Abstract
We investigated whether there is an association between increased risk for autism spectrum disorders (ASD) and selective serotonin reuptake inhibitors (SSRIs) used during pregnancy. This study used Denmark’s health and population registers to obtain information regarding prescription drugs, ASD diagnosis, and health and socioeconomic status. There were 1.5 % of cases and 0.7 % of controls exposed to SSRIs during the pregnancy period, and higher effect estimates observed with longer use. We found evidence that in utero exposure to SSRIs increases a child’s risk associated with ASD. These results, while adding to the limited knowledge on prenatal pharmacological exposures as potential ASD risk factors, need to be balanced against the benefits of indicated medication use by pregnant mothers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Selective serotonin reuptake inhibitors (SSRIs) are among the most commonly used medications in pregnancy, with prescription frequency estimates in pregnant women ranging from 0.7 to 1.4 % in Nordic countries (Jimenez-Solem et al. 2013; Kieler et al. 2012) and 5–13 % in the United States (Andrade et al. 2008; Cooper et al. 2007; Ramos et al. 2008). There is accumulating evidence that mothers treated with SSRIs during pregnancy may experience increased rates of adverse reproductive outcomes (Bakker et al. 2010; Lund et al. 2009). In addition, recent studies have suggested a possible link between prenatal antidepressant exposure and neurodevelopmental outcomes including altered speech perception (Weikum et al. 2012) and motor, social–emotional and adaptive behavior (Hanley et al. 2013).
A case–control study conducted in Northern California reported an autism spectrum disorders (ASD) odds ratio (OR) adjusted for age, race/ethnicity, and education of mother, birth weight, sex, and birth year of child, and birth facility associated with any prenatal SSRI use of 2.2 (95 % confidence interval (CI) 1.4, 2.3) (Croen et al. 2011). A Swedish population-based case–control study reported that SSRI use during pregnancy was associated with increased risk of ASD, that was higher among children with ASD without intellectual disability (adjusted for maternal psychiatric disorder, maternal age, paternal age, parental income, education, occupation, maternal country of birth, and birth parity OR 2.34, 95 % CI 1.90–5.06) compared to results for ASD with intellectual disability (adjusted OR 1.09, 95 % CI 0.41–2.91) (Rai et al. 2013). Two studies using the Danish registers reported similar associations. Sorensen et al. (2013) estimate a hazard ratio adjusted for parental age at conception, parental psychiatric history (except maternal affective disorder), gestational age, birth weight, sex, and parity of 1.5 (95 % CI 1.2–1.9), for ASD compared with unexposed children. The hazard ratio decreased to 1.2 (95 % CI 0.7–2.1) when the adjusted analysis was restricted to children of women with a diagnosis of affective disorder. Similarly, for any prenatal exposure, Hviid et al. reported a rate ratio of 1.20 (95 % CI 0.90–1.61) adjusted for year of birth, maternal parity, maternal age, country of origin, maternal place of residence, maternal smoking status, maternal employment status, other drug use before delivery and maternal psychiatric diagnoses before delivery (Hviid et al. 2013).
The issue of whether prenatal SSRI use or the indication for SSRI use is the risk factor remains unresolved. Associations between maternal depression, the chief indicating condition for SSRI use, and developmental psychopathology in children have been reported (Brennan et al. 2000; Caplan et al. 1989; Carter et al. 2001; Deave et al. 2008; Huot et al. 2004). Diagnoses for psychiatric disorders before the birth of the child are more common among parents of children with ASD than parents of children without a diagnosis of ASD, and maternal depression appears to be a greater risk factor than paternal depression (Bolton et al. 1998; Daniels et al. 2008; Rai et al. 2013).
We conducted a population-based case–control study of maternal prenatal SSRI use and risk of ASD, also utilizing the national health and population data registers of Denmark, and paying particular attention to the issue of confounding by indication and misclassification of the indicating condition in register data.
Methods
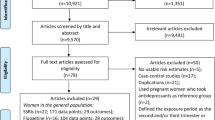
Eligible Participants
All children (n = 749,755) born in Denmark between January 1, 1997 and December 31, 2006 were identified through the Danish Civil Registration System (DCRS). The study population (n = 628,408) was then drawn from all biological singletons and one child randomly selected from multiple births. Children were also excluded if they could not be linked to their biological mother (n = 1,139), if she was not living in Denmark a year before delivery (n = 10,806), or if the child was of gestational age less than 23 weeks or greater than 43 weeks (n = 1,774). We restricted gestational age in our sample because extremely preterm or post-term birth have previously been associated with autism risk (Schendel and Bhasin 2008). The Institutional Review Board of Drexel University and the University of Copenhagen, Danish Data Protection Agency (Record No. 2010-41-4861) approved this study.
