Abstract
General practitioners (GPs) could have an important role in early diagnosis of autism. There have been no studies evaluating the knowledge of GPs regarding autism in Pakistan. We aimed to fill that gap by assessing knowledge and attitude of GPs in Karachi regarding autism. We conducted a cross-sectional survey of 348 GPs; only 148 (44.6%) had heard of “autism.” Our results show that GPs less than 30 years of age and those who obtained their Medical Degree in the last 5 years are more likely to report knowledge about autism: OR = 3.0; 95% CI: 1.71, 5.31, and OR = 2.56; 95% CI: 1.48, 4.42, respectively. In addition, among those reporting knowledge about autism, many held misconceptions regarding the signs and symptoms and etiology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Autism Spectrum Disorders (ASDs) are complex, lifelong neurodevelopmental and behavioral disorders manifesting in infancy or early childhood. Although the causes of ASDs are unknown, evidence suggests that the origins are likely genetic or the result of gene-environment interaction occurring in utero or very early in infancy. ASDs are characterized by impairments in social interaction and communication and by repetitive behavior (Rapin 1997). The prevalence of ASDs appears to be on the rise in developed countries and has become a serious public health concern (Fombonne 2005; Centers for Disease Control and Prevention (CDC) 2007) leading to commitment of resources to accurately assess prevalence and identify related risk factors (Centers for Disease Control and Prevention (CDC) 2007). In the developing world, however, reliable epidemiologic data on ASDs are rare due to a lack of research infrastructure and available research training programs. Epidemiological research in developing countries, where the environmental exposures may be very different from developed countries, will broaden epidemiological understanding of autism worldwide and lead to a better understanding of the etiology of ASD.
Pakistan is a developing country in South Asia with a population of 174(US Census Bureau 2009)—181 million (Population Reference Bureau 2009). Pakistan has approximately 63 medical education institutions of which 36 are private (Pakistan Medical and Dental Council 2009a). Only a few provide research training or offer workshops in health research (Dodani and LaPorte 2008). During the past three decades there has been an increase in the number of private medical schools in Pakistan that have developed formal health research training programs, including public health (Akhtar and Khan 2000). For example, during the past two decades Aga Khan University (AKU) has developed the first Masters level graduate training program in Epidemiology and Biostatistics, Health Policy Management, and a PhD level training program in Health Sciences. These are high quality health research training programs. However, for a country with a population of over 174 million people, the number of health related scientists is still very limited (Hyder et al. 2003).
In South Asian developing countries, including Pakistan, the prevalence of ASDs is unknown. This stems largely from a lack of existing research infrastructure and availability of well-trained and experienced human resources for conducting autism surveillance and research. In Pakistan, General Practitioners (GPs) constitute the backbone of the health care system as they are responsible for the initial assessment and treatment of about 80% of patients (Rauf and Saeed 2007). Since the majority of GPs in Pakistan practice in private clinics, it is critical that they have sufficient knowledge and skills to diagnose and manage not only common health problems, but also rarer disabilities, such as autism (Rauf and Saeed 2007), and that they are encouraged to make appropriate referrals. Therefore, knowledgeable GPs are a critical component of autism surveillance and research. In order to keep GPs abreast of new research findings regarding autism and have them effectively contribute to autism surveillance, it is critical that they are provided with training opportunities in epidemiology, biostatistics, etiology, and diagnosis of various diseases or health problems.
Several studies have evaluated GPs’ knowledge and skills related to common health problems and other disorders in South Asia including Pakistan. For example, a cross-sectional study evaluated the knowledge and practice of GPs and pediatricians regarding Attention Deficit Hyperactivity Disorder (ADHD) and Learning Disorder (LD) in Karachi. This study reported that only 13.7% of GPs and 21.6% of pediatricians had sufficient knowledge to screen and diagnose ADHD. More importantly, no GPs were adequately familiar with associated factors and clinical symptoms of LD (Jawaid et al. 2008). Similar studies have assessed the knowledge and skills of GPs in Pakistan and India (Roy et al. 2005) regarding common health problems and other disorders including diabetes (Kumar et al. 2006a), cancer and palliative care (Shaikh et al. 2008), helicobacter pylori infection (Ahmed et al. 2009), tuberculosis (Rizvi and Hussain 2001; Shah et al. 2003; Shehzadi et al. 2005; Vandan et al. 2008, 2009), acute respiratory infections (Iqbal et al. 1997), acute diarrhea (Patwari et al. 1991), malaria (Kamat 2001), sexually transmitted infections (Khandwalla et al. 2006), AIDS (Dobe 1995) and preventing tetanus (Dabas et al. 2005; Kumar et al. 2006b). These studies demonstrate that a high percentage of GPs in Pakistan and India lack sufficient knowledge regarding diagnosis and management of these diseases. Only one study has assessed diagnostic practices for autism among health care professionals; an Indian study that included 165 psychiatrists, 95 psychologists, and 677 pediatricians distributed educational packets about autism to the pediatricians who responded to the survey. This study reported that professionals perceived autism as a rare disorder and that most did not consider language disturbances central to the diagnosis of autism. About 80% of participants reported that the diagnosis of autism is difficult (Daley and Sigman 2002). A pilot study in Singapore, a more developed South Asian country, reported that most of the GPs lack sufficient knowledge regarding childhood developmental and behavioral disorders (Lian et al. 2003). However, to the best of our knowledge, there have not been any studies that systematically evaluate the knowledge and practices of GPs regarding ASDs in Pakistan or in any other developing countries in South Asia. Autism diagnosis is frequently missed in some developing countries in South Asia, including Pakistan, due to a lack of knowledge regarding its etiology and diagnostic criteria among health professionals (Kalra et al. 2005; Singhi and Malhi 2001). Improving knowledge among health professionals regarding autism is an essential component of research infrastructure in developing countries that would enable implementation of effective autism surveillance and research programs. Therefore, in this research we aimed to assess the knowledge and attitudes of GPs regarding ASDs in Karachi, the most populated city in Pakistan. Since several developing countries in South Asia follow a similar system of medical education (e.g., India, Pakistan, Bangladesh, Sri Lanka) and have similar infrastructure for health research, we believe our study findings may shed light regarding knowledge, attitude and practices of GPs regarding autism, an essential component of research infrastructure for autism in these South Asian countries.
