of children with ASD. Results showed that 65 % of the ASD sample displayed sensory issues compared to only 4 % of the TD sample. Specifically, 33 % of children with ASD showed visual seeking behaviors, 15 % showed auditory hyper-reactivity and 33 % showed tactile hyper-reactivity. Notably, these categories directly correspond to DSM-5 criteria. With respect to the TD group, our results are consistent with work on Sensory Processing Disorder showing that 5–16 % of otherwise TD children show sensory reactivity issues (Ahn et al. 2004; Miller et al. 2009). All TD children and nearly all children with ASD (94 %) successfully completed the SPS. Using item distribution inspection, we identified the five most differentiating tasks: two tactile tasks (Goo and Paint your Arm), two visual tasks (Sparkle and Round-and-Round) and one auditory task (Orchestra). These five tasks take about 10–15 min to administer for children with ASD. Thus, rather than using all 15 tasks, we propose using these five critical tasks when assessing sensory reactivity in children with ASD (Schoen et al. 2008). Future replication studies are important to further validate this finding.
The SSP combined with the SPS indicates that 65 % of children with ASD have definite sensory reactivity symptoms. None of the typically developing children fell into this category when the questionnaire and observation were combined, thus screening out participants who were likely incorrectly identified on the parent-report alone. Overall, results suggest that a combination of parent report questionnaires and clinician-administered observations may result in a highly specific approach to most accurately measure sensory reactivity.
Limitations
One limitation of the current study is the relatively small sample size. Despite this, we identified both group differences and an overlap across measures. Another limitation is the unequal gender ratio across groups with more male participants in the ASD group. It is important to also include female participants with ASD, as there is data to suggest that females with ASD have more sensory issues than males (Lai et al. 2011). Furthermore, our sample was limited to children who were verbal and had IQs ranging from 80 to 132. These results should be replicated in a larger sample, with younger children, including children who are minimally verbal and have intellectual disability. Future studies should also test the SPS in children with ASD compared to other clinical populations, such as children with Attention Deficit/Hyperactivity Disorder (ADHD).
Conclusion
This is the first study to test the use of a clinician-administered sensory observation, the SPS, in a sample of children with ASD. In summary, we show that a significant proportion of children with ASD have sensory reactivity abnormalities on different sensory measures. Parent reports and observations are important tools to screen for sensory reactivity issues and are feasible within the context of both clinical and research settings. Future research should focus on further development and validation of sensory reactivity measures for minimally verbal children (Patten et al. 2013). Additional research is also needed to establish a consensus about which measures should be used across disciplines and settings. Eventually, sensory reactivity subgroups may emerge to guide personalized therapies or to serve as biomarkers for treatment response. Based on our current results, we propose that a combination of a parent-report, such as the SSP, and at least the five most differentiating SPS observational tasks, would be the most sensitive and least burdensome method to alert clinicians and researchers to the presence of sensory reactivity issues.
References
Ahn, R. R., Miller, L. J., Milberger, S., & McIntosh, D. N. (2004). Prevalence of parents’ perceptions of sensory processing disorders among kindergarten children. American Journal of Occupational Therapy, 58(3), 287–293. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15202626.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC.
Auyeung, B., Baron-Cohen, S., Wheelwright, S., & Allison, C. (2008). The autism spectrum quotient: Children’s version (AQ-Child). Journal of Autism and Developmental Disorders, 38(7), 1230–1240. doi:10.1007/s10803-007-0504-z.
Ayres, A. J. (1989). Sensory integration and praxis test (SIPT). Los Angeles: Western Psychological Services.
Ayres, A. J., & Tickle, L. S. (1980). Hyper-responsivity to touch and vestibular stimuli as a predictor of positive response to sensory integration procedures by autistic children. Am J Occup Ther, 34(6), 375–381. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=6971048.
Baranek, G. T., & Berkson, G. (1994). Tactile defensiveness in children with developmental disabilities: Responsiveness and habituation. Journal of Autism and Developmental Disorders, 24(4), 457–471. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=7961330.
Baranek, G. T., Boyd, B. A., Poe, M. D., David, F. J., & Watson, L. R. (2007). Hyperresponsive sensory patterns in young children with autism, developmental delay, and typical development. American Journal of Mental Retardation, 112(4), 233–245. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17559291.
Baranek, G. T., David, F. J., Poe, M. D., Stone, W. L., & Watson, L. R. (2006). Sensory Experiences Questionnaire: Discriminating sensory features in young children with autism, developmental delays, and typical development. Journal Child Psychology Psychiatry, 47(6), 591–601. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16712636.
Baranek, G. T., Foster, L. G., & Berkson, G. (1997). Tactile defensiveness and stereotyped behaviors. American Journal of Occupational Therapy, 51(2), 91–95. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9124275.
