Abstract
The type, frequency and inter-relationships of emotional and behavioural problems in 863 children with autism spectrum disorder (ASD) were investigated using the population-based Database of children with ASD living in the North East of England (Daslne). A high rate of problems was reported, with 53 % of children having 4 or more types of problems frequently. Sleep, toileting and eating problems, hyperactivity, self injury and sensory difficulties were greater in children with lower language level and in special schooling. However, anxiety, tantrums and aggression towards others were frequent regardless of age, ability or schooling. The frequency of co-existing conditions, including such emotional and behavioural problems, in children with ASD has implications for designing appropriate support services for children and families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The core features of autism spectrum disorder (ASD) include impaired social interaction and communication skills, and restricted and repetitive interests and behaviours. However, individuals with ASD often experience additional health and mental health conditions and behavioural problems that can impact on their lives and on their families (Dominick et al. 2007; Hurtig et al. 2009). It is likely that the complexity of managing a child’s ASD needs together with behaviour and mental health problems contributes to the higher levels of stress and distress seen in families of children with ASD compared to other families (Allik et al. 2006a; Lecavalier et al. 2006; Manning et al. 2010).
The co-existing conditions can include a range of symptoms from emotional and behavioural problems (including aggression, temper tantrums, self injurious behaviour), sleep, feeding and eating problems and sensory sensitivities, and also learning and intellectual disabilities, as well as comorbid health and mental health diagnoses (such as epilepsy, attention deficit hyperactivity disorder (ADHD), anxiety, obsessive compulsive disorder and tic disorders). Many of these are also seen in typically developing children and children with other developmental disorders (Dominick et al. 2007). However, for parents and teachers, the co-existing conditions can be of equal or greater concern than the core features of ASD, and have a significant impact on behaviour management, learning acquisition and the development of social relationships (Pearson et al. 2006).
There is an increasing awareness of the importance of recognising co-existing conditions as part of the skills- and needs-based assessment and diagnosis of individuals with ASD and their families, which in turn should inform the child and family intervention care plan (NICE CG128 2011). However the reported rates of co-existing conditions have varied considerably. In a UK population-based cohort study, Simonoff and colleagues (Simonoff et al. 2008) investigated psychiatric disorders in a sample of 112 children with ASD aged 10–14 years, and identified that 70 % met criteria for at least one disorder, and 41 % had two or more disorders, most commonly social anxiety and ADHD. Studies of a broader range of co-existing conditions reported individual children may have as many as four or five different conditions (de Bruin et al. 2007; Dominick et al. 2007; Leyfer et al. 2006; Mattila et al. 2010). Researchers studying specific conditions have also reported wide prevalence variations in children and young people with ASD. For example the rates of parent-reported anxiety in children with ASD range from 22 to 84 % (Gadow et al. 2005; Kanne et al. 2009; MacNeil et al. 2009; Mattila et al. 2010; Pearson et al. 2006; Simonoff et al. 2008; White et al. 2009) and sleep problems have been identified in 31–80 % (Allik et al. 2006b; Couturier et al. 2005; Dominick et al. 2007; Krakowiak et al. 2008; Oyane and Bjorvatn 2005; Souders et al. 2009). Leekam et al. (2007) found that adverse sensory reactions occur in at least 90 % of individuals with ASD, and highlighted that these problems may cause disturbed and aggressive behaviour in low functioning individuals unable to explain their distress; in addition sensory reactions contribute to anxiety (Kern et al. 2007). Intellectual disability (IQ below 70) occurs in approximately 55 % of young people with ASD (Baird et al. 2006).
Research studies have also reported variable findings concerning the potential moderating role of a range of individual characteristics including the child’s age, type of ASD diagnosis, IQ and language ability, and whether these factors influence the presentation of symptoms or the child’s ability to cope with particular conditions. Dominick et al. (2007) reported that greater levels of ‘atypical behaviours’ were associated with the child having lower IQ and expressive and receptive language ability. Witwer and Lecavalier (2010) identified fewer psychiatric disorders in children with an IQ below 70; however, some other studies have found no correlation between IQ and psychiatric disorders (Brereton et al. 2006; Simonoff et al. 2008). Pearson et al. (2006) reported that diagnostic groups within ASD rather than ability level were predictive of different patterns of risk for ‘comorbid behavioural and emotional disabilities’.
