Abstract
Siblings of children with autism have an increased risk for autism spectrum disorders (ASD). As children with autism often exhibit an atypical trajectory of head circumference (HC) growth, HC may be an indicator of vulnerability to autism. This study investigated whether infant siblings of children with ASD (n = 77) with an atypical trajectory of HC growth were more likely than those without an atypical HC trajectory to develop autism symptoms. Results showed that infants who had larger HC at 12 months, and whose HC growth rate decelerated more rapidly between 12 and 24 months were more likely to exhibit autism symptoms than infants with more typical HC trajectories. Among infant siblings of children with autism, atypical HC growth might alert pediatricians to provide screening and/or referral for further evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Head Circumference as an Early Predictor of Autism Symptoms in Younger Siblings of Children with Autism
Autism is a lifelong neurodevelopmental disorder characterized by impaired social interaction and communication, and repetitive and stereotyped behaviors (DSM-IV TR; American Psychiatric Association 2000). Approximately 3–4 males are diagnosed with autism for every female (Scott et al. 2002; Wing 1981; Lord et al. 1982; Baird and August 1985; Volkar et al. 1993).
Although a diagnosis of ASD is not typically given until age 3 years or later in the United States, (Wiggins et al. 2006; Chawarska et al. 2007; De Giacomo and Fombonne 1998), a reliable ASD diagnosis can be rendered in children as young as age 2 (Lord et al. 2006; Cox et al. 1999). Early diagnosis for children with autism is critical, as early intensive behavioral intervention is associated with improved outcomes including higher rates of placement in typical educational settings (Rogers 1998; McEachin et al. 1993; Smith et al. 2000). Early age of intervention is considered an important factor in optimal outcomes (Harris and Handleman 2000; McGee et al. 1999).
Most parents of children with autism report that they had concerns by the time their child was 18 months of age (Wiggins et al. 2006; De Giacomo and Fombonne 1998). One study reported that parental concerns typically begin when their infant is 14–15 months of age (Chawarska et al. 2007). Symptoms of autism can be identified as early as 8–12 months of age. Communication impairments are one of the earliest indicators of ASD (Woods and Wetherby 2003) and at 12 months of age may include lack of pointing, orienting to name, showing objects, looking at faces of others, and gaze monitoring. Home videotape studies indicate that infants later diagnosed with autism can be distinguished from children with mental retardation or typical development by 12 months by how often they attend to people, orient to their names, smile at others, vocalize, seek physical contact, and engage in joint attention (Maestro et al. 2002; Osterling et al. 2002). Failure to respond to name distinguishes infants later diagnosed with autism from typically developing infants as young as 8–10 months (Werner et al. 2005; Baranek 1999; Osterling and Dawson 1994). By age two clear impairments in language development and social communication are evident including difficulties in making complex and single word vocalizations and sharing attention (Mars et al. 1998; Maestro et al. 2001; Werner and Dawson 2005).
Autism is highly heritable disorder and, as such, siblings of children with autism have a risk of developing autism of 2.8–7% (August et al. 1981; Bailey et al. 1996; Smalley et al. 1988; Veenstra-Vanderwheele and Cook 2003), while the general population has approximately a 0.6% prevalence of ASD (Fombonne 2005). Delays in language, social impairment and use of gestures are also present in siblings of children with autism, even in siblings who do not have an autism diagnosis (Piven et al. 1990; Toth et al. 2007; Mitchell et al. 2006; Cassel et al. 2007). As many as 30% of siblings of children with autism score below average on measures of IQ and language (Toth et al. 2007; Gamliel et al. 2007), although one study found the cognitive delays to be limited to the toddler and preschool period (Gamliel et al. 2007). Given this increased risk of an autism diagnosis and related autism symptoms, early detection and screening are important for siblings of children with autism. Despite this, siblings are not typically screened for autism as part of standard practice health care.
Bristol-Power and Spinella (1999) have stressed the need for routine developmental screening specifically for autism as part of well-child care. The Modified Checklist for Autism in Toddlers (M-CHAT) was developed as a 23-item parent report measure that assesses autism symptoms and can be administered easily by pediatricians. In the initial analysis six of the items were the best discriminators between children who did and did not develop autism; these were labeled critical items. In an initial study, 1,293 children were screened using the M-CHAT, of whom 58 were evaluated and 39 met criteria for an ASD (Robins et al. 2001). Adequate sensitivity and specificity have been reported for this measure. An early screening tool such as the M-CHAT is critical to ensuring each child with autism is diagnosed as soon as possible, not only to increase the probability that children receive intervention, but because a delay in diagnosis causes additional distress to parents (Robins et al. 2001).
