Abstract
Infants at risk for autism spectrum disorders (ASD) may have difficulty integrating smiles into initiating joint attention (IJA) bids. A specific IJA pattern, anticipatory smiling, may communicate preexisting positive affect when an infant smiles at an object and then turns the smile toward the social partner. We compared the development of anticipatory smiling at 8, 10, and 12 months in infant siblings of children with ASD (high-risk siblings) and without ASD (low-risk siblings). High-risk siblings produced less anticipatory smiling than low-risk siblings, suggesting early differences in communicating preexisting positive affect. While early anticipatory smiling distinguished the risk groups, IJA not accompanied by smiling best predicted later severity of ASD-related behavioral characteristics among high-risk siblings. High-risk infants appear to show lower levels of motivation to share positive affect with others. However, facility with initiating joint attention in the absence of a clear index of positive affective motivation appears to be central to the prediction of ASD symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The capacity to refer to objects and events within a social context (referential communication) typically emerges during the first year of life and is an important precursor of later social competence (Mundy et al. 2007). Referential communication is central to the development of social and language abilities and tends to be impaired in children with symptoms of Autism Spectrum Disorders (ASD; Dawson et al. 2004). Infant-initiated joint attention (IJA) is an early form of referential communication that develops toward the end of the first year of life and becomes more common in the second year. Initiating joint attention may involve the communication of positive affect, as when infants smile in the course of an IJA episode (Venezia et al. 2004). Both IJA and the expression of positive affect are areas of impairment in children with ASD (e.g., Adamson et al. 2009; Dawson et al. 2004; Mundy and Vaughan 2001). The current paper examines smiling occurring in conjunction with IJA to refine our understanding of the IJA deficits seen in children at risk for ASD.
Joint Attention and Affect in Typical Development
Joint attention is the coordination of attention between social partners and objects to share an experience (Bakeman and Adamson 1984). By 12 months of age, typically developing infants initiate joint attention through the use of gaze and gesture to direct the attention of a social partner to a shared experience (Mundy et al. 2007). Displays of positive affect (i.e., smiling) are likely to occur during an infant’s communicative gestures (e.g., offers) to the mother, particularly if the gestures involve gaze at the mother (Messinger and Fogel 1998). Infants also tend to produce more smiling when there is an attentive audience (e.g., a caregiver) for their smiling (Jones et al. 1991; Jones and Hong 2005; Jones and Raag 1989). Infants tend to display more smiles with accompanying gaze when they are engaged in active toy play and when their mother (Jones and Hong 2005) or another social partner (Jones and Raag 1989) is attentive and responds socially.
The timing of smiles in relation to gaze at the social partner during an IJA episode defines IJA smiling patterns and their presumptive meaning. Reactive smiles occur when an infant turns a gaze from an object to a social partner and then smiles (i.e., the smile is in “reaction” to gazing at the partner). Anticipatory smiles, on the other hand, occur when an infant first gazes at an object, smiles, then turns that smile to a social partner (i.e., the smile “anticipates” the gaze in time; Parlade et al. 2009). Anticipatory smiles have been studied in typically developing infants and emerge between 6 and 12 months of age (Jones et al. 1991; Jones and Hong 2001, 2005; Parlade et al. 2009; Venezia et al. 2004). Evidence suggests anticipatory smiles may be voluntary communicative signals of preexisting positive emotion (Venezia et al. 2004), while reactive smiles appear to be a response to gazing at the social partner.
Anticipatory smiling shows unique increases with development. In an infant-examiner assessment for joint attention behaviors (Early Social Communication Scales; Mundy et al. 2003), infants’ anticipatory smiles increased from 8 to 10 months and stabilized between 10 and 12 months, a developmental pattern unique to anticipatory smiling (Venezia et al. 2004). The frequency of reactive smiles and overall IJA episodes did not change over time, and the overall proportion of infant smiles during IJA episodes also did not change between 8 and 12 months of age. Parlade et al. (2009) found a similar developmental pattern in typically developing infants’ use of anticipatory smiles, with greater anticipatory smiling shown at 12 months than at 9 months. Again, there was no change found in infants’ use of reactive smiles.
Associations between anticipatory smiling in the first year and later social and emotional outcomes have been found in typically developing children (Parlade et al. 2009). Early anticipatory smiling was positively related to emotional expressivity and parent-reported social competence at 30 months. However, reactive smiling and overall IJA frequency were not similarly associated with social competence. These findings suggest that anticipatory smiling may be uniquely related to later social competencies, an area particularly relevant for children at risk for ASD.
Joint Attention and Affect in Autism Spectrum Disorders
Autism Spectrum Disorders (ASD) are characterized by social and communication impairments, as well as the presence of restricted or stereotyped patterns of behavior, interests, and activities. Joint attention impairments are a core deficit in ASD (Dawson et al. 2004), and children diagnosed with ASD display fewer instances of IJA than typically developing children or children with other developmental delays (e.g., Mundy et al. 1986, 1990). IJA impairments in children who go on to be diagnosed with ASD are usually evident from 1 year of age (Dawson et al. 2004; Toth et al. 2006). Deficits in IJA are associated with poorer outcomes, including social and language difficulties, in children with ASD (Dawson et al. 2004; Mundy et al. 2007).
