Abstract
This study examined whether girls and boys with ADHD show similar impairments in cognitive control from childhood into adolescence and the developmental relationship between cognitive control and ADHD symptoms. Participants include 8–17-year-old children with ADHD (n = 353, 104 girls) and typically developing (TD) controls (n = 241, 86 girls) with longitudinal data obtained from n = 137. Participants completed two go/no-go (GNG) tasks that varied in working memory demand. Linear mixed-effects models were applied to compare age-related changes in cognitive control for each GNG task among girls and boys with ADHD and TD controls and in relation to ADHD symptoms. Boys with ADHD showed impaired response inhibition and increased response variability across tasks. In contrast, girls with ADHD showed impaired response inhibition only with greater working memory demands whereas they displayed increased response variability regardless of working memory demands. Analysis of age-related change revealed that deficits in cognitive control under minimal working memory demands increase with age among girls with ADHD and decrease with age among boys with ADHD. In contrast, deficits in cognitive control with greater working memory demands decrease with age among both boys and girls with ADHD compared to TD peers. Among children with ADHD poor response inhibition during childhood predicted inattentive symptoms in adolescence and was associated with less age-related improvement in inattentive symptoms. These findings suggest that girls and boys with ADHD show differential impairment in cognitive control across development and response inhibition in childhood may be an important predictor of ADHD symptoms in adolescence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Attention-deficit/hyperactivity disorder (ADHD) is a highly prevalent neurodevelopmental disorder affecting 5–10% of children and adolescents worldwide, and is characterized by developmentally inappropriate levels of inattention, hyperactivity, and impulsivity (Polanczyk et al., 2014). Neuropsychological models of ADHD posit that deficits in cognitive control, including response inhibition/variability and working memory, underlie the symptoms of ADHD (Barkley, 1997; Nigg, 2005; Willcutt et al., 2005). Cognitive control has been defined in many ways, including the Research Domain Criteria (RDoC) definition of “a system that modulates the operation of other cognitive and emotional systems, in the service of goal-directed behavior, when prepotent modes of responding are not adequate to meet the demands of the current context” and those summarized by Nigg (2017) including “the ability to flexibly adjust behavior in the context of dynamically changing goals and task demands” (Carter & Krus, 2012, p. 89). The current study focuses on response inhibition, variability, and the impact of working memory on these processes as aspects of cognitive control that are strongly implicated in ADHD, with a recent meta-analyses showing the largest group difference effect sizes for working memory (0.54), response variability (0.53), and response inhibition (0.52) (Pievsky & McGrath, 2018). Considerable research on neuropsychological correlates of ADHD has provided evidence of response control deficits in ADHD, with studies reporting slower stop-signal reaction times (Dimoska et al., 2003; Senderecka et al., 2012), higher commission error rates (i.e., failure to inhibit a response to a stimulus) (Nigg, 1999; Pennington & Ozonoff, 1996; Willcutt et al., 2005) and greater response variability (i.e., trial-to-trial differences in response speed) (Epstein et al., 2011; Kofler et al., 2013; Lijffijt et al., 2005; Seymour et al., 2016; Rosch et al., 2013). Working memory deficits have also been implicated in ADHD (Kofler et al., 2019) and have been shown to predict poor social and family functioning and low academic achievement (Kofler et al., 2017).
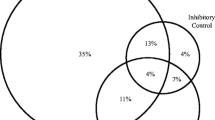
A growing literature has demonstrated substantial heterogeneity in cognitive control deficits in children with ADHD, with 30–50% of children demonstrating a deficit in a single domain (Kofler et al., 2019; Nigg, 2005; Willcutt et al., 2005). Consideration of multiple cognitive processes has been shown to better classify children with ADHD (Willcutt et al., 2005) and predict symptom persistence and remittance (Karalunas et al., 2017). Additionally, there is some evidence that children with ADHD perform worse during tasks involving differing cognitive control processes, with prior research demonstrating greater impairment in response inhibition and increased response variability in children with ADHD under conditions with greater working memory demands (Seymour et al., 2016; Vaurio et al., 2009). Despite the well-established heterogeneity in cognitive deficits in ADHD, there is a lack of research on whether and how individual differences in cognitive control impairments relate to clinical symptoms in children with ADHD (c.f., Biederman et al., 2009; Gordon & Hinshaw, 2020; Karalunas et al., 2017) which are also shown to be heterogeneous (c.f., Luo et al., 2019).
The clinical presentation and outcomes of children with ADHD also varies between individuals (Hechtman et al., 2016; Klein et al., 2012) with evidence of sex differences in functional outcomes. Specifically, girls with ADHD are more likely to have comorbid anxiety and depression, while boys with ADHD are more likely to present with disruptive behavioral disorders (e.g., Oppositional Defiant and Conduct Disorders) (Abikoff et al., 2002; Biederman et al., 2006, 2008; Gershon, 2002; Lahey et al., 2007; Rasmussen & Levander, 2009). Additionally, girls with ADHD demonstrate increased levels of self-harm behaviors and suicidal ideation, lower levels of self-esteem, and poorer coping skills compared to boys with ADHD (Rucklidge & Tannock, 2001). Furthermore, these affective symptoms and behaviors may contribute to why females with ADHD are twice as likely as males to be psychiatrically hospitalized in adulthood (Dalsgaard et al., 2002). Given the potential deleterious outcomes for children with ADHD, it is important to consider how heterogeneity in cognitive deficits relates to ADHD symptoms.
Despite this evidence for sex differences in functional outcomes in children with ADHD, there is a lack of research on sex differences in neurocognitive deficits that may contribute to these behavioral outcomes. One study using a subset of the current sample found evidence that boys, but not girls, with ADHD exhibit increased intrasubject variability and more inhibitory (commission) errors during a Go/No-Go (GNG) task with minimal working memory demands. In contrast, when given a complex GNG task with greater working memory demand, both boys and girls with ADHD exhibit higher error rates and intrasubject variability compared to their sex-matched controls (Seymour et al., 2016). Another study with adolescents, ages 13 to 17 years, showed that boys with ADHD showed greater intrasubject variability compared to girls with ADHD, suggesting that ADHD-related sex differences are also observed in adolescence (Rucklidge, 2006). However, most studies of cognitive deficits in the ADHD literature either exclusively include boys or include too few girls to reliably test for sex differences.
In addition to the lack of research bridging neurocognitive deficits and clinical symptoms and outcomes on ADHD, it also remains unclear whether and how the relationship between neurocognitive deficits and ADHD symptoms change over the course of development. Studies have shown that ADHD-associated impairments in inhibitory control and verbal working memory persist beyond adolescence and into young adulthood (Gordon & Hinshaw, 2020; Miller & Hinshaw, 2010). While ADHD symptoms and impairments are hypothesized to be the result of cognitive control deficits (e.g., Brown, 2013), few longitudinal studies have examined the development of cognitive control in children with ADHD and its relationship with ADHD symptoms (c.f., Karalunas et al., 2017). Most longitudinal studies have investigated the development of ADHD symptoms and cognitive control separately, highlighting the need for translational research bridging these literatures.
