Abstract
We examined comorbid psychiatric and neurodevelopmental disorders in fifty adult males (mean age 30 years) with Asperger syndrome (AS) diagnosed in childhood and followed up prospectively for almost two decades (13–26 years). Only three of the 50 men had never met criteria for an additional psychiatric/neurodevelopmental diagnosis and more than half had ongoing comorbidity (most commonly either ADHD or depression or both). Any psychiatric comorbidity increased the risk of poorer outcome. The minority of the AS group who no longer met criteria for a full diagnosis of an autism spectrum disorder were usually free of current psychiatric comorbidity. The high rate of psychiatric/neurodevelopmental comorbidities underscores the need for a full psychiatric/neurodevelopmental assessment at follow-up of males with AS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asperger syndrome (AS) is a relatively common disorder, affecting about .5 % of the general population of children (possibly about .8 % of the boys) (Gillberg and Gillberg 1989). It usually persists into early adulthood, and is still diagnosable according to stringent criteria in about 45 % of the male cases [and in another 25–30 % of male cases as other autism spectrum disorders (ASD)] around 30 years of age (Helles et al. 2015). It is currently subsumed under the ASD umbrella of the DSM-5 (APA 2013), where it is coded with the other clinical presentations of ASD, including the category that was previously separately coded as autistic disorder (AD) (APA 1994).
Co-existence with other named or separately coded psychiatric and physical disorders is the rule in ASD, at least in young children (Gillberg and Fernell 2014). This phenomenon is often referred to as “comorbidity” (Gillberg and Billstedt 2000), and has been dealt with in publications referring to early symptomatic syndromes eliciting neurodevelopmental clinical examinations (ESSENCE) (Gillberg 2010, 2014; Gillberg and Fernell 2014), in which it has been pointed out that a diagnosis of ASD in very young children almost always means that criteria for at least one other major (neurodevelopmental or physical) disorder are met. This has led to the introduction of the concept of autism plus (or ASD plus), which underscores the need for a holistic approach to assessment whenever a diagnosis of ASD (including AS) is made or considered (Gillberg and Fernell 2014). This approach would have to include a full screen for and consideration of all kinds of possible psychiatric diagnoses, including attention-deficit/hyperactivity disorder (ADHD), depression, anxiety disorders, psychosis, and suicidal behaviours.
There has been limited research into the psychiatric comorbidity of AS and other ASD, particularly in the adult population. The first study of AS comorbidity was published in 1998 and reported a 65 % rate of other psychiatric disorders in a sample of 35 children and adolescents (a few adults were also included) with a “primary” diagnosis of AS (Ghaziuddin et al. 1998).
Mattila et al. (2010) found that 37 of 50 school age children with AS or “high-functioning autism” had at least one other (usually two or more) psychiatric disorder. Some of these associated disorders (including depression) were associated with considerably poorer adaptive functioning. A controlled study of depressive symptoms in children and adolescents with (and without) AS or “high functioning autism” revealed such symptoms to be associated with poorer global functioning (Mazzone et al. 2012). Mukaddes et al. (2010) studied 37 individuals (32 male) with AS and a mean age of about 11 years, finding that 94 % of them had at least one additional psychiatric diagnosis based on results obtained using the Kidddie-SADS. The most common types of problems, as in the Mattila et al. study were “behaviour disorders” and “mood disorders”. There is conflicting evidence or complete lack of systematic studies regarding the association, if any, of AS with psychosis and suicidal behaviour in children and adolescents (Skokauskas and Gallagher 2010).
With one exception there does not appear to have been any prior systematic study of well-defined “psychiatric disorder” in adults with AS (Lugnegård et al. 2011). The only study published of this kind showed very high rates of associated psychiatric disorder, and depression had been present in 80 % during the lifetime of individuals with AS with a mean age of about 30 years. Interestingly, some studies have shown a high rate of AS and other ASD in schizophrenic psychoses but not a correspondingly high rate of psychosis in AS (Unenge Hallerback et al. 2012). This has led to speculation that when AS is recognized and psychoeducation provided from a young age the risk of “developing” psychosis is reduced, whereas in cases where the psychosis is recognized first and the connection with AS only later, the preventive effect of early psychoeducation has not been in place. Even though these conclusions admittedly are theoretical rather than supported by prospective empirical studies, they draw attention to the possibility that early intervention for the whole spectrum of problems that are usually attached to any of the diagnoses within the ESSENCE might have some very beneficial effect.