Methods
Participants and Design
We conducted a cross-sectional survey of 348 GPs in Karachi, Pakistan during June–August 2007. Pakistan is a developing country with a population of approximately 181 million (Population Reference Bureau 2009). According to the World Bank, Pakistan ranks 26th in terms of Gross Domestic Product (GDP) and belongs to lower- middle income developing country (World Bank 2008). The health budget was 3.9% of GDP in 2004 (World Health Organization 2005). Karachi is the largest metropolitan city in Pakistan with a population of nearly 14.5 million during the study period.
In order to practice medicine in Pakistan, physicians must be certified and licensed by the Pakistan Medical and Dental Council (PMDC), the national regulatory organization for medical education that sets standards for basic and higher qualifications in Medicine and Dentistry (Khan 2004). A total of 116,009 working physicians were registered in Pakistan during the study period of which 49009 were registered in Sindh province (Pakistan Medical and Dental Council 2009b), where Karachi is located.
For the sampling frame, we used the Mediguide: Comprehensive Medical Directory 5th Issue (Medi Publications: House of Medical Publications 2006) that lists 5,849 general practitioners for the city of Karachi.
Field work for this study was coordinated at Aga Khan University (AKU). The initial sampling focused on GPs practicing within a 30-min driving distance from AKU. Our goal was to recruit 384 practitioners. The initial distance was increased to ensure that we met our enrollment goal. Additionally, we sampled from private clinics and large government and private hospitals.
GPs with an MBBS (Bachelor of Medicine, Bachelor of Surgery) degree in Karachi, who were registered with Mediguide and provided verbal consent, were considered for this study. Physicians who worked in a military cantonment or military hospital, practiced as homeopathic practitioners, and had medical degrees to qualify them as medical specialists were not included in this study. All study participants (n = 348) were personally interviewed by the study coordinator and a team of research assistants selected from a pool of AKU and Dow Medical College students.
Sample Size and Power
The sample size calculation for this research was based on an estimation of the proportion of GPs in Karachi who are aware of ASDs. In order to estimate the proportion of GPs who are knowledgeable about ASDs within a margin of error of 5% with 95% confidence, we needed to interview about n = 384 GPs. The actual number of GPs interviewed for this study was 348. However, our post-hoc power analysis showed that this sample size was sufficient to detect significant observed odds ratios reported here with a power of at least 80%.
Procedure
A questionnaire was developed with four main sections. The first section asked about the demographics of the participating GPs, including age, sex, average number of patients seen weekly, average time spent for each patient, place/institution of medical training, number of years since graduation, number of years engaged in clinical practice, and whether they have heard of “autism.” Questions in the second section asked about sources of GPs’ knowledge of ASDs. At the beginning of the second section, if the GP indicated they had never heard of “autism,” the interviewer provided a brief description of autism. If the GP was still unaware of autism after the explanation, the interviewer did not continue the administration of the rest of the questionnaire.
The third section collected information about GPs’ attitudes toward the care of autistic children. The last section contained questions regarding physicians’ practices, such as administration of diagnostic tests and their referral process to appropriate specialists.
As medical education in Pakistan is delivered in English, the questionnaire was administered in English. To account for the differences between spoken English in Pakistan and the US, the questionnaire was pilot-tested with two Pakistani physicians who worked in the US. The pilot testing provided an opportunity to establish conceptual clarification, cultural congruence, and receive recommendations for feasibility of administration.
The data were doubly entered using paper forms and compared with the first entry such that discrepancies were resolved.
Descriptive statistics were used to characterize GPs who participated in this survey. The proportion of GPs who reported knowledge about autism was estimated. Independent two-sample t-tests were used to assess the association between ASD knowledge (Knowledgeable vs. not Knowledgeable) and continuous variables. Finally, logistic regression was used to identify factors associated with knowledge about autism among the GPs in Karachi. Unadjusted and adjusted odds ratios (OR) and their corresponding 95% confidence intervals (CI) were calculated. The criterion for keeping factors in the multivariable analysis was set at a p-value of less than 0.05. All data analyses were performed with the Statistical Package for the Social Sciences (SPSS) 17.0 (SPSS Inc. 2009).