Comparisons between studies are hard to interpret due to the different sampling frames, sample sizes, criteria and classifications used. Further studies are needed to identify what might be the accurate rates of co-existing conditions, and the risk and protective factors relevant for service planning and appropriate interventions and family support, to minimise distress and impairment for children with ASD and their families.
In this paper we present parent and professional-reported rates of co-existing conditions (including other developmental and psychiatric disorders, emotional problems, or problem behaviours) in children with ASD from a regional database. Children within the database have been shown to be representative of the population of children and young people with ASD living in North East England (McConachie et al. 2009). The sample is of sufficient size to allow further investigation of various predictors of the rates of parent-reported common emotional and behavioural problems in this representative sample of children with ASD (including autism, Asperger syndrome and ASD) from 2 to 18 years, with a broad range of skills and disabilities. Our expectation is that the findings contribute to the evidence base available to inform future service planning and provision for individuals with co-existing conditions and their families.
Methods
Participants and Procedures
Data were obtained from Daslne (the database of children with autism spectrum disorder living in the north east of England), which was established in 2003 to gather reliable information about children with ASD across six local areas (total population 1.3 million). The database is used for local service planning and to provide samples for recruitment to research studies. Over 60 % of children with ASD known to local service listings have been recruited to the database; the included children have been shown to be representative of the range of ages, type of ASD diagnosis and variety of educational provision attended across the local region (McConachie et al. 2009). Parents are invited to join the database shortly after their child receives an ASD diagnosis. Once parents have given informed consent, they are asked to complete the Daslne parent questionnaire. Parents also nominate a local professional involved in the child’s care to complete a questionnaire to confirm the clinical diagnosis of autism/ASD (based on ICD-10 diagnostic criteria for autism/PDD) and to provide an independent source of information about other medical diagnoses. A positive Ethics opinion for the database was granted in 2003.
At the time of analysis the database contained 990 children, aged between 2 and 18 years at time of registration. Of these, 51 were explicit refusals and 76 recently recruited to the database for whom parents had given consent but not yet returned a completed parent questionnaire about their child’s characteristics. Therefore the maximum number for whom data were available on parent-reported co-existing conditions was 863. The number of parent nominated local professionals who had returned the professional questionnaire about the child was 759.
Measures
The parent questionnaire includes information about the child’s ASD diagnosis, other developmental disorders (dyslexia; dyspraxia; ADHD; learning difficulties/developmental delay), current language level (on a graded 7 point scale from no speech to ‘uses sentences with good grammar’) and the child’s educational provision (preschool; mainstream; unit attached to mainstream; special school; college; other), together with information about other family members including siblings. Parents also give information about 10 common co-morbid problems (Table 1), rated as frequent (problem behaviour is present 3 or more times a week), sometimes (present once or twice a week), never or rare, and in the past only. The behaviours include ‘habit disorders’ (e.g. eating, sleeping, toileting) and other emotional and behavioural problems (e.g. anxiety, aggression and ‘hyper’/severely overactive periods). As well as correlates of individual problems, the total number (out of 10) of common problems reported by parents as frequent is analysed.
The professional questionnaire includes information about the child’s ASD diagnosis, estimate of level of learning difficulty (above average ability; average ability or mild only; moderate i.e. estimated IQ 50–70; severe or profound i.e. IQ estimated < 50), and also other medical conditions (list including Fragile X syndrome, muscular dystrophy, epilepsy). Together, the reported developmental disorders, learning disability, medical conditions, and common emotional and behavioural problems make up the ‘co-existing conditions’ referred to in this paper.
Analysis
Descriptive statistics were used for the rates of co-existing conditions (reported by parents or/and professionals). The reported data have differing denominators depending on the amount of missing data. From the range of known child characteristics, comparisons of proportions were made using Chi square for one within-child factor (language level) and one environmental factor (educational setting). The total number of parent-reported frequent common problems, and the known child characteristics from the database (age, gender, ASD diagnosis group, age at diagnosis, language level and education provision), were entered into univariate analysis with Pearson’s correlations, t tests and one way analysis of variance. Multiple regression analysis was then used to investigate which of the significantly related variables explained unique variance. Dummy variables were created for ASD diagnosis group, and education was analysed as mainstream versus other school type. Analyses were conducted using the Statistical Package for the Social Sciences v17.0 (SPSS).