With regard to the development of cognitive control processes, longitudinal studies report children with ADHD show linear improvements over time from childhood to emerging adulthood, characterized by improvements in response inhibition (decreased commission error rates) and working memory (increased digit span), before plateauing in emerging adulthood; however, when compared to their TD peers, children with ADHD continuously lag behind (Biederman et al., 2007, 2009; Gordon & Hinshaw, 2020; Skogli et al., 2014; van Lieshout et al., 2013, 2019). While several studies have examined developmental changes in ADHD-associated impairments in cognitive control, there is very limited examination of the impact of sex on these findings.
In contrast, clinical and community samples using self-, parent-, and teacher-reports have uncovered sex-related differences in ADHD symptom trajectories, such that boys with ADHD are more likely to show large symptom increases around age 7, while girls are more likely to show large symptom increases around pre-adolescence (Malone et al., 2010; Murray et al., 2018), and girls with ADHD are less likely to demonstrate hyperactive/impulsive symptoms compared to their male counterparts (Biederman et al., 2002; Newcorn et al., 2001). To our knowledge, only two studies examined heterogeneity in development of cognitive control processes in relation to longitudinal symptom change (Gordon & Hinshaw, 2020; Karalunas et al., 2017), reporting that developmental change in response inhibition, working memory, and global executive function (as measured by the Rey-Osterrieth Complex Figure Test) was unrelated to ADHD symptom change while individual differences in the rate of visual-spatial working memory improvement predicted ADHD symptom remission in ADHD. This study did not report any evidence of the impact of sex on developmental associations between cognitive control processes and symptom severity. Therefore, further research is necessary to understand how changes in cognitive control process, including response inhibition/variability and working memory, relate to inattentive and hyperactive/impulsive symptoms over development and how this relationship may differ between boys and girls with ADHD.
Current Study
The goal of this study is to extend the existing literature and to inform future developmental research through examination of age-related changes in cognitive control across childhood and adolescence using a combination of cross-sectional and longitudinal data. In particular, the analyses presented here expand upon previous research demonstrating ADHD-related sex differences in cognitive control in childhood (e.g., Seymour et al., 2016) to test the following hypotheses: (a) Boys with ADHD will show greater improvement in deficient response inhibition and variability from childhood through adolescence than girls with ADHD compared to same-sex TD children. (b) Boys and girls with ADHD will show similar improvement in deficient response inhibition and variability with increased WM demand from childhood through adolescence compared to same-sex TD children. (c) Response inhibition and variability will be related to ADHD symptoms across childhood and adolescence. (d) Poorer response inhibition and variability in childhood will predict less improvement in ADHD symptoms from childhood through adolescence.
Method
Participants
Participants include 594 children and adolescents with either a diagnosis of ADHD (n = 353; 104 girls) or TD controls (n = 241; 86 girls). Most participants (n = 574) had their first visit between age 8–12 years (Table 1) and 27% of this sample was included in previously published analyses with the same GNG tasks (Seymour et al., 2016). A subset of participants (n = 137) were recruited from the childhood sample to participate in adolescent follow-up visits providing longitudinal data and have completed either two visits (n = 108, 18%) or three visits (n = 29, 5% Fig. 1) with at least 1 year in between visits. Time between visits ranged from 1.41–9.49 years (mean = 3.73 years, mode = 2.06 years; Supplementary Fig. S1). Due to the longitudinal study being added on as a follow-up for eligible participants, data are considered missing by design and not due to attrition. All participants had a Full Scale Intelligence Quotient (FSIQ) and General Ability Index (GAI) above 80 (GAI range: 81–156) at the baseline visit using either (1) the Weschler's Intelligence Scales for Children current at the time of testing (WISC-IV: n = 378; WISC-V: n = 204), (2) the Wechsler Adult Intelligence Scale, 4th Edition (WAIS-IV) for 17 year-old participants (n = 2), or (3) the Wechsler Abbreviated Scale for Intelligence, 2nd Edition (WASI-II; n = 10). Participants were recruited from local schools, pediatricians (electronically via MyChart), community centers using flyers and word-of-mouth. Participants with ADHD were also recruited from local outpatient clinics. Study protocols were reviewed and approved by Johns Hopkins Medicine Institutional Review Board.
Age and sex distribution for children with ADHD (n = 353) and TD controls (n = 241) for the study visits. Each dot represents a study visit. Most participants had their initial study visit prior to age 13 years (n = 574). A subset of participants had two (n = 108) or three (n = 29) study visits. Online figures available in color
Procedures
All parents completed an initial telephone screening to determine eligibility. Children with a history of intellectual disability, seizures, traumatic brain injury, neurological illnesses, prenatal exposure to teratogons, genetic disorders, or other neurodevelopmental disorders (e.g., Autism Spectrum Disorders) were excluded from participation. Eligible participants completed two laboratory sessions for each visit. Sessions occurred within a period of six months to maintain validity of data collected between Session 1 and Session 2.
At each visit, a diagnosis of ADHD was determined using a structured or semi-structured parent interview, either the Diagnostic Interview for Children and Adolescents (DICA-IV; n = 352) or the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS; n = 389); the ADHD Rating Scale (ADHD-RS; n = 715) and the Conners Parent Rating Scale-Revised (n = 261) or –Version 3 (n = 449) were used to confirm diagnosis and to provide dimensional measures of ADHD symptom severity. Parents of all participants provided written consent, and all participants provided assent. All children taking stimulant medication (n = 203; see Table 1) were asked to withhold medication on the day prior to and day of testing. Children taking psychotropic medications other than stimulant medication (n = 4) did not discontinue their medication for study visits. Additionally, parents were instructed on both the diagnostic interview and report forms to make ratings based on their children's symptoms off medication.
Participants were included in the ADHD group if they (1) met criteria for an ADHD diagnosis either on the DICA-IV or K-SADS during the initial visit and (2) received a T-score of 60 or higher on the DSM Inattentive or DSM Hyperactive-Impulsive scales on the Conners Parent or Teacher (when available) rating scales (revised or 3rd edition), or a score of 2 or 3 (i.e., symptoms rated as occurring often or very often) on at least 6/9 items on the Inattentive or Hyperactivity/Impulsivity scales of the ADHD-RS Home or School (when available) Version. At the baseline visit, children with ADHD were allowed to meet criteria for comorbid psychiatric diagnoses on the DICA-IV or K-SADS including oppositional defiant disorder (ODD; n = 121), anxiety disorders (n = 48) and depressive disorders (n = 11) (Supplementary Table S1). Girls and boys with ADHD did not differ in comorbid diagnoses of ODD (p = 0.515), anxiety (p = 0.711) or depression (p = 0.404) at the baseline visit. Of the 85 children with ADHD who completed a follow-up visit, 8 children (9%) no longer met full diagnostic criteria for ADHD and comorbid diagnoses include ODD (n = 18), anxiety disorders (n = 10), and depressive disorders (n = 5). Master’s level clinicians conducted all diagnostic interviews and integrated information from rating scales to inform diagnoses under the supervision of licensed doctoral level clinical psychologists.