Children with ASD tend to exhibit lower levels of smiling, including smiles occurring with joint attention, than other children. They are less likely to combine smiles with eye contact while interacting both with their mothers and researchers (Dawson et al. 1990; Joseph and Tager-Flusberg 1997; Kasari et al. 1990). With respect to early development, lower levels of smiling in combination with gazing at the examiner are seen by 18 months in children with an eventual ASD diagnosis (Ozonoff et al. 2010). Difficulties in combining smiling with IJA suggest that children with ASD have difficulty sharing affective experiences with others. Indeed, sharing enjoyment is incorporated into possible symptomatology in the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM–IV–TR; American Psychiatric Association 2000) and observed behaviors during the Autism Diagnostic Observation Schedule (ADOS), an assessment of ASD-relevant behaviors (Lord et al. 1999). However, the timing of the coordination of IJA with positive affect, as in IJA with anticipatory smiling, has not been well-studied in the context of ASD.
Siblings at High Risk for ASD
Prospective studies of high-risk siblings (younger siblings of children diagnosed with ASD) allow for the examination of early developmental markers of ASD, which is not typically diagnosed until around 3 years of age. Recent estimates of the sibling recurrence rate of ASD indicate that approximately 1 in 5 high-risk siblings go on to an ASD outcome (Ozonoff et al. 2011). Moreover, a higher percentage of high-risk siblings without ASD demonstrate sub-clinical ASD deficits and other difficulties with communication than typically developing children (Landa and Garrett-Mayer 2006; Goldberg et al. 2005; Yirmiya et al. 2006, 2009). There is evidence that high-risk siblings produce fewer joint attention behaviors than siblings of children with no familial risk for ASD (low-risk siblings; e.g., Cassel et al. 2007; Goldberg et al. 2005; Presmanes et al. 2007; Rozga et al. 2011; Yirmiya et al. 2006) and spend less time gazing toward an object being referenced by a videotaped partner than controls (Bedford et al. 2012). In a recent study, Ibañez et al. (2012) examined the developmental trajectories of IJA in high- and low-risk siblings and found that high-risk siblings displayed lower levels of IJA at 8 months. In high-risk siblings, these IJA levels were associated with later ASD symptomatology. Neither Ibañez et al. (2012) nor others have examined anticipatory smiling and other IJA smiling patterns in high-risk siblings.
Current Study
The current study aimed to further specify IJA deficits seen in high-risk siblings by examining the integration of IJA with displays of positive affect. We compared the development of IJA smiling patterns (anticipatory smiling, reactive smiling, and IJA without smiling) in high-risk and low-risk infant siblings. IJA smiling patterns were examined within the context of initiating joint attention episodes during the Early Social Communication Scales (ESCS) at 8, 10, and 12 months of age. These smiling types were then used to predict ASD symptom severity during the ADOS at 30 months of age. Based on evidence from high-risk and typically developing children, we hypothesized that high-risk siblings would exhibit lower levels of anticipatory smiling than low-risk siblings and hypothesized that levels of anticipatory smiling within the high-risk group would predict later ASD symptomatology. We did not have hypotheses for group differences in reactive smiling or IJA without smiling, nor did we hypothesize associations between those IJA patterns and later symptomatology.
Methods
Participants
Participants were the infant siblings of children with a diagnosed Autism Spectrum Disorder (ASD; high-risk siblings, n = 56, 36 male) or children with no evidence of ASD (low-risk siblings, n = 26, 12 male) who were enrolled in a larger longitudinal study of child development, the Sibling Studies Measuring Infant Learning and Emotion (Sib SMILE) Project. High-risk siblings had at least one older sibling with a community diagnosis of ASD, which was confirmed upon study enrollment by administration of the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2000) and clinical diagnosis by a licensed clinical psychologist. Low-risk siblings had older siblings with no evidence of ASD, confirmed by a score lower than a conservative cutoff of 9 on the Social Communication Questionnaire (Berument et al. 1999), and no family history of ASD. High-risk siblings (White/Caucasian = 35.7 %, Hispanic/Latino = 51.8 %, Other = 12.5 %) did not differ from low-risk siblings (White/Caucasian = 37.0 %, Hispanic/Latino = 40.7 %, Other = 22.2 %) in ethnicity, χ2(2) = 1.57, p = .46.
Participants included those in the Ibañez et al. (2012) study of IJA (high-risk n = 40, low-risk n = 21) and an additional five low-risk and 16 high-risk infants. Smiling during IJA was not reported in Ibañez et al. The current study focused on IJA smiling types during the Early Social Communication Scales at 8, 10, and 12 months of age—participants had ESCS data at least one of these ages—and ASD-relevant outcomes. The ADOS was administered at 30 months of age and used to calculate levels of ASD symptom severity. Of the 82 participants, 63 were administered the ADOS; of the 56 high-risk siblings, 41 were administered the ADOS. Clinical best-estimate diagnosis was made at 36 months (high-risk n = 42, low-risk n = 21). Clinical best-estimate diagnosis was informed by the 30 month ADOS (high-risk n = 42, low-risk n = 21), the 36 month Mullen Scales of Early Learning (MSEL; high-risk n = 39, low-risk n = 19), and the 36 month Autism Diagnostic Interview-Revised (ADI-R; Lord et al. 1994; high-risk n = 34, low-risk n = 18). Three participants (2 high-risk, 1 low-risk) received clinical-best estimate diagnosis on the basis of the ADOS alone without data from the ADI or MSEL. Expressive and receptive language on the MSEL at 24 and 36 months of age were also used as measures of language outcome and to characterize the sample. See Table 1 for characterization of the study sample.
Procedure and Measures
This study examined IJA smiling patterns (i.e., anticipatory smiling, reactive smiling, and no smiling) within the ESCS, which was administered at infants’ 8-, 10-, and 12-month visits. The relationship between these smiling patterns and later ASD severity (measured during the ADOS) at 30 months was then examined.