There have also been studies of comorbidity in adult populations with other normal range intelligence ASDs than AS. High rates of comorbid diagnoses, especially high rates of ADHD, mood and anxiety disorders, have been reported (Hofvander et al. 2009; Joshi et al. 2013; Buck et al. 2014).
The aim of the present study was to examine the incidence and lifetime prevalence of psychiatric and neurodevelopmental disorders in a clinical cohort of males with AS diagnosed according to the Gillberg criteria in childhood and followed prospectively over two decades.
Secondary aims were to assess if global functioning is affected by psychiatric and/or neurodevelopmental comorbidity and if there are differences regarding comorbidity rates in relation to ASD diagnostic stability.
Methods
Participants
A group of 100 males with AS (Gillberg 1991; Gillberg and Gillberg 1989), who had been diagnosed at the Child Neuropsychiatric Clinic (CNC) in Gothenburg between 1985 and 1999 (Time 0/T0), 76 of whom had been followed up in 2002–2003 (Time 1/T1), were targeted for a further in-depth follow-up in 2011–2013 (Time 2/T2). The results of the T0 study and the follow-up at T1 have been published previously (Cederlund et al. 2008; Gillberg and Cederlund 2005). At T0 (i.e. before the year 2000) all children in the Gothenburg region raising suspicion of suffering from ASD, AD or AS were referred to the CNC for assessment. The 100 males were considered representative of all males diagnosed with AS in Gothenburg during the 1980’s and 1990’s (Cederlund and Gillberg 2004; Gillberg and Cederlund 2005). Initially, there had been a plan to also include 30 females, but only 7 cases were found to meet the inclusion criteria during the 15-year period covered, and because of the lack of statistical power, females were not included in the T0 study.
The original criteria for inclusion in the longitudinal study were as follows: (1) consecutive boys under age 16 years with a diagnosis of AS according to Gillberg’s criteria 1 established at the CNC from 1985–1999, and (2) Full Scale IQ (FSIQ) >70 at T0. The criteria for inclusion in the first follow-up (T1) were the same plus (3) age >16 years at T1 and (4) more than 5 years having elapsed since original diagnosis.
In Helles et al. (2015) a thorough analysis of attrition was presented. Of the 100 males at T0, 76 participated at T1 and 50 at T2, 47 participated in all three studies. No significant differences were found between T2 participants (n = 50) and non-participants (n = 50) regarding the T0 variables: age at diagnosis, FSIQ and verbal IQ (VIQ) on the WISC-III (Wechsler Intelligence Scale for Children—3rd edition), Autism Spectrum Screening Questionnaire (ASSQ) total scores, parents academic level, age of walking onset, or late speech development (speech before the age of 3). However, T0 performance IQ (PIQ) on the WISC-III was higher in the participating group (T2 group M = 98.1, non-participants at T2 group M = 91.1, Z = −2.19, p = . 029). When comparing the T2 group (n = 50) with those who participated at T1 but not at T2 (n = 26), we found no differences regarding the background variables mentioned above, except for PIQ which differed at T0 between the two groups (T2 participants M = 98.1, T1 but not T2 participants M = 90.2, Z = –2.02, p = .043). No significant differences at T1 were found between the T2 group and those participating only at T1 regarding VIQ on the WAIS-III, ASDI total scores, GAF scores, age, or clinical diagnosis at T1. However, differences were found between the T2 group and those participating at T1 but not T2 regarding FSIQ (T2 group M = 107.6, T1 not T2 group M = 97.0, Z = −2.77, p = .006), and PIQ on the WAIS-III (T2 group M = 106.3, T1 not T2 group M = 92.4, Z = −3.45, p = .001) at T1.
The mean age at T0 (n = 100) was 11.4 years (SD 3.8 years), at T1 21.8 years (SD 4.5 years) and at T2 30.2 years (SD 5.0 years, range 23–43 years). In Helles et al. (2015) results showed that 56 % of the individuals in the cohort no longer met full Gillberg criteria for AS in adult life, but a vast majority (78 %) still met criteria for any DSM-IV pervasive developmental disorder (ASD) diagnosis [AS (44 %), AD (18 %) or PDD-NOS (16 %)]. When using the new DSM-5, 38 % no longer meet full criteria for an ASD diagnosis.
