Abstract
Suitable screening instruments for the early diagnosis of autism are not readily available for use with preschoolers in non-Western countries. This study evaluated two tools: M-CHAT which is widely used internationally and one developed in Iran called Hiva. A population sample was recruited of nearly 3000 preschoolers in one Iranian city. Parents self-completed the two tools and children who screened positive were invited for a follow-up interview followed by a diagnostic assessment. The Hiva scale proved to be more efficacious in identifying children with ASD and the resulting prevalence rate was higher than that previously reported for Iranian 5 year olds. The study confirms the need to attune screening tools to the cultural contexts in which they are used.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Autism is defined as a lifelong, neuro-developmental disability with an onset usually before 3 years of age. It seriously impacts on a child’s reciprocal social interactions and communication and may be accompanied by stereotyped patterns of behaviours, interests, and activities; often with associated sensitivity to light, sound or touch (Charman et al. 2008). A diagnosis is mainly based on parental reports of the child’s history of social, communicative and play behaviors allied with observations of the child’s behaviours. Symptoms of autism usually become apparent at 12–15 months with a formal diagnosis taking place from 2 years onwards (Johnson et al. 2007).
Internationally prevalence rates for autism spectrum disorders (ASD) vary widely with an extensive systematic review suggesting a median rate globally of around 62 per 10,000 (Elsabbagh et al. 2012). However this figure is skewed towards high income countries where more studies have been conducted. Few robust studies have been undertaken in low and middle income countries where the rates reported are generally lower (Sun and Allison 2010). Samadi et al. (2012) reported a rate 6.26 per 10,000 out of 1.32 million 5-year-old Iranian children who went through the screening programme for autism in the three academic years from 2006 to 2009. In all these prevalence studies, boys outnumber girls in a ratio of around 4:1 (Mandy et al. 2012).
Cultural differences in recognizing the symptoms of autism has been implicated as one of the reasons for lower prevalence rates in non-Western cultures. Matson et al. (2011) contrasted symptoms of ASD between children from Israel, South Korea, the United Kingdom and the United States. Differences across countries were found on ratings of children’s nonverbal communication and socialization, verbal communication, insistence of sameness and restricted interests although not on their social relationships. Hence parents and professionals from certain cultures may place less importance on signs that are favoured in other cultures. This is further borne out by the increased rates found among immigrant families in adopted countries compared to the rates reported for their home country (Barkevik-Olsson et al. 2010; Keen et al. 2010).
International opinion favors early detection and diagnosis of autism disorders as this enables the child to receive early intervention to promote their development while offering guidance and support to concerned families (Wallace and Rogers 2010). This can be achieved through the developmental screening of all children using autism specific screening tools beginning at 18–24 months and throughout the preschool period (Lipkin and Hyan 2011). A variety of tools have been devised to do this. These are mainly based on parental reports and consist of a limited number of items to aid speedy administration. For example, ten item, autism screening tools have been developed for use with toddlers, children, adolescents and adults (Allison et al. 2012). Those individuals who screen positive—their scores equal or exceed a designated cut-off point—are then referred for further assessment such as a structured interview to confirm the child’s developmental history and rule out other conditions. If this confirms the possibility of autism, the child is referred for more detailed diagnostic assessment by trained assessors using standardized tools such as the autism diagnostic interview—revised (ADI-R; Le Couteur et al. 2008) and/or the autism diagnostic observational schedule (ADOS; Lord et al. 2001).
Various screening tools of proven usefulness for ASD have been developed and tested in western cultures but their applicability in low and middle income countries is questionable especially given the cultural variations in identification rates noted previously. The risk then is that the efficiency of the screening tool is diminished within that society (Wallis and Pinto-Martin 2008). Thus the choice of items that are included in the screening test is crucial and the effectiveness of the screening test needs to be assessed in terms of its sensitivity within the intended country of use. Indeed the same argument may apply when screening individuals from immigrant communities in Western countries. Samadi and McConkey (2014) therefore developed a ten item screening tool for use in Iran derived from the widely used Gilliam Autism Rating Scale (2006) which is based on the DSM-IV and ICD-10 criteria for autism. However this screening tool has not been tested for the population screening of preschoolers.