Early Social Communication Scales (ESCS)
The ESCS (Mundy et al. 2003) is a semi-structured assessment of infants’ nonverbal communication abilities, including joint attention, behavioral requesting, and social interaction behaviors. During the ESCS protocol, an infant is seated on the caregiver’s lap across from an examiner, who presents the infant with a series of toys, creating opportunities for the infant to initiate joint attention behaviors. After presenting and activating a toy, the examiner remains attentive and responds to the infant’s joint attention bids briefly. The current study focused on IJA bids previously coded during the ESCS (see Ibañez et al. 2012). Instances of IJA with the examiner (e.g., the infant making eye contact, pointing, and showing) were coded by coders trained to reliability and blind to infants’ risk group status.
IJA Smiling Patterns
Patterns of IJA smiling were assessed within the context of IJA episodes during the ESCS. IJA episodes (those including gaze) from coded ESCS assessments at 8, 10, and 12 months were examined and coded for smiling. Each episode was examined to determine if a smile occurred, using Facial Action Coding System (FACS; Ekman and Friesen 1978) criteria to determine smiles (presence of Action Unit 12, raised lip corners). For episodes with a smile, the timing of the smile within the IJA episode was then assessed. Videos of the IJA episodes were viewed in slow motion and frame by frame to allow for more accurate coding. A smile was coded if the gaze and smile overlapped in time, and it was then categorized as either an anticipatory or reactive smile. Anticipatory smiles were coded when the infant first gazed at the object, smiled while looking at the object, then gazed at the examiner with an already smiling face (i.e., the smile clearly preceded the gaze). Reactive smiles were coded when an infant gazed at an object, gazed up to the examiner (without a smile present), and then smiled after establishing gaze with the examiner. If the infant did not smile during the gaze portion of the interaction, a code of IJA without smiling was given. Smiles were coded by a primary coder blind to infants’ risk group status, and 22 % of tapes were also coded by a second coder for reliability; reliability assessments yielded 89 % mean agreement with a mean κ = .78.
As ESCS assessments were not uniform in length, rate per minute of IJA smiling types were used in analyses. This procedure controlled for varying ESCS length (and therefore potential opportunities to produce IJA) and the varying numbers of instances of IJA produced by infants. Rates per minute (rpm) for each pattern of IJA smiling were calculated by dividing the total number of instances of anticipatory smiling, reactive smiling, and IJA without smiling by the total length of the ESCS in minutes. See Table 1 for descriptive statistics for 8, 10, and 12 month data.
ASD Outcome
The Autism Diagnostic Observation Schedule (ADOS; Lord et al. 1999) is a play-based observational measure during which an examiner administers behavioral presses structured to elicit ASD-relevant behaviors in areas of social interaction, communication, and play; this assessment was administered at 30 months. Children received either Module 1 (n = 36) or Module 2 (n = 27) based on language level exhibited at the time of the 30-month assessment. Risk groups did not differ with respect to which ADOS Module was administered, χ 2(1) = .35, p = .55. High-risk siblings who completed (n = 41) and did not complete (n = 15) an ADOS did not differ on any of the IJA smiling patterns, ps > .27.
To provide a continuous measure of ASD symptomatology, ASD severity scores were calculated for each child (low-risk n = 22, high-risk n = 41) from ADOS scores based on Gotham et al. (2009) criteria. This resulted in calibrated severity scores ranging from 1 to 10 that accounted for the child’s age and language level. High-risk siblings (M = 3.07, SD = 1.86) had higher ASD severity scores than low-risk siblings (M = 1.55, SD = .80), t(61) = −3.66, p = .001. Ten high-risk siblings had calibrated severity scores at or above the cutoff for ASD (a score of 4 or above), and six had scores at or above the cutoff for autism (a score of 6 or above). No low-risk siblings had scores at or above the cutoffs for ASD or autism.
Clinical diagnosis procedures were performed at 36 months (n = 63). Among the 56 high-risk siblings, there were no differences in IJA smiling patterns between those who received a clinical best-estimate diagnosis procedure (n = 42) and those who did not (n = 14). The 30-month administration of the ADOS, the 36-month administration of the Autism Diagnostic Interview-Revised (ADI-R; Lord et al. 1994), and the 36-month administration of the MSEL were used to inform the DSM-IV-based clinical best-estimate diagnosis from a licensed psychologist. Twelve high-risk siblings received a diagnosis of ASD at 36 months, and no low-risk siblings were diagnosed with ASD.
Language Development Outcome
The Mullen Scales of Early Learning (MSEL; Mullen 1995) was administered at 24 months (low-risk n = 13, high-risk n = 43) and 36 months (low-risk n = 20, high-risk n = 39). Scales measuring non-verbal problem solving (visual reception), fine motor abilities, and expressive and receptive language were administered; t scores for expressive and receptive language scales were used in the current study. At 24 months, high-risk siblings (M = 45.74, SD = 12.57) did not differ in expressive language scores from low-risk siblings (M = 52.31, SD = 8.87), t(54) = 1.75, p = .09, or differ in receptive language scores (M = 46.00, SD = 12.07) from low-risk siblings (M = 51.23, SD = 9.92), t(54) = 1.42, p = .16. At 36 months, high-risk siblings (M = 48.26, SD = 9.41) had lower expressive language scores than low-risk siblings (M = 53.55, SD = 9.83), t(57) = 2.02, p = .049, and lower receptive language scores (M = 43.59, SD = 10.27) than low-risk siblings (M = 51.40, SD = 8.70), t(57) = 2.91, p = .005. When children diagnosed with ASD at 36 months were removed from analyses of 36 month MSEL, high-risk siblings without ASD (n = 29, M = 49.24, SD = 8.93) did not differ in expressive language scores from low-risk siblings (n = 19, M = 53.53, SD = 10.10), t(46) = 1.54, p = .13, but continued to have lower receptive language scores (M = 45.21, SD = 9.18) than low-risk siblings (M = 50.89, SD = 8.63), t(46) = 2.15, p < .05.
