Abstract
Depression is one of the most common mental health problems among U.S. adolescents, particularly among Latinos. Parent-child ratings of the presence and severity of child depressive symptoms show only low-to-moderate agreement. However, research has failed to examine discrepancies in populations with the highest levels of unmet need and little is known about patterns and predictors of parent-child agreement in ratings of depressive symptoms among ethnic minority families in community settings. Using a sample of 184 low-income, predominantly Latino, 5th through 7th grade students (63.6% female) at chronic risk for depression, this study utilized exploratory Latent Class Analysis (LCA) to uncover patterns of parent-child endorsement of core diagnostic depressive symptoms. Overall, children reported higher levels of core (i.e., depressed mood, anhedonia, irritability) and secondary (e.g., sleep disturbances) depressive symptoms relative to their parents. The three latent classes identified include a low endorsement and high agreement class (LH), high endorsement and high agreement class (HH), and high child endorsement and low agreement class (HCL). Multinomial regression models revealed that previous mental health service use and higher externalizing problems were associated with HH class membership, relative to HCL class membership. Findings provide evidence that a substantial number of children may have depressive symptoms that go undetected by their parents. Access to services among children at-risk for depression may be increased with psychoeducation to improve parental awareness and stigma reduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Depression is a common and recurrent mental health problem that causes significant academic, interpersonal, and physical impairment in the lives of children and adolescents (henceforth referred to as “children” unless otherwise specified) (Jaycox et al. 2009). The onset of depressive disorders typically occurs in adolescence, and lifetime prevalence rates increase steadily through this period (Merikangas et al. 2010). While rates of mood disorders in European American and African American children are comparable, Latino children are 1.4 times more likely to develop a depressive disorder in adolescence (Merikangas et al. 2010). Despite the significant impairment associated with Major Depressive Disorder (MDD), only 39.4% of adolescents meeting diagnostic criteria utilize mental health services (MHS) (Merikangas et al. 2011), and unmet need is particularly high among ethnic minority adolescents (Cummings and Druss 2011). More generally, children with internalizing problems (e.g., anxiety and depression) are less than half as likely to receive treatment relative to those with externalizing problems (e.g., conduct problems and aggression), with ethnic minority and immigrant children exhibiting the lowest rates of service use (Gudiño et al. 2008, 2009). Research is needed to evaluate whether parental under-recognition of mental health problems plays a critical role in the low rates of MHS use among children with depression, particularly among ethnic minority youth.
Patterns of Parent-Child Discrepancies
Best practices in evidence-based assessment of child mental health problems entail collecting and incorporating the reports of multiple informants, with the assumption that each informant provides unique and incrementally valid information (Hunsley and Mash 2007). However, when parents and their children rate the child’s emotional and behavioral problems, their ratings often diverge (i.e., rs ranging from 0.20 to 0.30; Achenbach et al. 1987; De Los Reyes et al. 2015), representing one of the most consistent findings in clinical child research. Two important patterns emerge from parent-child discrepancies research. First, meta analytic work demonstrates that, across studies, parent-child ratings of internalizing problems (r = 0.26) are consistently found to be more discrepant than ratings of externalizing problems (r = 0.32; De Los Reyes et al. 2015). In most cases, parent-child discrepancies in ratings of internalizing problems are driven by the child reporting more internalizing problems than their parents. Studies examining agreement in ratings of child depressive symptoms have found ratings to be particularly low (k = 0.09), with parents and their children agreeing on the presence of only 7.7% of symptoms (Grills and Ollendick 2003). Symptom level examinations demonstrate that, across disorders, informants more often agree on the presence and severity of symptoms that are observable relative to those that are not (Rescorla et al. 2017). These findings suggest that utilizing child reports of internalizing problems is important due to the covert nature of the problems, and the incongruity of a child’s experience with parental report.
A second important pattern in discrepancies research is that parents in clinical samples generally report more emotional and behavior problems than their child, while the inverse is observed in community samples. While Martin et al. (2004) found that 38.1% of parents of clinic-referred children reported more problems than their child, Barker et al. (2007) found that 74% of children in a community sample reported more problems than their parents. Parent-child agreement is also higher in clinical settings (Rescorla et al. 2017), in which children tend to have a more severe clinical presentation that both the parent and child endorse. Despite these findings, research has yet to examine the association between MHS use history and discrepancies, particularly as they relate to parental under-reporting of child mental health problems. As parents are considered gatekeepers to their child’s treatment, such research could elucidate critical information about a fundamental barrier to treatment. Ultimately, these patterns in discrepancies research suggest that children in non-referred samples with internalizing problems, and particularly depressive symptoms, are especially likely to have parents who under-report their symptoms.
Correlates of Parent-Child Discrepancies
Parental Depressive Symptoms
There is considerable evidence to suggest that when parents report elevated levels of their own psychopathology they are also more likely to over-report their child’s internalizing and externalizing problems. Specifically, the depression-distortion hypothesis has received substantial attention and posits that parental depressive symptoms promote a negative perceptual bias by which a child’s behavior is more readily perceived as problematic (Richters and Pellegrini 1989). In clinical samples, parental depressive symptoms are associated with parental over-reporting relative to child self-report of internalizing and externalizing problems (Youngstrom et al. 2000). However, there have been some inconsistencies in recent findings regarding the role of parental depressive symptoms (De Los Reyes and Kazdin 2005). While some studies find a small effect of parental depressive symptoms (Gartstein et al. 2009), others find that a depressive bias is not uniformly observed across symptom types and across child age and gender groups (Gartstein et al. 2009; Affrunti and Woodruff-Borden 2015), and others find no effect (Lewis et al. 2012). Furthermore, no study to date has documented the role of parental depressive symptoms on parent-child discrepancies in ratings of child problems among U.S. Latinos, and research is needed to understand whether this effect extends to this population.