By contrast one of the most commonly used screening tools with preschoolers is M-CHAT (Robins and Dumont-Mathieu 2006). This is a 23 item yes/no parent report checklist designed in the USA to screen for autism in toddlers aged 18–30 months and based around the original CHAT scale that was developed in the UK (Baron-Cohen et al. 1992). M-CHAT has subsequently been used internationally with research findings published from China (Wong et al. 2004), Arab countries (Seif Eldin et al. 2008), Mexico (Albores-Gallo et al. 2012), Spain (Canal-Bedia et al. 2011), Sweden (Nygren et al. 2012), Turkey (Kara et al. 2014) and Japan (Kamio et al. 2014). It has not been used previously in Iran.
The evidence for the efficacy of screening tools is gathered in three ways. Children with a diagnosis of ASD are compared on the screening test to a comparison group of peers who were normally developing. A second approach is to assess children when concerns have been expressed about their development and again compare them to normally developing peers. Both these approaches are likely to exaggerate the predictive validity of the screening test as a pre-selection has been made of children with known or suspected difficulties. The third approach is more stringent and uses the screening test with a total population of children in a defined area and age group and then follows up those who screened positive with a diagnostic assessment. This approach ensures that all children are given the opportunity to be screened thereby enhancing the identification of all those with the condition even if they have not sought an assessment. However there are two risks that the screening tool needs to minimise: the risk that some children will be identified as possibly having ASD when they do not (false positives) or children who do have ASD are not identified as such by the screening tool (false negatives).
Thus the aims of the present study were:
-
To assess the suitability of a screening tool developed in Iran for use with an Iranian child population aged 2 through 5 years of age;
-
To compare the Iranian tool—Hiva—with M-CHAT: an internationally used screening tool.
-
To estimate the prevalence rate for autism within a preschool population in one city of Iran.
Method
Screening Tools
Hiva
Hiva (meaning “wish” in Kurdish language) is a newly developed screening tool consisting of the ten most commonly occurring symptoms of autism as identified by Iranian parents and professionals of children from 3 years of age and an average age of 11 years. These items were all taken from the GARS-2 Scale (Gilliam 2006) all of whose items were derived from the DSM-IV definitions of ASD. As such, they cover the core symptoms of autism in terms of the triad of impairments: five items related to social interaction, three items reflect stereotyped behaviours and two items communication (see Table 4). Three of the ten items are also included in M-CHAT (items 1,5,9). In relation to other Hiva items, the following points should be noted.
Item 2—Use of ‘I’: With non-verbal children this item was scored as a fail. However in the follow-up interviews, children who identified an item as theirs by saying ‘mine’ or their name were deemed to pass.
Item 9—Finger flicking: In the Kurdish and Persian translation this covered all unusual finger and hand movements.
Item 10—Fearful behaviours: In the follow-up interviews it was clarified that this referred to social situations or new experiences.
The Chronbach alpha for Hiva was 0.89 and the positive predictive value was 0.87 in distinguishing children diagnosed with ASD from normally developing children and those with intellectual disability (Samadi and McConkey 2014). Copies of the scale are available from the authors in Kurdish and Persian.
M-CHAT
In the original validation study with 1293 children, M-CHAT has a sensitivity of 0.87, specificity of 0.99 but a low positive predictive value of 0.36 although this rose to 0.68 when combined with a follow-up interview to clarify parental understanding of the items and the child’s behaviours (Robins et al. 2001). In a further study with 3793 children, the positive predictive value was 0.74 although most of those assessed came from the sample of children referred because they were perceived to be of high risk for autism (Kleinmann et al. 2008). However Robins (2008) in a study of unselected toddlers reported a positive predictive value of 6 % but this rose to 57 % after follow-up interviews, In these studies the internal reliability of the M-CHAT was high with a Chronbach’s alpha of 0.85. International studies of M-CHAT have broadly replicated these findings.
M-CHAT was translated into Kurdish and Persian by the first author with the usual back translation procedures and these are available for downloading from the M-CHAT website: http://www.mchatscreen.com/Official_M-CHAT_Website.html.
Diagnostic Assessment
Children who passed the cutoff score on the Hiva measure and the follow up interview were assessed by the first author using the Persian version of ADI-R (Lord et al. 1994, Sasanfar and Toloie 2006). He had participated in the Iranian training course of ADI-R administration offered by the Iranian Special Education Organisation (ISEO). This entailed obtaining 90 % agreement with an experienced ADI-R assessor on three video-recorded assessments he had undertaken. Furthermore all the 11 identified cases of autism in this study were re-assessed by a trained evaluator uninvolved with the study. This confirmed ten cases of autism with a further case reassigned as both autism and intellectual disability.
