Abstract
The aims of this study were to investigate whether individuals with AS have impaired motor abilities and sensorimotor processing and whether these impairments were age-related. Sensorimotor abilities were examined using the Movement Assessment Battery for Children-2, and the Sensory Integration Praxis Test. Fifty boys with AS aged 7–14 years old were compared with typically developing boys. Overall, children with AS showed significant impairment of movement performance as well as proprioceptive and vestibular processing. There were no interaction effects of age and clinical group on level of performance deficit in any of the modalities tested. Increasing our understanding of motor and sensory impairment in AS could have treatment implications for those supporting individuals with AS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Movement Performance and Asperger’s Syndrome
Asperger’s syndrome (AS) is a condition largely considered in terms of dysfunction in the social domain. However, there have also been accounts of abnormal motor performance in children with AS going as far back as Hans Asperger’s early descriptions of the condition (1944). Subsequent reports have described high frequencies of relatively poorly specified disturbances in motor performance (Rinehart et al. 2001; Ghaziuddin and Butler 1998; Ghaziuddin et al. 1994). A variety of problems in motor coordination have been reported with children being described as clumsy or dyspraxic (Frith 1991), having impaired skills in playground games and hand-writing (Wing 1981), and lacking balance. Children with AS also show problems ignoring obstructions, for example, tripping over other people’s feet (Aarons and Gittens 1992). Green and colleagues have found that boys with AS meet criteria for motor impairment, with ball skills mainly being affected (Green et al. 2002). More recently, a study of 16 boys diagnosed with AS or high functioning autism (HFA) described problems in balance and motor skills and evidence of diadochokinesis, suggesting possible disturbances in motor planning. These observations may imply that individuals with autism spectrum conditions face problems with information processing. In addition, the authors noted a strong association between motor abilities, social withdrawal, and severity of autistic traits, suggesting that motor impairment is more integral to autism spectrum than previously thought (Freitag et al. 2007). Using a neurologic examination standardised for children, Jansiewicz et al. (2006) observed that HFA and AS participants displayed significant motor impairment compared to controls, with no significant differences between HFA and AS groups. However, some literature suggests that some aspects of motor problems seem to be specific to AS. When compared to participants with autism, Iwanaga et al. (2000) found that children with AS fell down on a standing and walking task more than those with HFA. The authors suggest this was a consequence of an impairment of a basic component of movement when standing. They further state that this may explain why some children with AS reportedly have an awkward stance and walk (Gillberg 1989). Rinehart et al. (2006) report motor planning deficits in people with HFA and people with AS, although they further suggest that there are qualitative differences in the deficit between these groups, which manifests as ‘motor clumsiness’ in AS and ‘abnormal posturing’ in HFA.
Sensory Integration and the Sensorimotor System in AS
The sensorimotor system is the mechanism that acquires sensory stimuli from the environment and integrates them in the central nervous system, thereby generating motor responses by activating various muscles for locomotion and performance of functional tasks (Fisher et al. 1991). There is compelling evidence to suggest that the sensorimotor system in AS, and in other autism spectrum conditions, is atypical. A recent article reports that 76% of Swedish preschool children diagnosed with ASD demonstrated a major abnormality in at least one sensory modality, and that this was particularly notable in two subgroups, including an AS subgroup (Klintwall et al. 2011).On a cerebral level, the somatosensory cortex processes proprioceptive information in order to provide conscious awareness of joint position and joint motion (Lephart and Fu 2000). A recent study has shown that there is an increased dependency on proprioception in autism conditions with stronger links between self-generated motor control and proprioceptive feedback than would be expected (Haswell et al. 2009). Further, this study showed an association between severity of social impairment and over-reliance on propriception (Haswell et al. 2009). In AS, people show deficits in body posturing, tandem gait and balance with closed eyes, which may indicate deficits in sensory modalities rather than the motor pathway (Weimer et al. 2001). Using the Sensory Profile Test (Dunn 1999), Dunn et al. (2002) found that children with AS scored significantly lower than typically developing children in 22 out of 23 items of the test, which is designed to measure multi-sensory abilities and assess the effect of this on performance. McAlonan and colleagues have shown that people with AS show impaired sensory gating, demonstrated by inhibition of the startle-prepulse in a test of prepulse inhibition (PPI), a neurological phenomenon in which a weak stimulus reduces the reaction to a second, stronger stimulus. The AS participants in that study did not modulate their response following the weak stimulus, which the authors suggest may be linked to volume reduction in grey matter in frontostriatal and cerebellar regions and excess white matter around the basal ganglia, as shown by MRI scanning (McAlonan et al. 2002). The authors note that findings from scanning comply with a theory postulated by Damasio and Mauren (1978) that clinical symptoms of autism, including motor disturbance would involve a system incorporating the frontal lobe and basal ganglia (Damasio and Mauren 1978).