Participants were included in the control group if they: (1) did not meet criteria for any psychiatric disorders at the initial visit on the DICA-IV or K-SADS, (2) remained below clinically significant scores (T < 60) on the Conners Parent and Teacher (when available) rating scales, and ADHD-RS Home and School (when available) Versions, and (3) did not have immediate family with ADHD. Participants were able to meet criteria for any psychiatric disorder at the follow-up visits.
Go/No-Go Tasks.
During each visit, participants completed a neuropsychological assessment battery, including the simple and complex go/no-go (GNG) tasks described below. Tests were administered in the same order to all participants, with simple GNG always preceding complex GNG, as part of a larger battery over two days. This procedure was used to avoid influencing performance on the simple test through confounds associated with the complex version.
Simple GNG Paradigm.
All participants included in these analyses completed the simple GNG task at baseline (n = 594) and follow-up visits (n = 166). The task stimuli consisted of green spaceships for “Go” trials (80% of trials) and red spaceships for “No-Go” trials (20% of trials), presented one at a time. Stimuli were present on-screen for 300 ms with an interstimulus interval of 2000 ms (trial length = 2300 ms) during which a fixation cross was present on-screen. Participants were instructed to push the spacebar with their index finger as quickly as possible in response to green spaceships. The use of familiar stimulus–response associations (green for “Go”; red for “No-Go”) minimized the perceptual and cognitive demands of the tests. Presentation cues were weighted towards green spaceships at a ratio of 4:1, intensifying the need to inhibit a habituated motor response. Go and No-Go trials appeared in pseudorandom order with the restrictions that there were never fewer than three “Go” trials before a “No-Go” cue and never more than two “No-Go” trials in a row. There were 11 practice trials (8 “Go” cues; 3 “No-Go” cues) followed by 217 experimental trials (173 “Go” cues; 44 “No-Go” cues). Responses and reaction times (RT) were recorded for the entire trial duration. The task duration was 8 min and 19 s. The primary dependent variables were commission error rate (ComRate), defined as incorrectly pressing for a red spaceship, and tau, an ex-Gaussian parameter quantifying the skewed tail of the RT distribution. Tau was examined as an index of response variability separate from response speed rather than standard deviation of RT, which is highly correlated with mean RT, given the ubiquitous findings of increased tau in the ADHD cognitive literature (Epstein et al., 2011; Kofler et al., 2013; Tamm et al., 2012).
Complex GNG Paradigm.
A subset of participants included in these analyses completed the complex GNG task at baseline (n = 408), and follow-up visits (n = 97). The trial structure of the complex GNG task was nearly identical to that of the simple GNG task, with the same stimulus and fixation duration, but included additional cognitive demands. Children were instructed to push the button as quickly as possible in response to a green spaceship and in response to a red spaceship preceded by an even number of green spaceships. Participants were told to refrain from responding to red spaceships preceded by an odd number of green spaceships. There were five practice trials to demonstrate an even sequence, six practice trials to demonstrate an odd sequence, and 11 practice trials with each type of sequence. The task consisted of 207 experimental trials including 163 green “Go” trials, 21 red “Go” cues (i.e., red spaceships preceded by an even number of green spaceships), and 23 red “No-Go” trials (i.e., red spaceships preceded by an odd number of green spaceships). Reaction times (RT) were recorded for the entire trial duration. The total time of this task was 7 min and 56 s. The primary dependent variables were ComRate and tau.
ADHD Rating Scale, 4th Edition (ADHD-RS).
The ADHD-RS was completed by parents of participants at baseline (n = 574), and follow-up visits (n = 138). This is an 18-question parent-report measure of DSM-IV ADHD symptoms that consists of two symptom subscales, inattention (9 items) and hyperactive/impulsive (9 items) rated as symptom frequency (i.e., occurring rarely, sometimes, often, or very often). Raw scores were calculated for the inattention (IA) and hyperactivity/impulsivity (HI) symptom scales by summing across the nine items in each symptom domain. Higher scores reflect a greater number of symptoms.
Statistical Analysis
Effects of Diagnosis, Sex and Age on GNG Performance.
To examine whether response control differs across girls and boys with ADHD compared to each other and same-sex TD children, regardless of age, linear mixed effects models were employed. These models included subject as a random effect whereas diagnosis, sex, and age were included as fixed effects. Diagnosis (0 – TD, 1 – ADHD) and sex (0 – boys, 1 – girls) were binary dummy-coded variables. For the age variable, the minimum age (8.00 years) was subtracted across all participants. The three-way interaction of diagnosis, sex, and age was used to derive age coefficients for the four subgroups, i.e., TD-Boys, TD-Girls, ADHD-Boys, and ADHD-Girls. The two-way interaction of diagnosis and sex were used to compare girls and boys with and without ADHD on ComRate and Tau for the simple and complex GNG tasks. The intraclass correlation coefficient (ICC) is reported for the diagnosis × sex model and effect size estimates are reported as partial eta-squared (ηp2). To investigate how response control changes with age and whether there is differential change with age across girls and boys with and without ADHD, linear mixed effects models including the three-way interaction of diagnosis, sex, and age were conducted. This method allows for the inclusion of multiple time points per participant while accounting for the unbalanced data structure of irregular time intervals between the study visits. Associations with age were compared between the subgroups (i.e., TD-Boys vs. ADHD-Boys, TD-Girls vs. ADHD-Girls, TD-Girls vs. TD-Boys, and ADHD-Girls vs. ADHD-Boys) for the four GNG measures (Simple GNG ComRate and Tau, Complex GNG ComRate and Tau). For complex GNG analyses, we also included simple GNG performance as a covariate to examine the effect of increased working memory demands after accounting for basic response control performance. Model parameters were estimated for each GNG outcome separately and an FDR correction was applied to correct for multiple comparisons among the four subgroups. Analyses were also conducted with GAI SES, and ODD (Conners ODD T-score) as a covariate and any change in results are described in footnotes. GAI was not included as a covariate in the primary analyses based on compelling statistical and conceptual rationale against covarying intellectual reasoning ability when investigating cognitive processes in ADHD (Dennis et al., 2009; Irwin et al., 2019). Modeling and visualization were performed in R using linear mixed model package lme4 (Bates et al., 2015). Bivariate correlations between all variables included in these analyses are reported in Supplementary Table S2. For participants with multiple visits, we included only their oldest visit in the correlation analyses.
Relationship between response control and ADHD symptoms.