In addition the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2001) was also used in the diagnostic assessment as the combination of these two tests has been shown to be beneficial in identifying children on the autism spectrum (Kim and Lord 2012). The first author had been trained in the use of ADOS while studying in the UK.
Study Population
This was a population-based, prevalence study undertaken in Mahabad, a small Kurdish city located in Western Azerbaijan province in the North West of Iran which borders Turkey and northern Iraq. This was chosen as it is located in one the least developed regions in Iran in which the first author had established good working relationships with official organizations and a series of activities on Autism awareness had already started in the city. Facilities for screening and follow-up assessments were also available and the city was of manageable size in which to undertake a population study. In the 2010 census, Mahabad’s population was 135,780 with Sunni Muslims the predominant religious group and Kurdish the commonly spoken language. However it cannot be claimed that the city is representative of all Iranian cities.
The target population for this study was preschool children aged 2 through 5 years totaling 16,210 in the 2010 census: 8327 (51.4 %) boys and 7883 girls (48.6 %) with approximately equal numbers of around 4000 for each year grouping. A representative sample of the preschool population at the 95 % confidence level and a 1.75 % margin of error would require a minimum of 2628 children to take part in this screening study.
Procedure
Families were recruited from a range of sources: including 20 private kindergartens and preschool centers supervised by Iranian Social Welfare Organization along with 19 public kindergartens and preschool centers supervised by Iranian Ministry of Education plus one major Day clinic and Mother and Child clinic supervised by the Social Security Organization and three private clinics provided by two pediatricians and one neurologist.
A series of workshops and meeting sessions were held for parents and staff in the various centres and clinics to publicize the study and increase awareness about autism using pamphlets, slides, video clips and oral presentations in Kurdish. All the head teachers of the kindergartens and preschool centers and the clinic heads and admission staff distributed an information sheet about the study to their parents along with the screening questionnaires which were in Kurdish. Parents also were given the option of participating via the Internet and a similar information sheet was incorporated into the online screening and referral system.
To prevent any possible duplication of cases, the child’s national number that is given to all Iranians at the birth, was requested along with the child’s date of birth and gender. It took parents around 10 min to complete the questionnaire which they returned in a sealed envelope to the facility their child attended.
Ethical Considerations
In Iran there are no formal ethical committees to approve this type of research. However international best practice was followed in line with the Declaration of Helsinki (1964) and it was undertaken with the full knowledge and cooperation of the participating services. Parents were assured of confidentiality. All participants gave informed consent for their participation in each phase of the study. Children who screened positive received a one-to-one interview with the first author to discuss next steps and if appropriate the child was offered a more thorough diagnostic assessment and onward referral to the appropriate agencies. Parents were also given an information sheet about autism and details of a resource pack devised in Iran (Samadi and Mahmoodizadeh 2014).
Sample Obtained
Four thousand self-completion questionnaires were distributed and 3299 (82 %) were collected from different centers. However 470 were deleted due to incomplete information or the child was over 5 years or under 2 years of age. Another 112 online responses were also collected, therefore the final sample was 2941. Thus the screened population exceeded the target set by over 300 and represents around 18 % of the preschool population in the city.
Details of the sample are given in Table 1. Compared to the preschool population in the city there is a slight oversampling of 2 years olds (23 % of whom were recruited) and an under-representation of 5 years olds (14 % recruitment).
Results
Positive Screens
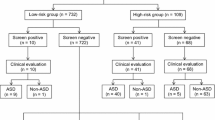
A follow-up interview is recommended to clarify parental responses on self-completion scales. Based on a cut-off score of three and above, 120 children (4.1 % of total) screened positive on both the M-CHAT and Hiva, a further 40 (1.4 %) on only Hiva and 437 (14.9 %) on only M-CHAT. Due to limited resources, it was decided to invite all those who had screened positive on Hiva (n = 160) for a follow up interview. However 51 parents did not respond; with proportionately more parents of 2 years olds not attending (44 % of those invited) compared to those with children aged 5 years (26 %). Also 17 of the 51 parents who did not come for interview, had children who screened positive only on M-CHAT but only one solely on Hiva scores.
One-to-one interviews in Kurdish were undertaken with 109 parents when the child’s developmental history and the questions on Hiva were reviewed and clarified. In all 34 children (31 %) were deemed unlikely to be positive screens and two (2 %) had other developmental conditions (PKU and severe intellectual disability). Proportionately more of these children were aged 5 years (29 % of the total).