Problems with sensory organisation have been demonstrated through deficits in ‘sway-referenced’ (balance) trials in people with autism. Difficulty with postural stability has been shown to be particularly notable when somatosensory processing was relied upon, and suggests a disturbance of multi-sense integration (Minshew et al. 2004). The authors of that study noted that as the participants did not have intellectual disability, the problems with stability could be directly related to autism. In the general population one sensorimotor model that has generated clinically useful therapeutic interventions, together with a standardised clinical assessment, is that of Sensory Integration theory. This theory states that “sensory integration is a neurobiological process that organises sensation from one’s own body and from the environment and makes it possible to use the body effectively within the environment.” (Ayres 1989, p. 11). According to sensory integration theory, problems in motor coordination in children are usually somatosensory-based and may include somatodyspraxia, a term utilised by Ayres (1989) to describe the difficulty in planning and carrying out skilled motor acts in the correct sequence. Using the ‘body effectively within the environment’ is ultimately reliant on motor skills, and thus it is clear from Ayres’ theory how disrupted sensory integration could lead to problems in motor function.
Development of Motor and Sensory Atypicalities
It has been suggested that movement problems in AS may be linked to developmental delay, with learning to walk in young children with autism spectrum conditions being delayed by several months (Manjiviona and Prior 1995). However, there is evidence of motor deficits persisting into adulthood in young adults with AS (Sahlander et al. 2008). Similarly, Minshew et al. (2004) reported that people with autism showed difficulty with postural control, never reaching levels of typically developing adults.
Despite advances in recent years the picture of sensory function in AS and its behavioural manifestations is still unclear and remains under-investigated, often overlooked in favour of studies of social cognition. Characterising movement and sensory profiles in AS is essential in supporting the future development of approaches to overcoming disturbances in sensorimotor functioning. The aims of this study were (a) to simultaneously investigate motor and sensory performance in children with AS in the context of Sensory Integration Theory and (b) to examine whether performance was affected by development. This should go some way to understanding if poor performance is the result of developmental delay.
Performance across a range of tasks sensitive to discrete proprioceptive and vestibular functions was examined. We hypothesised that children with AS would have a generalised impairment of these motor and sensory abilities compared to typically developing individuals. Furthermore, we investigated the relationship between sensorimotor performance and age, in order to examine whether any expected sensorimotor impairments observed in the AS group lessened with age.
Methods
Design
The Movement Assessment Battery for Children–2 (MABC-2; Henderson et al. 2007) and the Sensory Integration Praxis Test (SIPT; Ayres 1989) were used to investigate sensorimotor performance in a group of boys with AS and a matched control group. Overall frequencies of impaired performance (relative to standardised scores) were compared between the AS and the control participants. In addition, developmental trajectories in these groups were examined by comparing sensorimotor performance across age.
Participants
Fifty male children aged 7–14 years with AS were recruited together with 50 age-matched typically developing boys by contacting schools and educational authorities in England and by placing a notice on the National Autistic Society website. Exclusion criteria included diagnosis of developmental coordination disorder (DCD), severe sensory abnormalities and evidence of intellectual disability.