Results
A total of 348 GPs were interviewed. Of these, 16 GPs did not answer the main outcome variable: self-reported knowledge about autism. Therefore, a total of 332 GPs are included in this analysis. The mean age of GPs was 41.08 years, and about 67% of GPs were male. The average number of years since graduation was 16 years and the average number of years of practice was 14 years. Other summary characteristics of GPs are provided in Table 1.
Out of the 332 GPs analyzed, only 148 (44.6%) reported that they had heard of “autism.” Among those who had heard of “autism,” the reported sources of knowledge included the following: 45.5% from medical school training, 50.0% from medical journals, 53.4% from the media, and 5.6% from other organizations including pharmaceutical companies.
There was no significant difference by gender in relation to self-reported knowledge about autism: 43.8% for male versus 46.3% for female, (OR = 1.10; 95% CI: 0.69, 1.75). Physicians who were younger (age < 30) were more likely to report knowledge about autism (OR = 3.0; 95% CI: 1.71, 5.31). Physicians who obtained their first Medical Degree in the last 5 years were more likely to report knowledge about autism (OR = 2.56; 95% CI: 1.48, 4.42). Those who graduated from a private medical school were more likely to self-report knowledge about autism (OR = 2.29; 95% CI: 0.94, 5.63; p-value = 0.06). In addition, GPs who had psychology and/or pediatrics training during their ward rotation in medical school were more likely to report knowledge about autism as compared to the physicians who had neither of these rotations (OR = 2.35; 95% CI: 1.62, 3.96) (Table 2).
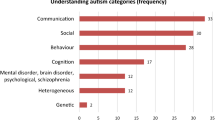
About 42% of those who reported having knowledge of autism also indicated working knowledge of autism in their practice (n = 62). Table 3 summarizes data concerning the knowledge and attitudes of GPs who claimed to have working knowledge of autism.
Discussion
ASDs affect millions of children in the world. Although the etiology of ASDs is not completely understood, early diagnosis of ASDs is important because it facilitates early intervention that has demonstrated improved educational and behavioral outcomes, including social, cognitive and communication functions (Fombonne 2005; Rapin 1997). Globally, pediatricians and GPs could have an important role in early diagnosis of autism (Committee on Children with Disabilities 2001; Barbaresi et al. 2006; Heidgerken et al. 2005; Johnson et al. 2007; Rhoades et al. 2007; Ashwell 2009). In most developing countries, including those in South Asia, GPs are often the only line of contact between the patient and the health care system and hence, may be responsible for the initial ASD diagnosis (Barbaresi et al. 2006; Kochanek 1991; Rauf and Saeed 2007; World Health Organization 2009) Therefore, development and implementation of any effective autism surveillance programs in these countries will require knowledgeable GPs as an essential component of the infrastructure that would enable effective and efficient ASD case identification.
Our data support that GPs in Karachi are deficient in their knowledge regarding autism. In fact, in our survey, more than half of GPs in Karachi (55.4%) reported that they had never heard of “autism.” About 42% of those who self-reported knowledge about autism (less than 20% of the total surveyed) indicated having a working knowledge of autism in their practice (n = 62). When these GPs were asked whether they agree with a true statement, “Autistic children show detachment from their parents,” most of the GPs (61%) agreed. However, when asked whether they agree with a false statement, “Autism is more prevalent among higher socioeconomic classes,” only 35.4% disagreed, 8.0% strongly disagreed, and 17.7% remained undecided. Similarly, when asked whether they agree with the statement, “Autism is more prevalent among higher educational classes,” only 37.0% disagreed, 9.6% strongly disagreed, and 20.9% remained undecided. This reported knowledge is contrary to recent epidemiological research findings that autism is prevalent among all socioeconomic and educational classes (Volkmar et al. 1997). Furthermore, only 27.4% disagreed, 9.8% strongly disagreed, and 29.0% remained undecided when asked if they agree with the statement, “Autism is a precursor for schizophrenia.” These views reflect the description of autistic children by the American Psychiatric Association in 1952 and 1968 (Volkmar et al. 1997). Findings in recent research show that patients with schizophrenia are significantly less likely to show symptoms of autism disorder (Konstantareas and Hewitt 2001). Interestingly, 16.1% strongly agreed and 29.0% agreed with the false statement, “Autism in children is mostly attributable to neglect in early childhood by parents.” This view reflects an outdated theory introduced by Kanner in 1943. Most recent studies suggest that autism is a multi-factorial disorder, perhaps a result of both genetic and environmental factors. Therefore, autism cannot be simply explained by cold parental interaction and neglect in childhood (Johnson et al. 2007; Volkmar et al. 1997). Finally, only 26.7% disagreed and 18.3% strongly disagreed with the false statement, “Autism is preventable.” A similar survey conducted at the University of Florida to assess the knowledge and beliefs about autism among 111 health professionals, including 20 pediatricians, 8 family practitioners, 18 psychiatrists, 5 neurologists, 9 speech pathologists, 16 clinical psychologists, and 35 other medical doctors or professionals (PhD, MS) working for the Center for Autism and Related Disabilities, reported that family practitioners’, pediatricians’ and neurologists’ belief patterns are consistent with outdated knowledge about autism. For example, the family practitioners, pediatricians, and neurologists were more likely to agree that autism occurs among higher socioeconomic and higher educational classes. Furthermore, primary health care providers were significantly more likely to attribute the causes of autism to parenting factors and parental psychopathology compared to specialists, psychiatrists, and speech pathologists (Heidgerken et al. 