Demographic and Sociocultural Factors
Although findings regarding patterns of discrepancies across gender, age, and socioeconomic status (SES) are largely inconclusive (De Los Reyes and Kazdin 2005), those regarding race/ethnicity are more consistent. Studies conducted with both clinical and community samples find that discrepancies across problem types are larger for families from ethnic minority backgrounds. African American and Latino parents have been found to be more likely than European American parents to under-report internalizing problems, including anxiety symptoms, relative to child self-report (Dirks et al. 2014; Youngstrom et al. 2000). In a sample of families enrolled in public systems of care, Lau et al. (2004) found that while children across racial/ethnic groups reported similar levels of emotional and behavioral problems, parent-report of their child’s problems varied widely. Specifically, relative to European American parents, African American and Latino parents reported significantly fewer child mental health problems. However, these studies are limited to making comparisons across racial/ethnic groups without examining specific variables that may account for these differences.
Racial/ethnic variations in parent-child discrepancies in ratings of child emotional and behavioral problems may be explained in part by cultural orientations that influence parental appraisal of child behaviors. Weisz and colleagues’ (1987) adult distress threshold model provides a useful framework for conceptualizing ethno-cultural factors that may influence parent–child reporting discrepancies. According to the model, culture plays an important role in determining the thresholds that adults use to decide whether or not child behaviors are maladaptive and warrant attention. Parents from interdependent cultures, which value interpersonal harmony and deference shown towards adults, may more readily identify their child’s externalizing problems while overlooking their child’s internalizing problems (Weisz et al. 1987). Indeed, patterns of divergent reports of child problems among ethnic minority parent-child dyads suggest that these parents may use higher thresholds than their children when rating child psychopathology, and especially for internalizing problems such as depressive symptoms (Lau et al. 2004; Roberts et al. 2005). These culturally-informed thresholds may influence parental recognition of symptoms and in turn, play a role in disparities in rates of depression and MHS use among ethnic minority children. Among Latino families in particular, emphasis on values such as respect for authority and familism may impact socialization goals and parental attunement to specific child problem types (e.g., greater attention to externalizing problems; Stein and Polo 2014).
Other cultural factors may also play a role in patterns of parent-child discrepancies across racial/ethnic groups, although their impact on discrepancies has not been directly tested. For example, approximately 60% of U.S.-born Latinos speak Spanish in the home and have parents who are foreign-born and have higher Spanish than English proficiency (Federal Interagency Forum on Child and Family Statistics 2015). No study to date, however, has examined the relation between parental language and patterns of endorsement of child symptoms across informants. Parental language may be associated with parent-child communication barriers, particularly about child depression, which is more common in second-generation compared to first-generation Latinos (Peña et al. 2008). In addition, even when recognizing their child’s depressive symptoms, Latino parents may not endorse them because of perceived stigma (Vega et al. 2010). Further research is needed to understand the role of cultural factors on parent-child discrepancies across racial/ethnic groups.
Research Gaps and Methodological Limitations
Several research gaps and methodological limitations are present in the informant discrepancies literature. First, research examining discrepancies is largely limited to studies comparing ratings across broad categories, with fewer studies focusing on specific symptoms. In particular, relatively less is known about discrepancies in reports of child depressive symptoms and studies that have been conducted are primarily limited to samples of clinic-referred children and their families. Given that child depressive disorders are the most likely disorders that parents under-report relative to their children (Martin et al. 2004), such information would have important clinical utility by informing practitioners integrating multi-informant reports about problems that are especially likely to be missed by parents.
Second, discrepancies research has largely ignored the impact of co-occurring mental health problems on discrepancies. Although Youngstrom et al. (2004) found that the presence of child manic symptoms is associated with worse parent-child agreement in ratings of child internalizing and externalizing problems, no study to date has evaluated externalizing problems as a predictor of discrepancies in ratings of internalizing problems. Given the high rates of co-occurring mental health problems among children (Merikangas et al. 2010), it is important to understand the ways in which parental endorsement of co-occurring problems impacts agreement in ratings of child depressive symptoms.
A third limitation is the lack of a gold standard by which to determine which informant is more accurate or valid. Despite contributions of novel methods to address this problem (e.g., examining discrepancies as they relate to clinician diagnoses; Breland-Noble and Weller 2012), they do not allow for one informant to be considered more accurate or valid in their reports. A novel strategy that addresses this limitation but has yet to be utilized is the inclusion of multiple reports from the same informant. A study examining parent-child discrepancies among children chronically endorsing elevated depressive symptoms could elucidate factors associated with parental under-reporting of depressive symptoms that are persistently self-reported by children.
A fourth limitation in discrepancies research is the reliance on difference scores, which present serious mathematical and interpretative challenges that can lead to erroneous conclusions about the nature of parent-child reporting patterns and their correlates (see Laird and De Los Reyes 2013). As an alternative, exploratory Latent Class Analysis (LCA; McCutcheon 1987) is a person-centered approach that can be used to identify classes of parent-child endorsement of child mental health problems characterized by varying levels of agreement. This approach has been used to identify classes of multi-informant reporting that are linked to theoretically relevant constructs (e.g., De Los Reyes et al. 2009; Lerner et al. 2017). For example, LCA has been used to identify clinically meaningful classes of parent-teacher ratings of autism spectrum disorder (ASD) symptoms in children (Lerner et al. 2017).