Baron-Cohen, S., Hoekstra, R. A., Knickmeyer, R., & Wheelwright, S. (2006). The autism-spectrum quotient (AQ)-adolescent version. Journal of Autism & Developmental Disorders, 36, 343-350. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16552625.
Bastiaansen, J. A., Meffert, H., Hein, S., Huizinga, P., Ketelaars, C., Pijnenborg, M., & de Bildt, A. (2011). Diagnosing autism spectrum disorders in adults: The use of Autism Diagnostic Observation Schedule (ADOS) module 4. Journal of Autism and Developmental Disorders, 41(9), 1256–1266. doi:10.1007/s10803-010-1157-x.
Ben-Sasson, A., Cermak, S. A., Orsmond, G. I., Tager-Flusberg, H., Carter, A. S., Kadlec, M. B., & Dunn, W. (2007). Extreme sensory modulation behaviors in toddlers with autism spectrum disorders. American Journal of Occupational Therapy, 61(5), 584–592. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17944296.
Boyd, B. A., Baranek, G., Sideris, J. T., Poe, M. D., Watson, L. R., Patten, E., & Miller, H. (2010). Sensory features and repetitive behaviors in children with autism and developmental delays. Autism Research, 3, 78–87.
Boyd, B. A., McBee, M., Holtzclaw, T., Baranek, G. T., & Bodfish, J. W. (2009). Relationships among repetitive behaviors, sensory features, and executive functions in high functioning autism. Research in Autism Spectrum Disorders, 3(4), 959–966. doi:10.1016/j.rasd.2009.05.003.
Brown, C., Tollefson, N., Dunn, W., Cromwell, R., & Filion, D. (2001). The adult sensory profile: Measuring patterns of sensory processing. American Journal of Occupational Therapy, 55(1), 75–82. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11216370.
Cheung, P. P., & Siu, A. M. (2009). A comparison of patterns of sensory processing in children with and without developmental disabilities. Research in Developmental Disabilities, 30(6), 1468–1480. doi:10.1016/j.ridd.2009.07.009.
Crane, L., Goddard, L., & Pring, L. (2009). Sensory processing in adults with autism spectrum disorders. Autism, 13(3), 215–228. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19369385.
Dunn, W. (1999). The sensory profile manual. San Antonio: The Psychological Corporation.
Dunn, W., Myles, B. S., & Orr, S. (2002). Sensory processing issues associated with Asperger syndrome: A preliminary investigation. American Journal of Occupational Therapy, 56(1), 97–102. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11833406.
Eeles, A. L., Spittle, A. J., Anderson, P. J., Brown, N., Lee, K. J., Boyd, R. N., & Doyle, L. W. (2013). Assessments of sensory processing in infants: A systematic review. Developmental Medicine and Child Neurology, 55(4), 314–326. doi:10.1111/j.1469-8749.2012.04434.x.
Goldsmith, H. H., Van Hulle, C. A., Arneson, C. L., Schreiber, J. E., & Gernsbacher, M. A. (2006). A population-based twin study of parentally reported tactile and auditory defensiveness in young children. Journal of Abnormal Child Psychology, 34(3), 393–407. doi:10.1007/s10802-006-9024-0.
Hilton, C. L., Harper, J. D., Kueker, R. H., Lang, A. R., Abbacchi, A. M., Todorov, A., & LaVesser, P. D. (2010). Sensory responsiveness as a predictor of social severity in children with high functioning autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(8), 937–945. doi:10.1007/s10803-010-0944-8.
Hoekstra, R. A., Bartels, M., Cath, D. C., & Boomsma, D. I. (2008). Factor structure, reliability and criterion validity of the Autism-Spectrum Quotient (AQ): A study in Dutch population and patient groups. Journal of Autism and Developmental Disorders, 38(8), 1555–1566.
Hoyle, R. H., Harris, M. J., & Judd, C. M. (2001). Research methods in social relations (7th ed.). Belmont, CA: Wadsworth.
Kern, J. K., Garver, C., Carmody, T., Andrews, A., Trivedi, J. K., & Mehta, J. A. (2007a). Examining sensory modulation in individuals with autism as compared to community controls. Research in Autism Spectrum Disorders, 2(1), 85–94.
Kern, J. K., Trivedi, M. H., Garver, C. R., Grannemann, B. D., Andrews, A. A., Savla, J. S., et al. (2006). The pattern of sensory processing abnormalities in autism. Autism, 10(5), 480–494. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16940314.
Kern, J. K., Trivedi, M. H., Grannemann, B. D., Garver, C. R., Johnson, D. G., Andrews, A. A., et al. (2007). Sensory correlations in autism. Autism, 11(2), 123–134. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17353213.
Kientz, M. A., & Dunn, W. (1997). A comparison of the performance of children with and without autism on the Sensory Profile. American Journal of Occupational Therapy, 51(7), 530–537. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9242859.