2005). To the best of our knowledge, we are the first to study knowledge of GPs related to ASDs in South Asian developing countries with a specific focus on Pakistan. However, a similar study has been conducted to assess knowledge of GPs regarding attention deficit hyperactivity disorder (ADHD) and learning disorder (LD) in Pakistan. This study reports that only 13.7% of GPs have sufficient knowledge to effectively screen for ADHD and none of the GPs are adequately familiar with the established risk factors and clinical symptoms of LD (Jawaid et al. 2008). Another study from Singapore evaluated the knowledge of GPs regarding childhood developmental and behavioral disorders and reported that only 37% of GPs achieved a passing (score of at least 75%) grade (Lian et al. 2003). Other studies from South Asia including Pakistan reported that a significant portion of GPs in South Asia lack sufficient knowledge and skills regarding diagnosis or management of common health issues, such as acute respiratory infections or tuberculosis (Ahmed et al. 2009; Aziz et al. 2006; Dabas et al. 2005; Dobe 1995; Kamat 2001; Kumar et al. 2006a, b; Patwari et al. 1991; Rizvi and Hussain 2001; Roy et al. 2005; Shah et al. 2003; Shaikh et al. 2008; Shehzadi et al. 2005; Uddin et al. 2008; Vandan et al. 2008, 2009). The data presented in this paper support that GPs in Pakistan are lacking important knowledge about autism and perhaps other diseases. Until GPs in Pakistan are knowledgeable about autism, significant ASD research progress cannot be expected.
Medical School Curriculum
Our survey revealed that only 12.9% of the GPs in Pakistan had psychiatry training and 44.1% had pediatrics training during ward rotations. Moreover, the GPs who had psychology and/or pediatrics training during ward rotations in medical school were more likely to report knowledge about autism as compared to those who had neither of these rotations (OR = 2.35; 95% CI: 1.62, 3.96). Among GPs who had heard about “autism,” only 45.5% reported that medical school was the source of their knowledge about autism. Shah et al. (2003) conducted a similar study in the United Kingdom to assess the effect of training during the medical school on medical students’ knowledge regarding autism. The study reported inadequate knowledge of senior medical students about autism and recommended that more emphasis be placed on teaching medical students about autism (Shah et al. 2003). The referral of ASD cases has increased after such educational intervention (Krishnamurthy 2008). A study conducted to assess the satisfaction of medical students in three public medical colleges in Karachi has shown that more than half of the senior medical students were not satisfied with the knowledge and skills gained in courses, including Behavioral Sciences and Pediatrics (Aziz et al. 2006).
All this evidence suggests that most GPs in Pakistan do not receive adequate training in child and adult psychiatry and neurology (Baig et al. 2006; Gadit 2008; Usman 2009; Wasay 2003). Psychiatry training is an important component of the medical curriculum (Walton and Gelder 1999). However, there are only about 300 psychiatrists and 85 consultant neurologists in Pakistan, for a population of over 174 million. This shortage of psychiatrists and neurologists in Pakistan may have an impact on the quality of medical education received in both private and public medical schools and the knowledge and practice of GPs regarding autism (Gadit 2006, 2007; Usman 2009). Herzig (2003) developed a new psychiatry curriculum to enable Malawi’s medical students (Central Africa) to address mental health issues and, as a result, observed an improved performance among medical doctors in promoting mental and behavioral health (Herzig 2003). Promoting psychiatric, pediatrics and neurology education, with an emphasis on training in general psychiatry, child psychiatry, and neurology in medical school curricula, might help improve the knowledge of GPs regarding autism (Gadit 2007; Herzig 2003; Walton and Gelder 1999). Some private medical schools in Pakistan have recognized the importance of structured training in Psychiatry (Gadit 2007) and included this training in their undergraduate medical curriculum with the resources available.
Health research training is also an important component of medical education that could help to develop critical thinking and inquiry based learning through research (Khan et al. 2006). Khan et al. (2009) conducted a study to evaluate the knowledge and attitudes of 339 residents and 70 interns towards research at Aga Khan University and identified poor level of knowledge towards research among both medical students and residents (Khan et al. 2009). Other investigations have concluded that there is only minimal research infrastructure in a majority of the medical schools in India (Deo 2008). As there have been significant advancements in various medical fields including autism in recent years, it appears that amending medical schools’ curricula and engaging medical students with research is an important strategy to improve knowledge and attitude of GPs toward autism in developing countries. Medical education institutions in Pakistan and India train a large number of GPs in South Asia and many of them continue their professional career in the United States (1,500 medical graduates enter residency training in US annually), Canada, the United Kingdom and several other western countries. However, in most of the medical schools in these developing countries, the medical curriculum has not been changed or updated to reflect new advancements in the understanding and management of ASD and conducting autism research (Aziz et al. 2006; Elahi et al. 1985; Naqvi 1997; Shafqat and Zaidi 2007; Supe and Burdick 2006; Talati and Pappas 2006; Sood and Adkoli 2000). Medical schools should review and evaluate their curricula periodically, develop effective programs to improve the knowledge and skills of medical professionals regarding autism. This cannot be achieved without evaluating existing training materials and developing a robust curriculum regarding autism and catering them to related clinical and epidemiological health research.