The present study addresses these limitations by focusing on a school-based sample of predominantly low-income and ethnic minority children who are identified as chronically at-risk for depression. Further, exploratory LCA is used to determine the number and nature of classes of parent-child endorsement of child core depressive symptoms (i.e., core features of MDD that are necessary criteria for diagnosis) on a structured diagnostic interview. Additionally, clinical and sociodemographic predictors of class membership are explored. The study’s aims and hypotheses are as follows:
Aim I: Endorsement Levels across Core and Secondary Symptoms.
It is expected that children will report higher levels of depressive symptoms than their parents. This pattern is expected to emerge for a) core symptoms (i.e., depressed mood, anhedonia, and irritability); and b) secondary symptoms (e.g., sleep disturbances).
Aim II: Parent-Child Endorsement Agreement Classes.
Using LCA, parent and child reports of each of the three core depressive symptoms will be used to explore endorsement agreement classes. No a priori hypotheses are made about the number, structure, and distribution of endorsement agreement classes. However, it is expected that the degree of endorsement of child core depressive symptoms will vary across child and parent reports, and that classes characterized by different levels of parent-child endorsement and agreement will be identified.
Aim III: Clinical, Demographic, and Sociocultural Predictors.
Theoretically relevant clinical, demographic, and sociocultural predictors of latent class membership will be explored. Clinical predictors include child externalizing problems, parental depressive symptoms, and past year MHS use. Demographic and sociocultural predictors include child age, gender, ethnicity, parental education, and parent interview language (i.e., Spanish versus English).
Method
Participants
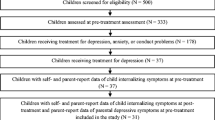
The sample includes 184 children chronically at-risk for depression, and their parents. Dyads were recruited from 10 elementary schools in a large metropolitan area in the Midwest. Children were 10 to 14 years of age (M = 11.8, SD = 1.0), 63.6% female, and in the 5th through 7th grade. Children identified as Latino (81.5%), African American (9.8%), European American (1.6%) or mixed race (7.1%). Latino children identified as Mexican American (64.8%), Puerto Rican (9.9%), Central or South American (3.7%), Cuban (0.6%), or mixed Latino/non-Latino ethnicity (21.0%). Parent participants included mothers (86.4%), fathers (7.6%), and other relatives (6.0%). Families were from primarily low SES backgrounds. Most (78.3%) reported annual incomes of $40,000 or less, and 71.3% of parents reported starting or completing high school or less as their highest level of education. Most parents were foreign-born (64.1%) and had lived in the U.S. for an average of 20.1 years. Among this sample of at-risk children, only about one in four (27.1%) had received any services to address emotional or behavioral problems in the past year. Services received included inpatient (n = 5; 2.7%), outpatient (n = 29; 15.8%), and school-based MHS (n = 32; 17.4%).
The present study includes two data collection points. Child data were collected from classroom surveys (Time 1) and individual interviews (Time 2), with Time 1 and Time 2 occurring an average of 2.9 months (SD = 2.2) or 102.6 days (SD = 64.1) apart. A total of 1249 children were surveyed at Time 1. Using data from Time 1, children at-risk for depression were oversampled and recruited for an individual interview in Time 2, in part to help identify those who would be more likely to be eligible for a later intervention. Out of 313 children interviewed at Time 2, 184 children (58.5%) reported elevated depressive symptoms at both time points. Chronically at-risk children were identified as those who scored 9 or greater on the Children’s Depression Inventory (CDI; Kovacs 1992) across both administrations. Previous work with at-risk children and early adolescents has demonstrated that they score at or above this threshold (Jaycox et al. 1994; Gillham et al. 1995; Hannan et al. 2000). At Time 1, children in the chronically at-risk sample had a mean CDI score of 19.0 (SD = 6.7). Based on established guidelines (Kovacs 1992; Rivera et al. 2005), the majority endorsed moderate (i.e., score of 13–18; n = 70; 38.0%) or severe (i.e., score of 19 or above; n = 84; 45.7%) depressive symptoms. At time 2, these same children had a mean CDI score of 16.4 (SD = 6.8), and the majority endorsed moderate (n = 59; 32.1%) or severe (n = 55; 29.9%) depressive symptoms. Compared to children not chronically at-risk, children in the chronic risk group were made up of a higher proportion of females (63.6%), X 2 (1, N = 313) = 4.20, p < 0.05, but did not significantly differ on any other demographic characteristics. All subsequent study analyses are conducted only with the chronic risk children.
Measures
Children’s Depression Inventory (CDI; Kovacs 1992)
The CDI is a widely used 27-item self-report measure of cognitive, affective, and behavioral depressive symptoms in children. For each item, children choose one of three sentences that describes how they have felt in the previous two weeks (e.g., “I feel like crying every day”, “I feel like crying most days”, “I feel like crying once in a while”). One item evaluating suicidal ideation was omitted. In the present study, the CDI was administered at two time points, once during the in-class survey (Time 1) and again during the in-person interview (Time 2), and serves as the indicator of chronicity of child depressive symptoms. The CDI demonstrated adequate internal consistency at Time 1 (α = 0.77) and Time 2 (α = 0.90).