Case and Control Definitions
Autism spectrum disorders diagnoses are based on data from the Danish National Hospital Register (DNHR) and the Danish Psychiatric Central Register (DPCR). Together, these registers include information on all inpatient and outpatient care from psychiatric hospitals and psychiatric wards in general hospitals in Denmark. The quality of the diagnosis of childhood autism in the Denmark registers has recently been investigated through a validation study that conducted detailed abstraction of the children’s medical records that were reviewed by autism experts. Register diagnosis of childhood autism was confirmed 94 % of the time with an additional 3 % classified with another ASD (Lauritsen et al. 2010). However, there is also still the possibility that true cases of ASD are not captured in the register. Subjects’ records from January 1, 1999 to March 31, 2011 were searched for International Classification of Diseases codes (ICD-10) of: F840, F841, F845, F848, and F849 (childhood autism, atypical autism, Asperger’s syndrome and pervasive developmental disorder-unspecified, respectively). Subjects were considered a case if any of these codes were present.
Controls were defined from the Danish Civil Registration System as individuals without ASD admission diagnoses. Ten controls per case were individually matched on birth month and year. Matching on birth month and year assured the same follow-up period for cases and controls, and thus the same opportunity to be identified in the register with an ASD diagnosis.
Exposure Definition
Pharmacologic exposure information was drawn from the Danish Drug Prescription Register (DDPR), which records all dispensed prescribed medication from any pharmacy, except hospital dispensaries, in Denmark. Selective serotonin reuptake inhibitor drug codes included in the analysis were N06AB03 (fluoxetine), N06AB04 (citalopram), N06AB05 (paroxetine), N06AB06 (sertraline), N06AB08 (fluvoxamine), and N06AB10 (escitalopram). We extracted from the DDPR information regarding unique personal identification number, dispense date, drug code [the WHO Anatomical Therapeutic Chemical classification system (ATC)], name of drug, number of packaged dispensed, and the number of defined daily dosage (DDD) per package. The ATC classification system and the DDD are used for the expressed purpose of facilitating drug utilization research (Lee et al. 2013) and these coding schemes have been employed in a variety of studies (Gislason et al. 2006; Kaae et al. 2010; Moth et al. 2008; Schernhammer et al. 2011).
Data for each individual were assembled from the three months prior to the estimated-date-of-conception (EDC) to birth. Exposure windows were defined as preconception (90 days prior to EDC), first trimester (within 90 days after EDC), second trimester (within 90–180 days after EDC), and third trimester (180 days after EDC to delivery date). A child was considered exposed during any window if the dispense date fell within the specified exposure period or the number of days supplied overlapped any portion of the time period. To calculate duration of use, the number of DDDs in each dispensed package for the period falling within a given exposure period, based on dispensed date, were summed. Duration was assessed for each trimester separately and dichotomized into two categories, use between 1 and 45 days and use ≥45 days, The reference group for determining the risk of duration of use was no exposure during at any time during the pregnancy.
Covariates
Variables reflecting parental age, parental psychiatric history, gestational age, birth weight, parental history of autoimmune disease, and number of live births, obstetric complications, and family socioeconomic status (a combination of parental income and highest level of education) were available in the Danish registers and were chosen a priori based on the literature (Atladottir et al. 2009, 2010; Burstyn et al. 2010; Daniels et al. 2008; Durkin et al. 2010; Giarelli et al. 2010; Larsson 2005; Schendel and Bhasin 2008). Gestational age was given in days from self-reported last menstrual period, and confirmed using an ultrasound date if the last menstrual period was uncertain.
Maternal psychiatric history prior to delivery was obtained by searching ICD codes in DCPR records starting in 1969. Psychiatric conditions that are indicators for SSRI use were given special consideration. One variable was created for history of maternal depression, the principal indication for SSRI use, and another for the presence of any other indication, including anxiety, obsessive–compulsive disorder, phobia, adjustment disorder and schizophrenia in the register.
Principal Statistical Analysis
Conditional logistic regression analysis estimated ORs associating maternal SSRI exposure variables with children’s ASD diagnoses. Parental age and sex of the child were included in all models. Other covariates were included in adjusted models only if they resulted in a 10 % or greater change in log-OR when added individually. To guard against joint confounding, any initially excluded covariate was individually added back to the adjusted model and retained if the log-OR changed by 10 %. Both stratification and adjustment for maternal depression and other indicators for SSRI use were conducted as initial approaches to address confounding by indication.
Sensitivity Analyses
We used a Monte Carlo simulation approach similar to the methods used by Bodnar et al. (2010) to explore the potential impact of under-reporting of SSRI use and depression in the register. To do this, we first simulated 1,000 datasets with a specified sensitivity and specificity. For each simulated dataset we fit an adjusted logistic regression model, then drew 1,000 samples from the multivariate normal distribution with a mean and variance equal to the model parameters for SSRI use and depression in the register. The 50th, 2.5th, and 97.5th percentiles from the resulting 1,000,000 samples then yielded the OR and 95 % CI for the effect estimate given the specified sensitivity and specificity.