Private and Public Medical Schools
Sixty-three medical institutions in the public and private sector in Pakistan are recognized by the PMDC. Among those, 36 are private and 27 belong to the public sector (Pakistan Medical and Dental Council 2009a). Aga Khan University Medical College (AKU-MC) was established in 1983 as Pakistan’s first private university. AKU aims to maintain international standards in its medical education programs while focusing on health issues relevant to the national health needs. AKU periodically have their educational and research programs reviewed by experts in the US, Canada, other developed countries, and Pakistan. In our study, 93.4% of GPs graduated from public universities and only 6.6% graduated from private universities. Though marginally significant, those who graduated from a private medical school were more likely to self-report knowledge about autism (OR = 2.29; 95% CI: 0.937, 5.63; p-value = 0.06). This difference could be attributed to the lack of significant change over the years in the training at public medical schools despite transformations in disease patterns, new findings in the field, and the health care needs of the community in Pakistan (Aziz et al. 2006; Naqvi 1997). Conversely, the curricula at private universities have been periodically reviewed and updated. Evidence shows graduates from private universities have done better in their professional and board exams in both Pakistan and the US (Gadit et al. 2008).
Continuing Medical Education
Our study revealed that GPs who are younger, graduated in recent years, and have less experience are more likely to report knowledge about autism. Furthermore, among the GPs who reported knowledge about autism, only 12.8% reported symposia or seminars as their source of knowledge about autism. Professional isolation of older GPs might be a contributing factor to their lack of knowledge of autism as they may be cut off from the teaching environment and may not have comparable opportunities to consult with their colleagues (Goulet et al. 2005). Countries like Canada and the UK have mandatory continuing medical education (CME) programs with competency assurance systems aimed at ensuring high quality and acceptable performance in practice to provide lifelong learning for physicians (Duffy and Holmboe 2006; Rauf and Saeed 2007). Continuing educational programs could be helpful in raising awareness about autism in developing countries. This can be achieved by conducting seminars or special courses and workshops throughout the country.
The evidence presented here highlights a lack of infrastructure for autism research in Pakistan. Knowledgeable GPs play an important role in the identification of ASD cases in Pakistan. Since GPs in Pakistan lack sufficient knowledge about ASD, it is imperative that the GPs are trained regarding ASD. This can be achieved through development and delivery of ASD educational material in medical school curricula as well as providing continuing medical education regarding ASD to the practicing physicians including the GPs. There are a limited number of physicians in Pakistan with formal ASD training. Private medical universities such as AKU have faculty with formal training in ASDs and could serve as the training center for ASDs in Pakistan as well as some other countries in the region. The government medical schools can benefit from the private medical schools by promoting collaborations with ASD experts available in the private medical schools. We believe short- and long-term ASD training will potentially lead to increased ASD knowledge among medical graduates as well as practicing GPs, necessarily improving diagnosis, management and research productivity related to autism in the region.
This is the first study regarding ASDs in a South Asian developing country, Pakistan, demonstrating a significant gap in the current state of the knowledge, attitude and practice of GPs in Pakistan regarding ASDs. This gap not only implies systemic problems in the practice and delivery of health care services by GPs in Pakistan, but also suggests that they may not be able to effectively contribute to the creation of domestic knowledge and insight into ASDs in Pakistan through systematic hypothesis driven clinical and epidemiological research. It also suggests that systematic research training programs are needed to establish an evidence-based platform for continued research and practice in the country as it relates to different aspects of ASDs.
Since several developing countries in South Asia follow a similar system of medical education (e.g., India, Pakistan, Bangladesh, Sri Lanka), we believe our study findings may be generalized to other countries in the region. With no information about knowledge and practice of health care providers regarding autism, the research infrastructure for autism will remain underdeveloped in South Asia. We recommend systematic evaluation of knowledge of GPs in these countries as part of an effort to develop research infrastructure for autism in other developing South Asian countries.
Human Subject Review
We obtained IRB approvals from Michigan State University (MSU), Aga Khan University (AKU), and The University of Texas Health Science Center at Houston (UTHSC-H).
Limitations
As described in our sampling strategy it is possible that the sample selected for this study may not represent a random sample from all GPs practicing in Karachi. In addition, the results of our study may have been influenced by sampling bias due to selection of GPs who agreed to participate in this study. Furthermore, this study was based on self-reported knowledge about autism. Several questions in this study (e.g., sources of information) may have been affected by recall bias due to a significant length of time since the graduation of the practitioners.
Conclusions
Our study identifies knowledge deficits concerning autism etiology and diagnosis among GPs practicing in Karachi, Pakistan. The lack of knowledge and unawareness among GPs not only affects the early diagnosis of autism and intervention but also suggests that GPs and other health professionals would not be able to effectively contribute to autism surveillance. Despite differences in knowledge of GPs trained in private medical schools as compared to the public sector in Pakistan, both private and public schools would benefit from developing robust curricula regarding autism, to enable the physicians to effectively contribute to autism research and surveillance.