Lai, M., Lombardo, M., Pasco, G., Ruigrok, A., Wheelwright, S., Sadek, S., et al. (2011). A behavioral comparison of male and female adults with high functioning autism spectrum conditions. PLoS One, 6(6), e20835. doi:10.1371/journal.pone.0020835.
Lane, A. E., Dennis, S. J., & Geraghty, M. E. (2011). Brief report: Further evidence of sensory subtypes in autism. Journal of Autism and Developmental Disorders, 41(6), 826–831. doi:10.1007/s10803-010-1103-y.
Leekam, S. R., Nieto, C., Libby, S. J., Wing, L., & Gould, J. (2007). Describing the sensory abnormalities of children and adults with autism. Journal of Autism and Developmental Disorders, 37(5), 894–910. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17016677.
Lord, C., Rutter, M., DiLavore, P. S., Risi, S., Gotham, K., & Bishop, D. (2012). Autism diagnostic observation schedule, second edition (ADOS-2) mannual (Part I): Modules 1–4. Torrance, CA: Western Psychological Services.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism diagnostic interview-revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7814313.
Miller, L. J., Nielsen, D. M., Schoen, S. A., & Brett-Green, B. A. (2009). Perspectives on sensory processing disorder: A call for translational research. Frontiers in Integrative Neuroscience, 3, 22. doi:10.3389/neuro.07.022.2009.
Mottron, L., Dawson, M., Soulieres, I., Hubert, B., & Burack, J. (2006). Enhanced perceptual functioning in autism: An update, and eight principles of autistic perception. Journal of Autism and Developmental Disorders, 36(1), 27–43. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16453071.
Patten, E., Ausderau, K. K., Watson, L. R., & Baranek, G. T. (2013). Sensory response patterns in nonverbal children with ASD. Autism Research and Treatment, 2013, 436286. doi:10.1155/2013/436286.
Pfeiffer, B., Kinnealey, M., Reed, C., & Herzberg, G. (2005). Sensory modulation and affective disorders in children and adolescents with Asperger’s disorder. American Journal of Occupational Therapy, 59(3), 335–345. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15969281.
Rust, J., & Golomok, S. (1999). Modern psychometrics: The science of psychological assessment (2nd ed.). London: Routledge.
Schoen, S., Miller, L. J., & Green, K. E. (2008). Pilot study of the Sensory Over-Responsivity Scales: Assessment and inventory. American Journal of Occupational Therapy, 62(4), 393–406. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18712002.
Schoen, S. A., Miller, L. J., & Sullivan, J. C. (2014). Measurement in sensory modulatin: The sensory processing scale assessment. The American Journal of Occupational Therapy, 68(5), 522–530.
Tomchek, S. D., & Dunn, W. (2007). Sensory processing in children with and without autism: A comparative study using the short sensory profile. American Journal of Occupational Therapy, 61(2), 190–200. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17436841.
Watling, R. L., Deitz, J., & White, O. (2001). Comparison of Sensory Profile scores of young children with and without autism spectrum disorders. The American Journal of Occupational Therapy, 55(4), 416–423. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11723986.
Wechsler, D. (1999). Wechsler abbreviated scale of intelligence. San Antonio, TX: The PsychologicalCorporation.
Wiggins, L. D., Robins, D. L., Bakeman, R., & Adamson, L. B. (2009). Brief report: Sensory abnormalities as distinguishing symptoms of autism spectrum disorders in young children. Journal of Autism and Developmental Disorders, 39(7), 1087–1091. doi:10.1007/s10803-009-0711-x.
Acknowledgments
Thanks to all participants for taking part in our research. Special thanks to the Seaver Autism Center team; especially Sarah Soffes, B.A., Lauren Bush, B.A., Jesslyn Jamison, B.A., Lilly Schwartz, B.A., Stacey Lurie, B.A. and John Servinskas, B.A. Also thanks to Michael Parides, Lucy Miller and Sarah Schoen. This work was supported by Grants from the Beatrice and Samuel A. Seaver Foundation. T.T. received funding from the Wallace Research Foundation, the Seaver Foundation and the Autism Science Foundation during the period of this work. A.K. received research support from the NIH, the Autism Science Foundation, the Seaver Foundation, Seaside Therapeutics, and Hoffmann-La Roche Pharmaceuticals.
Author Contributions
TT designed the study, analyzed the data, wrote the initial draft of the paper, and participated in revising the manuscript and addressing the reviewers’ comments. KB, AK and JDB helped with designing the study. TT, KB, PS, ATW, DH, MG, DG and AK helped with testing and data acquisition. All authors assisted with manuscript development and participated in revising the manuscript and addressing the reviewers’ comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Tavassoli, T., Bellesheim, K., Siper, P.M. et al. Measuring Sensory Reactivity in Autism Spectrum Disorder: Application and Simplification of a Clinician-Administered Sensory Observation Scale. J Autism Dev Disord 46, 287–293 (2016). https://doi.org/10.1007/s10803-015-2578-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-015-2578-3