There are some distinct differences between Gillberg’s and DSM-IV’s AS criteria. Gillberg and DSM-IV criteria both require marked social deficits and special interest, rituals or other stereotyped behaviours, but Gillberg criteria also require pedantic, superficially perfect and/or stereotyped expressive speech and literal understanding of language with odd prosody, non-verbal communication deficits, and motor clumsiness. Gillberg’s criteria allow for early speech and developmental difficulties and subnormal range IQ, whereas DSM-IV criteria require normal speech development and normal range IQ. Leekam et al. (2000) showed that Gillberg’s AS is, in fact, more closely related to AD than to AS according to the ICD-10/DSM-IV. The Leekam et al. study also showed that, if you rigidly adhere to the criterion of normal early development in terms of social and cognitive abilities (that is one of the foundations of the ICD-10 AS diagnosis), very few individuals with ASD (if any) actually really meet ICD-10 (or DSM-IV) criteria for AS.
Procedure
In the T2 study invitation letters were sent to 93 of the 100 men. They were then personally invited over the phone to take part in the study. Seven individuals were not contacted because they had previously (at T1) declared that they would not be interested in further participation in the study. Of the remaining 93 individuals in the study group, 1 had died since T1 (cause unknown), 35 declined to participate in the study, and 7 were unreachable. All participants at T2 gave written consent to participate in the study.
The 35 men who declined participation cited the following reasons: (1) no specific reason (n = 16), (2) felt they had no difficulties and did not want to be reminded of the diagnosis (n = 5), (3) felt misunderstood by society because of their diagnosis and were reluctant to talk about AS (n = 5), and (4) first agreed to participate in the study but missed/postponed their appointments on several occasions, and finally decided not to participate, because (a) it would be too stressful (n = 5), (b) they had changed their mind (n = 2) or (c) they had wanted to say no directly but had difficulties in doing so (n = 2). The seven participants who were unreachable had a home address (but not a telephone number) in official records, and did not reply to our several mail requests.
The research team comprised a psychiatrist and a clinical psychologist, both with extensive experience in the field of ASD and other developmental disorders. Data was collected during a 4–6 h visit to the Gillberg Neuropsychiatry Centre. The majority of the group (n = 46) were assessed at the Centre, one was assessed at home, two were interviewed over the phone, and one participant did not agree to be interviewed but allowed us to interview his parents. Diagnostic assessment and GAF scoring was made by the first author (ICG) in all cases with support from either the second (AH) or third (EB) author. Ethical approval was obtained from the Regional Ethical Approval Board in Gothenburg (reference: 508-10). All participants provided informed, written consent before participation.
Measures and Assessment Methods at T0
All individuals had been assessed by experienced clinicians working at the CNC at T0. Diagnosis of AS had been made using Gillberg’s criteria for AS (all also met DSM-IV/ICD-10 AS or AD symptom criteria). Medical records from T0 provided information of formal comorbid diagnoses at T0.
Measures and Assessment Methods at T1 and T2
Comorbid diagnosis assessed were as follows: ADHD (assessed at both T1 and T2), DCD (assessed only at T1), tic disorders (assessed only at T1), depressive disorders, including dysthymia and suicidal risks (assessed at both T1 and T2), anxiety disorder, including GAD, social phobia, panic disorder and specific phobias (assessed only at T2), OCD (assessed only at T2), bipolar disorder (assessed only at T2), psychosis (assessed only at T2). All diagnostic assessments were made by the first author (ICG) with support by either the second (AH) or third (EB) author.
Diagnosis of ADHD
The Adult ADHD Self-Report Scale (ASRS) (Kessler et al. 2007) was used at T2, and the Swanson, Nolan and Pelham Scale-IV (SNAP-IV) (Swanson 1992) at T1 to measure ADHD symptoms. The ASRS has two parts, but only part A (core symptoms relating to diagnosis) was used here. SNAP-IV gives a total ADHD score and also has subscores, but only the total score regarding ADHD was used in the present study. A diagnosis of ADHD was made in cases scoring above cut-off on any of the scales and showing clinical impairment from reported ADHD-problems, or in individuals who, in other unstructured or semi-structured portions of the psychiatric assessment reported on symptoms and impairments that corresponded to a clinical DSM-IV-diagnosis of ADHD.