Results
Analytic Approach
Correlations were used to examine the relationships between IJA smiling patterns. Hierarchical linear modeling (HLM; Raudenbush and Bryk 2002; Singer and Willett 2003) was used to compare the development of IJA smiling patterns (anticipatory smiling, reactive smiling, and IJA without smiling) in high-risk and low-risk siblings from 8 to 12 months of age. In these models, linear and quadratic representations of age were first examined as predictors at the observation level, and risk group status (high-risk group or low-risk group) was then examined as a predictor at the individual level. The linear age variable (time) was referenced to 8 months (the age of the first observation and an age coincident with the emergence of anticipatory smiling), and assigned values such that age = 0, 2, 4 corresponded to ages 8, 10, and 12 months. The quadratic age variable (time 2) was calculated by squaring the centered linear age variable. Linear and quadratic age parameters were modeled as random effects when they exhibited significant variance between infants and were otherwise modeled as fixed effects. The effect of risk group status on random effects was then ascertained. Additional models using gender as a predictor were not significant, ps > .28. HLM modeling was then repeated after removing the 12 high-risk siblings who received an ASD diagnosis to determine the role of these children in the risk-group analyses. Deviance statistics and parameter estimates were used to determine if predictors were retained in final models. Full Information Maximum Likelihood was used in modeling to allow participants with missing data to contribute to the estimation of parameters.
Modeled intercept estimates of each smiling pattern from the hierarchical linear models were then correlated with ASD severity at 30 months to determine the relationship between each IJA pattern and later outcome. Intercept estimates for predictive analyses were provided under an Empirical Bayesian approach as implemented in Raudenbush et al. (2004). The calculation of these estimates is based on the premise that intercepts are distributed randomly and that their reliability is associated with both intra- and inter-individual stability of children’s data points (Raudenbush and Bryk 2002). For the sake of concreteness, outcome analyses were repeated with the observed 8 month values of each smiling pattern.
IJA Smiling Patterns
Anticipatory smiling and reactive smiling were correlated with one another in the full sample at 8 months, r(51) = .68, p < .001, but neither anticipatory smiling, r(51) = −.13, p = .37, nor reactive smiling, r(51) = .07, p = .61, were associated with IJA without smiling. Identical patterns were observed within each risk group. In high-risk siblings, anticipatory and reactive smiling were correlated at 8 months, r(34) = .40, p < .05, but neither anticipatory smiling, r(34) = .06, p = .74, nor reactive smiling, r(34) = .15, p = .41, were associated with IJA without smiling. In low-risk siblings, anticipatory and reactive smiling were correlated at 8 months, r(17) = .81, p < .001, but neither anticipatory smiling, r(17) = −.37, p = .15, nor reactive smiling, r(34) = −.11, p = .68, were associated with IJA without smiling.
Developmental Trajectories
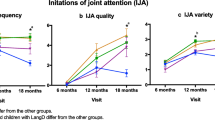
Descriptive statistics for anticipatory smiling, reactive smiling, and IJA without smiling rates per minute (used in analyses) are presented in Table 1, and group trajectories are presented in Figs. 1, 2 and 3. The intraindividual, or within subjects, variance in IJA smiling patterns (anticipatory, reactive, and no smiling) from 8 to 12 months was modeled at Level 1, while the interindividual, or between subjects, variance in IJA smiling patterns was modeled at Level 2 with group status included as a predictor; gender was also examined as a predictor but was not retained in final models as it was not significant. This was done separately for anticipatory smiling, reactive smiling, and IJA without smiling.
IJA with Anticipatory Smiling
The final model for anticipatory smiling included significant fixed linear and quadratic age terms. Intercepts exhibited significant random variance and group status was included in the final model as a significant predictor of the intercept. With the inclusion of group status as a predictor, model fit improved from previous models that did not include group status as a predictor, χ2(1, n = 82) = 7.94, p = .005 (see Table 2 for the final model summary). High-risk siblings exhibited lower intercepts than low-risk siblings, indicating that high-risk siblings had lower levels of anticipatory smiling than low-risk siblings. As group status did not significantly predict linear or quadratic age terms these terms were not included in the final model. These results indicate that high-risk siblings had lower levels of anticipatory smiling at 8 months and suggest that these differences persisted over time (see Fig. 1).
IJA with Reactive Smiling
The final model for IJA with reactive smiling included significant fixed effects of linear and random effects of quadratic age. Intercepts exhibited significant random variance, but group status was not retained as a predictor in the final model as model fit did not improve with the inclusion of group status, χ2(1, n = 82) = 2.21, p = .13 (see Table 2 for final model summary). These results indicate that risk groups exhibited similar levels of reactive smiling and similar developmental trajectories (see Fig. 2).