Head Circumference
Macroencephaly in autism was first noted by Kanner (1943), the first person to describe the disorder. Recent studies indicate that autism is associated with enlarged total cerebral volume, abnormal electroencephalograms, increased white matter, and decreased gray matter (Mouridsen et al. 2000; Courchesne et al. 2003). Abnormalities in the medial temporal lobe, cerebellum, and amygdala have been observed (Sparks et al. 2002).
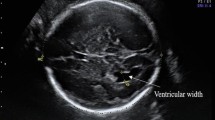
Head circumference in children younger than age 6 is a good index of total brain volume (r = 0.93; Bartholomeusz et al. 2002). Head circumference in children with autism is often smaller than normal or normal at birth (Courchesne et al. 2001, 2003; Dawson et al. 2007), yet increases faster than normal at around 4 months of age (Courchesne and Pierce 2005; Redcay and Courchesne 2005; Gilberg and de Souza 2002). Approximately 60% of children with autism show this atypical trajectory to an extreme degree, while only 6% of typically developing children show this atypical trajectory (Courchesne et al. 2003). As noted in a study by Courchesne et al. (2003), at ages 2–4 years, 90% of boys with autism had larger than normal brain volumes, and 37% met criteria for developmental macroencephaly (measurement above 97th percentile). The trajectory appeared to be early overgrowth followed by abnormally slow growth (Courchesne et al. 2001). Fidler et al. (2000) found an increased prevalence of macroencephaly not only in children with autism, but in their first-degree relatives. In a longitudinal study of head growth in autism, Dawson and colleagues (2007) found that accelerations in head growth appear to occur between 6–12 months, but that after 12 months, the rate of head growth decelerates and is not significantly different from normal rates of head growth. Thus, children with autism may be characterized by small or normal head size at birth, rapid growth in the first year, followed by a deceleration in rate of HC growth, reaching normal rates during the toddler years.
Some studies have examined whether atypical HC growth is associated with specific autism symptoms. Deutsch and Joseph (2003) examined associations between HC and language ability, IQ, and executive function in a sample of children with ASD. Head circumference was measured at one discrete time point between 4 and 14 years of age; the only significant association was between HC and discrepancies between verbal and nonverbal IQ. Courchesne et al. (2003) found that smaller head circumference at birth was associated with worse verbal scores among children who had functional language, while HC increase during infancy was associated with worse scores on a repetitive behavior scale. Fidler et al. (2000) also found an association between macroencephaly and stereotyped behavior, but did not find any other symptom associations. In contrast to these findings Mraz et al. (2007) sample showed a relation between HC and symptoms related to social impairment. More research is needed to clarify the relationship between specific symptom domains and HC growth trajectories in autism.
The present study represents a unique contribution to the literature by examining early patterns of HC trajectory in very young siblings of children with autism in relation to autism symptoms evident in toddlerhood. We investigated two specific hypotheses. First, in an independent sample of infants at risk for autism, we sought to replicate the Dawson et al. (2007) finding that among infants who were later diagnosed with autism, an atypical acceleration in HC trajectory growth during the first year is followed by a deceleration by 12–24 months such that rates of HC growth during toddlerhood do not differ from normal rates. Second, we tested the hypothesis that in a sample of infants at risk for autism, infant siblings who exhibited an atypical trajectory of HC growth during the infant–toddler period would be more likely to develop autism symptoms by toddlerhood. If this hypothesis is supported, pediatricians and other health professionals following infant siblings could then use HC data regularly collected at well-baby check-ups as an early warning sign of risk for autism. Children thus identified as at-risk could be closely monitored and later referred for diagnostic and early intervention services if appropriate, potentially decreasing the average age of diagnosis by a year or more.
Methods
Participants
Participants were 77 younger siblings of children with ASD. The younger siblings initially entered into the study at 18–24 months of age. Participants were recruited from the Center on Human Development and Disability, the UW Autism Center, local public health agencies, pediatric offices, and Birth-to-Three Centers. Children born premature were excluded from the sample.