Because the observed SSRI exposure prevalence (0.7 %) was below published estimates, we simulated an increase in the prevalence of SSRI exposure to 3 %, a rate similar to that reported in the literature in other Nordic countries (Bakker et al. 2008; Kieler et al. 2012). We assumed that (a) under-reporting was non-differential with respect to outcome (exposure precedes occurrence of outcome) and (b) specificity was 100 % (because it is unlikely a prescription for an SSRI would be documented in the register when none was given). Sensitivity was assumed to be 26 %, the level expected if true SSRI exposure prevalence was 3 % and observed exposure prevalence was 0.7 %. A similar approach was used to examine the impact of under-ascertainment of maternal depression because published estimates of the prevalence of maternal depression during pregnancy in Europe range from 3 to 17 % (Evans et al. 2001; Josefsson et al. 2001; Lund et al. 2009; Olsen et al. 2004)—much higher than our observed prevalence of 0.6 %. In our simulations, we increased maternal depression prevalence to 5 % and then 15 %, and assumed this to be non-differential with respect to ASD case status. Specificity was assumed to be 100 % and sensitivity was set to 14 and 4.7 % to reflect the under-reporting of true depression prevalence rates of 5 and 15 %, respectively.
Lastly, we performed a sensitivity analysis to determine how robust our quantitative estimates were to unmeasured confounding. Following the method of Lin et al. (1998) we assumed a binary confounder U existed such that U increased the risk of ASD, and that U was more prevalent in SSRI-exposed mothers than in unexposed mothers. Given the strength of relationship of U with ASD, and the prevalence of U in the exposed and unexposed, it is therefore possible to estimate odds ratios that are corrected for this unmeasured confounder U. We estimated corrected odds ratios over a range of plausible parameters.
Results
Study Sample
There were 5,215 children diagnosed with ASD and 52,150 controls in the study sample for exposure anytime during pregnancy. Children with ASD were more likely than controls to be male, have older parents, and have a mother with history of depression (Table 1). There were 77 mothers with depression and 365 without depression who had used SSRIs.
Associations of Any SSRI Use with ASD
We observed on average a doubling of odds for ASD regardless of exposure window (Table 2). After accounting for the parental age and child sex, adjusted OR of ASD for any SSRI exposure during pregnancy was 2.0 (95 % CI 1.6–2.6). Effect estimates and CI widths did not change dramatically with adjustment for other covariates. Further adjustment for maternal depression and any SSRI indication yielded effect estimates equal to 1.9 (95 % CI 1.5–2.5) and 1.8 (95 % CI 1.4–2.3), respectively.
In analyses restricted to subsets of (1) only mothers with a diagnosis of depression, and (2) only mothers with depression and other psychiatric conditions associated with SSRI before the birth of the child, the SSRI effect estimates were close to the null with broad CIs (data not shown). Effect estimates for the mothers without SSRI indications where close to the estimates reported for the full data sets (data not shown).
Effect of Duration of Use of SSRI
The median duration of use during pregnancy was 119 days among mothers of cases compared to that of controls (75 days) (Table 1). SSRI use longer than 45 days, in each exposure window except for the third trimester, regardless of exposure period, resulted in slightly higher odds ratios than exposure of 45 days or less compared to the unexposed reference group (Table 3). In the third trimester, exposure to SSRIs for less than 45 days had virtually the same ORs as exposure for more than or equal to 45 days in the fully adjusted model.
Analysis of Impact of Misclassification of SSRI Use and Maternal Depression
Table 4 shows the results from simulation analyses exploring the influence of misclassification. The first row presents effect estimates and confidence bounds for any prenatal SSRI exposure from simulations assuming increased SSRI prevalence and non-differential misclassification as described above. Estimates for the full sample were close to the comparable (Model 1) adjusted estimate in Table 2, suggesting that exposure misclassification is unlikely to have strongly influenced results. The following rows show results from simulations investigating the potential effects of non-differential under-reporting of maternal depression. By increasing the assumed depression prevalence to 5 %, the pooled effect estimate, 2.2 (95 % CI 1.9–2.4), was comparable to Model 1 estimates shown in Table 2. At 15 % assumed depression prevalence, the SSRI effect was only moderately altered. Under the assumed 15 % depression prevalence scenario we also estimated depression-stratified effects. A positive association was observed in both strata, though the effect was smaller among mothers with depression, with median adjusted odds ratios and confidence intervals of 1.4 (95 % CI 0.9–2.4). The effect among mothers without depression had a median adjusted odds ratio and confidence interval of 2.1 (1.5–3.0).
In our analysis that investigated the impact of unmeasured confounding, we find evidence to suggest that our results remain moderately robust (see “Appendix” in Table 5). For example, if there were an unmeasured confounder U that doubled the risk of ASD, and had 50 % prevalence in SSRI-exposed mothers and only 5 % prevalence in SSRI-unexposed mothers, the corrected OR would still be 1.3 (1.0, 1.6).