The remaining 73 (2.6 % of the total sample) were referred for a diagnostic assessment which included reviewing the child’s medical and developmental history through interviews with parents or care givers mostly in Kurdish but with clarifications in Persian if required. In addition, the first author undertook clinical observations and the administration of the ADI-R and ADOS. The largest number of children assessed were 5 years of age (n = 31) followed by 4 year olds (n = 21); 3 year olds (n = 12) and 2 year olds (n = 9).
In all, 11 children (15 % of those assessed clinically) met the criteria for autism based on ADI-R and a further 17 children (23 %) were deemed to have an ASD based mainly on ADOS. In terms of ages; they represent 0.9 % of all 2 years screened; 0.7 % of 3 year olds; 1.0 % of 4 year olds and 1.2 % of 5 years old. Overall 68 % were male. All these children were referred to the relevant organisation according to their age for follow-up.
However 45 children (62 % of those assessed) did not receive the diagnosis of autism and therefore could be considered to be false positives although some of these children had other impairments and developmental difficulties. Proportionately more were aged four and 5 years. Parents of this group of children were given feedback in a group session on how they could promote their child’s development and manage unusual behaviours. The ISEO bureau was also informed of the children identified in this sample for further assessment.
Comparison of the Psychometric Properties of the Two Screening Tools
As Charman and Gotham (2013) noted, the three main parameters in assessing the efficacy and utility of screening tools are:
-
1.
Sensitivity the proportion of individuals with ASD who have a positive screen result. This should be high so that all those with ASD are picked up at screening.
-
2.
Specificity is the proportion of individuals with ASD who have a negative screen result. This too should be high otherwise the proportion of children falsely identified as ASD on the screening would entail costly diagnostic examinations and unnecessary concern to parents.
-
3.
Positive predictive value (PPV) is the proportion of individuals with a positive screen result who have the disorder. Ideally this would be close to 100 % but rarely is.
Table 2 summarises these values for the two screening tools when used with the Iranian sample and obtained through the use of RoC scaling (SPSS vers 20).
As the table shows, the positive predictive value of the Hiva based solely on parental ratings could be further enhanced by taking account of the follow-up interview which was undertaken with all the children who scored above the cut-off on Hiva. On Hiva, the follow-up interview suggested that one-third of the children assessed were unlikely to have ASD which reduces the number of positive screens from 161 to 107 and thus increases the PPV to 38 %.
Resources did not permit for all children who screened positive on M-CHAT (n = 557) to have a follow-up interview. However a past study in the USA with toddlers aged up to 30 months had identified a rise in PPV from 6 to 57 % when a follow-up interview was undertaken. But in this study, follow-up interviews would have been necessary with over three times as many parents compared to those identified using the Hiva cut-off (Table 2).
The internal consistency of the two scales was explored using Chronbach alpha. This was also done for each age grouping as shown in Table 3.
These scores are noticeably lower than those reported previously for M-CHAT of 0.86 and for Hiva of 0.89, although both these values were obtained with selected samples of children who had a diagnosis of ASD or were referred for this purpose. The variation over the age groups suggests that with preschool children the items on both tools are reflective of different types of developmental difficulties.
Table 4 presents the items from Hiva that distinguishes those given a diagnosis from three other groupings of children: (1) those who were screened at interview and then were assessed but a diagnosis of ASD was not given, (2) those who were interviewed but no assessment was thought necessary and (3) those who scored under the cut-off. Although some caution needs to be exercised due to small numbers, this information suggests that certain items on Hiva are more prone to creating false positives and should be probed particularly at interview. For instance: a higher proportion of children not assessed as ASD passed the two items: ‘Making high-pitched sounds’ and ‘Flicks fingers rapidly in front of face’ than did those who were assessed as ASD. The latter item in the Kurdish and Persian translation of the scale covers all unusual hand and finger movements, such as hand flapping. Also high proportions of those children removed at interview had also passed these items.
The M-CHAT contains six items which are identified as critical for a diagnosis of ASD as shown in Table 5 but on none of them did the proportion of children identified as ASD exceed 50 %. Also the false positives (children assessed as not ASD) were highest for items relating to imitation and pointing. This suggests cultural differences in the interactions that Iranian parents consider indicative of difficulties with their child compared to those in western societies.