Instruments
The Modified Checklist for Autism in Toddlers (M-CHAT)
The M-CHAT, which consists of 23 yes/no items assessing early symptoms of autism, is a reliable measure designed to detect children at risk for autism/PDD by 18 months of age. Children pass or fail the M-CHAT based on the number of symptoms endorsed by their parent indicating whether they are at risk for autism. The M-CHAT yields a total item score and a critical item score (critical items are those found to be the best discriminators of autism versus no autism in the initial study). Internal reliability for the entire checklist (α = 0.85) and for the critical items (α = 0.83) is adequate. Sensitivity has been found to be 0.87 and specificity has been found to be 0.99 (Robins et al. 2001).
Early Developmental Interview (EDI)
The EDI is a retrospective parent interview that assesses symptoms across four domains in the first 2 years of a child’s development. Parents are asked to report on their infant’s social responsiveness, language and communication skills, sensory-motor behaviors, and regulatory behaviors at 3-month time points from birth to 2 years of age. Children with autism, developmental delay, and typical development significantly differ on the EDI beginning at 12–15 months (Werner et al. 2005).
Records Review
Developmental and diagnostic evaluation records were requested for the older sibling in order to confirm a diagnosis of ASD. All older siblings were given a diagnosis of autism, PDD, or Asperger’s by a psychologist, neurologist, or developmental pediatrician based on DSM criteria.
Medical records and well-baby records for the younger sibling were requested and used to derive HC measurements taken at well-baby check-ups by the infant’s pediatrician. Measurements were extracted for each time point available during the first 2 years, with a minimum of four HC data points necessary for inclusion in the sample. Each measurement was independently entered into the database by two different research assistants and a third researcher resolved any discrepancies in the data.
Procedure
Parents who agreed to participate completed the M-CHAT when the younger sibling was 18–24 months old. If the child failed the M-CHAT, the parent was called by a clinician and asked specific follow-up questions for items endorsed (Robins et al. 2001). A phone interview was conducted with parents to collect data using the EDI when the younger sibling was 2–4 years old. Release of information forms were obtained to request medical records of well-baby check-ups for each participating child.
Data Analyses
Head circumference measurements were converted to z-scores for the child’s age based on the most recent Center for Disease Control reference data (2002) developed by the National Center for Health Statistics. Multilevel modeling analyses, conducted using the Hierarchical Linear Modeling software package (HLM; Bryck and Raudenbush 2002) were used to determine the association between infant–toddler patterns of HC trajectories and behavioral symptoms of autism at 18–24 months as assessed by the M-CHAT, and between 22 and 24 months as measured by the EDI. The growth trajectories of HC for each child were modeled with three parameters: a slope for HC between 0 and 12 months, the slope for HC between 12 and 24 months and the Level 1 intercept for the model which was placed at 12 months. Thus, each child’s HC measurements were repeated as the rate of change from 0 to 12 (slope), absolute level at 12 months (intercept), and rate of change from 12 to 24 months (slope). Symptom measures and sex were entered at Level 2 when examined. Controlling the HC measurements for height did not change the pattern of results, so height was not included in the reported analyses. Data were available on HC and M-CHAT scores for 77 children and on all measures for 71 children.
Results
Overall Sample
Early Developmental Interview communication scores at 22–24 months had a mean raw score of 1.49 (SD = 2.16) and EDI social scores at 22–24 months had a mean of 1.65 (SD = 2.73). The mean M-CHAT critical items score was 0.82 (SD = 1.40) and 29.9% of subjects failed the M-CHAT. The average age at administration was 33 months for the EDI and 20 months for the M-CHAT.
Head circumference values at 12 months of age (Level 1 intercept term) were significantly higher than CDC norms in this high risk sample. One-sample, two-tailed t-tests were run on the z-scores at intercepts 6, 8, 10, and 12 months. The z-scores at each time point were significantly greater than zero (HC was significantly greater than the average), and the mean z-score increased with age. The minimum z-score was 0.45 and the minimum t was 4.49 (p < 0.05).