Discussion
In a large population-based case–control study we observed an increased risk of ASD associated with in utero exposure to SSRIs. The effect was present in all exposure windows considered and persisted after adjustment for SSRI indications. Croen et al. (2011) observed comparable magnitude associations in each exposure period, which also persisted in that sample after statistical adjustment for maternal depression. Rai et al. (2013) also observed similar associations in their full analyses of maternal SSRI use during pregnancy and ASD as well as in their analysis looking at ASD without intellectual disability, but slightly attenuated results for ASD with intellectual disability. This study adds to previously available evidence by examining prenatal duration of SSRI use—observing the largest associations in the highest duration categories. However, these duration-response effects were not consistently monotonic across trimesters. It is also possible that the higher effect estimates found with longer duration of use may be confounded by the severity of depression. In other words, more serious depression may lead to the SSRI duration levels sufficient to increase risk of having a child with ASD.
While our analyses suggested that there was an independent effect of prenatal SSRI use, other studies by Sorsensen et al. and Hviid et al. using the same Danish registers have not found such evidence. Adjusting for confounding by indication poses a substantive challenge in studying prenatal SSRI use and ASD risk since maternal depression is also a plausible risk factor for ASD. In the Danish registers, accounting for this confounding by indication is a particular challenge. The published literature indicates a higher rate of maternal depression in other Nordic countries compared to what is found in the registers (Evans et al. 2001; Jimenez-Solem 2012; Josefsson et al. 2001; Kieler et al. 2012; Lund et al. 2009; Olesen et al. 2001), suggesting that depression prevalence as measured in our study (and in the other published studies using Danish register data) was underestimated. This underreporting is likely because the majority of people with depression in Denmark are diagnosed and treated by a general practitioner and not a psychiatrist, and thus the depression prevalence rate from the Danish Psychiatric Central Register (DPCR) is susceptible to under-reporting since many of these patients would not be included.
Several strategies can be employed to account for the confounding from maternal depression: (1) regression adjustment; (2) stratified analyses; (3) sibling analyses; and (4) negative controls; and (5) simulation analyses. However, each of these strategies is not without challenges. Regression adjustment and stratified analyses are both problematic in the face of underreporting of maternal depression and would lead to incomplete control for confounding by indication. Moreover, due to the small number of women in our sample with maternal depression (n = 77), the stratified effect estimates were imprecise and therefore not very informative.
Sibling analyses, similar to twin studies, can partially account for confounding from familial genetic or environmental sources, such as maternal depression (Susser et al. 2010). Sorensen et al. compared estimates in families with at least two full siblings, and interpreted the results as showing no independent SSRI effect, while acknowledging the sibling results may still be biased if there is non-shared confounding between siblings (Frisell et al. 2012). Negative controls are used to indicate that potential confounding may exist, if a result with a non-causal explanation is observed (Lipsitch et al. 2010). For example, if an association is found between the negative control (pre-conception SSRI) exposure and ASD risk, this result is not likely to be meaningful, since there is no mechanism for pre-conception SSRI usage to affect a child. Hviid et al. used this strategy and suggested this as possible evidence that no independent SSRI effect exists. However, the choice of negative controls can be complicated, since the negative control must not be in any way associated with the outcome. Given the complex relationship between SSRI usage and subsequent effects on depressive state as well as continuing SSRI usage, pre-conception SSRI usage may not be a wholly valid negative since it can still possibly be associated with ASD risk. In our sensitivity analyses estimating trimester-specific effects based on considering only those with exclusive medication use in a single trimester window as exposed had results that were comparable to those shown in Table 2 with similar magnitude effect estimates. This suggests that preconception and early first trimester effect estimates still persist.
Finally, we used a simulation-based approach to account for confounding by indication. Because of the underreporting of maternal depression, we used simulation analyses to approximate effect estimates, assuming a higher expected prevalence of depression. These analyses, described fully in the “Appendix”, in fact show more elevated effect estimates, and suggest that an independent effect of SSRI usage on ASD is possible. Furthermore, we also looked at the effect of unmeasured confounding to determine how robust our quantitative findings were (“Appendix”). We find it unlikely that such an unmeasured confounder or residual confounding, after adjustment for parental age, sex of child, history of maternal depression, and other SSRI indications, would be powerful enough to wholly explain our findings.
Selective serotonin reuptake inhibitors are known to cross the placenta (Borue et al. 2007), and there are several biologically plausible explanations for our findings involve serotoninergic pathways during development (Anderson et al. 2004; Cook et al. 1988; Lam et al. 2006; Whitaker-Azmitia 2001). Abnormalities in serotonin metabolism are one of the few consistent biological observations associated with ASD (Anderson et al. 1987) and several lines of evidence suggest that alterations in the serotonergic neurotransmitter system might be a mechanistic pathway leading to ASD (Anderson et al. 1987; Cook et al. 1988). Animal models have suggested adverse neurodevelopmental outcomes in the offspring associated with prenatal SSRI exposure (Vorhees et al. 1994) (Maciag et al. 2006). Also prenatal stress and certain serotonin transporter genotypes may have the combined effect of producing changes in social interaction and social interest in the offspring consistent with those observed in individuals with ASD (Jones and Klin 2009). Together these findings suggest that, mechanistically, prenatal exposure to SSRIs may operate directly on the developing brain.