Continuing medical education and continuing reassessment and certification of medical faculty and health practitioners may help to increase knowledge and improve standard practices of GPs. Specifically, we advocate additional training in ASDs as well as developing a policy to promote healthcare providers’ knowledge of autism and health research in Pakistan in order to ensure early diagnosis and identification of ASD cases to develop an effective autism surveillance program.
Further research will be required to evaluate the knowledge of health professionals regarding autism and the impact of GPs knowledge and attitude on diagnosis and intervention in other developing countries.
References
Ahmed, S., Salih, M., Jafri, W., Ali Shah, H., & Hamid, S. (2009). Helicobacter pylori infection: Approach of primary care physicians in a developing country. BMC Gastroenterology, 9, 23.
Akhtar, T., & Khan, A. J. (2000). Health research capacity in Pakistan (A country report prepared for the WHO and COHRED Regional Consultation on Health Research for Development). Andean and Caribbean Network for Research in Health Policy and Systems. Retrieved March 19, 2010, from: http://www.revmed.unal.edu.co/red/prioridad/health%20research%20resources%20in%20pakistan.pdf.
Ashwell, G. (2009). Autism and Asperger’s syndrome. InnovAiT, 2, 651–656.
Aziz, A., Kazi, A., Jahangeer, A., & Fatmi, Z. (2006). Knowledge and skills in community oriented medical education (COME) self-ratings of medical undergraduates in Karachi. The Journal of the Pakistan Medical Association, 56, 313–317.
Baig, L. A., Akram, D. S., & Ali, S. K. (2006). Development of the community-oriented medical education curriculum of Pakistan: A case report on the national initiative on curriculum development. Education for Health: Change in Learning and Practice, 19, 223–228.
Barbaresi, W. J., Katusic, S. K., & Voigt, R. G. (2006). Autism: A review of the state of the science for pediatric primary health care clinicians. Archives of Pediatrics Adolescent Medicine, 160, 1167–1175.
Centers for Disease Control and Prevention (CDC). (2007). Prevalence of autism spectrum disorders-autism and developmental disabilities monitoring network, 14 sites, United States, 2002. Morbidity and Mortality Weekly Report (MMWR), 56, 12–28.
Committee on Children With Disabilities. (2001). The pediatrician’s role in the diagnosis and management of autistic spectrum disorder in children. Pediatrics, 107, 1221–1226.
Dabas, P., Agarwal, C. M., Kumar, R., Taneja, D. K., Ingle, G. K., & Saha, R. (2005). Knowledge of general public and health professionals about tetanus immunization. Indian Journal of Pediatrics, 72, 1035–1037.
Daley, T. C., & Sigman, M. D. (2002). Diagnostic conceptualization of autism among indian psychiatrists, psychologists, and pediatricians. Journal of Autism and Developmental Disorders, 32, 13–23.
Deo, M. G. (2008). Undergraduate medical students’ research in India. Journal of Postgraduate Medicine, 54, 176–179.
Dobe, M. (1995). Awareness on AIDS among health care professionals. Indian Journal of Public Health, 39, 105–108.
Dodani, S., & LaPorte, R. E. (2008). Ways to strengthen research capacity in developing countries: Effectiveness of a research training workshop in Pakistan. Public Health, 122, 578–587.
Duffy, F. D., & Holmboe, E. S. (2006). Self-assessment in lifelong learning and improving performance in practice: Physician know thyself. JAMA: The Journal of the American Medical Association, 296, 1137–1139.
Elahi, F., Siddiqui, M. G., & Jafarey, N. A. (1985). A retrospective look at the medical curriculum. Journal of the Pakistan Medical Association, 35, 85–92.
Fombonne, E. (2005). Epidemiology of autistic disorder and other pervasive developmental disorders. Journal of Clinical Psychiatry, 66(Suppl 10), 3–8.
Gadit, A. A. (2006). Medical system: Need for appraisal and suggestions. Journal of the College of Physicians and Surgeons, 16, 681.
Gadit, A. A. (2007). Psychiatry in Pakistan: 1947–2006: A new balance sheet. Journal of the Pakistan Medical Association, 57, 453–463.
Gadit, A. A. (2008). Research qualifications in medicine: What is the importance? Journal of the Pakistan Medical Association, 58, 93–94.
Gadit, A. A., Shiwani, M. H., & Abbasi, Y. (2008). Safe medical practice in Pakistan: Are we prepared to adopt a path? Journal of the Pakistan Medical Association, 58, 145–147.
Goulet, F., Jacques, A., & Gagnon, R. (2005). An innovative approach to remedial continuing medical education, 1992–2002. Academic Medicine, 80, 533–540.
Heidgerken, A. D., Geffken, G., Modi, A., & Frakey, L. (2005). A survey of autism knowledge in a health care setting. Journal of Autism and Developmental Disorders, 35, 323–330.
Herzig, H. (2003). Teaching psychiatry in poor countries: Priorities and needs. A description of how mental health is taught to medical students in Malawi, Central Africa. Education for Health (Abingdon.), 16, 32–39.
Hyder, A. A., Akhter, T., & Qayyum, A. (2003). Capacity development for health research in Pakistan: The effects of doctoral training. Health Policy and Planning, 18, 338–343.
Iqbal, I., Pervez, S., & Baig, S. (1997). Management of children with acute respiratory infections (ARI) by general practitioners in Multan—An observational study. Journal of the Pakistan Medical Association, 47, 24–28.