Results
Data were available from 863 children aged 2–18 years; Table 2 shows the sample characteristics. For children reported by parents as having a diagnosis of Autism the male:female ratio was 5.5:1; for those with a diagnosis of Asperger syndrome the ratio was considerably greater at 8.8:1.
Rates of Developmental Disorders and Medical Conditions
The most commonly reported co-existing condition reported by parents was learning difficulties/developmental delay (Table 3). This applied both to children with a diagnosis of autism (55 %) of whom nearly half were under the age of 6 years, and also those with an ASD diagnosis (45 %), where the age spread was more even. Professional estimates of children’s ability put the proportion with moderate to severe learning difficulties even higher in autism (69 %) but lower in ASD (35 %). For the few children with Asperger syndrome identified by professionals as having learning difficulties, the estimate was of moderate difficulty. The proportions of other parent-reported co-existing conditions were all low, the most frequently reported being dyspraxia, in 19 % of children with Asperger syndrome. As all the individual medical conditions listed in the professional questionnaire were reported infrequently, they were combined in the table. Eighteen (2.6 %) children were reported as having epilepsy.
Ten commonly Reported Emotional and Behavioural Problems
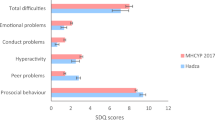
Figure 1 shows how many children had a total of from 1 to 10 problems reported to occur frequently (at least 3 times per week). For the whole sample 52.6 % of the children were reported to have four or more of the listed problems occurring frequently. Sensory reactions, and faddiness about eating were the most common problems reported to occur frequently (57 and 58 % of the children respectively) (see Fig. 2).
Relationship Between Common Problems and Language Level
Table 4 presents problems which occurred frequently as related to children’s language level, grouping children who spoke in fluent sentences, and those who used phrase speech, single words or no words. Language does, of course, overlap with characteristics such as age, level of ability and diagnostic group. Most of the common problems occurred more frequently in those children with less well developed language (difference significant for sleep problems, toileting issues, hyperactive periods, self injury, eating problems and sensory issues). However, language level did not significantly differentiate the frequency of temper tantrums, aggression to others, reluctance to separate and anxiety, fears and phobias.
Relationship Between Common Problems, and Children’s School Type
The distribution of frequent problems also differed according to the type of school attended by children. Again, this environmental factor overlaps with characteristics such as language and level of ability. School types were categorised as preschool, mainstream school, unit attached to mainstream school (communication difficulties and/or ASD specific), and special school (see Table 5). Analysis compared children who attended mainstream school, with those who attended any other school. Sleep problems, toileting problems, hyperactive periods, self injury, reluctance to separate, eating problems and sensory issues were significantly more likely in children who attended special schools. However, school type did not differentiate the likelihood of frequent temper tantrums, aggression to others, and anxiety, fears and phobias. Though a lower proportion than for children in special school, it is notable that 55 % of children with ASD in mainstream school had frequent problems regarding eating, and 51 % had frequent sensory issues.
Predictors of Common Problems
Univariate analyses indicated that gender, and age at diagnosis were not significantly related to the number of frequent common problems; child age and ASD diagnosis group were (analyses not presented here). Therefore child age, ASD diagnosis group, language ability and education provision were entered into multiple regression analysis to investigate the strongest predictors of the total number of frequent common problems (see Table 6).
Age, language level and whether the child attended mainstream school or not significantly predicted unique aspects of the variance. Older children with good language attending mainstream school were reported by parents as showing fewer frequent problems. Nevertheless over half the children aged 12 and above had frequent problems with anxiety and sensory issues.
Discussion
This is the largest community study to investigate the prevalence, frequency and predictors of additional diagnoses and behaviour problems in children with ASD. Our large population-based sample allowed us to investigate common problems in children with ASD across a range of ages, types of ASD diagnosis, different language levels and learning difficulties, and attending different types of school.
Common Problems
Over half of the children in our study experience four or more of the ten common problems reported by parents, at least three times a week. This confirms the high rates of co-existing problems experienced by children with ASD reported in other studies (de Bruin et al. 2007; Gadow et al. 2005; Hurtig et al. 2009; Kanne et al. 2009; Leyfer et al. 2006; Simonoff et al. 2008; Witwer and Lecavalier 2010) and illustrates the very significant day-to day difficulties faced by children and parents. Our findings highlight the importance of clinicians identifying these issues with parents, so that they can be suitably addressed (Joshi et al. 2010).