The item analyses of the two scales were further confirmed when the correlations of scores between the two tests were calculated and these are also shown for each age group as well as for the total sample in Table 6.
Although all the correlations were significant (p < 0.001) the amount of shared variance was <50 % which suggests the two tests focus on different aspects of children’s behaviours especially in the younger age groups.
Finally a test–retest evaluation on a sample of 100 parents of preschool children selected at random showed a high correlation between two administrations of Hiva (r = 0.98) after a 1 week interval. Also in a sample of 59 children, the correlation between parents’ ratings and those of kindergarten teachers was r = 0.95. Comparable data is not available for M-CHAT.
Prevalence of Autism
The 28 children identified as ASD in this sample of 2941 children, represents a prevalence rate of 95.2 per 10,000 [confidence interval (CI) at 95 % of 66–137]. For those diagnosed with autism (n = 11) the prevalence rates are 37.4 per 10,000 (CI 16–49).
However there was a noticeable age effect. For children aged 2 and 3 years, the prevalence rate for ASD was 77 per 10,000 (CI 42–141) and for autism was 15 per 10,000 (CI 4–56). Whereas for children aged 4 and 5 years, the prevalence rate for ASD was 110 per 10,000 (CI 69–173) and for autism it was 55 per 10,000 (CI 29–104).
These figures—even at the lower confidence levels—are much higher than the previously reported rate for 5 year olds in Iran of 6.26 per 10,000 (Samadi et al. 2012).
Discussion
This study had a number of strengths. It was based on an unselected population of preschoolers in one Iranian city with a high response rate from parents who were approached to participate in the study. It used a scale that had been developed in Iran—albeit for use with older children—and comparisons were drawn with an internationally recognised screening tool: albeit one designed for use with younger children. Also children were diagnosed using internationally recognized diagnostic tools for ASD and the children diagnosed with autism were cross-checked with two assessors independently.
That said, there are two limitations to be borne in mind. First, families who were not attending any clinic or preschool facility were not able to be included in the study. Second it is possible that parents who were more concerned about their child’s development took part in the initial screening and in the diagnostic assessments which would inflate the prevalence levels reported here.
Overall the Hiva scale proved to be more efficacious in terms of sensitivity, specificity and positive predictive value than did M-CHAT. Two reasons may count account for this. Hiva included items that seem to be particularly salient with Iranian parents in terms of their expectations of children’s behaviour and their interactions with children as the item analyses of the scales showed. Also these items may be more suited with older preschoolers whereas M-CHAT was developed for use with younger children.
These reasons might also account for the discrepancies between this study and other international studies cited previously which better replicated the screening properties of the original M-CHAT. A further point of difference was the use of a population sample in this study rather than identified samples. However further international studies would usefully illuminate the type of adaptations needed to produce efficacious screening tools for ASD.
Screening tools also can be assessed in terms of their utility and in this respect too Hiva was preferable. It is quicker to administer; containing only ten items in line with the AQ-10 scales recently produced in the UK (Allison et al. 2012). Hiva identified many fewer children who scored above the cut-off which reduced the number of follow-up interviews required to confirm parental ratings and also the number of diagnostic assessments to be undertaken which is an important consideration when the personnel to undertake these assessments are scarce in countries such as Iran. Nonetheless the findings underscore the need for follow-up interviews with parents to clarify their understanding of the items and their child’s responses. This may be especially crucial when there are no terms in local languages that fully convey the English meaning. Certain items on Hiva have been identified that require particular probing so as to increase its positive predictive value combined with follow-up interviews. The procedures devised for use with the revised M-CHAT-R (Robins et al. 2009) provide a useful model in this regard. Follow-up interviews could be done by telephone and by trained personnel who have experience of children with ASD (Robins 2008). It is also possible that some of these children may have other developmental difficulties for which the family would appreciate further advice and guidance.
The Hiva scale was developed specifically for use in Iran and may have limited applicability in other countries although this remains to be tested. Alternatively it could be that existing screening tools other than M-CHAT-including the recently revised M-CHAT-R (Robins et al. 2014) or the Q-Chat-10 (Allison et al. 2012)—would be more suited across cultures but again this is open to further investigation along the lines adopted here. A third course of action would be to develop new screening tools for particular cultures and again this study serves as a model for how this might be done. For example the appropriateness of certain items from M-CHAT on pointing and eye contact has been questioned when used in Mexican and Asian cultures (Albores-Gallio et al. 2012; Wallis and Pinto-Martin 2008).