The implications of reported associations between prenatal SSRI use and ASD risk need to be weighed against the evidence on health consequences of discontinuation of SSRI treatment. Direct associations between depression and developmental psychopathology have been hypothesized as operating through mechanisms involving the changing intrauterine environment or maternal stress response. Maternal hypothalamo–pituitary–adrenal (HPA) activity in response to psychological stress, which can be caused by depression, has been linked to adverse neurodevelopmental effects (Rice et al. 2007).
From a public health perspective, the epidemiologic evidence on the link between prenatal SSRI exposure and ASD risk must still be cautiously interpreted. In weighing potential risk tradeoffs involving discontinuation of SSRI treatment, it should be noted that the ASD prevention potential associated with prenatal SSRI exposure avoidance is modest. We estimated the population attributable fraction (Hanley 2001) based on observed adjusted OR of 1.9 for any prenatal SSRI exposure and the observed exposure prevalence (0.7 %) and that reported in the literature (3 %) (Bakker et al. 2008; Kieler et al. 2012). Based on the assumption that the associations are causal, this calculation suggests that between 0.6 and 1.7 % of the ASD cases in the population could be prevented if prenatal SSRI exposure was eliminated; an estimate quite similar to that of Rai et al. (2013). From a mechanistic perspective, however, these epidemiologic data add evidence to basic neurobiologic research (Bonnin and Levitt 2011) suggesting that maternal prenatal serotonin metabolism may be part of a causal pathway to ASD worth further study.
Considering the effect sizes being observed in the epidemiologic research and the challenges posed by confounding and misclassification, further epidemiologic investigations of prenatal SSRI exposure and ASD risk would best be undertaken when large sample sizes are available with good quality information on both exposure and indicating conditions. Also, given a history where mothers were, for decades, inappropriately blamed for causing their child’s condition, (Kanner 1968) additional attention should be given to how findings from this, and any future epidemiologic studies of prenatal SSRI and ASD risk, are communicated to the general public (Yudell 2013).
References
Anderson, G. M., Czarkowski, K., Ravski, N., & Epperson, C. N. (2004). Platelet serotonin in newborns and infants: Ontogeny, heritability, and effect of in utero exposure to selective serotonin reuptake inhibitors. Pediatric Research, 56, 418–422.
Anderson, G. M., et al. (1987). Whole blood serotonin in autistic and normal subjects. Journal of Child Psychology and Psychiatry, 28, 885–900.
Andrade, S. E., et al. (2008). Use of antidepressant medications during pregnancy: A multisite study. American Journal of Obstetrics and Gynecology, 198(194), e1–e5.
Atladottir, H. O., et al. (2009). Association of family history of autoimmune diseases and autism spectrum disorders. Pediatrics, 124, 687–694.
Atladottir, H. O., et al. (2010). Maternal infection requiring hospitalization during pregnancy and autism spectrum disorders. Journal of Autism and Developmental Disorders, 40, 1423–1430.
Bakker, M. K., Kerstjens-Frederikse, W. S., Buys, C. H., de Walle, H. E., & de Jong-van den Berg, L. T. (2010). First-trimester use of paroxetine and congenital heart defects: A population-based case–control study. Birth Defects Research Part A: Clinical and Molecular Teratology, 88, 94–100.
Bakker, M. K., Kolling, P., van den Berg, P. B., de Walle, H. E., & de Jong van den Berg, L. T. (2008). Increase in use of selective serotonin reuptake inhibitors in pregnancy during the last decade, a population-based cohort study from the Netherlands. British Journal of Clinical Pharmacology, 65, 600–606.
Bodnar, L. M., Siega-Riz, A. M., Simhan, H. N., Diesel, J. C., & Abrams, B. (2010). The impact of exposure misclassification on associations between prepregnancy BMI and adverse pregnancy outcomes. Obesity (Silver Spring), 18, 2184–2190.
Bolton, P. F., Pickles, A., Murphy, M., & Rutter, M. (1998). Autism, affective and other psychiatric disorders: Patterns of familial aggregation. Psychological Medicine, 28, 385–395.
Bonnin, A., & Levitt, P. (2011). Fetal, maternal, and placental sources of serotonin and new implications for developmental programming of the brain. Neuroscience, 197, 1–7.
Borue, X., Chen, J., & Condron, B. G. (2007). Developmental effects of SSRIs: Lessons learned from animal studies. International Journal of Developmental Neuroscience, 25, 341–347.
Brennan, P. A., Hammen, C., Andersen, M. J., Bor, W., Najman, J. M., & Williams, G. M. (2000). Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology, 36, 759–766.