AS Group
All AS participants had a diagnosis of AS made by a clinical service according to criteria set out by DSM-IV and ICD-10. As a secondary verification, we also interviewed parents using the Autism Diagnostic Inventory-R (Rutter et al. 1994). We were not able to interview eight of the 50 participants. The mean subtest scores for those interviewed are: social interaction mean 23.3 ± 6.3, range 11–30; communication and language mean 19.7 ± 4.9, range 11–26; restricted and repetitive behaviours mean 8.4 ± 3.3, range 1–12; abnormalities of development evident at or before 36 months mean 3.6 ± 1.4, range 1–7. Medical, psychological and educational reports were inspected by the research team to further verify suitability. IQ was measured with the Wechsler Abbreviated Scale of Intelligence (WASI; The Psychological Corporation 1999). AS participants had a mean age of 10.72 years (SD = 2.55) and full scale IQ of ≥80, with a mean score of 106 (SD = 15.1).
Control Group
To exclude the possibility of an undiagnosed autism spectrum condition the parents of the control participants were interviewed with the Childhood Asperger Syndrome Test (CAST) and none of the selected children scored at or above the cut-off of the test (Williams et al. 2005). Control participants had a mean age of 10.84 years (SD = 2.21) and no intellectual disabilities. According to their parents they had no known neurological or psychiatric disorder and were not on medication.
Assessments
Movement Assessment Battery for Children–2 (MABC-2)
The MABC-2 was developed by Henderson et al. (2007) and has been standardised on 1172 children aged between 3 and 16 years in the UK. The MABC-2 takes approximately 40 min to complete. It assesses three domains of motor ability: (a) Manual Dexterity (threading a lace), (b) Aiming and Catching (throwing and caching a tennis ball) and (c) Balance (balancing on a board, walking heel to toe).
Sensory Integration & Praxis Test (SIPT)
The SIPT developed by Ayres (1989) has been standardised on 1997 children aged between 4 and 8 years. It focuses on the processing and integration of sensory information, and how this is reflected in movement. In the current study seven tasks were selected that examine the effect of sensory processing (vestibular and proprioceptive processing) on motor ability, as described in Table 1.
Procedure
Each participant was assessed in a single session. Before the testing procedure every task was explained and participants had one or two practice trials. All participants were assessed on the MABC-2 test first and then the SIPT. During the testing procedure all participants had two breaks of 10 min each.
Analysis
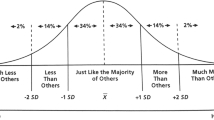
Raw scores from each task of the MABC-2 were standardised, based on the age of the participants, to an equivalent standard score corresponding to the percentile rank of the performance in the general population according to MABC-2 guidelines. This gives a performance score for each of the three domains of the test and a total motor performance score for the whole MABC-2. Individual scores from each of the seven tasks employed from the SIPT were calculated and transformed, according to the test guidelines, into z scores against the normative sample of the test, reflecting the magnitude of deviation from them. Scores from the MABC-2 and each of the seven tasks from the SIPT were checked for normality in distribution in each group by tests for skewness (normality between −1 and 1) and kurtosis (normality between −3 and 3) using SPSS (SPSS Inc., IL, USA). MABC-2 scores were analysed using multivariate ANOVA. As some components of SIPT did not follow a normal distribution, scores for SIPT were analysed using unpaired t test comparisons if normality was met and Mann–Whitney tests if normality was not met.
Possible effects of age on MABC-2 or SIPT performance were examined by assessing main effects and interaction of group and age using an ANCOVA in SPSS. Significance levels are set at p < 0.05 throughout.
Ethical Considerations
Ethical approval was obtained from the Local Research Ethics Committee. The experimenters adhered to the code of conduct authorized by their research institutes. The basic rights to privacy and respect of the participants were followed and all personal information remains confidential.
Results
Group Differences in Performance on the MABC-2
Figure 1 shows that control participants scored higher on MABC-2 overall (Fig. 1a; p < 0.01, t = −13.92). Control participants obtained a group mean score of 11.3 (±0.31 sem), scoring higher than the AS group whose mean score was 5.1 (±0.32 sem). Controls scored higher than AS participants in the individual tests comprising the MABC-2 (Fig. 1b), attaining a mean of 12.48 (±0.31) compared to 6.08 (±0.41) for Aim and Catch; 8.88 (±0.36) compared to 5.24 (±0.31) for Manual Dexterity; and 12.28 (±0.29) compared to 6.8 (±0.38) for Balance respectively. A multivariate ANOVA showed a statistically significant difference between groups by domain F (3, 96) = 72.23; p < 0.001; Wilk’s Lambda = 0.31; partial eta squared = 0.69. Considered separately, results for the dependent variables demonstrated significantly impaired performance on each of the constituent domains of the MABC-2 compared to the control group (Fig. 1b; p < 0.001, Bonferroni adjusted, for aim and catch, F (1, 98) = 152.5; manual dexterity, F (1, 98) = 59.41 and balance, F (1, 98) = 132.31, respectively).