Our findings also raise the issue as to whether the scales need to be developed for specific age bands of children: a strategy that has been followed in England with the development of AQ scales for adults, adolescents, children and toddlers (Allison et al. 2012) which recognise that pertinent symptoms of autism will vary according to the developmental level of functioning of the person. This point is especially valid in the preschool period between 18 months and 5 years when children’s behavioural repertoires widen considerably and which may account for the variations in the properties of the tools that were evident across the different age groups in this study. Also Wiggins et al. (2012) identified three distinct subgroups among toddlers diagnosed with ASD which supports a dimensional profile of ASD rather than a unitary concept. This would explain the low internal consistency scores found with younger preschoolers in this study on both M-CHAT and Hiva. Similarly the criteria used to assess unusual behaviours across cultures may also vary across age groupings although by 5 years of age, there was more consistency in parental ratings across the Hiva items.
These arguments are especially salient given that the primary purpose of any screening tool is to identify children who may require particular interventions. One consequence is that screening tests developed in the USA and UK may underestimate the presence of ASD in children when applied in other cultures (Mandell et al. 2009). Indigenously produced screening tests could remedy this deficit while possibly retaining international comparability of the prevalence of ASD provided the criteria for its diagnosis remain universal.
Nonetheless the prevalence rates identified in this study should be treated as indicative rather than definitive when making comparisons within Iran and with other countries. The relatively small numbers of children diagnosed when added to the limitations of the sample—one city in Iran—means that the CIs for the prevalence rates are large. Even so, the prevalence rate for all preschoolers at the lower confidence level of 16.0 per 10,000 exceeds the rate previously reported for 5 year olds of 6.25 per 10,000 although in less developed provinces (in which Mahabad is located) the rate was lower again at 3.88 per 10,000 (Samadi et al. 2012). The suggests that the national screening programme for autism undertaken by the ISEO underestimates the numbers of school-age children with autism. The reasons for this are not clear. It may be that there is greater awareness of ASD in Iran which has resulted in increased numbers of children coming forward for assessment in this city. An ongoing study is examining updated prevalence rates from the national screening of all 5 year olds. However it is also possible that a proportion of preschool children with ASD are diverted from schools and do not participate in the national screening programme. This study is the first indication of the extent of those unknown to education. It also highlights the likely numbers of preschool children and families who would benefit from specialist advice and support. A starting point is the provision of information to parents and preschool personnel allied with the provision of training workshops (Samadi et al. 2013). Also the Iranian Social Welfare Organization has started to provide educational and intervention services for children with ASD from two to 5 years old and this data will help justify the extension to these services nationally. Plans are in hand to extend the use of Hiva to five other provinces in the north, central, south and eastern parts of Iran which will help to produce more robust indication of prevalence rates and confirm any regional variations.
In conclusion, Hiva has the potential to provide a suitable screening tool for preschool children in Iran when used in combination with a follow-up interview. Further studies are needed of its use in ascertaining more robust prevalence rates of ASD among Iranian preschool children coupled with suitable intervention strategies to support and guide these families and the personnel working in pre-school facilities and clinics.
References
Albores-Gallo, L., Roldán-Ceballos, O., Villarreal-Valdes, G., Betanzos-Cruz, B. X., Santos-Sánchez, C., Martínez-Jaime, M., et al. (2012). M-CHAT Mexican version validity and reliability and some cultural considerations. International Scholarly Research Network—Neurology, 2012, 408694.
Allison, C., Auyeung, B., & Baron-Cohen, S. (2012). Toward brief “red flags” for autism screening: the short autism spectrum quotient and the short quantitative checklist in 1,000 cases and 3,000 controls. Journal of the American Academy of Child and Adolescent Psychiatry, 51(2), 202–212.
Barkevik-Olsson, M., Gillberg, C., & Fernell, E. (2010). Prevalence of autism in children of Somali origin living in Stockholm: Brief report of an at-risk population. Developmental Medicine and Child Neurology, 52(12), 1167–1168.
Baron-Cohen, S., Allen, J., & Gillberg, C. (1992). Can autism be detected at 18 months? The needle, the haystack, and the CHAT. British Journal of Psychiatry, 161, 839–843.