IJA Without Smiling
The final model for IJA without smiling did not include significant terms for linear or quadratic age. Intercepts exhibited significant random variance, but model fit did not improve with the inclusion of group status as a predictor, χ2(1, n = 82) = 1.75, p = .18, and group status was not retained in the final model (see Table 2 for final model summary). These results indicate that risk groups showed similar levels of IJA without smiling, and levels of IJA without smiling did not change with age (see Fig. 3).
Role of ASD Diagnosis
To ascertain the role of diagnosed children, final models for anticipatory smiling, reactive smiling, and IJA without smiling were re-run with children diagnosed with ASD removed from the analyses. For anticipatory smiling, group status remained a significant predictor of the intercept, β 01 = −.16, SE = .06, p = .01, indicating that high-risk siblings without an ASD diagnosis exhibited lower levels of anticipatory smiling than low-risk siblings. With siblings with an eventual ASD diagnosis removed, group status was not a significant predictor of either the intercept for reactive smiling, β 01 = −.07, SE = .06, p = .27, or the intercept for IJA without smiling, β 01 = −.09, SE = .13, p = .51.
Associations with Outcome
ASD Severity
We examined associations of ASD severity first with intercept estimates and then with observed 8 month values of each IJA pattern (see Table 3). Only analyses for the high-risk group are reported, due to the lack of variability in ASD severity among low-risk siblings. In high-risk siblings, there were no associations between calibrated ASD severity scores and anticipatory or reactive smiling. However, in high-risk siblings, both intercept, r(39) = −.32, p = .04, and observed 8 month levels of IJA without smiling, r(26) = −.57, p = .002, were associated with ASD severity (also see Fig. 4).
Associations between IJA without smiling at 8 months and ASD severity at 30 months in high-risk siblings. Note. ASD severity reflects calibrated ADOS severity scores (Gotham et al. 2009). The cutoff for ASD is a severity score of 4 or above, and the cutoff for autism is a score of 6 or above
Language Development
Bayesian intercept estimates and observed 8 month values of each IJA pattern were examined in relation to participants’ expressive and receptive language scores at 24 and 36 months. There were no associations between IJA smiling patterns and either expressive or receptive language scores in either low-risk or high-risk siblings at 24 months, all ps > .16, or at 36 months, all ps > .12.
Discussion
Difficulties in initiating joint attention (IJA) are a core feature of ASD and frequently characterize infant siblings at high risk for ASD (Cassel et al. 2007; Dawson et al. 2004; Ibañez et al. 2012). Children diagnosed with ASD also tend to display less positive affect than children without ASD (Joseph and Tager-Flusberg 1997; Kasari et al. 1990), but little is known about how high risk siblings use affect in the context of initiating joint attention. To further specify the content of the IJA deficits seen in children with ASD and high-risk infant siblings, we examined IJA that was and was not characterized by positive affect, and how these IJA smiling patterns were associated with later outcomes. This appears to be the first study to examine the timing of smiles and eye contact during IJA in the context of ASD risk, and to examine the relationship between early IJA smiling patterns and later ASD symptom severity. High-risk siblings showed an early deficit in anticipatory smiling. Among high-risk siblings, however, only IJA without smiling was associated with later ASD severity scores.
In both high- and low-risk siblings, there was developmental change in anticipatory smiling between 8 and 12 months of age. Anticipatory smiling increased from 8 to 10 months, and the rate of change decreased between 10 and 12 months. This developmental pattern is similar to that found previously in typically developing children (Parlade et al. 2009; Venezia et al. 2004) and suggests a period of rapid emergence followed by a period of consolidation. Developmental trajectories of reactive smiling were similar to those of anticipatory smiling, while there was no change developmentally in IJA without smiling between 8 and 12 months. The inverted U shape characteristic of both IJA smiling patterns (see Figs. 1, 2) reflects a more general curvilinear pattern in the development of IJA, in which the development of language may contribute to perturbed IJA growth (Ibañez et al. 2012; Mundy et al. 2007). The findings suggest that previously documented developmental changes in overall IJA may be due to changes in IJA with smiling (anticipatory and reactive smiling), as IJA without smiling did not change between 8 and 12 months of age.
There were no risk group differences in baseline levels (i.e., intercept) or developmental trajectories (i.e., slope) of either reactive smiling or IJA without smiling. High-risk and low-risk siblings exhibited similar baseline levels of these IJA smiling patterns and similar trajectories from 8 to 12 months. As hypothesized, however, there were group differences in anticipatory smiling such that high-risk siblings exhibited lower levels of anticipatory smiling than low-risk siblings at baseline (8 months). High-risk siblings did not differ from low-risk siblings in developmental trajectories, thus group differences in anticipatory smiling appeared to persist across age. This indicates that high-risk siblings showed an early, continuing deficit in sharing positive affect across the first year.
The unique deficit seen in anticipatory smiling suggests that high-risk siblings may have particular difficulties coordinating early affect and gaze to share affective experiences through anticipatory smiling. The lack of group differences in reactive smiling indicates that high-risk infants have specific difficulties in sharing preexisting positive affect, underscoring the importance of the timing of the smile. Sharing preexisting positive affect with another person (as in anticipatory smiling) may be indicative of an infant’s developing understanding that one’s emotional experiences can be shared with others (Parlade et al. 2009; Venezia et al. 2004).