Diagnosis of DCD and Tic Disorder
Developmental coordination disorder (DCD) and Tic disorder was diagnosed in cases showing clear signs of DCD in childhood based on the information obtained in connection with the Diagnostic Interview for Social and COmmunication Disorders (DISCO-11) (Leekam et al. 2002), a semi-structured interview for use with a parent/other close informant of a person with a suspected ASD, interview performed at T1. There was a plan to use the DISCO-11 for all participants at T2, but only 21 out of the 50 participant’s parents were interviewed, because (a) the participant did not allow an interview with their parent (14 cases), (b) the participant did not have a parent alive to interview (5 cases) or (c) the parent did not agree to or could not participate in the interview for other reasons (10 cases). At T1, the DISCO-11 had been used in most cases. Because AS according to Gillberg’s criteria include clumsiness as a criterion most individuals in the cohort were suspected of having shown DCD-like features in childhood. To differentiate between AS clumsiness and DCD, the second criteria of DCD, i.e. that the motor coordination difficulties had to have given impairments in everyday life was emphasized.
Diagnosis of Depression
The beck depression inventory (BDI) (Beck and Steer 1996) was used at T1 and T2 to measure depression symptoms. A diagnosis of depression was made on the basis of results obtained at the mini international neuropsychiatric interview (MINI) (Sheehan et al. 1998)—a widely used psychiatric structured diagnostic interview instrument for psychiatric diagnosis according to the DSM-was used at T2, and also in those cases screening positive on the BDI and showing clinical impairment from the symptoms reported on that scale, even in cases when the MINI did not provide results consistent with a full diagnosis of depression.
Diagnosis of All Other Psychiatric Disorders Named Above
Results from MINI were also used to assess previous or current anxiety disorders (GAD, social phobia, panic disorder, agoraphobia and PTSD), current OCD, previous or current bipolar disorder, previous or current psychosis, current eating disorders, previous or current antisocial personality disorder, and current drug and alcohol dependency.
Assessment of Intelligence and Global Functioning
The Wechsler Adult Intelligence Scale 3rd edition (WAIS-III) (Wechsler 2002), was used to assess FSIQ, VIQ, and PIQ at both T1 and T2.
The GAF (APA 1994) was used to measure general functioning, with scores of 70 and above indicating good functioning or only mildly abnormal psychosocial situation.
Data Analysis
All data analysis was made with IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp, Armonk, NY, USA). Non-parametric statistics was used and all significance tests were two-tailed. With a view to increasing comparability/readability, means are presented even in cases where the statistical analysis was made based on medians or ranks.
Comparisons between the different comorbid psychiatric disorders and GAF scores at T2 were made with the Mann–Whitney U test. The total number of comorbid diagnoses fulfilled in the group with a stable ASD diagnosis and the group who no longer met criteria for an ASD diagnosis was also compared using the Mann–Whitney U test.
ASRS scores at T2, SNAP-IV scores at T1 and BDI scores at T1 and T2 were correlated with WAIS-III FSIQ, VIQ and PIQ scores at T1 and T2 respectively.
Results
Attrition
An analysis of attrition regarding T0 and T1 factors previously published were presented in the Methods section. Analysis of attrition in regards to psychiatric/neurodevelopmental measures used at T1 show that there are no significant differences regarding SNAP-IV scores or BDI scores between the 47 individuals that participated at both T1 and T2 and the 29 individuals that only participated at T1.
Current or Past Psychiatric/Neurodevelopmental Comorbidity
Current psychiatric comorbidity (including current ADHD), was found in 27 of the 50 men (54 %). Forty-seven out of 50 individuals (94 %) had shown clear signs of another psychiatric/neurodevelopmental disorder, either currently and/or in the past (Table 1).
Type and Number of Psychiatric/Neurodevelopmental Disorders
The most common comorbid disorder reported was DCD, with 33 out of 50 (66 %) having shown clear signs of DCD during childhood/adolescence. Twenty-two out of 50 (44 %) had a reported tic disorder in childhood/adolescence (6 individuals met criteria for Tourette’s disorder and 16 had either vocal or motor tics). Fourteen men (28 %) had clear signs of a current diagnosis of ADHD.
Twenty-nine out of the 50 men (58 %) had at least at one point in their life met criteria for a diagnosis of depression (either previously (n = 15) or currently (n = 14), most of whom also had had episodes of depression before the study).