Head circumference z-scores increased at a rate of .078 z-score points per month between 0 and 12 months of age, a slope that was significantly higher than the CDC normative data, t(76) = 8.57, p < 0.001). Between 12 and 24 months, however, the slope or rate of growth in HC for the at-risk sample as a whole was compared to CDC norms using a one-sample t-test and was not found to be significantly different, t (76) = 0.46, p = 0.650; see Table 1.
Sex Differences
Since autism affects more boys than girls, further analyses were conducted to determine if HC patterns were different for boys versus girls. The rate of change in HC from 12 to 24 months (coeff. = 0.04, p = 0.02) and intercept at 12 months (coeff. = −0.55, p = 0.03) were significantly different for boys versus girls, even when taking into account the differing HC norms for boys and girls when converting into z-scores (Table 2, Fig. 1). Head circumference growth for boys increased more rapidly until 12 months, and then leveled off more steeply than for girls.
Independent samples t-tests were performed to examine levels of communication symptoms, t(df) = 1.886, p = 0.064, and social symptoms, t(df) = 2.130, p = 0.037 on the EDI and the M-CHAT critical items score, t(df) = 1.789, p = 0.079 for boys versus girls. The only significant difference was in social symptoms between 22 and 24 months on the EDI, with boys exhibiting more symptoms than girls. However, when the rate of change for HC was re-examined after controlling for M-CHAT critical items, trajectories for boys versus girls were no longer significantly different. Between 0 and 12 months there was a significant M-CHAT pass/fail by sex interaction for slope such that girls who failed the M-CHAT had a lower intercept at birth and a slope that increased much more rapidly (coeff. = −0.03, p = 0.07). The HLM analysis was rerun including only the significant findings (Table 3).
Head Circumference Association with Symptoms
Head circumference slopes and intercepts were significantly associated with EDI social symptoms and communication symptoms at 22–24 months, and M-CHAT critical item scores (critical items on the M-CHAT are largely made up of social and communication symptoms). The rate of change between 12 and 24 months (coeff. = −0.01, p = 0.048) was associated with social symptoms on the EDI at 22–24 months. The slope of HC between 12 and 24 months leveled off more steeply for children exhibiting more social symptoms (Table 4, Fig. 2). Figure 2 illustrates the change in HC z scores over time. To illustrate this and in subsequent figures we chose three high frequency scores. EDI communication symptoms at 22–24 months showed significant differences at the 12 month intercept (coeff. = 0.13, p = 0.04) and at the slope between 12 and 24 months (coeff. = −0.01, p = 0.01). Children with higher levels of communication symptoms had a larger HC at 12 months and a slope that leveled off more rapidly between 12 and 24 months (Table 5, Fig. 3).
The intercept at 12 months was significantly different for children with differing numbers of M-CHAT critical item totals (coeff. = 0.19, p = 0.02). Children with more critical symptoms on the M-CHAT had a larger HC at 12 months (Table 6). To illustrate the relationship between M-CHAT and slope of HC, see Fig. 4 which plots that relationship at three different levels of M-CHAT scores as an illustrative example.
Discussion
We replicated the finding of Dawson et al. (2007) that autism or autism symptoms are associated with an increased acceleration of HC growth from 6 to 12 months, followed by a deceleration of HC growth from 12 to 24 months such that rates of HC during toddlerhood are not different from the general population. Furthermore, results of this study supported the hypothesis that atypical HC growth trajectories may serve as an indicator of vulnerability for the development of autism symptoms. Infant siblings who exhibited larger HC at 12 months and showed a greater deceleration of HC growth from 12 to 24 months were more likely to exhibit autism symptoms by toddlerhood. This was true with respect to the development of social and communication symptoms, but not repetitive behaviors. This may be because the children in this sample were very young, and repetitive behaviors are not often evident until children become older (Lord 1995).
Infant siblings who were male were more likely to show atypical HC trajectories than were female infant siblings, even after accounting for sex differences in normative HC growth. This difference in HC trajectories may be because boys have a higher risk of developing autism than girls, and therefore may exhibit more symptoms (Wing 1981; Lord et al. 1982; Baird and August 1985). However, the results of this study may not be fully explained by the higher risk of autism in boys given that symptom levels in this sample were essentially the same for boys versus girls.