Even when high-risk siblings diagnosed with ASD were removed from analyses, high-risk siblings (without ASD) exhibited lower levels of anticipatory smiling than low-risk siblings. This persistent deficit in high-risk siblings both with and without ASD may be a characteristic of an emerging broader autism phenotype (BAP). The BAP refers to subclinical differences in traits and abilities seen in family members of individuals with ASD (Gerdts and Bernier 2011). Patterns similar to those observed in this study have been reported at 12 months among high-risk siblings without an eventual ASD diagnosis who were over-represented in clusters of infants exhibiting difficulties on the Autism Observation Scale for Infants (AOSI), which includes measures of affective response, coordination of gaze and action, and social-communicative behaviors (Georgiades et al. 2013). Differences in anticipatory smiling and related behaviors between high-risk siblings (including those without ASD) and low-risk siblings suggests the possibility that difficulties communicating preexisting positive affect to a social partner may characterize the early BAP.
Although risk group differences were found in early anticipatory smiling, contrary to our hypothesis, there was no association between anticipatory smiling and later ASD symptom severity. IJA without smiling was the most common pattern of IJA at every age in both risk groups. As anticipatory and reactive smiling occurred at lower frequencies than IJA without smiling, it is possible that these IJA smiling patterns were less stable predictors of later symptomatology than IJA without smiling. However, similar findings—in which behavioral and neurophysiological characteristics that distinguish high-risk and low-risk groups do not predict ASD-related outcomes among the high-risk siblings—have been reported previously. For example, early differences in infants’ gaze patterns—less fixation to the eyes relative to the mouth in a mother-infant interaction at 6 months—were characteristic of a high-risk group, but this pattern was not associated with later ASD outcome (Young et al. 2009). High-risk siblings with and without a later diagnosis of ASD have also been found to exhibit higher rates of repetitive and stereotyped movements than low-risk siblings (Damiano et al. 2013). Likewise, early patterns of neurophysiological functioning that distinguish high-risk and low-risk siblings exist even when excluding children who proceed to an ASD diagnosis (Tierney et al. 2012). The current results, then, add to a growing literature in which characteristics that distinguish high-risk siblings in the first year of life are not necessarily associated with later symptomatology.
There were no differences between high- and low-risk siblings in IJA without smiling. Within the high-risk group, however, IJA without smiling was associated with later ASD severity. Specifically, infants with lower levels of IJA without smiling at 8 months exhibited higher levels of later ASD symptomatology. IJA without smiling was not associated with either anticipatory smiling or reactive smiling, indicating that this non-affective pattern of IJA may index a different psychological process than IJA coordinated with smiling. Initiating joint attention in a neutral behavioral context may primarily index the social referencing function of IJA. That is, infants appear to be seeking information from a social partner during IJA without smiling rather than using IJA to communicate preexisting positive affect or using IJA to make positive emotional connection. An infant’s use of IJA that is not affectively motivated may index an early behavioral ability that can be beneficially employed for a range of non-affective social functions. In typically developing infants, time spent in neutral affect expression may allow for cognitive activity to be devoted to communicative signals relevant to learning (e.g., language learning; Bloom et al. 1988; Bloom and Capatides 1987). The ability to share attention in a more neutral context, rather than sharing attention motivated by sharing or experiencing positive affect, may be particularly relevant to infants’ later ASD symptomatology. It may allow infants to best learn social information from the interactions they have initiated. That is, IJA without smiling may allow infants to reference a social partner not to share a preexisting emotional experience or to engage in a shared smile, but to better understand the partner’s pragmatic relationship to the object or event being referenced. IJA without smiling was not associated with language outcomes at 24 or 36 months (neither expressive nor receptive language). Rather, IJA without smiling appears to be uniquely associated with levels of ASD symptomatology, rather than broader developmental difficulties.
The current study expands our previous understanding of IJA deficits and their relationship to ASD severity. Ibañez et al. (2012) found that high-risk infants exhibited lower levels of overall IJA at baseline (8 months), and that these baseline levels of IJA predicted later ASD severity. The examination of specific IJA smiling patterns in the current study highlights the potential importance of the coordination of positive affect with joint attention in infants at risk for ASD. Early group differences in IJA are most pronounced in IJA that is a vehicle for sharing positive affect (i.e., anticipatory smiling), with high-risk siblings sharing less preexisting positive affect with a social partner. However, the relationship between IJA and ASD severity appears to be driven by IJA in a more neutral context, suggesting that the ability to utilize IJA routinely, in the absence of a specific positive affective motivation, may be an especially important skill for high-risk siblings. This interpretation is buttressed by recent findings in a study by Nichols et al. (2013). While high-risk siblings exhibited lower levels of social smiling (smiling combined with eye contact) than low-risk siblings as a whole, early eye contact that was not coordinated with a smile best distinguished between infant siblings with and without later ASD symptomatology. Low levels of motivation to share preexisting positive affect with others may be particularly relevant to the early emerging broad autism phenotype, while the proclivity to reference a partner for non-affective goals may index a capacity to obtain information from social experience that is important for ASD-related outcomes for high-risk siblings.
References
Adamson, L. B., Bakeman, R., Deckner, D. F., & Romski, M. (2009). Joint engagement and the emergence of language in children with autism and Down syndrome. Journal of Autism and Developmental Disorders, 39(1), 84–96. doi:10.1007/s10803-008-0601-7.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4, text rev ed.). Washington, DC: Author.
Bakeman, R., & Adamson, L. B. (1984). Coordinating attention to people and objects in mother–infant and peer–infant interaction. Child Development, 55(4), 1278–1289. doi:10.2307/1129997.
Bedford, R., Elsabbagh, M., Gliga, T., Pickles, A., Senju, A., Charman, T., et al. (2012). Precursors to social and communication difficulties in infants at-risk for autism: Gaze following and attentional engagement. Journal of Autism and Developmental Disorders, 42(10), 2208–2218. doi:10.1007/s10803-012-1450-y.