In keeping with the findings of the small study by Dominick et al. (2007), most problem behaviours occur more frequently in children with lower expressive language ability, and in those children attending special school. We also found age to be a significant predictor, with older children generally having fewer of the common problems; this is in keeping with Mattila et al. (2010) recent finding that current psychiatric disorders were more common in primary school-age than in secondary school-age participants. However, anxiety, fears and phobias are still frequent in secondary school age participants and those with fluent language, as has been found by others for more able children (de Bruin et al. 2007; Gadow et al. 2005; White et al. 2009; Witwer and Lecavalier 2010)
This is the second population-based study to find that the type of ASD diagnosis was not a predictor of behaviour problems (over and above age, language and school placement)(c.f. Simonoff et al. 2008). Snow and Lecavalier (2010) suggest that the validity of the distinctions between ASD subgroups is unclear and it is cognitive function, rather than the ASD subtype, that is of more value; this conceptualisation is reinforced by the proposed changes to diagnostic categories in DSM-V and ICD-11.
Our study illustrates a higher prevalence of sensory reactions experienced by younger children and those attending special school. Sensory reactions were the second most common problem reported at least 3 times a week. Leekam et al. (2007) and Tomchek and Dunn (2007) report that over 90 % of individuals with ASD experience sensory problems; comparisons are difficult, however, due to different sampling frames and methodology.
We have identified parent reported sleeping problems occurring frequently in 45 % of children. This comes towards the lower end of the range reported by other studies (31–80 %) (Allik et al. 2006b; Dominick et al. 2007; Krakowiak et al. 2008; Mattila et al. 2010; Oyane and Bjorvatn 2005; Souders et al. 2009) which may be explained by our reporting a level of frequency where the problem is likely to be disruptive to family life, not simply prevalence, and also our reporting across the age range. Eating problems were the most commonly reported behaviour. Other studies, comparing the types of eating problems, such as food selectivity by type and texture, or food refusal, support the high prevalence of eating problems (Ahearn et al. 2001; Dominick et al. 2007; Schreck and Williams 2006). Although toileting problems are recognised as common in children with ASD, and guidance is available to parents in the form of literature and the websites of many organisations, only one recent study has reported figures for enuresis and encopresis in ASD (Simonoff et al. 2008: 11 and 6.6 % of children respectively). Our study suggests a much higher prevalence of problems experienced by families, which may not come to the attention of services.
Anxiety, fears and phobias were reported commonly by parents (43 %). In keeping with the findings of many others, our study showed higher rates of anxiety in higher functioning children with ASD (Gadow et al. 2005; Pearson et al. 2006; White et al. 2009). However, for a very young sample (17–37 months) Davis et al. (2010) found that toddlers with an autism diagnosis showed more anxiety than those with a diagnosis of pervasive developmental disorder not otherwise specified (PDD-NOS), so the prevalence of anxiety in children with ASD may have an age dependent distribution.
Self Injurious behaviour (SIB) was the least reported behaviour (14 %); the highest prevalence was found in children with an autism diagnosis and a low level of language, and it may be one trigger for placement in special schooling. Dominick et al. (2007) found a higher rate of SIB, present in almost a third of children with autism, and related to expressive language level but not to cognitive ability; however, the small sample size of that study makes the true interpretation of rates of SIB uncertain. Temper tantrums were the third most common behaviour problem reported in our study. Few other studies have focused on temper tantrums as a specific problem behaviour (de Bruin et al. 2007; Dominick et al. 2007); however Horner et al. (2002) discuss behaviours that include temper tantrums, aggression and SIB as major barriers to effective social development and amongst the most likely to be identified for intervention.
The impact of high levels of common emotional and behaviour problems in children with ASD on families is well documented, with families experiencing higher levels of stress and distress than families of typically developing children or children with other disabilities (Allik et al. 2006a; Lecavalier et al. 2006; Manning et al. 2010). As Manning et al. (2010) emphasise, given that child behaviour problems play a large role in creating increased family stress, there should be provision for the support and training of parents to enable them to manage their child’s difficult behaviours. Many local services for child and adolescent mental health and/or learning disability now offer parent group courses following the child’s diagnosis of ASD, to help parents in understanding the roots of their child’s difficulties, and thus appropriate strategies to adopt (e.g. Pillay et al. 2011; Tonge et al. 2006). In addition such groups enable mutual support between families.