Six men showed clear signs of antisocial personality disorder, five met criteria for generalised anxiety disorder, four men had a diagnosis of current OCD, three reported agoraphobia, two individuals reported social phobia, two reported alcohol dependency, two reported psychotic symptoms previously (one of whom had bipolar disorder), and one had bipolar disorder without psychotic symptom previously.
When looking at life-time prevalence of psychiatric/neurodevelopmental comorbidity three individuals had no reported additional diagnoses, 11 individuals had one comorbid diagnosis, 15 had two reported diagnosis, 10 had three diagnoses, six had four diagnoses, and five have five diagnoses or more.
As regards current psychiatric comorbidity, 23 out of 50 individuals had no comorbid diagnosis, 12 had one comorbid diagnosis, 10 had two diagnoses, and five had three diagnoses or more.
Psychiatric Disorder Related to GAF-Scores
Having a diagnosis of ADHD was significantly negatively related GAF scores (Table 2). No other single psychiatric or developmental diagnosis was specifically related to GAF score, but having any comorbid diagnosis was significantly negatively related to GAF scores, as was having ever had any comorbid diagnosis.
Psychiatric Disorder Related to Neuropsychological Test Findings
SNAP-IV scores from T1 correlated negatively with WAIS-III scores at T1 regarding FSIQ (rho = −.590, 95 % CI −.750 to −.365, p < .001), VIQ (rho = −.547, 95 % CI −.720 to −.309, p < .001) and PIQ (rho = −.46, 95 % CI −.659 to −.200, p < .001). ASRS part A scores correlated negatively with WAIS-III scores at T2 regarding FSIQ (rho = −.34, 95 % CI −.566 to −.066, p = .022) and PIQ (rho = −.38, 95 % CI −.601 to −.105, p = .010). No other psychiatric assessment tool correlated with WAIS-III scores.
Comorbidity Relating to Stability of ASD Diagnosis
In Helles et al. (2015) it was shown that at T2 11 out of the 50 men no longer met criteria of any ASD diagnosis currently, even though they had done so in childhood (and, in most cases, also in adolescence/young adulthood). A comparison of comorbidity rates between those still fulfilling criteria for an ASD diagnosis and those who did not was made (Table 3). The No ASD group had significantly fewer comorbid diagnoses ever and currently (Table 4). Unlike the “persistent” ASD group, the No ASD group did not have OCD, GAD, psychosis, bipolar disorder or alcohol dependency (but a few met criteria for ADHD and/or depression).
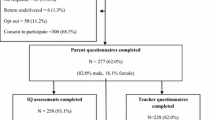
In the Helles et al. (2015) study it was shown that in this cohort eight individuals who met a DSM-IV ASD diagnosis did not fulfil a DSM-5 ASD diagnosis. In Fig. 1 there is a presentation of comorbid disorders in the group fulfilling both DSM-IV and DSM-5 ASD, the group fulfilling only DSM-IV ASD and the group fulfilling neither DSM-IV nor DSM-5 ASD. Sample sizes in each subgroup are too small to make a reliable statistical analysis but it seems that those individuals who fulfil DSM-IV ASD but not DSM-5 criteria are more similar to those who meet both DSM-IV and DSM-5 ASD than those who meet neither DSM-IV nor DSM-5 criteria for ASD.
Discussion
Only three (6 %) of the 50 men with AS in this cohort had never met criteria for an additional psychiatric/neurodevelopmental diagnosis. More than half (54 %) had ongoing comorbidity at the time of the examination, the majority of whom had either ADHD or depression or both. ADHD was significantly related to negative outcome in terms of dimensional GAF scores. Having any psychiatric/neurodevelopmental comorbidity either previously and/or currently was negatively related to outcome as measured on the GAF scale. The minority of the AS group who no longer met criteria for a full ASD diagnosis was often free of current psychiatric comorbidity (73 % fulfilled no psychiatric/neurodevelopmental diagnosis). It is possible that this minority, with very good outcome, has what Gillberg and Fernell (2014) have referred to as “Autism Only” (i.e. without major comorbidity). These authors have proposed that it is only “Autism Plus” (i.e. ASD with significant early onset and persistent comorbidity) that has a poor outcome and that the prognosis in this group may well be predicted more by comorbidity than the autism per se.