Berument, S., Rutter, M., Lord, C., Pickles, A., & Bailey, A. (1999). Autism screening questionnaire: Diagnostic validity. The British Journal of Psychiatry, 175, 444–451. doi:10.1192/bjp.175.5.444.
Bloom, L., Beckwith, R., & Capatides, J. B. (1988). Developments in the expression of affect. Infant Behavior and Development, 11(2), 169–186. doi:10.1016/S0163-6383(88)80004-3.
Bloom, L., & Capatides, J. B. (1987). Expression of affect and the emergence of language. Child Development, 58(6), 1513–1522. doi:10.2307/1130691.
Cassel, T. D., Messinger, D. S., Ibanez, L. V., Haltigan, J. D., Acosta, S. I., & Buchman, A. C. (2007). Early social and emotional communication in the infant siblings of children with autism spectrum disorders: An examination of the broad phenotype. Journal of Autism and Developmental Disorders, 37(1), 122–132. doi:10.1007/s10803-006-0337-1.
Damiano, C. R., Nahmias, A., Hogan-Brown, A. L., & Stone, W. L. (2013). What do repetitive and stereotyped movements mean for infant siblings of children with autism spectrum disorders? Journal of Autism and Developmental Disorders, 43(6), 1326–1335. doi:10.1007/s10803-012-1681-y.
Dawson, G., Hill, D., Spencer, A., Galpert, L., & Watson, L. (1990). Affective exchanges between young autistic children and their mothers. Journal of Abnormal Child Psychology, 18(3), 335–345. doi:10.1007/BF00916569.
Dawson, G., Toth, K., Abbott, R., Osterling, J., Munson, J., Estes, A., et al. (2004). Early social attention impairments in autism: Social orienting, joint attention, and attention to distress. Developmental Psychology, 40(2), 271–283. doi:10.1037/0012-1649.40.2.271.
Ekman, P., & Friesen, W. V. (1978). Facial action coding system. Palo Alto, CA: Consulting Psychologist Press.
Georgiades, S., Szatmari, P., Zwaigenbaum, L., Bryson, S., Brian, J., Roberts, W., et al. (2013). A prospective study of autistic-like traits in unaffected siblings of probands with autism spectrum disorder. JAMA Psychiatry, 70(1), 42–48. doi:10.1001/2013.jamapsychiatry.1.
Gerdts, J., & Bernier, R. (2011). The broader autism phenotype and its implications on the etiology and treatment of autism spectrum disorders. Autism Research and Treatment, 2011. doi: 10.1155/2011/545901.
Goldberg, W. A., Jarvis, K. L., Osann, K., Laulhere, T. M., Straub, C., Thomas, E., et al. (2005). Brief report: Early social communication behaviors in the younger siblings of children with autism. Journal of Autism and Developmental Disorders, 35(5), 657–664. doi:10.1007/s10803-005-0009-6.
Gotham, K., Pickles, A., & Lord, C. (2009). Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(5), 693–705. doi:10.1007/s10803-008-0674-3.
Ibañez, L. V., Grantz, C. J., & Messinger, D. S. (2012). The development of referential communication and autism symptomatology in high-risk infants. Infancy,. doi:10.1111/j.1532-7078.2012.00142.x.
Jones, S. S., Collins, K., & Hong, H. (1991). An audience effect on smile production in 10-month-old infants. Psychological Science, 2(1), 45–49. doi:10.1111/j.1467-9280.1991.tb00095.x.
Jones, S. S., & Hong, H. (2001). Onset of voluntary communication: Smiling looks to mother. Infancy, 2(3), 353–370. doi:10.1207/S15327078IN0203_4.
Jones, S. S., & Hong, H. (2005). How some infant smiles get made. Infant Behavior & Development, 28(2), 194–205. doi:10.1016/j.infbeh.2005.02.003.
Jones, S. S., & Raag, T. (1989). Smile production in older infants: The importance of a social recipient for the facial signal. Child Development, 60(4), 811–818. doi:10.2307/1131021.
Joseph, R. M., & Tager-Flusberg, H. (1997). An investigation of attention and affect in children with autism and Down syndrome. Journal of Autism and Developmental Disorders, 27(4), 385–396. doi:10.1023/A:1025853321118.
Kasari, C., Sigman, M., Mundy, P., & Yirmiya, N. (1990). Affective sharing in the context of joint attention interactions of normal, autistic, and mentally retarded children. Journal of Autism and Developmental Disorders, 20(1), 87–100. doi:10.1007/BF02206859.
Landa, R., & Garrett-Mayer, E. (2006). Development in infants with autism spectrum disorders: A prospective study. Journal of Child Psychology and Psychiatry, 47(6), 629–638. doi:10.1111/j.1469-7610.2006.01531.x.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Leventhal, B. L., DiLavore, P. C., et al. (2000). The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30, 205–223.
Messinger, D. S., & Fogel, A. (1998). Give and take: The development of conventional infant gestures. Merrill-Palmer Quarterly: Journal of Developmental Psychology, 44(4), 566–590.
Mullen, E. (1995). Mullen scales of early learning. Circle Pines, MN: American Guidance Service.
Mundy, P., Block, J., Delgado, C., Pomares, Y., Van Hecke, A., & Parlade, M. (2007). Individual differences and the development of joint attention in infancy. Child Development, 78(3), 938–954. doi:10.1111/j.1467-8624.2007.01042.x.