Other Co-existing Conditions
Of the children in our study half had another parent- or professional-reported developmental or medical condition, predominantly learning difficulties, ADHD and dyspraxia. As found previously (Gillberg and Billstedt 2000), learning difficulties were the most common additional diagnosis in those with autism, and dyspraxia was more prevalent in children with Asperger syndrome. Edelson (2006) reported that of the epidemiological surveys they reviewed, 40–55 % of children with autism also have ‘mental retardation’ (IQ < 70). However, in the present study, one limitation is that the questionnaire did not differentiate between levels of learning difficulties. The prevalence of ADHD in the current study was lower than found in recent studies (Gadow et al. 2005; Kanne et al. 2009; Leyfer et al. 2006; Mattila et al. 2010; Simonoff et al. 2008). This was not unexpected, as parents completed the questionnaire shortly after the diagnosis of ASD and not all children would by then have received assessment and diagnosis for other symptoms and behaviours; another possible reason is the lack of access to additional assessment services (e.g. paediatric occupational therapy). It can be difficult to disentangle the features of conditions such as ADHD from the characteristics of ASD, when for many reasons children with ASD find it difficult to concentrate and absorb information, if distracted by sensory issues or anxiety.
Strengths and Limitations
The study uses information from a regional database of children with ASD which includes over 60 % children known to have an ASD diagnosis in the North East of England, with over 80 % of parents completing the parent questionnaire giving further information about the family and the child’s characteristics. This provides high quality data; parents are generally good at recognising their child’s characteristics and accurately reporting about their children (Allik et al. 2006b; Gadow et al. 2005; Hurtig et al. 2009; Oliver et al. 2002; Souders et al. 2009). This methodology is also supported by the findings of Lee et al. (2010), who validated parent-informed questionnaires from the web-based parent report database, the Interactive Autism network (IAN), and found a high concordance rate with clinic-based assessments. Nevertheless there are some limitations with data collected in this way. For example, co-existing medical conditions are likely to be under-estimated; children who receive a first diagnosis of some other condition (such as muscular dystrophy, epilepsy or hearing impairment) may not be referred on for further diagnostic assessment in relation to abnormal social communication or other behaviours. Parents may somewhat underestimate their child’s level of learning difficulties; furthermore, the professional questionnaire asked for an estimate of level of ability (which may or may not have been backed up by cognitive assessment results) introducing further potential sources of inaccuracy. In terms of common problems, particularly anxiety and sensory reactions, the lack of self-report from older children and young people is also a limitation.
The findings are expected to be generalisable, given previous analysis that showed participants in Daslne are representative of the known population of children with a diagnosis of ASD. Nevertheless, the observed levels of reported co-existing conditions might be subject to unknown sources of bias given that 40 % of the area’s families did not participate. Many factors in addition to those analysed will affect levels of common problems experienced, including family deprivation, parent mental health, and so on. Such data are not held on the database, but can be measured in specific studies and general surveys; in the future, we will survey how these children’s co-existing conditions have changed over time, their impact on parents’ quality of life, and the effectiveness of local services in helping parents and young people manage the conditions.
Conclusions
Co-existing conditions are common in children with ASD. The high rates of frequent emotional and behavioural problems reported by parents in our study, added to the ASD symptomatology, often in the context of learning difficulties, cause very high levels of stress for family members. The knowledge that children with ASD in mainstream school have frequent co-existing conditions such as temper tantrums, anxiety, eating issues and sensory sensitivities puts an onus on clinicians to discuss all co-existing conditions with all parents, and together with other professionals, offer intervention, or management advice about adapting the environment, and managing behavior. Effective and timely treatment and support are required from the statutory and voluntary services to adequately support children with ASD and their families.
References
Ahearn, W., Castine, T., Nault, K., & Green, G. (2001). An assessment of food acceptance in children with autism or pervasive developmental disorder-not otherwise specified. Journal of Autism and Developmental Disorders, 31, 505–511.