Canal-Bedia, R., García-Primo, P., Martín-Cilleros, M., Borbujo, J., Guisuraga-Fernández, Z., Herráez-García, L., et al. (2011). Modified checklist for autism in toddlers: Cross-cultural adaptation and validation in Spain. Journal of Autism and Developmental Disorders, 41(10), 1342–1351.
Charman, T., & Gotham, K. (2013). Measurement Issues: Screening and diagnostic instruments for autism spectrum disorders—lessons from research and practise. Child and Adolescent Mental Health, 18(1), 52–64.
Charman, T., Loucas, T., Pickles, A., Simonoff, E., Chandler, S., Meldrum, D., et al. (2008). Autistic symptomatology and language ability in autism spectrum disorder and specific language impairment. Journal of Child Psychology and Psychiatry, 49(11), 1184–1192.
Elsabbagh, M., Divan, G., Koh, Y., Shin Kim, Y., Kauchali, S., Marcín, C., et al. (2012). Global prevalence of autism and other pervasive developmental disorders. Autism Research, 5, 160–179.
Gilliam, J. (2006). GARS-2: Gilliam Autism Rating Scale-second edition. Austin, TX: PRO-ED.
Johnson, C. P., Myers, S. M., & American Academy of Pediatrics Council on Children with Disabilities. (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120(5), 1183–1215.
Kamio, Y., Inada, N., Koyama, T., Inokuchi, E., Tsuchiya, K., & Kuroda, M. (2014). Effectiveness of using the modified checklist for autism in toddlers in two-stage screening of autism spectrum disorder at the 18-month health check-up in Japan. Journal of Autism and Developmental Disorders, 44, 194–203.
Kara, B., Mukaddes, N.M., Altınkaya, I., Güntepe, D., Gökçay, G. & Özmen, M. (2014). Using the Modified Checklist for Autism in Toddlers in a well-child clinic in Turkey: Adapting the screening method based on culture and setting. Autism, 18(3), 331–338.
Keen, D. V., Reid, F. D., & Arnone, D. (2010). Autism, ethnicity and maternal immigration. British Journal of Psychiatry, 196, 274–281.
Kim, S. H., & Lord, C. (2012). Combining information from multiple sources for the diagnosis of autism spectrum disorders for toddlers and young preschoolers from 12 to 47 months of age. Journal of Child Psychology and Psychiatry, 53(2), 143–151.
Kleinmann, J. M., Robins, D. L., Ventola, P. E., Pandey, J., Boorstein, H. C., Esser, E. L., et al. (2008). The modified checklist for autism in toddlers: A follow-up study investigating the early detection of autism spectrum disorders. Journal of Autism and Developmental Disorders, 38(5), 827–839.
Le Couteur, A., Haden, G., Hammal, D., & McConachie, H. (2008). Diagnosing autism spectrum disorders in pre-school children using two standardised assessment instruments: the ADI-R and the ADOS. Journal of Autism and Developmental Disorders, 38(2), 362–372.
Lipkin, P. H., & Hyan, S. L. (2011). Should all children be screened for Autism Spectrum Disorders? American Family Physician, 84(4), 365–367.
Lord, C., Rutter, M., DiLavore, P. D., & Risi, S. (2001). Autism diagnostic observation schedule. Los Angeles, CA: Western Psychological Services.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism diagnostic interview—revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24, 659–685.
Mandell, D. S., Wiggins, L. D., Carpenter, L. A., et al. (2009). Racial/ethnic disparities in the identification of children with Autism Spectrum Disorders. American Journal of Public Health, 99, 493–498.
Mandy, W., Chilvers, R., Chowdhury, U., Salter, G., Seigal, A., & Skuse, D. (2012). Sex differences in autism spectrum disorder: evidence from a large sample of children and adolescents. Journal of Autism and Developmental Disorders, 42(7), 1304–1313.
Matson, J. L., Worley, J. A., Fodstad, J. C., et al. (2011). A multinational study examining the cross cultural differences in reported symptoms of autism spectrum disorders: Israel, South Korea, the United Kingdom, and the United States of America. Research in Autism Spectrum Disorders, 5, 1598–1604.
Nygren, G., Cederlund, M., Sandberg, E., Gillstedt, F., Arvidsson, T., Gillberg, I. C., et al. (2012). The prevalence of autism spectrum disorders in toddlers: A population study of 2-year-old Swedish children. Journal of Autism and Developmental Disorders, 42, 1491–1497.
Robins, D. L. (2008). Screening for autism spectrum disorders in primary care settings. Autism, 12, 537–556.