a Overall performance on MABC-2 for control and AS participants. White dots represent controls whilst black dots represent AS participants. ***indicates that p < 0.001; **p < 0.01; *p < 0.05, respectively. b Performance on aim and catch, dexterity and balance components within MABC-2 for control and AS participants. ***indicates that p < 0.001; **p < 0.01; *p < 0.05, respectively
After checking for outliers and linearity of fit, performance on MABC-2 was found not to correlate with any of the ADI subset scores, as measured by Pearson one-tailed correlation coefficient (p > 0.05; data not shown).
Performance on the Sensory Integration & Praxis Test (SIPT) Tasks
Figure 2 indicates that control participants scored higher than the AS group on all seven aspects of SIPT. Controls scored a mean of 0.91 (±0.12) compared to −0.46 (±0.13) for kinaesthesia; 0.94 (±0.09) compared to −0.75 (±0.17) for graphaesthesia; 1.69 (±0.11) compared to –0.17 (±0.18) for localisation; 1.38 (±0.1) compared to −0.83 (±0.2) for postural praxis; 1.17 (±0.08) compared to −0.92 (±0.16) for sequencing praxis; 1.4 (±0.09) compared to −0.34 (±0.15) for bilateral motor control; and 1.92 (±0.12) compared to −0.94 (±0.17) for standing and walking balance. Analysis using t tests (and Mann–Whitney tests for those results that were not normally distribution) confirmed that these differences were statistically significant. Figure 2a–g, Bonferroni adjusted; p < 0.001 for kinaesthesia, t = −7.74; graphaesthesia, t = −8.71; localisation of tactile stimuli, t = −8.76; postural praxis, U = 228.5, z = −7.06; sequencing, t = −11.64; bilateral motor coordination, U = 153.5, z = −7.58; and standing and walking balance, t = −13.53, respectively.
Performance on the Movement Assessment Battery 2 (MABC-2) Across Ages
We investigated whether or not, within the age ranges included in this study, there was a differential rate of sensorimotor development in AS and if that determined impairment in motor performance, by use of ANCOVA. Age was entered as a covariate predictor and was found not to interact with group in predicting score. There were no significant effects of age or interaction effects for overall MABC-2 score or in MABC-2 components (p > 0.05; data not shown).
Performance on the Sensory Integration & Praxis Test (SIPT) Across Ages
Using ANCOVA with age as a covariate we found that there were no significant interaction effects of age and clinical group in any of the seven components of the SIPT investigated (p > 0.05; data not shown).
Discussion
In this study, validated measures were used to describe aspects of movement performance and sensory integration performance in a group of boys with AS compared to a control group comprising age-matched typically developing boys. We have demonstrated that participants with AS have significant impairments across the sensorimotor functions investigated. The impaired motor performance reflected in the MABC-2 test scores confirms previously reports that children with AS have atypical motor functioning (e.g. Rinehart et al. 2001; Attwood 1998; Wing 1981). Our findings also suggest that movement and SIPT problems persist into later childhood.