These findings underscore the need to always include a full psychiatric/neurodevelopmental assessment whenever a (male) patient is referred for work-up (or follow-up for that matter) under a preliminary or definitive diagnosis of AS (or another ASD). The link between ADHD and poor GAF outcome in the AS group may be of particular importance given the evidence that effective treatments (ranging from martial arts and yoga through working memory training to medications Diamond and Lee 2011) for ADHD symptoms can be expected to reduce some of the negative outcomes associated with this diagnosis (Politte et al. 2014). Only two individuals in the study hade received treatment with central stimulants, which does appear to indicate quite a remarkable degree of undermedication in this context.
The most common additional neurodevelopmental/psychiatric problem that the individuals had ever fulfilled was DCD. This could, at least partly, have been produced by the fact that the Gillberg AS diagnosis (based on Hans Asperger’s clinical descriptions) requires a degree of motor clumsiness for full AS criteria to be met. However, those actually receiving a diagnosis of DCD in the study were not merely “a little bit clumsy” but were impaired by their motor coordination problems. The finding highlights the need to be active in the diagnosis of DCD in individuals who are referred for assessment/follow-up of AS or other ASDs. There are good (e.g. task-oriented motor training programmes) interventions available for the treatment of DCD (Kirby et al. 2014; Smits-Engelsman et al. 2013), interventions that may even help to reduce, not only the motor control problems, but rates of depression and anxiety as well.
Depression is clearly also a very common problem in AS (Mazzone et al. 2013; Lugnegård et al. 2011) and needs to be monitored in all patients at every follow-up point. Depression in AS may be related to ongoing bullying or recent environmental change, and such factors need to be screened for in all individuals who come to health services under the “umbrella diagnosis” of AS.
It is perhaps of significance that there was only one case of schizophrenic psychosis in the whole sample. As mentioned in the Introduction, patients whose AS has remained unrecognized/undiagnosed in childhood and who later get a diagnosis of schizophrenic psychosis very often have an early history consistent with quite a severe form of ASD. In a study by Lugnegard et al. (2013) 40 % of those with schizophrenic psychosis examined around age 30 years had such a history. Given the relatively similar population prevalence estimates for schizophrenia and AS one would, of course, suspect a high rate of schizophrenia in individuals who have AS in childhood. Our finding of only 2 % in the present cohort is therefore somewhat surprising, but consistent with results a follow-up study of AS by Lugnegård et al. (2011). Speculatively, these authors have discussed the possibility that the early diagnosis, early psychoeducation of parents and the boys themselves, and enhanced support at school could have reduced stress (and perhaps stress hormone) levels to such an extent that the “descent” into schizophrenia was avoided in these cases? This is, of course, a hypothetical question given that our study was not designed to answer this specific question, but it is difficult to find a more reasonable interpretation of the findings.
There was no case of proven suicide in the study, but we do not know the cause of death in the one case who had died during the follow-up period. This low rate of suicide is also unexpected given that older reports based on clinical experience (Gillberg 2002; Wing 1981) as well as systematic studies (Takara and Kondo 2014; Paquette-Smith et al. 2014) would tend to suggest a raised rate of suicide attempts and completed suicides.
The new DSM-5 criteria for ASD will exclude some individuals with ASD according to the DSM-IV (Helles et al. 2015). Results from this study indicate that this group (i.e. fulfilling DSM-IV ASD but not the DSM-5 ASD) shows about the same amount of comorbidity as those with ASD according to the DSM-5. This adds some support to the limitations of the ASD concept according to the DSM-5.
The limitations of the study include the relatively small sample size, the failure to identify a reasonably sized sample of females, and the rather considerable attrition rate. Even so, this AS group of males followed systematically for 20 years is the largest to date, and we do not have indications that the group actually examined differed in any major way from those of the original cohort, who, for various reasons, did not participate in the follow-up study. All information collected during this second follow-up has been self-reported (either in a clinical interview or in a survey) which could be perceived as a limitation as individuals with ASD can have difficulties in understanding and expressing emotions. Hurtig et al. (2009) has shown that individuals with ASD and average intelligence are proficient at reporting psychiatric symptoms, indicating that this might not be a limitation at all.
In summary, this study showed that the vast majority of all young boys with AS have developmental trajectories into young adulthood that include very important psychiatric/neurodevelopmental comorbidity. The finding that ADHD, depression, and DCD were the most common comorbidities has positive clinical implications, given that all three have well-documented effective psychological, physical and medical treatments associated with them.
References
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders: DSM-IV (4th ed.). Washington, DC: American Psychiatric Association.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, VA: American Psychiatric Association.