Diagnostic Interview Schedule for Children (DISC; Costello et al. 1984)
Diagnostic depressive symptoms were assessed using the DISC, a structured interview used to diagnose children consistent with criteria from the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association 2013). The DISC can be administered by trained lay interviewers. Parents and children were administered parallel versions of the MDD module, which includes questions assessing the presence of three core symptoms (DSM-5 diagnostic Criterion A1), including depressed mood, diminished interest/anhedonia, and irritability, and 18 secondary symptoms (DSM-5 diagnostic Criteria A2 to A9) such as insomnia/hypersomnia, feelings of worthlessness, and indecisiveness. In the present study, parent and child reports of the core depressive symptoms are used in LCA to determine levels of endorsement and agreement across informants.
Child Behavior Checklist (CBCL; Achenbach and Rescorla 2001)
The 35-item externalizing broadband scale of the CBCL was used to assess externalizing problems in children. Parents rated whether items such as “Gets in many fights” were true of their child in the past 6 months on a scale with anchors of 0 (not at all true), 1 (somewhat or sometimes true), and 2 (very true or often true). The CBCL has demonstrated high test-retest reliability and validity among both English- (Achenbach and Rescorla 2001) and Spanish-speaking samples (Rubio-Stipec et al. 1990), and demonstrated high internal consistency (α = 0.89).
Service Assessment for Children and Adolescents (SACA; Horwitz et al. 2001)
The SACA was administered to parents to assess for child past-year MHS use, including inpatient, outpatient, and school-based services. The parent version of the SACA has demonstrated fair to excellent validity when compared to actual service use (Hoagwood et al., 2000), and high test-retest reliability among both English- and Spanish-speaking samples (Horwitz et al. 2001; Bean et al. 2003).
Center for Epidemiologic Studies Depression Scale (CES-D; Radloff 1977)
The CES-D is a 20-item measure that assesses the frequency of depressive symptoms. Parents rated items such as “I felt like everything I did was an effort” on a scale ranging from 0 (rarely or none of the time) to 4 (almost or all of the time). Reliability and validity of the English and Spanish versions of CES-D have been established in both community and clinical samples (Radloff 1977; Roberts 1992). The CES-D demonstrated high internal consistency (α = 0.90).
Demographics
Children responded to items about their age, sex, race/ethnicity, and country of origin. Parents also responded to items about their race/ethnicity, family income, country of origin, length of time living in the U.S. (when applicable), and educational attainment. Parents indicated their highest level of education using categories from 1 (never went to school) to 8 (training beyond 4-year college) and their household income using categories from 1 ($5000 to $10,000) to 8 ($100,000 and up).
Procedure
Parents first learned about the study through a consent form sent home to request their child’s participation in a classroom survey. Parental consent and student assent were obtained for the student survey (Time 1). Parents of children who completed the survey were contacted by phone and recruited to participate in individual interviews (Time 2), after separately obtaining parental consent and student assent for this phase of the study. Parent and child interviews were conducted simultaneously and in separate rooms. A majority of parents (51.6%) were interviewed in Spanish, and all but one child was interviewed in English. Parents received a cash incentive and children received a gift card for their participation. Study procedures were reviewed and approved by DePaul University’s Institutional Review Board as well as by the local school district’s Research Review Board.
Results
Endorsement Levels Across Symptoms
Paired sample t-tests were conducted to determine whether endorsement levels of DSM-5 core and secondary depressive symptoms significantly differed by informant. As predicted, children endorsed significantly more core depressive symptoms (M = 1.79; SD = 0.96) than their parents (M = 1.24; SD = 1.07), t(183) = 5.67, p < 0.001. Also as predicted, children endorsed significantly more secondary depressive symptoms (M = 7.77; SD = 3.11) than their parents (M = 2.86; SD = 2.99), t(183) = 16.31, p < 0.001.
Differences in the proportion of children and parents endorsing each of the three core depressive symptoms were examined using McNemar chi-square tests. Children were significantly more likely than their parents to endorse depressed mood (53.8% versus 43.5%; χ2 = 4.21, p < 0.05), anhedonia, (51.1% versus 27.2%; χ2 = 21.01, p < 0.001), and irritability, (73.9% versus 53.3%; χ2 = 16.30, p < 0.001) (see Fig. 1).
Parent-Child Endorsement Agreement Classes—Model Selection
Exploratory LCA were conducted using Mplus Version 7.1 (Muthén and Muthén 2013). A total of six observed indicators were entered into the model, which included child and parent report of the three DSM-5 core depressive symptoms (i.e., depressed mood, anhedonia, irritability). Absolute and relative fit of latent models were evaluated using several evaluation fit criteria including the Bayesian Information Criterion (BIC), Akaike Information Criterion (AIC), Bootstrapped Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (BLMR-LR), and entropy index.
Results indicated that a three-class solution provided the best fit to the data (see Fig. 2) and that the model did not show any further improvement in evaluation criteria with the addition of a fourth class (see Table 1). The three-class solution had a lower AIC value than a two-class solution as well as satisfactory entropy. The BLMR-LR was significant for the three-class solution, indicating that three classes provided a significantly better fit to the data than did two classes. The three-class solution also provided optimal theoretical utility, as it captured parent-child dyads with a low probability of endorsement of any core depressive symptoms, while these dyads were contained within another class in the two-class solution. A core MDD symptom was considered to have a high versus low probability of endorsement if informants had a higher or lower than 50% probability of endorsing the symptom.