We then examined the relationship between ADHD symptoms and GNG performance (regardless of age) among girls and boys with ADHD. First, we tested whether baseline GNG performance (i.e., performance at the initial visit) moderated the relationship between age and ADHD symptoms using linear mixed models with the two-way interaction of GNG measure (ComRate or Tau) × Age predicting ADHD symptoms. We followed-up these analyses to look at longitudinal relationships among the sample of children with ADHD (n = 70) with Simple GNG data in childhood (ages 8–12 years) and ADHD-RS symptom raw scores in childhood and at an adolescent follow-up visit (ages 12–17 years, time between follow up visits: M = 3.74 years, range from 1.41–9.49 years) to determine whether response control in childhood predicts change in ADHD symptoms from childhood to adolescence using linear regression. These models include baseline Simple GNG ComRate or Tau as predictors of change in parent-rated IA and HI symptoms (child symptoms – adolescent symptoms) controlling for baseline symptoms, age at baseline, and difference in age from baseline to follow-up.
Results
Participant Characteristics.
Participant demographics are listed in Table 1. At visit 1, for boys and girls, there was no diagnostic group difference in age, socioeconomic status (SES), or race (% white); however, GAI was significantly higher in TD children compared with ADHD same-sex peers, particularly among boys. Girls and boys with ADHD did not differ in parent-rated ADHD symptoms of IA and HI. Diagnostic groups did not differ in the amount of time between visits (p = 0.951).
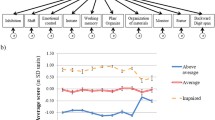
Simple GNG Response Inhibition (ComRate).
Linear mixed effects models testing for effects of diagnosis, sex, and their interaction (regardless of age) revealed a significant Diagnosis × Sex interaction for ComRate (β = -0.07, p = 0.025, ηp2 = 0.01, ICC = 0.26; Fig. 2, Supplementary Table S2). Subgroup comparisons indicated that boys with ADHD made more commission errors than TD boys (β = 0.11, p < 0.001), and ADHD girls (β = -0.12, p < 0.001), whereas girls with ADHD did not differ from TD girls (β = 0.04, p = 0.205).Footnote 1 Analyses examining associations with age revealed improved response inhibition with age across groups (ps < 0.001, Supplementary Table S3). Furthermore, there was a significant Diagnosis × Sex × Age interaction (β = 0.02, p = 0.046, ηp2 = 0.02; Supplementary Table S3), such that the diagnostic difference in the effect of age on ComRate differs for boys and girls. As shown in Fig. 3a-b, atypical response inhibition decreases with age among boys with ADHD (i.e., reduced deficits for ADHD compared to TD boys with increasing age), whereas atypical response inhibition increases with age among girls with ADHD (i.e., increased deficits for ADHD compared to TD girls with increasing age). Subgroup comparisons revealed that girls with ADHD showed less improvement in response inhibition with age compared to TD girls (β = -0.02, p = 0.016) and boys with ADHD (β = -0.02, p < 0.001), whereas age-related change was similar among boys with ADHD and TD boys (β = 0.00, p = 0.872).Footnote 2 Supplementary Fig. S2 shows individual data points within Diagnosis × Sex subgroups for Simple GNG ComRate.
Model-fitted age-related change in Simple GNG performance with the best fit line and 95% confidence intervals for each diagnosis by sex subgroup. Comparison of age-related change in Simple GNG ComRate for a TD boys versus ADHD boys and b TD girls versus ADHD girls. Comparison of age-related change in Simple GNG Tau for c TD boys versus ADHD boys and d TD girls versus ADHD girls. *p < 0.05 for the diagnostic group difference in the age effect. Online figures available in color
Simple GNG Response Variability (Tau).
Similar to the findings for ComRate, there was a significant Diagnosis × Sex interaction for tau (β = -0.18, p = 0.039, ηp2 = 0.01; ICC = 0.22; Fig. 2, Supplementary Table S2), with a different pattern among the subgroup comparisons. Boys with ADHD showed higher tau than TD boys (β = 0.38, p < 0.001) as did girls with ADHD compared to TD girls (β = 0.20, p = 0.006), although the effect was larger in boys.Footnote 3 Analyses examining associations with age revealed reduced response variability with age across participants (ps < 0.001). As with ComRate, there was also a significant Diagnosis × Sex × Age interaction (β = 0.06, p = 0.028, ηp2 = 0.03; Supplementary Table S3). As shown in Fig. 3c-d, atypical response variability decreases with age among boys with ADHD (i.e., reduced deficits for ADHD compared to TD boys with increasing age), whereas atypical response variability does not change with age among girls with ADHD. Subgroup comparisons revealed that boys with ADHD tended to show a greater reduction in response variability with age compared to TD boys (β = -0.03, p = 0.036, did not survive FDR correction) whereas age associations did not differ among girls with ADHD compared to TD girls (β = 0.02, p = 0.232).Footnote 4
Complex GNG Response Inhibition (ComRate).
Contrary to the findings for the simple GNG task, there was no evidence of a Diagnosis × Sex interaction for Complex GNG ComRate (β = 0.00, p = 0.959, ηp2 < 0.01; ICC = 0.29; Fig. 2, Supplementary Table S2), with more commission errors among both boys and girls with ADHD compared to TD boys and girls (βs = 0.10, ps < 0.001) and no difference among girls and boys with ADHD (β = -0.03, p = 0.301). Analyses examining associations with age revealed improved response inhibition with age under conditions with increased working memory demand across participants (ps < 0.01), with some evidence of differential associations with age across subgroups (Diagnosis × Sex × Age interaction, β = -0.02, p = 0.089, ηp2 = 0.01; Fig. 4a-b, Supplementary Table S3). A priori subgroup comparisons revealed that girls with ADHD showed more improvement with age for Complex GNG ComRate compared to TD girls (β = -0.02, p = 0.019) and boys with ADHD (β = -0.02, p = 0.018), whereas age-related change was similar among boys with ADHD and TD boys (β = 0.00, p = 0.849).Footnote 5
Model-fitted age-related change in Complex GNG performance (adjusted for Simple GNG performance) with the best fit line and 95% confidence intervals for each diagnosis by sex subgroup. Comparison of age-related change in Complex GNG ComRate for a TD boys versus ADHD boys and b TD girls versus ADHD girls. Comparison of age-related change in Complex GNG Tau for c TD boys versus ADHD boys and d TD girls versus ADHD girls. *p < .05 for the diagnostic group difference in the age effect. Online figures available in color
Complex GNG Response Variability (Tau).
For Complex GNG tau, there was a Diagnosis × Sex interaction (β = -0.24, p = 0.039, ηp2 = 0.01; ICC = 0.27; Fig. 2, Supplementary Table S2), with subgroup comparisons revealing higher tau among boys with ADHD compared to TD boys (β = 0.43 p < 0.001) and higher tau among girls with ADHD compared to TD girls (β = 0.20, p = 0.032) across the age range, although the effect was larger in boys.Footnote 6 Analyses examining associations with age revealed significantly reduced Complex GNG tau with age for boys with ADHD (p = 0.002) and TD girls (p < 0.001), but not for girls with ADHD (p = 0.319) or TD boys (p = 0.187), with evidence of differential associations with age across subgroups (Diagnosis × Sex × Age interaction, β = 0.07, p = 0.020, ηp2 = 0.07; Fig. 4c-d, Supplementary Table S3). Subgroup comparisons revealed that girls with ADHD showed less improvement in response variability with age compared to TD girls (p = 0.047), although this effect did not survive the FDR correction and no other subgroup comparisons approached significance.