Mundy, P., Delgado, C., Block, J., Venezia, M., Hogan, A., & Siebert, J. (2003). A manual for the abridged Early Social Communication Scales (ESCS). Coral Gables, FL: University of Miami, Department of Psychology.
Mundy, P., Sigman, M., & Kasari, C. (1990). A longitudinal study of joint attention and language development in autistic children. Journal of Autism and Developmental Disorders, 20(1), 115–128. doi:10.1007/BF02206861.
Mundy, P., Sigman, M. D., Ungerer, J., & Sherman, T. (1986). Defining the social deficits of autism: The contribution of non-verbal communication measures. Child Psychology & Psychiatry & Allied Disciplines, 27(5), 657–669. doi:10.1111/j.1469-7610.1986.tb00190.x.
Mundy, P., & Vaughan, A. (2001). Joint attention and its role in the diagnostic assessment of children with autism. Assessment for Effective Intervention, 27(1–2), 57–60. doi:10.1177/073724770202700108.
Nichols, C. M., Ibañez, L. V., Foss-Feig, J. H., & Stone, W. L. (2013). Social smiling and its components in high-risk infant siblings without later asd symptomatology. Journal of Autism and Developmental Disorders,. doi:10.1007/s10803-013-1944-2.
Ozonoff, S., Losif, A., Baguio, F., Cook, I. C., Hill, M., Hutman, T., et al. (2010). A prospective study of the emergence of early behavioral signs of autism. Journal of the American Academy of Child and Adolescent Psychiatry, 49(3), 256–266. doi:10.1097/00004583-201003000-00009.
Ozonoff, S., Young, G. S., Carter, A., Messinger, D., Yirmiya, N., Zwaigenbaum, L., et al. (2011). Recurrence risk for autism spectrum disorders: A baby siblings research consortium study. Pediatrics, 128(3), e488–e495. doi:10.1542/peds.2010-2825.
Parlade, M., Messinger, D. S., Delgado, C. F., Kaiser, M., Van Hecke, A., & Mundy, P. C. (2009). Anticipatory smiling: Linking early affective communication and social outcome. Infant Behavior & Development, 32(1), 33–43. doi:10.1016/j.infbeh.2008.09.007.
Presmanes, A. G., Walden, T. A., Stone, W. L., & Yoder, P. J. (2007). Effects of different attentional cues on responding to joint attention in younger siblings of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 37(1), 133–144. doi:10.1007/s10803-006-0338-0.
Raudenbush, S. W., & Bryk, A. S. (2002). Hierarchical linear models: Applications and data analysis methods (2nd ed.). Thousand Oaks, CA: Sage Publications Inc.
Raudenbush, S., Bryk, A., Cheong, Y. F., Congdon, R., & du Toit, M. (2004). HLM 6: Hierarchical linear & nonlinear modeling. Lincolnwood, IL: Scientific Software International Inc.
Rozga, A., Hutman, T., Young, G. S., Rogers, S. J., Ozonoff, S., Dapretto, M., et al. (2011). Behavioral profiles of affected and unaffected siblings of children with autism: Contribution of measures of mother–infant interaction and nonverbal communication. Journal of Autism and Developmental Disorders, 41(3), 287–301. doi:10.1007/s10803-010-1051-6.
Singer, J. D., & Willett, J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press.
Tierney, A. L., Gabard-Durnam, L., Vogel-Farley, V., Tager-Flusberg, H., & Nelson, C. A. (2012). Developmental trajectories of resting EEG power: An endophenotype of autism spectrum disorder. PLoS One, 7(6), e39127. doi:10.1371/journal.pone.0039127.
Toth, K., Munson, J., Meltzoff, A. N., & Dawson, G. (2006). Early predictors of communication development in young children with autism spectrum disorder: Joint attention, imitation, and toy play. Journal of Autism and Developmental Disorders, 36(8), 993–1005. doi:10.1007/s10803-006-0137-7.
Venezia, M., Messinger, D. S., Thorp, D., & Mundy, P. (2004). The development of anticipatory smiling. Infancy, 6(3), 397–406. doi:10.1207/s15327078in0603_5.
Yirmiya, N., Gamliel, I., Pilowsky, T., Feldman, R., Baron-Cohen, S., & Sigman, M. (2006). The development of siblings of children with autism at 4 and 14 months: Social engagement, communication, and cognition. Journal of Child Psychology and Psychiatry, 47(5), 511–523. doi:10.1111/j.1469-7610.2005.01528.x.
Yoder, P., Stone, W. L., Walden, T., & Malesa, E. (2009). Predicting social impairment and ASD diagnosis in younger siblings of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 39(10), 1381–1391. doi:10.1007/s10803-009-0753.
Young, G. S., Merin, N., Rogers, S. J., & Ozonoff, S. (2009). Gaze behavior and affect at 6 months: Predicting clinical outcomes and language development in typically developing infants and infants at risk for autism. Developmental Science, 12(5), 798–814. doi:10.1111/j.1467-7687.2009.00833.x.
Acknowledgments
We would like to thank the families who have participated in our study. This research was supported by the National Institutes of Health (R01 HD047417& R01 HD057284), the Marino Autism Research Institute (MARI), the National Science Foundation (0808767 & 1052736), National Institute of General Medical Sciences (1R01GM105004), and Autism Speaks.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gangi, D.N., Ibañez, L.V. & Messinger, D.S. Joint Attention Initiation With and Without Positive Affect: Risk Group Differences and Associations with ASD Symptoms. J Autism Dev Disord 44, 1414–1424 (2014). https://doi.org/10.1007/s10803-013-2002-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-013-2002-9