Beck, A., & Steer, R. (1996). Beck depression inventory manual—Swedish version. Fagernes: Psykologiforlaget.
Buck, T. R., Viskochil, J., Farley, M., Coon, H., McMahon, W. M., Morgan, J., et al. (2014). Psychiatric comorbidity and medication use in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(12), 3063–3071.
Cederlund, M., & Gillberg, C. (2004). One hundred males with Asperger syndrome: A clinical study of background and associated factors. Developmental Medicine and Child Neurology, 46(10), 652–660.
Cederlund, M., Hagberg, B., Billstedt, E., Gillberg, I. C., & Gillberg, C. (2008). Asperger syndrome and autism: A comparative longitudinal follow-up study more than 5 years after original diagnosis. Journal of Autism and Developmental Disorders, 38(1), 72–85.
Diamond, A., & Lee, K. (2011). Interventions shown to aid executive function development in children 4 to 12 years old. Science, 333, 959–964.
Ghaziuddin, M., Weidmer-Mikhail, E., & Ghaziuddin, N. (1998). Comorbidity of Asperger syndrome: A preliminary report. Journal of Intellectual Disability Research, 42(Pt 4), 279–283.
Gillberg, C. (1991). Clinical and neurobiological aspects of Asperger syndrome in six family studies. In U. Frith (Ed.), Autism and Asperger Syndrome. Cambridge: Cambridge University Press.
Gillberg, C. (2002). A guide to Asperger syndrome. Cambridge: Cambridge University Press.
Gillberg, C. (2010). The ESSENCE in child psychiatry: Early symptomatic syndromes eliciting neurodevelopmental clinical examinations. Research in Developmental Disabilities, 31(6), 1543–1551.
Gillberg, C. (2014). ESSENCE gathers the diagnoses into a whole. Lakartidningen, 111(39), 1643–1646.
Gillberg, C., & Billstedt, E. (2000). Autism and Asperger syndrome: Coexistence with other clinical disorders. Acta Psychiatrica Scandinavica, 102(5), 321–330.
Gillberg, C., & Cederlund, M. (2005). Asperger syndrome: Familial and pre-and perinatal factors. Journal of Autism and Developmental Disorders, 35(2), 159–166.
Gillberg, C., & Fernell, E. (2014). Autism plus versus autism pure. Journal of Autism and Developmental Disorders, 44(12), 3274–3276.
Gillberg, I. C., & Gillberg, C. (1989). Asperger syndrome—Some epidemiological considerations: A research note. Journal of Child Psychology and Psychiatry, 30(4), 631–638.
Helles, A., Gillberg, C. I., Gillberg, C., & Billstedt, E. (2015). Asperger syndrome in males over two decades: Stability and predictors of diagnosis. Journal of Child Psychology and Psychiatry, 56(6), 711–718.
Hofvander, B., Delorme, R., Chaste, P., Nyden, A., Wentz, E., Stahlberg, O., et al. (2009). Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry, 9, 35.
Hurtig, T., Kuusikko, S., Mattila, M. L., Haapsamo, H., Ebeling, H., Jussila, K., et al. (2009). Multi-informant reports of psychiatric symptoms among high-functioning adolescents with Asperger syndrome or autism. Autism, 13(6), 583–598.
Joshi, G., Wozniak, J., Petty, C., Martelon, M. K., Fried, R., Bolfek, A., et al. (2013). Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: A comparative study. Journal of Autism and Developmental Disorders, 43(6), 1314–1325.
Kessler, R. C., Adler, L. A., Gruber, M. J., Sarawate, C. A., Spencer, T., & Van Brunt, D. L. (2007). Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a representative sample of health plan members. International Journal of Methods in Psychiatric Research, 16(2), 52–65.
Kirby, A., Sugden, D., & Purcell, C. (2014). Diagnosing developmental coordination disorders. Archives of Disease in Childhood, 99(3), 292–296.
Leekam, S., Libby, S., Wing, L., Gould, J., & Gillberg, C. (2000). Comparison of ICD-10 and Gillberg’s criteria for Asperger syndrome. Autism, 4(1), 11–28.
Leekam, S. R., Libby, S. J., Wing, L., Gould, J., & Taylor, C. (2002). The diagnostic interview for social and communication disorders: Algorithms for ICD-10 childhood autism and Wing and Gould autistic spectrum disorder. Journal of Child Psychology and Psychiatry, 43(3), 327–342.