Class 1, labeled Low Endorsement and High Agreement (LH) (n = 64; 34.8%), is a class characterized by a relatively low probability of child and parent endorsement of depressed mood or anhedonia, but a moderate likelihood of child and parent endorsement of irritability.
Class 2, labeled High Endorsement and High Agreement (HH) (n = 68; 37.0%), is a class characterized by a relatively high probability of symptom endorsement by both children and parents. The probability of parent-child endorsement of anhedonia and irritability was comparably high, and parents had a 100% probability of endorsing depressed mood while children were very likely to endorse this symptom.
Class 3, labeled High Child Endorsement and Low Agreement (HCL) (n = 52; 28.3%), is a class characterized by relatively high probability of child endorsement and low probability of parent endorsement across all three core depressive symptoms. Children had a 100% probability of endorsing depressed mood and were very likely to endorse anhedonia and irritability. In contrast, parents were very unlikely to endorse depressed mood, anhedonia, or irritability.
Predictors of Class Membership
Multinomial logistic regressions were conducted to examine clinical and sociodemographic predictors of endorsement agreement classes. Dummy codes were used for past year MHS use (Use = 1, No Use = 2), ethnicity (Latino = 1, Non-Latino = 2), gender (Male = 1, Female = 2), and parent interview language (English = 1, Spanish = 2). The HCL class was selected as the reference group for all regressions, which allowed for the comparison between the HCL and HH class and the elucidation of factors associated with parental under-reporting of child depressive symptoms.
Clinical Predictors
When entered independently, parental endorsement of child externalizing problems, [LR χ2 (2, N = 183) = 29.16, p < 0.001]; and past year MHS use, [LR χ2 (2, N = 183) = 11.48, p < 0.01], emerged as significant predictors of class membership, while parental depressive symptoms did not, [LR χ2 (2, N = 183) = 5.10, p = 0.08]. Comparisons among classes are reported for all three of these predictors. Higher odds of belonging to the HH class, relative to the HCL class, were found among children with higher externalizing problems, (OR = 8.67, p < 0.001), and past year MHS use history (OR = 2.33, p < 0.05). Dyad membership to the LH class, relative to the HCL class, was not found to be associated with externalizing problems (OR = 0.93, p = 0.86), or past year MHS use (OR = 0.62, p = 0.31). Finally, parental depressive symptoms were not associated with dyad membership in the HCL class relative to the LH class (OR = 0.62, p = 0.35) or HH class (OR = 1.64, p = 0.25).
When clinical predictors were entered in the combined predictors model, only parental endorsement of child externalizing problems, [LR χ2 (2, N = 183) = 18.79, p < 0.001], remained as a significant predictor of class membership. Specifically, higher child externalizing problems were associated with dyad membership in the HH class relative to the HCL class (OR = 7.52, p < 0.001), but did not predict membership in the LH class relative to the HCL class (OR = 1.18, p = 0.73).
Demographic and Sociocultural Predictors
When entered independently, child age, [LR χ2 (2, N = 184) = 4.20, p = 0.12]; child gender, [LR χ2 (2, N = 184) = 0.76, p = 0.69]; parental education, [LR χ2 (2, N = 184) = 1.17, p = 0.56]; and child ethnicity, [LR χ2 (2, N = 184) = 1.93, p = 0.38], did not emerge as significant predictors of class membership. Parent interview language was the only variable that significantly predicted class membership, [LR χ2 (2, N = 184) = 9.05, p < 0.05]. However, parent language did not significantly predict membership in the HH class (OR = 1.89, p = 0.09) or the LH class (OR = 0.65, p = 0.27), relative to the HCL class.
When demographic and sociocultural predictors were entered in the combined predictors model, parent language remained a significant predictor of class membership, [LR χ2 (2, N = 184) = 11.41, p < 0.01]. Parents interviewed in Spanish were more likely to belong to the HCL class, relative to the LH class (OR = 2.69, p < 0.05), but were not more likely to belong to the HH class, relative to the HCL class (OR = 0.74, p = 0.49).
Discussion
Consistent with previous research on informant discrepancies in non-clinical and ethnic minority samples (Barker et al. 2007; Dirks et al. 2014), the present study found that, relative to their parents, children were more likely to endorse the three core symptoms of DSM-5 criteria for MDD, including depressed mood, anhedonia, and irritability. The same pattern was found for secondary symptoms such as weight and appetite changes, sleep disturbances, and concentration difficulties. This pattern emerged in a sample of children identified based on chronic and elevated self-reports of depressive symptoms using an independent measure, underscoring that significant parental under-reporting is present even among children who are consistently experiencing depressive symptoms.
Using LCA, the present study uncovered patterns of parent-child endorsement of core depressive symptoms. This analytic approach addressed limitations in discrepancies research by eliminating the statistical problems with the difference score approach. LCA revealed three classes of parent-child endorsement with unique patterns and each representing a substantial portion of the sample. The LH and HH classes were characterized by high parent-child agreement and, respectively, by relatively low and high probability of endorsement. In contrast, over one in four dyads were classified as belonging to the HCL class, in which parent-child endorsement disagreement was present. This class was characterized by a relatively high probability of child endorsement and low probability of parent endorsement across all three core depressive symptoms.