Burstyn, I., Sithole, F., & Zwaigenbaum, L. (2010). Autism spectrum disorders, maternal characteristics and obstetric complications among singletons born in Alberta, Canada. Chronic Diseases in Canada, 30, 125–134.
Caplan, H. L., Cogill, S. R., Alexandra, H., Robson, K. M., Katz, R., & Kumar, R. (1989). Maternal depression and the emotional development of the child. British Journal of Psychiatry, 154, 818–822.
Carter, A. S., Garrity-Rokous, F. E., Chazan-Cohen, R., Little, C., & Briggs-Gowan, M. J. (2001). Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social–emotional problems and competencies. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 18–26.
Cook, E. H, Jr, Leventhal, B. L., & Freedman, D. X. (1988). Free serotonin in plasma: Autistic children and their first-degree relatives. Biological Psychiatry, 24, 488–491.
Cooper, W. O., Willy, M. E., Pont, S. J., & Ray, W. A. (2007). Increasing use of antidepressants in pregnancy. American Journal of Obstetrics and Gynecology, 196(544), e1–e5.
Croen, L. A., Grether, J. K., Yoshida, C. K., Odouli, R., & Hendrick, V. (2011). Antidepressant use during pregnancy and childhood autism spectrum disorders. Archives of General Psychiatry, 68, 1104–1112.
Daniels, J. L., et al. (2008). Parental psychiatric disorders associated with autism spectrum disorders in the offspring. Pediatrics, 121, e1357–e1362.
Deave, T., Heron, J., Evans, J., & Emond, A. (2008). The impact of maternal depression in pregnancy on early child development. BJOG, 115, 1043–1051.
Durkin, M. S., et al. (2010). Socioeconomic inequality in the prevalence of autism spectrum disorder: Evidence from a US cross-sectional study. PLoS One, 5, e11551.
Evans, J., Heron, J., Francomb, H., Oke, S., & Golding, J. (2001). Cohort study of depressed mood during pregnancy and after childbirth. BMJ, 323, 257–260.
Frisell, T., Oberg, S., Kuja-Halkola, R., & Sjolander, A. (2012). Sibling comparison designs: Bias from non-shared confounders and measurement error. Epidemiology, 23, 713–720.
Giarelli, E., et al. (2010). Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disability and Health Journal, 3, 107–116.
Gislason, G. H., et al. (2006). Long-term compliance with beta-blockers, angiotensin-converting enzyme inhibitors, and statins after acute myocardial infarction. European Heart Journal, 27, 1153–1158.
Hanley, J. A. (2001). A heuristic approach to the formulas for population attributable fraction. Journal of Epidemiology and Community Health, 55, 508–514.
Hanley, G. E., Brain, U., & Oberlander, T. F. (2013). Infant developmental outcomes following prenatal exposure to antidepressants, and maternal depressed mood and positive affect. Early Human Development, 89, 519–524.
Huot, R. L., Brennan, P. A., Stowe, Z. N., Plotsky, P. M., & Walker, E. F. (2004). Negative affect in offspring of depressed mothers is predicted by infant cortisol levels at 6 months and maternal depression during pregnancy, but not postpartum. Annals of the New York Academy of Sciences, 1032, 234–236.
Hviid, A., Melbye, M., & Pasternak, B. (2013). Use of selective serotonin reuptake inhibitors during pregnancy and risk of autism. New England Journal of Medicine, 369, 2406–2415.
Jimenez-Solem, E., et al. (2012). Exposure to selective serotonin reuptake inhibitors and the risk of congenital malformations: A nationwide cohort study. BMJ Open, 2, 1–9.
Jimenez-Solem, E., et al. (2013). SSRI use during pregnancy and risk of stillbirth and neonatal mortality. American Journal of Psychiatry, 170, 299–304.
Jones, W., & Klin, A. (2009). Heterogeneity and homogeneity across the autism spectrum: The role of development. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 471–473.
Josefsson, A., Berg, G., Nordin, C., & Sydsjo, G. (2001). Prevalence of depressive symptoms in late pregnancy and postpartum. Acta Obstetricia et Gynecologica Scandinavica, 80, 251–255.
Kaae, J., Boyd, H. A., Hansen, A. V., Wulf, H. C., Wohlfahrt, J., & Melbye, M. (2010). Photosensitizing medication use and risk of skin cancer. Cancer Epidemiology Biomarkers & Prevention, 19, 2942–2949.
Kanner, L. (1968). Autistic disturbances of affective contact. Acta Paedopsychiatr, 35, 100–136.
Kieler, H., et al. (2012). Selective serotonin reuptake inhibitors during pregnancy and risk of persistent pulmonary hypertension in the newborn: Population based cohort study from the five Nordic countries. BMJ, 344, d8012.
Lam, K. S., Aman, M. G., & Arnold, L. E. (2006). Neurochemical correlates of autistic disorder: A review of the literature. Research in Developmental Disabilities, 27, 254–289.