Lugnegård, T., Hallerbäck, M. U., & Gillberg, C. (2011). Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Research in Developmental Disabilities, 32(5), 1910–1917.
Lugnegard, T., Unenge Hallerback, M., Hjarthag, F., & Gillberg, C. (2013). Social cognition impairments in Asperger syndrome and schizophrenia. Schizophrenia Research, 143(2–3), 277–284.
Mattila, M. L., Hurtig, T., Haapsamo, H., Jussila, K., Kuusikko-Gauffin, S., Kielinen, M., et al. (2010). Comorbid psychiatric disorders associated with Asperger syndrome/high-functioning autism: A community- and clinic-based study. Journal of Autism and Developmental Disorders, 40(9), 1080–1093.
Mazzone, L., Postorino, V., De Peppo, L., Fatta, L., Lucarelli, V., Reale, L., et al. (2013). Mood symptoms in children and adolescents with autism spectrum disorders. Research in Developmental Disabilities, 34(11), 3699–3708.
Mazzone, L., Ruta, L., & Reale, L. (2012). Psychiatric comorbidities in asperger syndrome and high functioning autism: diagnostic challenges. Annals of General Psychiatry, 11(1), 16.
Mukaddes, N. M., Herguner, S., & Tanidir, C. (2010). Psychiatric disorders in individuals with high-functioning autism and Asperger’s disorder: Similarities and differences. The World Journal of Biological Psychiatry, 11(8), 964–971.
Paquette-Smith, M., Weiss, J., & Lunsky, Y. (2014). History of suicide attempts in adults with Asperger syndrome. Crisis, 35(4), 273–277.
Politte, L. C., Henry, C. A., & McDougle, C. J. (2014). Psychopharmacological interventions in autism spectrum disorder. Harvard Review of Psychiatry, 22, 76–92.
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., et al. (1998). The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(Suppl 20), 22–33.
Skokauskas, N., & Gallagher, L. (2010). Psychosis, affective disorders and anxiety in autistic spectrum disorder: Prevalence and nosological considerations. Psychopathology, 43(1), 8–16.
Smits-Engelsman, B. C., Blank, R., van der Kaay, A. C., Mosterd-van der Meijs, R., Vlugt-van den Brand, E., Polatajko, H. J., et al. (2013). Efficacy of interventions to improve motor performance in children with developmental coordination disorder: A combined systematic review and meta-analysis. Developmental Medicine and Child Neurology, 55(3), 229–237.
Swanson, J. M. (1992). School-based assessments and intervention for ADD students. Irvine, CA: KC Publications.
Takara, K., & Kondo, T. (2014). Comorbid atypical autistic traits as a potential risk factor for suicide attempts among adult depressed patients: A case–control study. Annals of General Psychiatry, 13, 33. doi:10.1186/s12991.
Unenge Hallerback, M., Lugnegard, T., & Gillberg, C. (2012). Is autism spectrum disorder common in schizophrenia? Psychiatry Research, 198(1), 12–17.
Wechsler, D. (2002). WAIS-III, Wechsler Adult Intelligence Scale, third edition: Technical Manual. San Antonio, TX: Psychological Corporation.
Wing, L. (1981). Asperger’s syndrome: A clinical account. Psychological Medicine, 11(1), 115–129.
Acknowledgments
The study was supported by funding from: Centre for Research and Development in Gavleborg and the Child and Adolescent Psychiatric Clinic in Gavle, VG Region Scientific Fund, the Jerring Fund, Wilhelm and Martina Lundgren Foundation, Petter Silfverskiold Foundation, Golje Foundation, AnnMarie and Per Ahlqvist Foundation, the Swedish Child Neuropsychiatry Science Foundation, and the Gillberg Neuropsychiatry Centre.
Author contribution
ICG, EB and CG designed the study. ICG, AH and EB performed the data collection. AH perfomed all the analysis. ICG, AH and CG wrote the manuscript. EB critically edited the manuscript. AH is guarantor of this work and had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interest.
Rights and permissions
About this article
Cite this article
Gillberg, I.C., Helles, A., Billstedt, E. et al. Boys with Asperger Syndrome Grow Up: Psychiatric and Neurodevelopmental Disorders 20 Years After Initial Diagnosis. J Autism Dev Disord 46, 74–82 (2016). https://doi.org/10.1007/s10803-015-2544-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-015-2544-0