Jawaid, A., Zafar, A. M., Naveed, A., Sheikh, S., Waheed, S., Zafar, M. A., et al. (2008). Knowledge of primary paediatric care providers regarding attention deficit hyperactivity disorder and learning disorder: A study from Pakistan. Singapore Medical Journal, 49, 985–993.
Johnson, C. P., Myers, S. M., & The Council on Children with Disabilities. (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120, 1183–1215.
Kalra, V., Seth, R., & Sapra, S. (2005). Autism—Experiences in a tertiary care hospital. Indian Journal of Pediatrics, 72, 227–230.
Kamat, V. R. (2001). Private practitioners and their role in the resurgence of malaria in Mumbai (Bombay) and Navi Mumbai (New Bombay), India: Serving the affected or aiding an epidemic? Social Science and Medicine, 52, 885–909.
Khan, A. J. (2004). Scope of medical colleges in private sector. Journal of Ayub Medical College, Abbottabad, 16, 1–3.
Khan, H., Khan, S., & Iqbal, A. (2009). Knowledge, attitudes and practices around health research: The perspective of physicians-in-training in Pakistan. BMC Medical Education, 9, 46.
Khan, H., Khawaja, M., Waheed, A., Rauf, M., & Fatmi, Z. (2006). Knowledge and attitudes about health research amongst a group of Pakistani medical students. BMC Medical Education, 6, 54.
Khandwalla, H. E., Luby, S., & Rehman, S. (2006). Knowledge, attitudes and practices regarding sexually transmitted infections among general practitioners and medical specialists in Karachi, Pakistan. Journal of Pakistan Medical Association, 56, S31–S33.
Kochanek, T. T. (1991). The role of the physician in early intervention screening for infants and toddlers. Rhode Island Medical Journal, 74, 275–280.
Konstantareas, M. M., & Hewitt, T. (2001). Autistic disorder and schizophrenia: Diagnostic overlaps. Journal of Autism and Developmental Disorders, 31, 19–28.
Krishnamurthy, V. (2008). A clinical experience of autism in India. Journal of Developmental and Behavioral Pediatrics, 29, 331–333.
Kumar, D., Bajaj, S., & Mehrotra, R. (2006a). Knowledge, attitude and practice of complementary and alternative medicines for diabetes. Public Health, 120, 705–711.
Kumar, R., Taneja, D. K., Dabas, P., & Ingle, G. K. (2006b). Practices and knowledge regarding prevention of tetanus among doctors in Delhi. Asia-Pacific Journal of Public Health, 18, 30–32.
Lian, W. B., Ho, S. K., Yeo, C. L., & Ho, L. Y. (2003). General practitioners’ knowledge on childhood developmental and behavioural disorders. Singapore Medical Journal, 44, 397–403.
Medi Publications: House of Medical Publications. (2006). Mediguide: Comprehensive medical directory (2004–2005) (5th ed.). Karachi, Pakistan: S. M. S. Yunus.
Naqvi, A. S. (1997). Problems of medical education in Pakistan. Journal of Pakistan Medical Association, 47, 267–269.
Pakistan Medical and Dental Council. (2009a). Medical institutions in public & private sector in Pakistan. Pakistan Medical and Dental Council. Retrieved March 19, 2010, from: http://dev.plexushosting.com/PMDC/AboutUs/RecognizedMedicalDentalColleges/tabid/109/Default.aspx.
Pakistan Medical and Dental Council. (2009b). Total number of doctors (M.B.B.S) in Pakistan. Pakistan Medical and Dental Council. Retrieved March 19, 2010, from: http://dev.plexushosting.com/PMDC/Statistics/tabid/103/Default.aspx.
Patwari, A. K., Anand, V., Kumar, H., Aneja, S., & Mullick, D. (1991). Knowledge and perceptions of residents regarding case management of acute diarrhea. Indian Pediatrics, 28, 887–892.
Population Reference Bureau. (2009). 2009 World Population Data Sheet. Population Reference Bureau. Retrieved March 19, 2010, from: http://www.prb.org/pdf09/09wpds_eng.pdf.
Rapin, I. (1997). Autism. The New England Journal of Medicine, 337, 97–104.
Rauf, M. A., & Saeed, A. B. (2007). Competency assurance of general practitioners-role of regulatory authority. Journal of the Pakistan Medical Association, 57, 573–574.
Rhoades, R. A., Scarpa, A., & Salley, B. (2007). The importance of physician knowledge of autism spectrum disorder: Results of a parent survey. BMC Pediatrics, 7, 37.
Rizvi, N., & Hussain, M. (2001). Survey of knowledge about tuberculosis amongst family physicians. Journal of the Pakistan Medical Association, 51, 333–337.
Roy, S. K., Roy, S. K., Bagchi, S., Bajpayee, A., Pal, R., & Biswas, R. (2005). Study of KAP of the private medical practitioners about national disease control programmes. Indian Journal of Public Health, 49, 256–257.
Shafqat, S., & Zaidi, A. K. (2007). Pakistani physicians and the repatriation equation. The New England Journal of Medicine, 356, 442–443.