We suggest that movement performance in AS may be underlined by problems with sensory integration, although we acknowledge that our chosen assessments make defining causation difficult. Nonetheless, our data are compatible with the suggestion that these impairments are underpinned by an underlying difficulty with processing proprioceptive and other sensory information (Weimer et al. 2001) and may suggest that AS participants employ atypical internal models relating motor coordination to proprioception as previously suggested (Haswell et al. 2009). According to the literature, proprioceptive and vestibular processing and tactility have a substantial impact on movement performance (Lephart and Fu 2000; Smith-Roley et al. 2001) and problems in these senses can disrupt ‘body schema’ (the internalised model of the body in action). In AS, this may have generated problems in motor planning, where it appears that individuals had difficulties in planning simple actions perhaps because of sensory impairments. This could explain the difficulty individuals with AS had in keeping their balance in the MABC-2 balance task and their impaired performance on the SIPT standing and walking balance task. Moreover, participants with AS scored lower in the graphaesthesia and localisation tasks, which are associated with the interpretation of tactile and proprioceptive information, and in postural praxis, which is considered as an indicator of dyspraxia, itself associated with problems in sensory processing (Ayres 1989). Poor performance on the bilateral motor coordination task in the current study further suggests that participants with AS faced motor impairments associated with weak proprioceptive and vestibular processing (Ayres 1989). Defining the causative relationship between movement performance and sensory integration should be a target for further studies.
Our findings raise a question as to whether it is more appropriate to consider the sensorimotor impairments observed in AS as a symptom set forming part of the core nature of the syndrome (Kaplan et al. 2001, 2006) or as a co-existing condition, as some children with AS do not have significant movement problems (Dewey and Tupper 2004). The current study showed that atypical function is present to a significant degree in most of those with AS, rather than just being a particular problem for a small proportion, which may suggest that this is a core part of the syndrome. However, a number of participants with AS did not demonstrate movement difficulty to the same extent as the majority of the group. Detailed interviews revealed that one of the boys with AS, who demonstrated performance on the balance task close to that of typically developing children spent a significant amount of time skate-boarding, which may have improved his balancing abilities. Another boy, who demonstrated good fine-motor skills but great difficulty riding a bicycle, had special interest in playing the guitar. Although we cannot be certain of the direction of the relationship (as boys with fine motor skills might be drawn to guitar playing), these examples may give us hope that motivation and practice could help to improve movement performance in AS, which Barnett and Henderson (1992) have previously observed with individuals with DCD.
Impairments in movement performance and sensorimotor processing cause anxiety and confusion when individuals with AS have to participate in novel activities. This could be an additional factor contributing to the manifestation of behavioural problems and the tendency to develop fixed routines of activities (Smith-Roley et al. 2001). Children with DCD have poor self esteem and self perception with respect to physical activities and have limited participation in sports teams or play time (Chen and Cohn 2003; Losse et al. 1991). We suggest that poor movement performance may exacerbate the reduced opportunities for social inclusion experienced by individuals with AS, as typically developing children are reported to value performance in sports more than for example, academic performance (Nikitaras and Ntoumanis 2003; Chase and Dummer 1992). Individuals with AS could be a target for bullying because of low self esteem, anxiety in social settings, lack of confidence and limited success in sports (Attwood 2007). Adolescents with AS are less physically fit than peers (Borremans et al. 2010), which may be the consequence of a vicious cycle of anxiety and poor performance impacting on sports participation. This clearly will impact on physical health and underlines the importance of addressing movement difficulties. Movement performance and associated psychological barriers should be considered in intervention programmes for children with AS.
There were some limitations to our study. SIPT is standardised for children younger than in our sample which may explain why the controls performed so well, and makes the AS deficits even more profound. We acknowledge that anxiety and impulsivity that characterises AS could have affected performance. We have suggested that problems with performance in childhood may persist into later life. This is in line with another study that showed that people with autism did not reach adult levels of postural control (Minshew et al. 2004). However, that study did show improvement in the autism group from age 12, perhaps suggesting that our age range was limited. Despite this, we believe that our findings from validated tasks within a large cohort are very valuable and should inform further research and services.
Conclusions
This research on sensorimotor performance in people with AS has attempted to investigate an important aspect of everyday life for children with AS that has been relatively neglected in favour of a focus on social cognitive aspects of AS. Individuals with AS face significant impairments in movement performance and sensory processing and consideration of these could benefit well being in clinical and educational settings responsible for supporting children with AS.
References
Aarons, M., & Gittens, T. (1992). The handbook of Autism. A guide for parents and professionals. London: Routledge.
Attwood, T. (1998). Asperger's syndrome a guide for parents and professionals. London: Jessica Kingsley Publishers.
Attwood, T. (2007). The complete guide to Asperger’s syndrome. London: Jessika Kingsley Publishers.