Robins, D. L., Casagrande, K., Barton, M., et al. (2014). Validation of the modified checklist for Autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics, 133(1), 37–45.
Robins, D. L., & Dumont-Mathieu, T. M. (2006). Early screening for autism spectrum disorders: Update on the modified checklist for autism in toddlers and other measures. Developmental and Behavioral Pediatrics, 27(2), S111–S119.
Robins, D., Fein, D. & Barton, M. (2009) Modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F)TM. http://www.mchatscreen.com/ Accessed Sep 2014).
Robins, D. L., Fein, D., Barton, M. L., & Green, J. A. (2001). The modified checklist for autism in toddlers: An initial study investigating the early detection of autism and pervasive developmental disorders. Journal of Autism and Developmental Disorders, 31(2), 131–144.
Samadi, S.A. & Mahmoodizadeh, A. (2014). Omid early intervention resource kit for children with autism spectrum disorders and their families, Early Child Development and Care, 184(3), 354–369.
Samadi, S., Mahmoodizadeh, A., & McConkey, R. (2012). A national study of the prevalence of autism among five-year-old children in Iran. Autism 16(1), 5–14
Samadi, S. A. & McConkey, R. (2014). The utility of the Gilliam Autism Rating Scale for identifying Iranian children with autism. Disability and Rehabilitation, 36(6), 452–456
Samadi, S. A., McConkey, R. & Kelly, G. (2013). Enhancing parental wellbeing and coping through a family-centred, short course for Iranian parents of children with an Autism Spectrum Disorder. Autism, 17(1), 27–43
Sasanfar, R., & Toloie, A. (2006). Standardising and normalizing the autism diagnostic interview—revised on Iranian population. Tehran: The Iranian Special Education Organisation.
Seif Eldin, A., Habib, D., Noufal, A., Farrag, S., Bazaid, K., Al-Sharbati, M., et al. (2008). Use of M-CHAT for a multinational screening of young children with autism in the Arab countries. International Review of Psychiatry, 20(3), 281–289.
Sun, X., & Allison, C. (2010). A review of the prevalence of autism spectrum disorder in Asia. Research in Autism Spectrum Disorders, 4(2), 156–167.
Wallace, K. S., & Rogers, S. J. (2010). Intervening in infancy: implications for autism spectrum disorders. Journal of Child Psychology and Psychiatry, 51(12), 1300–1320.
Wallis, K. E., & Pinto-Martin, J. (2008). The challenge of screening for autism spectrum disorder in a culturally diverse society. Acta Paediatrica, 97, 539–540.
Wiggins, D. L., Robins, D., Adamson, L., Bakeman, R., & Henrich, C. (2012). Support for a dimensional view of autism spectrum disorders in toddlers. Journal of Autism and Developmental Disorders, 42, 191–200.
Wong, V., Hui, L., Lee, W., Leung, L., Ho, P., Lau, W., et al. (2004). A modified screening tool for autism (checklist for autism in toddlers [CHAT-23]) for Chinese children. Pediatrics, 114, 166–176.
Acknowledgments
Our sincere thanks to the following for their assistance in recruiting families: Dr. Faygh Zhiyan (Tamine Ejtemaei Day Clinic); Dr. Fatah Shadoman (Private Pediatrician clinic); Mr. Amir Ghaderi (Behzisti, Mahabad); Norafza Charity Foundation in Mahabad and the head teachers of the preschools and kindergartens who participated in the study. Also to Mrs. Ayshe Varei from Andishe kindergarten who facilitated the test–retest and inter-rater reliability of the Hiva screening scale and staff at the Tamine Ejtemaei Day clinic for their assistance and hospitality. Dr. Zahra Noparast, Mrs Maryam Mohammad Poursaid and Farzaneh Ghanimi from the Department of Rehabilitation of Iran Social Welfare Organization and Ameneh Mahmoodizadeh from Iranian Special Education Organization evaluation and diagnosis department, who helped with the data collection. Finally we are indebted to the all the parents and children who took part in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
This study does not contain identifiable patient data. All participants gave informed consent for their participation in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Samadi, S.A., McConkey, R. Screening for Autism in Iranian Preschoolers: Contrasting M-CHAT and a Scale Developed in Iran. J Autism Dev Disord 45, 2908–2916 (2015). https://doi.org/10.1007/s10803-015-2454-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-015-2454-1