Larsson, H. J., et al. (2005). Risk factors for autism: Perinatal factors, parental psychiatric history, and socioeconomic status. American Journal of Epidemiology, 161, 916–925. (discussion 926–8).
Lauritsen, M. B., et al. (2010). Validity of childhood autism in the Danish Psychiatric Central Register: Findings from a cohort sample born 1990–1999. Journal of Autism and Developmental Disorders, 40, 139–148.
Lee, D., Majumdar, S. R., Lipton, H. L., Soumerai, S. B., Hennessy, S., & Davis, R. L. (2013). Special applications of pharmacoepidemiology. In B. L. Strom & S. E. Kimmel (Eds.), Textbook of pharmacoepidemiology (pp. 399–445). Philadelphia: Wiley.
Lin, D. Y., Psaty, B. M., & Kronmal, R. A. (1998). Assessing the sensitivity of regression results to unmeasured confounders in observational studies. Biometrics, 54, 948–963.
Lipsitch, M., Tchetgen Tchetgen, E., & Cohen, T. (2010). Negative controls: A tool for detecting confounding and bias in observational studies. Epidemiology, 21, 383–388.
Lund, N., Pedersen, L. H., & Henriksen, T. B. (2009). Selective serotonin reuptake inhibitor exposure in utero and pregnancy outcomes. Archives of Pediatrics and Adolescent Medicine, 163, 949–954.
Maciag, D., et al. (2006). Neonatal antidepressant exposure has lasting effects on behavior and serotonin circuitry. Neuropsychopharmacology, 31, 47–57.
Moth, G., Schiotz, P. O., & Vedsted, P. (2008). A Danish population-based cohort study of newly diagnosed asthmatic children’s care pathway: Adherence to guidelines. BMC Health Services Research, 8, 130.
Olesen, C., Thrane, N., Nielsen, G. L., Sorensen, H. T., & Olsen, J. (2001). A population-based prescription study of asthma drugs during pregnancy: Changing the intensity of asthma therapy and perinatal outcomes. Respiration, 68, 256–261.
Olsen, L. R., Mortensen, E. L., & Bech, P. (2004). Prevalence of major depression and stress indicators in the Danish general population. Acta Psychiatrica Scandinavica, 109, 96–103.
Rai, D., Lee, B. K., Dalman, C., Golding, J., Lewis, G., & Magnusson, C. (2013). Parental depression, maternal antidepressant use during pregnancy, and risk of autism spectrum disorders: Population based case–control study. BMJ, 346, f2059.
Ramos, E., St-Andre, M., Rey, E., Oraichi, D., & Berard, A. (2008). Duration of antidepressant use during pregnancy and risk of major congenital malformations. British Journal of Psychiatry, 192, 344–350.
Rice, F., Jones, I., & Thapar, A. (2007). The impact of gestational stress and prenatal growth on emotional problems in offspring: A review. Acta Psychiatrica Scandinavica, 115, 171–183.
Schendel, D., & Bhasin, T. K. (2008). Birth weight and gestational age characteristics of children with autism, including a comparison with other developmental disabilities. Pediatrics, 121, 1155–1164.
Schernhammer, E., Hansen, J., Rugbjerg, K., Wermuth, L., & Ritz, B. (2011). Diabetes and the risk of developing Parkinson’s disease in Denmark. Diabetes Care, 34, 1102–1108.
Sorensen, M. J., et al. (2013). Antidepressant exposure in pregnancy and risk of autism spectrum disorders. Clinical Epidemiology, 5, 449–459.
Susser, E., Eide, M. G., & Begg, M. (2010). Invited commentary: The use of sibship studies to detect familial confounding. American Journal of Epidemiology, 172, 537–539.
Vorhees, C. V., Acuff-Smith, K. D., Schilling, M. A., Fisher, J. E., Moran, M. S., & Buelke-Sam, J. (1994). A developmental neurotoxicity evaluation of the effects of prenatal exposure to fluoxetine in rats. Fundamental and Applied Toxicology, 23, 194–205.
Weikum, W. M., Oberlander, T. F., Hensch, T. K., & Werker, J. F. (2012). Prenatal exposure to antidepressants and depressed maternal mood alter trajectory of infant speech perception. Proceedings of the National Academy of Sciences of the USA, 109(Suppl 2), 17221–17227.
Whitaker-Azmitia, P. M. (2001). Serotonin and brain development: Role in human developmental diseases. Brain Research Bulletin, 56, 479–485.
Yudell, M., Tabor, H. K., Dawson, G., Rossi, J., Newschaffer, C. (2013). Priorities for autism spectrum disorders risk communication and ethics. Autism, 17(6), 701–722.
Acknowledgments
We thank Karyn Heavner, Ph.D., for assisting with data management, and implementation of Monte Carlo simulations. Fees to access Denmark’s national’s registers were funded by Drexel University Department of Epidemiology and Biostatistics (Dr. Newschaffer). Dr. Gidaya’s travel was funded in part through a travel award through Drexel University.