Shah, S. K., Sadiq, H., Khalil, M., Noor, A., Rasheed, G., Shah, S. M., et al. (2003). Do private doctors follow national guidelines for managing pulmonary tuberculosis in Pakistan? Eastern Mediterranean Health Journal, 9, 776–788.
Shaikh, A. J., Khokhar, N. A., Raza, S., Kumar, S., Haider, G., Haider, A. G., et al. (2008). Knowledge, attitude and practices of non-oncologist physicians regarding cancer and palliative care: A multi-center study from Pakistan. Asian Pacific Journal of Cancer Prevention, 9, 581–584.
Shehzadi, R., Irfan, M., Zohra, T., Khan, J. A., & Hussain, S. F. (2005). Knowledge regarding management of tuberculosis among general practitioners in northern areas of Pakistan. Journal of the Pakistan Medical Association, 55, 174–176.
Singhi, P., & Malhi, P. (2001). Clinical and neurodevelopmental profile of young children with autism. Indian Pediatrics, 38, 384–390.
Sood, R., & Adkoli, B. V. (2000). Medical education in Indiaûproblems and prospects. Journal, Indian Academy of Clinical Medicine, 1, 210–212.
SPSS Inc. (2009). Statistical Package for the Social Sciences (SPSS), Software Statistics 17.0.1 for Windows (Version 17.0.1). SPSS Inc.
Supe, A., & Burdick, W. P. (2006). Challenges and issues in medical education in India. Academic Medicine, 81, 1076–1080.
Talati, J. J., & Pappas, G. (2006). Migration, medical education, and health care: A view from Pakistan. Academic Medicine, 81, S55–S62.
Uddin, M. T., Islam, M. N., & Uddin, M. J. (2008). A survey on knowledge of nutrition of physicians in Bangladesh: Evidence from Sylhet data. South East Asian Journal of Medical Education, 2, 14–17.
Usman, U. (2009). International issues: Neurology training in Pakistan: My experience as a neurology resident. Neurology, 72, e58–e60.
U.S.Census Bureau. (2009). Demographic Indicators International Data Base (IDB) (Pakistan). U.S. Census Bureau. Retrieved May 08, 2009, from: http://www.census.gov/ipc/www/idb/country.php.
Vandan, N., Ali, M., Prasad, R., & Kuroiwa, C. (2008). Physicians’ knowledge regarding the recommended anti-tuberculosis prescribed medication regimen: A cross-sectional survey from Lucknow, India. The Southeast Asian Journal of Tropical Medicine and Public Health, 39, 1072–1075.
Vandan, N., Ali, M., Prasad, R., & Kuroiwa, C. (2009). Assessment of doctors’ knowledge regarding tuberculosis management in Lucknow, India: A public-private sector comparison. Public Health, 123, 484–489.
Volkmar, F. R., Klin, A., & Cohen, D. J. (1997). Diagnosis and classification of autism and related conditions: consensus and issues. In D. J. Cohen & F. R. Volkmar (Eds.), Handbook of autism and pervasive developmental disorders (2nd ed., pp. 5–40). New York: Wiley.
Walton, H., & Gelder, M. (1999). Core curriculum in psychiatry for medical students. Medical Education, 33, 204–211.
Wasay, M. (2003). Neurological care in Pakistan: Actions are needed. Journal of the Pakistan Medical Association, 53, 576.
World Bank. (2008). World Bank’s Data Group. World Bank (Quick Reference Tables). Retrieved March 22, 2010, from: http://web.worldbank.org/WBSITE/EXTERNAL/DATASTATISTICS/0,,contentMDK:20399244~menuPK:1504474~pagePK:64133150~piPK:64133175~theSitePK:239419,00.html.
World Health Organization. (2005). Mental Health Atlas 2005. (revised edition ed.) Geneva, Switzerland. World Health Organization.
World Health Organization. (2009). Mental health in primary care. World Health Organization. Retrieved February 11, 2009, from: http://www.euro.who.int/MENTALHEALTH/TOPICS/20090825_1.
Acknowledgments
We would like to acknowledge the generous support of the Department of Psychiatry at Aga Khan University (AKU) during the data collection period. Specifically, we would like to acknowledge the support provided by Dr. Murad Moosa Khan and Dr. Ehsan Ullah Syed for providing office space and supervising the project coordinator during his stay on the AKU campus. This project could not have been completed without the assistance of our local data collection team Aziez Ahmed, Hassan Bashir, Abdul Latif Bikak, Mediha Iqbal, Muntazir Hussain, Samia Hussain, Faraz Karim, Abdul Shahid Sattar, Nabeel Siddiqui, and Shunaiber Tauhid. We acknowledge partial financial support provided by Epidemiology department and College of Human Medicine at Michigan State University. Also, we acknowledge the support provided by Dr. Manouchehr Ardjomand-Hessabi and Ms. Kari Bloom in the Biostatistics/Epidemiology/Research Design (BERD) Core of the Center for Clinical and Translational Sciences (CCTS) for this project. CCTS is mainly funded by NIH CTSA grant (UL1 RR024148), awarded to the UTHSC-Houston in 2006.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rahbar, M.H., Ibrahim, K. & Assassi, P. Knowledge and Attitude of General Practitioners Regarding Autism in Karachi, Pakistan. J Autism Dev Disord 41, 465–474 (2011). https://doi.org/10.1007/s10803-010-1068-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-010-1068-x