Allik, H., Larsson, J.-O., & Smedje, H. (2006a). Health-related quality of life in parents of school-age children with Asperger syndrome or high-functioning autism. Health Qual Life Outcomes, 4, 1.
Allik, H., Larsson, J.-O., & Smedje, H. (2006b). Insomnia in school-age children with Asperger syndrome or high-functioning autism. BMC Psychiatry, 6(1), 18.
Baird, G., Simonoff, E., Pickles, A., Chandler, S., Loucas, T., Meldrum, D., et al. (2006). Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP). The Lancet, 368(9531), 210–215.
Brereton, A. V., Tonge, B. J., & Einfeld, S. L. (2006). Psychopathology in children and adolescents with autism compared to young people with intellectual disability. Journal of Autism and Developmental Disorders, 36(7), 863–870.
Couturier, J., Speechley, K., Steele, M., Norman, R., Stringer, B., & Nicolson, R. (2005). Parental perception of sleep problems in children of normal intelligence with pervasive developmental disorders: Prevalence, severity, and pattern. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 815–822.
Davis, T. E., I. I. I., Fodstad, J. C., Jenkins, W. S., Hess, J. A., Moree, B. N., Dempsey, T., et al. (2010). Anxiety and avoidance in infants and toddlers with autism spectrum disorders: Evidence for differing symptom severity and presentation. Research in Autism Spectrum Disorders, 4(2), 305–313.
de Bruin, E., Ferdinand, R., Meester, S., de Nijs, P., & Verheij, F. (2007). High rates of psychiatric co-morbidity in PDD-NOS. Journal of Autism and Developmental Disorders, 37(5), 877–886.
Dominick, K. C., Davis, N. O., Lainhart, J., Tager-Flusberg, H., & Folstein, S. (2007). Atypical behaviors in children with autism and children with a history of language impairment. Research in Developmental Disabilities, 28(2), 145–162.
Edelson, M. G. (2006). Are the majority of children with autism mentally retarded?: A systematic evaluation of the data. Focus Autism Other Developmental Disabilities, 21(2), 66–83.
Gadow, K. D., Devincent, C. J., Pomeroy, J., & Azizian, A. (2005). Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism, 9(4), 392–415.
Gillberg, C., & Billstedt, E. (2000). Autism and Asperger syndrome: Coexistence with other clinical disorders. Acta Psychiatrica Scandinavica, 102, 321–330.
Horner, R. H., Carr, E. G., Strain, P. S., Todd, A. W., & Reed, H. K. (2002). Problem behavior interventions for young children with autism: A research synthesis. Journal of Autism and Developmental Disorders, 32(5), 423–446.
Hurtig, T., Kuusikko, S., Matilla, M.-L., Haapsamo, H., Ebeling, H., Jussila, K., et al. (2009). Multi-informant reports of psychiatric symptoms among high functioning adolescents with Asperger syndrome or autism. Autism, 13(6), 583–598.
Joshi, G., Petty, C., Wozniak, J., Henin, A., Fried, R., Galdo, M., et al. (2010). The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: A large comparative study of a psychiatrically referred population. Journal of Autism and Developmental Disorders, 40, 1361–1370.
Kanne, S., Abbacchi, A., & Constantino, J. (2009). Multi-informant ratings of psychiatric symptom severity in children with autism spectrum disorders: The importance of environmental context. Journal of Autism and Developmental Disorders, 39(6), 856–864.
Kern, J. K., Trivedi, M. H., Grannemann, B. D., Garver, C. R., Johnson, D. G., Andrews, A. A., et al. (2007). Sensory correlations in autism. Autism, 11(2), 123–134.
Krakowiak, P., Goodlin-Jones, B., Hertz-Picciotto, I., Croen, L. A., & Hansen, R. L. (2008). Sleep problems in children with autism spectrum disorders, developmental delays, and typical development: A population-based study. Journal of Sleep Research, 17(2), 197–206.
Lecavalier, L., Leone, S., & Wiltz, J. (2006). The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research, 50(3), 172–183.
Lee, H., Marvin, A. R., Watson, T., Piggot, J., Law, J. K., Law, P. A., et al. (2010). Accuracy of phenotyping of autistic children based on internet implemented parent report. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 153B(6), 1119–1126.