Conflict of interest
All authors and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
We used simulation analyses to explore the effects of under-reporting of SSRI use and depression in the register. For each simulation, a Monte Carlo approach was used simulating 1,000 datasets to randomly assign an unexposed mother to being exposed from a normal distribution. From each of the 1,000 simulated datasets we obtained the odds ratio and then took 1,000 samples from each odds ratio normal distribution. We then took the median effect estimate from these 1,000,000 samples as the odds ratio and the 2.5 and 97.5 % percentile to estimate the 95 % confidence interval. Models used in the simulations were unconditional logistic regressions adjusting for the matching variables as covariates.
Because the observed SSRI exposure prevalence (0.7 %) was below published estimates for other Nordic countries (Kieler et al. 2012) we completed simulations increasing the observed prevalence of SSRI exposure from 0.7 to 3 %. We assumed under-reporting was non-differential with respect to outcome by keeping sensitivity and specificity equal in case and control groups. Specificity was assumed to be 100 %, because it is unlikely a prescription for an SSRI would be documented in the register when none was given, and sensitivity was assumed to be 26 % because that corresponds to a true SSRI use prevalence of 3 %.
Simulations also examined the impact of under-ascertainment of maternal depression (which would lead to incomplete control for confounding by indication) because published estimates of the prevalence of maternal depression during pregnancy in Europe range from 3 to 17 % (Evans et al. 2001; Josefsson et al. 2001; Lund et al. 2009; Olsen et al. 2004)—higher than our observed prevalence of 0.6 %. Simulations were done increasing maternal depression prevalence to 5 % and then 15 %. Maternal depression under-reporting was assumed to be non-differential with respect to ASD case status because depression is assessed prior to the birth of the child and, thus, could not be influenced by subsequent diagnosis of the offspring. Specificity was assumed to be 100 %; in other words, all mothers truly without a history of depression where assumed to be correctly classified as without depression in the register, and sensitivity was set to 4.7 % to reflect the under-reporting needed where the true depression prevalence of 15 %.
Table 4 shows the results from simulation analyses exploring the influence of misclassification. The first row presents effect estimates and confidence bounds for any prenatal SSRI exposure from simulations assuming increased SSRI prevalence and non-differential misclassification as described above. Estimates for the full sample were very close to the comparable Model 1 adjusted (parental age and sex of the child) estimate in Tables 2, suggesting that exposure misclassification is unlikely to have strongly influenced results. The following rows show results from simulations investigating the potential effects of non-differential under-reporting of maternal depression. By increasing the assumed depression prevalence to 5 %, the pooled effect estimate, 2.2 (95 % CI 1.9–2.4), is extremely close to the comparable Model 1 adjusted (parental age and sex of the child) estimates shown in Table 2. At 15 % assumed depression prevalence, the SSRI effect is only moderately attenuated. Under the assumed 15 % depression prevalence scenario we also estimated depression-stratified effects. A positive association was observed in both strata, though the effect was smaller among mothers with depression, with median adjusted odds ratios and confidence intervals of 1.4 (95 % CI 0.9–2.4) and 2.1 (1.5–3.0), respectively. These results suggest that the original restriction approach to controlling for confounding by indication may have been influenced by depression misclassification.
Lastly, we performed a sensitivity analysis to determine how robust our quantitative estimates were to unmeasured confounding. Following the method of Lin et al. (1998) we assumed a binary confounder U existed such that U increased the risk of ASD, and that U was more prevalent in SSRI-exposed mothers than in unexposed mothers. Given the strength of relationship of U with ASD, and the prevalences of U in the exposed and unexposed, it is therefore possible to estimate odds ratios that are corrected for this unmeasured confounder U. We estimated corrected odds ratios over a range of plausible parameters.
In our analysis to measure the impact of unmeasured confounding, our results appear to be moderately robust. For example, if there were an unmeasured confounder U that doubled the risk of ASD, and had 50 % prevalence in SSRI-exposed mothers and only 5 % prevalence in SSRI-unexposed mothers, the corrected OR would still be 1.3 (1.0, 1.6). Similarly, if U doubled the risk of ASD, and was 40 % prevalent in SSRI-exposed mothers and only 10 % prevalent in SSRI-unexposed mothers, the corrected OR would be 1.4 (1.1, 1.8). We find it unlikely that such an unmeasured confounder or residual confounding, after adjustment for parental age, sex of child, history of maternal depression, and other SSRI indications, would be powerful enough to wholly explain our findings.
Rights and permissions
About this article
Cite this article
Gidaya, N.B., Lee, B.K., Burstyn, I. et al. In Utero Exposure to Selective Serotonin Reuptake Inhibitors and Risk for Autism Spectrum Disorder. J Autism Dev Disord 44, 2558–2567 (2014). https://doi.org/10.1007/s10803-014-2128-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-014-2128-4