The HCL class was identified using a sample of children that has received limited attention in discrepancies research. Discrepancies research has primarily focused on clinical samples of children with externalizing concerns, and less is known about patterns derived from samples of ethnic minority and low-income children at risk for depression in community settings. Clinical samples are typically characterized by parental over-reporting of child emotional and behavioral problems—which are more often misconduct and other externalizing problems—relative to children themselves (Rescorla et al. 2017). However, the present study found that depressive symptoms are under-detected for a large group of children in community settings. This underscores that, although multiple informants are key in evidence-based assessment of child psychopathology (Hunsley and Mash 2007), outreach to children themselves is critical and over-reliance on parental reports of child depressive symptoms should be avoided. This is an important finding, as best practices for integrating and interpreting multi-informant reports in evidence-based assessment have yet to be established (De Los Reyes et al. 2015; Youngstrom and Van Meter 2016).
A class characterized by parental over-reporting of child depressive symptoms was not identified, which is in sharp contrast with a number of previous studies conducted primarily in clinical settings and when focusing on child externalizing problems (e.g., Martin et al. 2004). This is due, at least in part, to the fact that depressive symptoms were the focus of the study, the sample was drawn from schools rather than clinics, and families were selected based on chronicity of depressive symptoms as determined by child self-reports. Although the study was strengthened by the use of child self-report across two time points, future work should evaluate independent indicators of depression (e.g., behavioral observations, psychophysiology; Nelson et al. 2017) as they relate to parent-child endorsement agreement.
Clinical Factors
To our knowledge, the present study is the first to investigate whether co-occurring externalizing problems are associated with parent-child endorsement patterns in ratings of child internalizing problems. As parental reports of externalizing problems increased, dyads were much more likely to belong to the HH class relative the HCL class, in which parents underreported depressive symptoms (including irritability) relative to their children. This suggests that parents may be more likely to detect or report depressive symptoms among those children who are also manifesting externalizing behaviors such as misconduct or aggression. It may also be that parents endorsing both high levels of internalizing and externalizing problems are more willing to report child mental problems in general, either due to increased recognition or lower levels of perceived stigma. Finally, it is important to note that parents reported on both their child’s depressive symptoms and externalizing problems. As a result, these associations may be due at least in part to shared method variance among parent reports. To address this possibility, future work should examine the association between independent observations of child internalizing and externalizing problems (e.g., teacher reports, behavioral observations; De Los Reyes et al. 2009) and parent-child agreement in reports of child depressive symptoms to determine the impact that co-occurring externalizing problems have on parental recognition of child depressive symptoms.
Past year MHS use was associated with HH class membership, but only when considered independently and not in the presence of other clinical predictors. Given that externalizing problems are more likely to lead to mental health treatment (Gudiño et al. 2008), their presence may have initiated MHS use for children in the present sample and explained the lack of significance of MHS use when entered in the combined clinical model. This finding reiterates that children with chronic depressive symptoms without a history of receiving MHS are more likely to have parents who under-report their symptoms, suggesting that lack of parental awareness of the child’s distress may impede access to services. In this school-based sample of children reporting chronically elevated depressive symptoms, only approximately one in four received past-year inpatient, outpatient, or school-based MHS. This pattern is consistent with previous research demonstrating that low-income ethnic minority children are among the least likely to receive treatment (Gudiño et al. 2009). In addition to parental under-recognition, barriers such as low availability of providers, lack of income or insurance, and perceived stigma may have prevented parents from obtaining MHS for their child (Garland et al. 2013).
The finding that a substantial proportion of children with chronic and elevated symptoms are likely to have parents who are either unaware or underestimate their mood problems raises important questions regarding the longitudinal course for children with undetected and prolonged distress. Future work should determine the trajectory of symptoms, levels of impairment, and MHS use among HCL children. These children may experience significant functional impairment and be at increased risk for developing maladaptive responses that are more likely to receive attention from adults and initiate MHS (e.g., conduct problems; Gudiño et al. 2008; Rescorla et al. 2017). Their problems with depression, including subthreshold symptoms, may also take a severe course, resulting in increased suicidality and rates of hospitalization over time (Klein et al. 2009).
Although the depression-distortion hypothesis has received support in the literature (De Los Reyes and Kazdin 2005), parental depressive symptoms did not predict endorsement agreement classes in the present study. This is consistent with recent mixed findings in studies evaluating depression as a bias of parental reporting (Affrunti and Woodruff-Borden 2015; Lewis et al. 2012). Overall, these findings suggest that bias due to psychological distress may be less prevalent in community samples. Parental depressive symptoms may contribute to the initiation of MHS for children in clinical samples, where parents tend to report higher levels of child depressive symptoms than their child, and particularly when parents self-report elevated depressive symptoms (Youngstrom et al. 2000). Another possibility is that parental depressive symptoms in clinical samples are higher and that parents in community samples may not be as likely to misinterpret child behaviors as problematic. Given that a predictor of discrepancies that has received support in the literature was not associated with endorsement agreement classes, future work should evaluate parental depressive symptoms and other established predictors using alternative methods that address the limitations of previous findings obtained using difference scores.