Leekam, S., Nieto, C., Libby, S., Wing, L., & Gould, J. (2007). Describing the sensory abnormalities of children and adults with autism. Journal of Autism and Developmental Disorders, 37(5), 894–910.
Leyfer, O., Folstein, S., Bacalman, S., Davis, N., Dinh, E., Morgan, J., et al. (2006). Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders, 36(7), 849–861.
MacNeil, B. M., Lopes, V. A., & Minnes, P. M. (2009). Anxiety in children and adolescents with autism spectrum disorders [Review]. Research in Autism Spectrum Disorders, 3(1), 1–21.
Manning, M. M., Wainwright, L., & Bennet, J. (2010). The double ABCX model of adaptation in racially diverse families with a school-age child with autism. Journal of Autism and Developmental Disorders, 41, 320–331.
Mattila, M.-L., Hurtig, T., Haapsamo, H., Jussila, K., Kuusikko-Gauffin, S., Kielinen, M., et al. (2010). Comorbid psychiatric disorders associated with Asperger syndrome/high-functioning autism: A community- and clinic-based study. Journal of Autism and Developmental Disorders, 40(9), 1080–1093.
McConachie, H., Barry, R., Spencer, A., Parker, L., Le Couteur, A., & Colver, A. (2009). Daslne: The challenge of developing a regional database for autism spectrum disorder. Archives of Disease in Childhood, 94(1), 38–41.
National Institute for Clinical Excellence. (2011). CG128 Autism in children and young people: NICE guideline. Retrieved March 14, 2012, from http://guidance.nice.org.uk/CG128/NICEGuidance/pdf/English.
Oliver, B., Dale, P. S., Saudina, K. J., Petrill, S. A., Pike, A., & Plomin, R. (2002). The validity of a parent-based assessment of cognitive abilities in three-year olds. Early Child Development and Care, 172(4), 337–348.
Oyane, N., & Bjorvatn, B. (2005). Sleep disturbances in adolescents and young adults with autism and Asperger syndrome. Autism, 9, 83–94.
Pearson, D. A., Loveland, K. A., Lachar, D., Lane, D. M., Reddoch, S. L., Mansour, R., et al. (2006). A comparison of behavioral and emotional functioning in children and adolescents with autistic disorder and PDD-NOS. Child Neuropsychology, 12(4), 321–333.
Pillay, M., Alderson-Day, B., Wright, B., Williams, C., & Urwin, B. (2011). Autism spectrum conditions—enhancing nurture and development (ASCEND): An evaluation of intervention support groups for parents. Clinical Child Psychology and Psychiatry, 16, 5–20.
Schreck, K., & Williams, K. (2006). Food preferences and factors influencing food selectivity for children with autism spectrum disorders. Research in Developmental Disabilities, 27, 353–363.
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929.
Snow, A. V., & Lecavalier, L. (2010). Comparing autism, PDD-NOS, and other developmental disabilities on parent-reported behaviour problems: Little evidence for ASD subtype validity. Journal of Autism and Developmental Disorders, 41, 302–310.
Souders, M. C., Mason, T. B. A., Valladares, O., Bucan, M., Levy, S. E., Mandell, D. S., et al. (2009). Sleep behaviours and sleep quality in children with autism spectrum disorders. Sleep, 32(12), 1566–1578.
Tomchek, S. D., & Dunn, W. (2007). Sensory processing in children with and without autism: A comparative study using the short sensory profile [Article; Proceedings Paper]. American Journal of Occupational Therapy, 61(2), 190–200.
Tonge, B., Brereton, A., Kiomall, M., Mackinnon, A., King, N., & Rinehart, N. (2006). Effects on parental mental health of an education and skills training program for parents of young children with autism: a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 561–569.
White, S. W., Oswald, D., Ollendick, T., & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229.
Witwer, A. N., & Lecavalier, L. (2010). Validity of comorbid psychiatric disorders in youngsters with autism spectrum disorders. Journal of Developmental and Physical Disabilities, 22(4), 367–380.
Acknowledgments
We are grateful for funding and other support for the Daslne database to the Northern Rock Foundation and the Children’s Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maskey, M., Warnell, F., Parr, J.R. et al. Emotional and Behavioural Problems in Children with Autism Spectrum Disorder. J Autism Dev Disord 43, 851–859 (2013). https://doi.org/10.1007/s10803-012-1622-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-012-1622-9