Relationship between Response Control and ADHD Symptoms
To better understand how task-based measures of response control relate to ADHD symptom dimensions, we examined correlations between GNG performance and parent-rated symptoms of ADHD separately for the IA and HI symptom domains. Correlations among the full sample of 8–17 year-olds (regardless of age) revealed moderate positive correlations between most GNG performance measures and ADHD symptoms (rs range from 0.24 to 0.36; see Suplementary Table S2).
Linear mixed models testing whether baseline simple GNG performance moderates the relationship between ADHD symptoms and age revealed a significant effect for Simple GNG ComRate and IA symptoms only among the overall ADHD group (β = 1.24, p = 0.012, ηp2 = 0.01). Specifically, children with ADHD with good response inhibition at baseline (i.e., commission error rate below 0.62; Supplementary Fig. S3) showed a negative relationship between age and IA symptoms. In contrast, children with ADHD with poor baseline response inhibition (i.e., commission error rate above 0.62) there was no significant relationship between age and IA symptoms.
To better understand how response control in childhood predicts ADHD symptoms in adolescence, linear regression models were conducted among the sample of children with ADHD (n = 70) with Simple GNG ComRate and Tau in childhood as predictors of ADHD symptom change from childhood to adolescence controlling for baseline symptoms, age at baseline, and difference in age from baseline to follow-up. Among children with ADHD, ADHD symptoms were strongly correlated between timepoints for both IA (r = 0.50) and HI (r = 0.53). Results revealed a negative relationship between Simple GNG ComRate and change in IA symptoms (β = -7.65, p = 0.031), such that poor response inhibition in childhood predicts less improvement in IA symptoms from childhood to adolescence with a stronger effect among boys than girls with ADHD (Table 2). There was no significant relationship between Simple GNG ComRate and HI symptom change (β = -1.52, p = 0.688) or Simple GNG Tau and IA (β = 0.002, p = 0.875) or HI (β = 0.002, p = 0.859) symptom change.
Discussion
The current study advances and integrates the existing ADHD cognitive and clinical literature by evaluating the impact of sex on developmental changes in cognitive control and ADHD symptoms as well as the relationship between cognitive control and ADHD inattentive and hyperactive/impulsive symptoms. Overall, our findings suggest that there are ADHD-related sex differences in these developmental patterns from childhood to adolescence. Specifically, girls with ADHD show increased deficits in cognitive control under minimal working memory demands with age, whereas boys with ADHD show decreased deficits with age. In contrast, boys and girls with ADHD both show decreased deficits in cognitive control under greater working memory demands across development. Lastly, our findings suggest a significant relationship between response inhibition and ADHD inattentive symptoms from childhood to adolescence such that boys with ADHD who demonstrate poor response inhibition during childhood show greater inattentive symptoms during adolescence and less improvement in inattentive symptoms over time. No significant relationship between cognitive control and ADHD symptoms was found in girls with ADHD.
These findings replicate those reported in previous studies regarding ADHD-related sex differences in cognitive control. Seymour et al. (2016) found that boys with ADHD made more inhibition errors compared to TD peers on a GNG task with minimal working memory demand (d = 0.62), whereas the performance of girls with ADHD did not differ from that of TD girls (d = 0.18). In contrast, Seymour et al. found that both boys and girls with ADHD made more inhibition errors compared to TD peers when working memory demands were increased (girls d = 0.59, boys d = 0.61), although this study was underpowered to detect the Diagnosi s × Sex × Task interaction. It is worth noting that increased response variability is observed in girls and boys with ADHD, regardless of working memory demands, consistent with prior work (e.g., Epstein et al., 2011; Seymour et al., 2016). Our findings offer further insight into developmental changes in cognitive control in children with ADHD, revealing that although girls with ADHD did not show deficits in response inhibition under minimal working memory demands in childhood, they showed less improvement in response inhibition with age resulting in greater deficits in adolescence. One other study examining girls with and without ADHD found a different developmental pattern, such that girls with ADHD showed greater deficits in response inhibition compared to TD girls in childhood (Gordon & Hinshaw, 2020). One reason for this discrepancy could be differences in age range of the recruited participants. Gordon and Hinshaw’s sample included girls as young as 6 years old, whereas our sample includes children 8 years and older. Gordon and Hinshaw therefore captured a developmental period early in childhood when cognitive control deficits exist between girls with and without ADHD. This might thereby explain the reported difference, since the developmental pattern observed in adolescence is similar to the pattern reported in this study, such that girls with ADHD begin to lag behind TD girls.
Our analyses across age revealed that children with ADHD who have poor cognitive control in childhood were likely to have less improvement in inattentive symptoms with age. These findings stand in contrast to findings from the two prior longitudinal studies of cognitive control in children with ADHD. In one study, investigators found that childhood response inhibition (as measured by a Stop Signal task) was unrelated to the trajectory of ADHD symptoms regardless of level of cognitive impairment in childhood (Karalunas et al., 2017). However, this study did reveal that age-related improvements in visual spatial working memory were related to a decrease in inattentive symptoms, but only for children with ADHD with impaired working memory at age 7. An additional study focusing only on girls also revealed that the persistence or desistence of ADHD symptoms was unrelated to the developmental trajectory of response inhibition or working memory (Gordon & Hinshaw, 2020). One possible explanation for these discrepancies may be the different tasks used to assess cognitive control across these studies. Our simple and complex GNG tasks provide measures of response inhibition errors, variability and, indirectly, working memory through increased cognitive load. These variables could yield a different pattern of results across age compared to the Stop-Signal, Spatial Span-backwards (Karalunas et al., 2017) or Digit Span (Gordon & Hinshaw, 2020) variables.
The ADHD-related sex differences in developmental cognitive control patterns and the relationship with ADHD presentation may relate to differences in the clinical presentation of ADHD in boys and girls. There is a growing literature on sex-related differences in the clinical presentation and outcomes of ADHD (Biederman et al., 2008; Dalsgaard et al., 2002; Hechtman et al., 2016; Lahey et al., 2016; Rasmussen & Levander, 2009; Stern et al., 2020) such that girls show less hyperactive symptoms and higher rates of anxiety and depression while boys show more inattentive symptoms and higher rates of externalizing disorders. Though our findings do not directly measure functional outcomes, girls with ADHD showed less age-related improvement in cognitive control under minimal working memory demands compared to TD girls and boys with ADHD, suggesting a possible neurocognitive basis for poorer functional outcomes. In addition, the lack of persistent cognitive deficits found in boys with ADHD during adolescence may be consistent with the developmental lag model of ADHD. In other words, boys with ADHD may have a maturational delay such that greater cognitive deficits are observed in childhood, but as the brain matures during adolescence, these cognitive deficits improve for boys, but not girls, with ADHD. The persistent developmental lag observed in girls with ADHD may explain why girls have worse functional outcomes compared to boys with ADHD.