Demographic and Sociocultural Factors
The present study is among the first in discrepancies research to utilize a sample comprised primarily of Latino children, a group at heightened risk for depression that has received limited attention in discrepancies research. The study is also the first to examine ethnicity, SES, language, and informant discrepancies within the same sample. Previous research has demonstrated that, relative to European American parents, ethnic minority parents are more likely to under-report child mental health problems relative to child self-report (Lau et al. 2004; Roberts et al. 2005). However, consistent with Dirks and colleagues’ (2014) finding that almost one fourth (22%) of African American children in their sample reported clinically significant anxiety that their parents did not, the present study found that a comparably large portion of the sample was characterized by lower parent than child report. Given that difference scores examine sample-level discrepancies, they yield the conclusion that ethnic minority and low-income families under-report their child’s depressive symptoms. LCA was an optimal analytic approach because it revealed that most parent-child reports converged, suggesting that previous studies with ethnic minority and low-income families may also be characterized by comparably high levels of agreement.
There was evidence that parents interviewed in Spanish were more likely to under-report child symptoms. Language may impact discrepancies directly as an artifact, causing assessment questions to be interpreted discordantly due to differences in concepts inherent to language translation. Even so, the DISC has been validated for use with both English- and Spanish-speaking populations (Shaffer et al., 2000; Bravo et al., 2001). Alternatively, discrepancies may stem from language-based communication difficulties between predominately U.S.-born children, and their predominately foreign-born parents. Parental language may also serve as a proxy for cultural differences, which impact parental perception of child mental health problems (Weisz et al. 1987). Thus, parents and children in these families may be most likely to show disagreement in their endorsement of child depressive symptoms because they view them through different cultural lenses. Foreign-born and Spanish-speaking parents may also have less exposure to Western conceptions of child mental health, and may be less likely than children, who have greater U.S. exposure, to recognize indicators of a mental health problem (Rescorla et al. 2017). Finally, even when recognizing their child’s depressive symptoms, these parents may be less likely to disclose their child’s problems because of stigma. Previous research has shown that depressed low-income Latino immigrants are more likely to perceive stigma about depression than adults from other ethnic groups, and when doing so, are less likely to disclose their mental health problem or initiate treatment (Vega et al. 2010).
A limitation of the present study is that language dominance was assumed based on parents’ interview language. The study did not account for fluent bilingual parents, who are dominant in both English and Spanish, and future research should incorporate indicators of proficiency in both languages as predictors. More research in this area is needed to address the intersection between culture, ethnicity, and informant discrepancies. Future studies should focus on additional ethnic/racial comparisons and more direct assessment of cultural variables (e.g., familism) and parent-child cultural conflicts.
More generally, the findings in this study have implications for early detection and intervention for children with mental health problems. In particular, children with undetected depressive symptoms, such as those in the HCL class, are a crucial group to target, and psychoeducation and school-based programs could help raise teacher and parental awareness. Similarly, school-based services should include efforts to evaluate and focus on depression, even among children who present with or are referred due to misconduct and academic difficulties.
References
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles. Burlington: University of Vermont, Research Center for Children, Youth, & Families.
Achenbach, T. M., McConaughy, S. H., & Howell, C. T. (1987). Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychological Bulletin, 101, 213–232. https://doi.org/10.1037/0033-2909.101.2.213.
Affrunti, N. W., & Woodruff-Borden, J. (2015). The effect of maternal psychopathology on parent–child agreement of child anxiety symptoms: a hierarchical linear modeling approach. Journal of Anxiety Disorders, 32, 56–65. https://doi.org/10.1016/j.janxdis.2015.03.010.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Barker, E. T., Bornstein, M. H., Putnick, D. L., Hendricks, C., & Suwalsky, J. D. (2007). Adolescent-mother agreement about adolescent problem behaviors: direction and predictors of disagreement. Journal of Youth and Adolescence, 36, 950–962. https://doi.org/10.1080/00224490902954315.
Bean, D. L., Rotheram-Borus, M. J., Leibowitz, A., Horwitz, S. M., & Weidmer, B. (2003). Spanish-language services assessment for children and adolescents (SACA): reliability of parent and adolescent reports. Journal of the American Academy of Child & Adolescent Psychiatry, 42(2), 241–248. https://doi.org/10.1097/00004583-200302000-00019.
Bravo, M., Ribera, J., Rubio-Stipec, M., Canino, G., Shrout, P., Ramírez, R., ... & Taboas, A. M. (2001). Testretest reliability of the Spanish version of the Diagnostic Interview Schedule for Children (DISC-IV). Journal of Abnormal Child Psychology, 29(5), 433–444.
Breland-Noble, A., & Weller, B. (2012). Examining African American adolescent depression in a community sample: the impact of parent/child agreement. Journal of Child and Family Studies, 21(5), 869–876. https://doi.org/10.1007/s10826-011-9547-z.
Costello, E. J., Edelbrock, C., Dulcan, M. K., Kalas, R., & Klarich, S. (1984). Report on the NIMH Diagnostic Interview Schedule for Children (DISC). Washington, DC: National Institute of Mental Health.
Cummings, J. R., & Druss, B. G. (2011). Racial/ethnic differences in mental health service use among adolescents with major depression. Journal of the American Academy of Child & Adolescent Psychiatry, 50(2), 160–170. https://doi.org/10.1016/j.jaac.2010.11.004.
De Los Reyes, A., & Kazdin, A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509. https://doi.org/10.1037/0033-2909.131.4.483.
De Los Reyes, A., Henry, D. B., Tolan, P. H., & Wakschlag, L. S. (2009). Linking informant discrepancies to observed variations in young children’s disruptive behavior. Journal of Abnormal Child Psychology, 37(5), 637–652. https://doi.org/10.1007/s10802-009-9307-3.