There are several limitations that should be considered when interpreting the results of this study. Parents who were interested in participating in the study may be more likely to be concerned about their child’s development than parents not interested in the study; therefore an ascertainment bias is possibly present in our sample. The results of this study may not be representative of the entire population of younger siblings with children with autism. Also, the younger siblings did not undergo diagnostic evaluations as part of this study. Despite these limitations, there was a variety of symptom levels present in the younger siblings and those symptoms were associated with atypical head circumference trajectories.
Siblings deemed at-risk on the M-CHAT were more likely to show more rapid HC growth from birth to 12-months and a more rapid decline in rate of HC growth from 12 to 24 months. If these findings are replicated with prospective data, siblings of children with autism who are at risk for autism might be detected at earlier ages than is currently possible. Infant siblings who regularly see a pediatrician might be screened for HC at well-baby check-ups with their pediatrician and, if an atypical pattern of HC is found, subsequent screening with the M-CHAT or other appropriate early autism screening tools would allow for an earlier referral for diagnosis and treatment, if needed. This potentially could decrease the average age of diagnosis of autism by a year or more by using a practical and low cost procedure with data that are widely available and routinely used in regular visits to pediatricians. With such screening methods, it is hoped that more children with autism will be detected and referred for more extensive evaluation at a very early age, ultimately leading to earlier intervention and improved outcomes for children with autism.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders, fourth edition, text revision. Washington, DC: American Psychiatric Association.
August, G. J., Stewart, M. A., & Tsai, L. (1981). The incidence of cognitive disabilities in the siblings of autistic children. British Journal of Psychiatry, 138, 416–422.
Bailey, A., Phillips, W., & Rutter, M. (1996). Autism: Towards an integration of clinical, genetic, neuropsychological and neurobiological perspectives. Journal of Child Psychology & Psychiatry, 37, 89–126.
Baird, T. D., & August, G. J. (1985). Familial heterogeneity in infantile autism. Journal of Autism and Developmental Disorders, 15, 315–322.
Baranek, G. T. (1999). Autism during infancy: A retrospective video analysis of sensory-motor and social behaviors at 9–12 months of age. Journal of Autism and Developmental Disorders, 29, 213–224.
Barthlomeusz, H. H., Courchesne, E., & Karns, C. M. (2002). Relationship between head circumference and brain volume in healthy normal toddlers, children, and adults. Neuropediatrics, 33, 239–241.
Bristol-Power, M. M., & Spinella, G. (1999). Research on screening and diagnosis in autism: A work in progress. Journal of Autism and Developmental Disorders, 29, 435–438.
Byrk, A. S., & Raudenbush, S. W. (2002). Hierarchical linear models: Applications and data analysis methods. Thousand Oaks: Sage.
Cassel, T. D., Messinger, D. S., Ibanez, L. V., Haltigan, J. D., Acosta, S. I., & Buchman, A. C. (2007). Early social and emotional communication in the infant siblings of child with autism spectrum disorders: An examination of the broad phenotype. Journal of Autism and Developmental Disorders, 37, 122–132.
Chawarska, K., Paul, R., Klin, A., Hannigen, S., Dichtel, L. E., & Volkmar, F. (2007). Parental recognition of developmental problems in toddlers with autism spectrum disorders. Journal of Autism and Developmental Disorders, 37, 62–72.
Courchesne, E., Carper, R., & Akshoomoff, N. (2003). Evidence of brain overgrowth in the first year of life in autism. Journal of the American Medical Association, 290, 337–344.
Courchesne, E., Karns, C. M., Davis, H. R., Ziccardi, R., Carper, R. A., Tigue, Z. D., Chisum, H. J., Moses, P., Pierce, K., Lord, C., Lincoln, A. J., Pizzo, S., Schreibman, L., Haas, R. H., Akshoomoff, N. A., & Couchesne, R. Y. (2001). Unusual brain growth patterns in early life in patients with autistic disorder an MRI study. Neurology, 57, 245–254.
Courchesne, E., & Pierce, K. (2005). Brain overgrowth in autism during a critical time in development: Implications for frontal pyramidal neuron and interneuron development and connectivity. International Journal of Developmental Neuroscience, 23, 153–170.
Cox, A., Charman, T., Baron-Cohen, S., Drew, A., Klein, K., Baird, G., Swettenham, J., & Wheelwright, S. (1999). Autism spectrum disorders and 20 and 42 months of age: Stability of clinical and ADI-R diagnosis. Journal of Child Psychology and Psychiatry, 40, 719–732.