It is also important to consider these findings with regard to their potential impact on clinical assessment and treatment planning. Predictive analyses indicate that response inhibition during childhood moderates the relationship between response control and number of IA symptoms in adolescence, particularly for boys with ADHD, such that boys with ADHD who have poor cognitive control in childhood have more IA symptoms during adolescence. This suggests that childhood measures of response control could add value to clinical assessments by informing the likelihood of ADHD symptom persistence or remittance in young boys. Currently, clinicians rely on DSM-5 criteria and parent- and self-reported measures of symptomology to diagnose ADHD and develop treatment plans. These assessment tools probe general behaviors with scales of impairments susceptible to environmental and cultural influences (Bell, 2011). The results of the current study suggest that objective measures of cognitive control are capable of differentiating individuals with and without ADHD and can be used to make predictions about age-related change. Although predictive models of executive functioning or symptom severity can include parent- and self-reported information, the inclusion of objective measures of cognitive control could lead to more precise predictions of clinical outcomes in children with ADHD providing additional insight into heterogeneity in ADHD. Furthermore, current assessment tools lack the capacity to predict persistence and remittance in children with ADHD. The use of objective measures of cognitive impairment, such as assessing cognitive control through a GNG task, could provide clinicians with unbiased data to potentially inform recommendations for treatment, although further work is needed in this area. Further research should focus on achieving a more precise understanding of the developmental trajectories of cognitive control and other neurocognitive deficits implicated in ADHD using large longitudinal samples. Futhermore, it is necessary to replicate our findings and evaluate the reliability and validity of the computerized instrument (Bauer et al., 2012) before the results can have clinical utility and bridge the gap between cognitive and clinical psychology research.
This study provides novel information on sex differences in the development of cognitive control in relation to ADHD symptoms providing a foundation for further research on this important topic. Some limitations of this study should be noted, including the inclusion of parent- and self-reported information, reliance on primarily cross-sectional behavioral data and the focus on only a few cognitive processes (response inhibition and variability, and working memory) and functional outcomes (ADHD symptoms). It is also important to note that 61% of participants with ADHD regularly took stimulant medication at the time of the study, which may have resulted in underreporting of ADHD symptoms. Despite being instructed to report their child’s behavior off medication, parents may not regularly observed their children’s behaviors without medication. Future studies involving participants on medication and parent- and self-reported information should include confidence ratings to help remove additional noise. Additionally, the use of cross-lagged panel models applied in this study prohibits parsing of between- versus within-person variance (Curran et al., 2014), emphasizing the need for future longitudinal research that can address both between- and within-person changes. Although the limited longitudinal data in our sample may fail to accurately capture within-person developmental changes during this time period, it does inform our understanding of general developmental patterns to guide longitudinal hypotheses. Future studies involving primarily longitudinal data will be important to advance this literature and understand individual trajectories of change in cognitive control in relation to functional outcomes extending beyond ADHD symptoms, including academic achievement, emergence of comorbidities, and impairment in social, academic, and family functioning. Furthermore, future studies should extend these findings to examine the developmental relationship between cognitive and behavioral symptoms of ADHD, and brain structure and function to directly address questions about neurodevelopmental lag in children with ADHD.
In conclusion, our findings of ADHD-related sex differences in the developmental patterns of cognitive control in relation to ADHD symptoms from childhood to adolescence advances and integrates the existing ADHD cognitive and clinical literature. The ultimate goal of this work is to better understand the cognitive phenotype of ADHD as a potential predictor of clinical outcome or response to intervention. These findings suggest the importance of research focused on identifying whether cognitive impairments differ in girls and boys with ADHD depending on cognitive process, developmental stage, or comorbidities. Taking this approach will be critical for parsing the heterogeneity of ADHD in terms of clinical presentation, cognitive impairments, and functional outcomes, towards a goal of early identification and prevention as well as improving interventions for ADHD.
Notes
Including GAI, SES, and ODD symptoms as covariates for the Simple GNG ComRate model results in a weaker Diagnosis × Sex interaction (p = 0.097), although the a priori subgroup comparisons are similar with a significant effect of diagnosis for boys (p < 0.001) and not for girls (p = 0.269), as well as an effect of sex within the ADHD group (p < 0.001).
Including GAI, SES, and ODD symptoms as covariates for the Simple GNG ComRate model examining effects of age results in a weaker Diagnosis × Sex × Age interaction (p = 0.096), although a priori subgroup comparisons are similar with an effect of diagnosis among girls (p = 0.018) but not boys (p = 0.786) as well as an effect of sex within the ADHD group (p = 0.002).
Including GAI, SES, and ODD symptoms as covariates for the Simple GNG Tau model results in a weaker Diagnosis × Sex interaction (p = 0.059), whereas the a priori subgroup comparisons suggest a significant effect of diagnosis for boys (p < 0.001) but not for girls (p = 0.124).
Including GAI, SES, and ODD symptoms as covariates for the Simple GNG ComRate model examining effects of age results in a weaker Diagnosis × Sex × Age interaction (p = 0.091), and a priori subgroup comparisons no longer show a significant effect of diagnosis among boys (p = 0.106).
Including GAI, SES, and ODD symptoms as covariates for the Complex GNG ComRate model examining effects of age suggests there is not a Diagnosis × Sex × Age interaction (p = 0.266), and a priori subgroup comparisons no longer show a significant effect of diagnosis among girls (p = 0.248) or a sex effect within the ADHD group (p = 0.172).
Including GAI, SES, and ODD symptoms as covariates for the Complex GNG Tau model results in a weaker Diagnosis × Sex interaction (p = 0.049). The a priori subgroup comparisons revealed a significant effect of diagnosis for boys (p < 0.001) whereas it was no longer significant for girls (p = 0.211).
References
Abikoff, H. B., Jensen, P. S., Arnold, L. L. E., et al. (2002). Observed classroom behavior of children with ADHD: Relationship to gender and comorbidity. Journal of Abnormal Child Psychology, 30(4), 349–359. https://doi.org/10.1023/A:1015713807297
Barkley, R. A. (1997). Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65–94. https://doi.org/10.1037/0033-2909.121.1.65
Bates, D., Mächler, M., Bolker, B. M., & Walker, S. C. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. https://doi.org/10.18637/jss.v067.i01
Bauer, R. M., Iverson, G. L., Cernich, A. N., Binder, L. M., Ruff, R. M., & Naugle, R. I. (2012). Computerized neuropsychological assessment devices: joint position paper of the American Academy of Clinical Neuropsychology and the National Academy of Neuropsychology. Archives of Clinical Neuropsychology, 27(3), 362–373.