Ayres, A. J. (1989). Sensory integration and praxis tests. California: Western Psychological Publishers.
Barnett, A. L., & Henderson, S. E. (1992). Some observations on the figure drawings of clumsy children. British Journal of Educational Psychology, 62, 341–355.
Borremans, E., Rintala, P., & McCubbin, J. A. (2010). Physical fitness and physical activity in adolescents with Asperger syndrome: A comparative study. Adaptive Physical Activity Quarterly, 4, 308–320.
Chase, M. A., & Dummer, G. M. (1992). The role of sports as a social status determinant for children. Research Quaterly for Exercise and Sport, 63(4), 418–424.
Chen, H., & Cohn, E. S. (2003). Social participation for children with developmental coordination disorder: Conceptual evaluation and intervention considerations. Physical and Occupational Therapy in Pediatrics, 23(4), 61–78.
Damasio, A. R., & Mauren, R. G. (1978). A neurological model for childhood autism. Archives of Neurology, 35, 777–786.
Dewey, D., & Tupper, D. E. (Eds.). (2004). Developemental motor disorders. A Neuropsychological Perspective. London: Guilford Press.
Dunn, W. (1999). Sensory profile. San Antonio TX: The Psychological Cooperation.
Dunn, W., Myles-Smith, B., & Orr, S. (2002). Sensory processing issues associated with Asperger syndrome: A preliminary investigation. American Journal of Occupational Therapy, 56(2), 97–102.
Fisher, G. A., Murray, E. A., & Bundy, A. A. (1991). Sensory integration. Theory and practice. Philadelphia: F.A. Davis Company.
Freitag, C. M., Kleser, C., Schneider, M., & von Gontard, A. (2007). Quantitative assessment of neuromotor function in adolescents with high functioning autism and Asperger syndrome. Journal of Autism and Developmental Disorders, 37, 948–959.
Frith, U. (1991). Autism and Asperger’s syndrome. Cambridge: Cambridge University Press.
Ghaziuddin, M., & Butler, E. (1998). Clumsiness in autism and Asperger syndrome: A further report. Journal of Intellectual Disability Research, 42(1), 43–48.
Ghaziuddin, M., Butler, E., Tsai, L., & Ghaziuddin, N. (1994). Is clumsiness a marker for Asperger’s syndrome? Journal of Intellectual Disability Research, 38, 519–527.
Gillberg, C. (1989). Asperger syndrome in 23 Swedish children. Developmental Medicine and Child Neurology, 31, 520–531.
Green, D., Baired, G., Barnett, A. L., Henderson, L., Huber, J., & Henderson, S. E. (2002). The severity and nature of motor impairment in Asperger’s syndrome: A comparison with specific developmental disorder of motor function. Journal of Child Psychology, 43(5), 655–668.
Haswell, C., Izawa, J., Dowell, L. R., Mostofsky, S. H., & Shadmehr, R. (2009). Representations of internal models of action in the autistic brain. Nature Neuroscience, 12(8), 970–972.
Henderson, S. E., Sugden, D. A., & Barnett, A. L. (2007). Movement assessment battery for children-2 (Movement ABC-2) (2nd ed.). London: Harcourt Assessment.
Iwanaga, R., Kawasaki, C., & Tsuhada, R. (2000). Brief Report: Comparison of sensory-motor and cognitive function between autism and Asperger’s syndrome in preschool children. Journal of Autism and Developmental Disorders, 30(2), 169–174.
Jansiewicz, E. M., Goldberg, M. C., Newschaffer, C. J., Denckla, M. B., Landa, R., & Mostofsky, S. H. (2006). Motor signs distinquish children with High Functioning Autism and Asperger’s syndrome from controls. Journal of Autism and Developmental Disorders, 36, 613–621.
Kaplan, B. J., Crawford, S., Cantell, M. H., Kooistra, L., & Dewey, D. (2006). Comorbidity, co-occurrence, and continuum: What’s in a name? Child: Care, Health and Development, 32(6), 723–731.