Dawson, G., Munson, J., Webb, S. J., Nalty, T., Abbott, R., & Toth, K. (2007). Rate of head growth decelerates and symptoms worsen in the second year of life in autism. Biological Psychiatry, 15, 458–464.
De Giacomo, A., & Fombonne, E. (1998). Parental recognition of developmental abnormalities in autism. European Child & Adolescent Psychiatry, 7, 131–136.
Deutsch, C. K., & Joseph, R. M. (2003). Brief report: Cognitive correlates of enlarged head circumference in children with autism. Journal of Autism and Developmental Disorders, 33, 209–215.
Fidler, D. J., Bailey, J. N., & Smalley, S. L. (2000). Macroencephaly in autism and other pervasive developmental disorders. Developmental Medicine & Child Neurology, 42, 737–740.
Fombonne, E. (2005). The changing epidemiology of autism. Journal of Applied Research in Intellectual Disabilities, 18, 281–294.
Gamliel, I., Yirmiya, N., & Sigman, M. (2007). The development of young siblings of children with autism from 4 to 54 months. Journal of Autism and Developmental Disorders, 37, 171–183.
Gillberg, C., & de Souza, L. (2002). Head circumference in autism, Asperger syndrome, and ADHD: A comparative study. Developmental Medicine and Child Neurology, 44, 296–300.
Harris, S. L., & Handleman, J. S. (2000). Age and IQ at intake as predictors of placement for young children with autism: A four- to six-year follow-up. Journal of Autism and Developmental Disorders, 21, 281–290.
Kanner, L. (1943). Autistic disturbances of affective contact. Nervous Child, 2, 217–250.
Lord, C. (1995). Follow-up of two year-olds referred for possible autism. Journal of Child Psychology and Psychiatry, 36, 1365–1382.
Lord, C., Risi, S., DiLavore, P. S., Shulman, C., Thurm, A., & Pickles, A. (2006). Autism from 2 to 9 years of age. Archives of General Psychiatry, 63, 694–701.
Lord, C., Schopler, E., & Revicki, D. (1982). Sex differences in autism. Journal of Autism and Developmental Disorders, 12, 317–330.
Maestro, S., Muratori, F., Barbieri, F., Casella, C., Cattaneo, V., Cavallaro, M. C., Cesari, A., Milone, A., Rizzo, L., Viglione, V., Stern, D. D., & Palacio-Espasa, F. (2001). Early behavioral development in autistic children: The first 2 years of life through home movies. Psychopathology, 34, 147–152.
Maestro, S., Muratori, F., Cavallaro, M. C., Pei, F., Stern, D., Golse, B., et al. (2002). Attentional skills during the first 6 months of age in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 1239–1245.
Mars, A. E., Mauk, J. E., & Dowrick, P. W. (1998). Symptoms of pervasive developmental disorders as observed in prediagnostic home videos of infants and toddlers. Journal of Pediatrics, 132, 500–504.
McEachin, J. J., Smith, T., & Lovaas, O. I. (1993). Long-term outcome for children with autism who received early intensive behavioral treatment. American Journal on Mental Retardation, 97, 359–372.
McGee, G. G., Morrier, M., & Daly, T. (1999). An incidental teaching approach to early intervention for toddlers with autism. Journal of the Association for Persons with Severe Handicaps, 24, 133–146.
Mitchell, S., Brian, J., Zwaigenbaum, L., Roberts, W., Szatmari, P., Smith, I., & Bryson, S. (2006). Early language and communication development of infants later diagnosed with autism spectrum disorder. Developmental and Behavioral Pediatrics, 27, S69–S78.
Mouridsen, S. E., Rich, B., & Isager, T. (2000). A comparative study of genetic and neurobiological findings in disintegrative psychosis and infantile autism. Psychiatry and Clinical Neurosciences, 54, 441–446.
Mraz, K. D., Green, J., Dumont-Mathieu, T., Makin, S., & Fein, D. (2007). Correlates of head circumference growth in infants later diagnosed with autism spectrum disorders. Journal of Child Neurology, 22, 700–713.
National Center for Health Statistics Center for Disease Control. (2002). Clinical growth charts. National Health and Nutrition Examination Survey [On-line]. Available: http://www.cdc.gov/nchs/about/major/nhanes/growtOFCharts/clinical_charts.htm.