Bell, A. S. (2011). A critical review of ADHD diagnostic criteria: What to address in the DSM-V. Journal of Attention Disorders, 15(1), 3–10. https://doi.org/10.1177/1087054710365982
Biederman, J., Ball, S. W., Monuteaux, M. C., Mick, E., et al. (2008). New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. Journal of the American Academy of Child and Adolescent Psychiatry, 47(4), 426–434. https://doi.org/10.1097/CHI.0b013e31816429d3
Biederman, J., Mick, E., Faraone, S. V., Braaten, E., Doyle, A., Spencer, T., et al. (2002). Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic. American Journal of Psychiatry, 159(1), 36–42. https://doi.org/10.1176/appi.ajp.159.1.36
Biederman, J., Monuteaux, M. C., Mick, E., Spencer, T., Wilens, T. E., Klein, K. L., et al. (2006). Psychopathology in females with attention-deficit/hyperactivity disorder: A controlled, five-year prospective study. Biological Psychiatry, 60, 1098–1105. https://doi.org/10.1016/j.biopsych.2006.02.031
Biederman, J., Petty, C. R., Ball, S. W., Fried, R., Doyle, A. E., Cohen, D., et al. (2009). Are cognitive deficits in attention deficit/hyperactivity disorder related to the course of the disorder? A prospective controlled follow-up study of grown up boys with persistent and remitting course. Psychiatry Research, 170(2–3), 177–182. https://doi.org/10.1016/j.psychres.2008.09.010
Biederman, J., Petty, C. R., Fried, R., Doyle, A. E., et al. (2007). Stability of executive function deficits into young adult years: a prospective longitudinal follow-up study of grown up males with ADHD. ActaPsychiatricaScandinavica, 116(2), 129–136. https://doi.org/10.1111/j.1600-0447.2007.01008.x
Brown, T. (2013). A new understanding of ADHD in children and adults: Executive function impairments. Routledge. https://doi.org/10.4324/9780203067536
Carter, C. S., & Krus, M. K. (2012). Dynamic cognitive control and frontal-cingulate interactions. In M. I. Posner (Ed.), Cognitive neuroscience of attention (2nd ed., pp. 88–98). New York: Guilford Press.
Curran, P. J., Howard, A. L., Bainter, S. A., Lane, S. T., & McGinley, J. S. (2014). The separation of between-person and within-person components of individual change over time: A latent curve model with structured residuals. Journal of consulting and clinical psychology, 82(5), 879.
Dalsgaard, S., Mortensen, P. B., Frydenberg, M., & Thomsen, P. H. (2002). Conduct problems, gender and adult psychiatric outcome of children with attention-deficit hyperactivity disorder. British Journal of Psychiatry, 181(4), 416–421. https://doi.org/10.1192/bjp.181.5.416
Dennis, M., Francis, D. J., Cirino, P. T., Schachar, R., Barnes, M. A., & Fletcher, J. M. (2009). Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. Journal of the International Neuropsychological Society : JINS, 15(3), 331–343. https://doi.org/10.1017/S1355617709090481
Dimoska, A., Johnstone, S. J., Barry, R. J., & Clarke, A. R. (2003). Inhibitory motor control in children with attention-deficit/hyperactivity disorder: Event-related potentials in the stop-signal paradigm. Biological Psychiatry, 54(12), 1345–1354. https://doi.org/10.1016/S0006-3223(03)00703-0
Epstein, J. N., Langberg, J. M., Rosen, P. J., et al. (2011). Evidence for higher reaction time variability for children with ADHD on a range of cognitive tasks including reward and event rate manipulations. Neuropsychology, 25(4), 427–441. https://doi.org/10.1037/a0022155
Gershon, J. (2002). A Meta-Analytic Review of Gender Differences in ADHD. Journal of Attention Disorders, 5(3), 143–154. https://doi.org/10.1177/108705470200500302
Gordon, C. T., & Hinshaw, S. P. (2020). Executive Functions in Girls With and Without Childhood ADHD Followed Through Emerging Adulthood: Developmental Trajectories. Journal of Clinical Child and Adolescent Psychology, 49(4). https://doi.org/10.1080/15374416.2019.1602840
Hechtman, L., Swanson, J. M., Sibley, M. H., et al. (2016). Functional Adult Outcomes 16 Years After Childhood Diagnosis of Attention-Deficit/Hyperactivity Disorder: MTA Results. Journal of the American Academy of Child and Adolescent Psychiatry, 55(11), 945–952. https://doi.org/10.1016/j.jaac.2016.07.774
Irwin, L. N., Kofler, M. J., Soto, E. F., & Groves, N. B. (2019). Do children with attention-deficit/hyperactivity disorder (adhd) have set shifting deficits? Neuropsychology, 33(4), 470–481. https://doi.org/10.1037/neu0000546
Karalunas, S. L., Gustafsson, H. C., Dieckmann, N. F., Tipsord, J., Mitchell, S. H., & Nigg, J. T. (2017). Heterogeneity in development of aspects of working memory predicts longitudinal ADHD symptom change. Journal of Abnormal Psychology, 126(6), 774–792. https://doi.org/10.1037/abn0000292
Klein, R. G., Mannuzza, S., Ramos Olazagasti, M. A., et al. (2012). Clinical and functional outcome of childhood attention-deficit/ hyperactivity disorder 33 years later. Archives of General Psychiatry, 69(12), 1295–1303. https://doi.org/10.1001/archgenpsychiatry.2012.271
Kofler, M. J., Irwin, L. N., Soto, E. F., Groves, N. B., Harmon, S. L., & Sarver, D. E. (2019). Executive Functioning Heterogeneity in Pediatric ADHD. Journal of Abnormal Child Psychology, 47(2), 273–286. https://doi.org/10.1007/s10802-018-0438-2
Kofler, M. J., Rapport, M. D., Sarver, D. E., et al. (2013). Reaction time variability in ADHD: A meta-analytic review of 319 studies. Clinical Psychology Review, 795–811. https://doi.org/10.1016/j.cpr.2013.06.001
Kofler, M. J., Sarver, D. E., Spiegel, J. A., Day, T. N., Harmon, S. L., Wells, E. L., & Author, C. (2017). Heterogeneity in ADHD: Neurocognitive Predictors of Peer, Family, and Academic Functioning. Child Neuropsychology, 23(6), 733–759. https://doi.org/10.1080/09297049.2016.1205010
Lahey, B. B., Hartung, C. M., Loney, J., Pelham, W. E., Chronis, A. M., & Lee, S. S. (2007). Are There Sex Differences in the Predictive Validity of DSM-IV ADHD Among Younger Children? Journal of Clinical Child and Adolescent Psychology, 36(2), 113–126. https://doi.org/10.1080/15374410701274066
Lahey, B. B., Lee, S. S., Sibley, M. H., Applegate, B., Molina, B. S. G., & Pelham, W. E. (2016). Predictors of Adolescent Outcomes among 4–6 Year Old Children with Attention-Deficit/Hyperactivity Disorder. Journal of Abnormal Psychology, 125(2), 168–181. https://doi.org/10.1037/abn0000086
Lijffijt, M., Kenemans, J. L., Verbaten, M. N., & Van Engeland, H. (2005). A meta-analytic review of stopping performance in attention-deficit/ hyperactivity disorder: Deficient inhibitory motor control? Journal of Abnormal Psychology, 114(2), 216–222. https://doi.org/10.1037/0021-843X.114.2.216
Luo, Y., Weibman, D., Halperin, J. M., & Li, X. (2019). A Review of Heterogeneity in Attention Deficit/Hyperactivity Disorder (ADHD). Frontiers in Human Neuroscience, 13. https://doi.org/10.3389/fnhum.2019.00042
Malone, P. S., Eck, K. V., Flory, K., & Lamis, D. A. (2010). A Mixture-Model Approach to Linking ADHD to Adolescent Onset of Illicit Drug Use. Developmental Psychology, 46(6), 1543–1555. https://doi.org/10.1037/a0020549
Miller, M., & Hinshaw, S. P. (2010). Does childhood executive function predict adolescent functional outcomes in girls with ADHD? Journal of Abnormal Child Psychology, 38(3), 315–326. https://doi.org/10.1007/s10802-009-9369-2
Murray, A. L., Booth, T., Eisner, M., Auyeung, B., Murray, G., & Ribeaud, D. (2018). Sex differences in ADHD trajectories across childhood and adolescence. Developmental Science, 22(1). https://doi.org/10.1111/desc.12721
Newcorn, J. H., Halperin, J. M., Jensen, P. S., et al. (2001). Symptom profiles in children with ADHD: Effects of comorbidity and gender. Journal of the American Academy of Child and Adolescent Psychiatry, 40(2), 137–146. https://doi.org/10.1097/00004583-200102000-00008
Nigg, J. T. (1999). The ADHD response-inhibition deficit as measured by the stop task: Replication with DSM-IV combined type, extension, and qualification. Journal of Abnormal Child Psychology, 27(5), 393–402. https://doi.org/10.1023/A:1021980002473
Nigg, J. T. (2005). Neuropsychologic theory and findings in attention-deficit/hyperactivity disorder: the state of the field and salient challenges for the coming decade. Biological psychiatry, 57(11), 1424–1435. https://doi.org/10.1016/j.biopsych.2004.11.011
Nigg, J. T. (2017). Annual Research Review: On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry, 58(4), 361–383.