Kaplan, B. J., Dewey, D., Crawford, S., & Wilson, B. N. (2001). The term co-morbidity is of questionable value in reference to developmental disorders: Data and theory. Journal of Learning Disabilities, 34(6), 555–565.
Klintwall, L., Hom, A., Eriksson, M., Höglund Carlsson, L., Barnevik Olsson, M., Hedvall, Å., et al. (2011). Sensory abnormalities in Austism: A brief report. Research in Developmental Disabilities, 32, 795–800.
Lephart, S. M., & Fu, F. H. (Eds.). (2000). Proprioception and neuromuscular control in joint stability. Leeds: Human Kinetics.
Losse, A., Henderson, L., Elliman, D., Hall, D., Knight, E., & Jongmans, M. (1991). Clumsiness in children-do they grow out of it? A 10-year follow-up study. Developmental Medicine and Child Neurology, 33, 55–68.
Manjiviona, J., & Prior, M. (1995). Comparison of Asperger syndrome and high-functioning autistic children on a test of motor impairment. Journal of Autism and Developmental Disorders, 25(1), 23–29.
McAlonan, G. M., Daly, E., Kumari, V., Critchley, H. D., van Amelsvoort, T., Suckling, J., et al. (2002). Brain anatomy and sensoritmotor gating in Asperger’s syndrome. Brain, 127, 1594–1606.
Minshew, N. J., Sung, K., Jones, B. L., & Furman, J. M. (2004). Underdevelopment of the postural control system in autism. Neurology, 63, 2056–2061.
Nikitaras, N., & Ntoumanis, N. (2003). Criteria of personal, boys' and girls' popularity as ranked by Greek adolescents. Perceptual and Motor Skills, 97, 281–288.
Rinehart, N. J., Bellgrove, M. A., Tonge, B. J., Brereton, A. V., Howells-Rankin, D., & Bradshaw, J. L. (2006). An examination of movement kinematics in young people with high-functioning autism and Asperger’s disorder: Further evidence for a motor planning deficit. Journal of Autism and Developmental Disorders, 36, 757–767.
Rinehart, N. J., Bradshaw, J. L., Brereton, A. V., & Tonge, B. J. (2001). Movement preparation in high-functioning Autism and Asperger’s disorder: A serial choice reaction time task involving motor reprogramming. Journal of Autism and Developmental Disorders, 31(1), 79–88.
Rutter, M., LeCourteur, A., & Lord, C. (1994). Autism diagnostic interview, revised (ADI-R). Los Angeles: Western Psychological Services.
Sahlander, C., Mattsson, M., & Bejerot, S. (2008). Motor function in adults with Asperger’s disorder: A comparative study. Physiotheapy Theory Practice, 24, 73–81.
Smith-Roley, S., Imperatore-Blanche, E., & Schaaf, R. (2001). Understanding sensory integration with diverse populations. New York: Therapy Skill Builders.
WASI. (1999). Wechsler abbreviated scale of intelligence. San Antonio: The Psychological Corporation.
Weimer, A., Shatz, A. M., Ballantyne, A. O., & Trauner, D. A. (2001). Motor impairment in Asperger syndrome: Evidence for a deficit in proprioception. Journal of Developmental and Behavioural Paediatrics, 22, 92–101.
Williams, J., Scott, F., Scott, C., Allison, C., Bolton, P., Baron-Cohen, S., et al. (2005). The CAST (Childhood Asperger Syndrome Test). Autism, 9(1), 45–68.
Wing, L. (1981). Asperger’s syndrome: A clinical account. Psychological Medicine, 11, 115–129.
Acknowledgments
We are very grateful to the children, their parents and their teachers who participated in the study, to the U.K. National Autistic Society and to the UK Sensory Integration Network. We would like to thank for supporting this research project the Greek Scholarships Foundation and the UK Health Foundation. Also we would like gratefully to acknowledge Professor Simon Baron-Cohen, Dr. Lorna Wing & Dr. Judith Gould for their support and advice on this research project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siaperas, P., Ring, H.A., McAllister, C.J. et al. Atypical Movement Performance and Sensory Integration in Asperger’s Syndrome. J Autism Dev Disord 42, 718–725 (2012). https://doi.org/10.1007/s10803-011-1301-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-011-1301-2