Osterling, J., & Dawson, G. (1994). Early recognition of children with autism: A study of first birthday home video tapes. Journal of Autism and Developmental Disorders, 24, 247–257.
Osterling, J. A., Dawson, G., & Munson, J. A. (2002). Early recognition of 1-year-old infants with autism spectrum disorder versus mental retardation. Development and Psychopathology, 14, 239–251.
Piven, J., Gayle, J., Chase, G. A., Fink, B., Landa, R., Wzorek, M. M., et al. (1990). A family history study of neuropsychiatric disorders in the adult siblings of autistic individuals. Journal of the American Academy of Child and Adolescent Psychiatry, 29, 177–183.
Redcay, E., & Courchesne, E. (2005). When is the brain enlarged in autism? A meta-analysis of all brain size reports. Biological Psychiatry, 58, 1–9.
Robins, D. L., Fein, D., Barton, M. L., & Green, J. A. (2001). The modified checklist for autism in toddlers: An initial study investigating the early detection of autism and pervasive developmental disorders. Journal of Autism and Developmental Disorders, 31, 131–144.
Rogers, S. J. (1998). Empirically supported comprehensive treatments for young children with autism. Journal of Clinical Child Psychology, 27, 168–179.
Scott, F. J., Baron-Cohen, S., Bolton, P., & Brayne, C. (2002). Brief report: Prevalence of autism spectrum conditions in children aged 5–11 years in Cambridgeshire, UK. Autism, 6, 231–237.
Smalley, S. L., Asarnow, R. F., & Spence, A. (1988). Autism and genetics. Archives of General Psychiatry, 30, 405–416.
Smith, T., Groen, A. D., & Wynn, J. W. (2000). Randomized trial of intensive early intervention for children with pervasive developmental disorder. American Journal on Mental Retardation, 105, 269–285.
Sparks, B. G., Friedman, S. D., Shaw, D. W., Aylward, E. H., Echelard, D., Artru, A. A., et al. (2002). Brain structural abnormalities in young children with autism spectrum disorder. Neurology, 59, 184–192.
Toth, K., Dawson, G., Meltzoff, A. N., Greenson, J., & Fein, D. (2007). Early social, imitation, play, and language abilities of young non-autistic siblings of children with autism. Journal of Autism and Developmental Disorders, 37, 145–157.
Veenstra-Vanderweele, J., & Cook, E. H. Jr. (2003). Genetics of childhood disorders: XLVI. Autism, part 5: Genetics of autism. Development and Neurobiology, 42, 116–118.
Volkar, F. R., Szatmari, P., & Sparrow, S. S. (1993). Sex differences in pervasive developmental disorders. Journal of Autism and Developmental Disorders, 4, 579–591.
Werner, E., & Dawson, G. (2005). Validation of the phenomenon of autistic regression using home videotapes. Archives of General Psychiatry, 62, 889–895.
Werner, E., Dawson, G., Munson, J., & Osterling, J. (2005). Variation in early developmental course in autism and its relation with behavioral outcome at 3–4 years of age. Journal of Autism & Developmental Disorders, 35, 337–350.
Wiggins, L. D., Baio, J., & Rice, C. (2006). Examination of the time between first evaluation and first autism spectrum diagnosis in a population-based sample. Journal of Developmental & Behavioral Pediatrics, 27, S79–S87.
Wing, L. (1981). Sex ratios in early childhood autism and related conditions. Psychiatric Research, 5, 129–137.
Woods, J. J., & Wetherby, A. M. (2003). Early identification of and intervention for infants and toddlers who are at risk for autism spectrum disorder. Language, Speech, and Hearing Services and Schools, 34, 180–193.
Acknowledgments
We wish to thank the children and parents who participated in this study. This research was funded by grants from the National Institute of Child Health and Human Development (U19HD34565, P50HD066782, and R01HD-55741) and the National Institute of Mental Health (U54MH066399; R01HD039961).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elder, L.M., Dawson, G., Toth, K. et al. Head Circumference as an Early Predictor of Autism Symptoms in Younger Siblings of Children with Autism Spectrum Disorder. J Autism Dev Disord 38, 1104–1111 (2008). https://doi.org/10.1007/s10803-007-0495-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-007-0495-9