Pennington, B. F., & Ozonoff, S. (1996). Executive Functions and Developmental Psychopathology. Journal of Child Psychology and Psychiatry, 37(1), 51–87. https://doi.org/10.1111/j.1469-7610.1996.tb01380.x
Pievsky, M. A., & McGrath, R. E. (2018). The neurocognitive profile of attention-deficit/hyperactivity disorder: A review of meta-analyses. Archives of Clinical Neuropsychology, 33(2), 143–157.
Polanczyk, G. V., Willcutt, E. G., Salum, G. A., Kieling, C., & Rohde, L. A. (2014). ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. International Journal of Epidemiology, 43(2), 434–442. https://doi.org/10.1093/ije/dyt261
Rasmussen, K., & Levander, S. (2009). Untreated ADHD in adults are there sex differences in symptoms, comorbidity, and impairment? Journal of Attention Disorders, 12(4), 353–360. https://doi.org/10.1177/1087054708314621
Rucklidge, J. J. (2006). Gender differences in neuropsychological functioning of New Zealand adolescents with and without attention deficit hyperactivity disorder. International Journal of Disability, 53(1), 47–66. https://doi.org/10.1080/10349120600577402
Rucklidge, J. J., & Tannock, R. (2001). Psychiatric, psychosocial, and cognitive functioning of female adolescents with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 40(5), 530–540. https://doi.org/10.1097/00004583-200105000-00012
Senderecka, M., Grabowska, A., Szewczyk, J., Gerc, K., & Chmylak, R. (2012). Response inhibition of children with ADHD in the stop-signal task: An event-related potential study. International Journal of Psychophysiology, 85(1), 93–105. https://doi.org/10.1016/j.ijpsycho.2011.05.007
Seymour, K. E., Mostofsky, S. H., & Rosch, K. S. (2016). Cognitive load differentially impacts response control in girls and boys with ADHD. Journal of Abnormal Child Psychology, 44(1), 141–154. https://doi.org/10.1007/s10802-015-9976-z
Rosch, K. S., Dirlikov, B., & Mostofsky, S. H. (2013). Increased intrasubject variability in boys with ADHD across tests of motor and cognitive Control. Journal of Abnormal Child Psychology, 41(3), 485–495. https://doi.org/10.1007/s10802-012-9690-z
Skogli, E. W., Egeland, J., Andersen, N., Hovik, K. T., & Øie, M. (2014). Few differences in hot and cold executive functions in children and adolescents with combined and inattentive subtypes of ADHD. Child Neuropsychology, 20(2), 162–181. https://doi.org/10.1080/09297049.2012.753998
Stern, A., Agnew-Blais, J. C., Danese, A., Fisher, H. L., et al. (2020). Associations between ADHD and emotional problems from childhood to young adulthood: a longitudinal genetically sensitive study. Journal of Child Psychology and Psychiatry. https://doi.org/10.1111/jcpp.13217
Tamm, L., Narad, M. E., Antonini, T. N., O’Brien, K. M., Hawk, L. W., & Epstein, J. N. (2012). Reaction time variability in ADHD: A Review. Neurotherapeutics, 9, 500–508. https://doi.org/10.1007/s13311-012-0138-5
van Lieshout, M., Luman, M., Buitelaar, J., Rommelse, N. N. J., & Oosterlaan, J. (2013). Does neurocognitive functioning predict future or persistence of ADHD? A systematic review. Clinical Psychology Review, 33(4), 539–560.
van Lieshout, M., Luman, M., Schweren, L. J., Twisk, J. W. R., Faraone, S. V., et al. (2019). The course of neurocognitive functioning and prediction of behavioral outcome of ADHD affected and unaffected siblings. Journal of Abnormal Child Psychology, 47(3), 405–419.
Vaurio, R. G., Simmonds, D. J., & Mostofsky, S. H. (2009). Increased intra-individual reaction time variability in attention-deficit/hyperactivity disorder across response inhibition tasks with different cognitive demands. Neuropsychologia, 47, 2389–2396. https://doi.org/10.1016/j.neuropsychologia.2009.01.022
Willcutt, E. G., Doyle, A. E., Nigg, J. T., Faraone, S. V., & Pennington, B. F. (2005). Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry, 57(11), 1336–1346. https://doi.org/10.1016/j.biopsych.2005.02.006
Funding
This research was supported by the National Institutes of Health (SM: R01MH078160 and R01MH085328; KR: K23MH101322 and R03MH119457; KES: K23MH107734 and Brain and Behavior Foundation NARSAD Young Investigator’s Award).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests
There are no conflicts of interest to report.
Disclaimer
This work was prepared while Karen Seymour was employed at Johns Hopkins University and Kennedy Krieger Institute. The opinions expressed in this article are the author's own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dr. Seymour is now employed at the National Institutes of Health Center for Scientific Review.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
DeRonda, A., Zhao, Y., Seymour, K.E. et al. Distinct Patterns of Impaired Cognitive Control Among Boys and Girls with ADHD Across Development. Res Child Adolesc Psychopathol 49, 835–848 (2021). https://doi.org/10.1007/s10802-021-00792-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-021-00792-2