De Los Reyes, A., Augenstein, T. M., Wang, M., Thomas, S. A., Drabick, D. A., Burgers, D. E., & Rabinowitz, J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141, 858–900. https://doi.org/10.1037/a0038498.
Dirks, M. A., Weersing, V. R., Warnick, E., Gonzalez, A., Alton, M., Dauser, C., … Woolston, J. (2014). Parent and youth report of youth anxiety: evidence for measurement invariance. Journal of Child Psychology and Psychiatry, 55(3), 284–291. https://doi.org/10.1111/jcpp.12159.
Federal Interagency Forum on Child and Family Statistics (2015). American’s children: key national indicators of well-being, 2015. Retrieved from http://childstats.gov/americaschildren/index.asp.
Garland, A. F., Haine-Schlagel, R., Brookman-Frazee, L., Baker-Ericzen, M., Trask, E., & Fawley-King, K. (2013). Improving community-based mental health care for children: translating knowledge into action. Administration and Policy in Mental Health and Mental Health Services Research, 40(1), 6–22. https://doi.org/10.1007/s10488-012-0450-8.
Gartstein, M. A., Bridgett, D. J., Dishion, T. J., & Kaufman, N. K. (2009). Depressed mood and maternal report of child behavior problems: another look at the depression–distortion hypothesis. Journal of Applied Developmental Psychology, 30(2), 149–160. https://doi.org/10.1016/j.appdev.2008.12.001.
Gillham, J. E., Reivich, K. J., Jaycox, L. H., & Seligman, M. E. (1995). Prevention of depressive symptoms in schoolchildren: two-year follow-up. Psychological Science, 6(6), 343–351. https://doi.org/10.1111/j.1467-9280.1995.tb00524.x.
Grills, A. E., & Ollendick, T. H. (2003). Multiple informant agreement and the anxiety disorders interview schedule for parents and children. Journal of the American Academy of Child & Adolescent Psychiatry, 42(1), 30–40. https://doi.org/10.1097/00004583-200301000-00008.
Gudiño, O. G., Lau, A. S., & Hough, R. L. (2008). Immigrant status, mental health need, and mental health service utilization among high-risk Hispanic and Asian Pacific islander youth. Child & Youth Care Forum, 37(3), 139–152. https://doi.org/10.1007/s10566-008-9056-4.
Gudiño, O. G., Lau, A. S., Yeh, M., McCabe, K. M., & Hough, R. L. (2009). Understanding racial/ethnic disparities in youth mental health services: do disparities vary by problem type? Journal of Emotional and Behavioral Disorders, 17, 3–16. https://doi.org/10.1177/1063426608317710.
Hannan, A. P., Rapee, R. M., & Hudson, J. L. (2000). The prevention of depression in children: a pilot study. Behaviour Change, 17(2), 78–83. https://doi.org/10.1375/bech.17.2.78.
Hoagwood, K., Horwitz, S., Stiffman, A., Weisz, J., Bean, D., Rae, D., Compton, W., Cottler, L., Bickman, L., & Leaf, P. (2000). Concordance between parent reports of children's mental health services and service records: The Services Assessment for Children and Adolescents (SACA). Journal of Child and Family Studies, 9(3), 315–331. https://doi.org/10.1023/A:1026492423273.
Horwitz, S. M., Hoagwood, K., Stiffman, A. R., Summerfeld, T., Weisz, J. R., Costello, E. J., … Norquist, G. (2001). Reliability of the services assessment for children and adolescents. Psychiatric Services, 52(8), 1088–1094. https://doi.org/10.1176/appi.ps.52.8.1088.
Hunsley, J., & Mash, E. J. (2007). Evidence-based assessment. Annual Review of Clinical Psychology, 3, 29–51. https://doi.org/10.1146/annurev.clinpsy.3.022806.091419.
Jaycox, L. H., Reivich, K. J., Gillham, J., & Seligman, M. E. (1994). Prevention of depressive symptoms in school children. Behaviour Research and Therapy, 32(8), 801–816.
Jaycox, L. H., Stein, B. D., Paddock, S., Miles, J. V., Chandra, A., Meredith, L. S., … Burnam, M. A. (2009). Impact of teen depression on academic, social, and physical functioning. Pediatrics, 124(4), e596–e605. https://doi.org/10.1542/peds.2008-3348.
Klein, D. N., Shankman, S. A., Lewinsohn, P. M., & Seeley, J. R. (2009). Subthreshold depressive disorder in adolescents: predictors of escalation to full-syndrome depressive disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 48(7), 703–710. https://doi.org/10.1097/CHI.0b013e3181a56606.
Kovacs, M. (1992). Children’s depression inventory. New York: Multi-Health Systems.
Laird, R. D., & De Los Reyes, A. (2013). Testing informant discrepancies as predictors of early adolescent psychopathology: why difference scores cannot tell you what you want to know and how polynomial regression may. Journal of Abnormal Child Psychology, 41(1), 1–14. https://doi.org/10.1007/s10802-012-9659-y.
Lau, A. S., Garland, A. F., Yeh, M., McCabe, K. M., Wood, P. A., & Hough, R. L. (2004). Race/ethnicity and inter-informant agreement in assessing adolescent psychopathology. Journal of Emotional and Behavioral Disorders, 12(3), 145–156. https://doi.org/10.1177/10634266040120030201.
Lerner, M. D., De Los Reyes, A., Drabick, D. A. G., Gerber, A. H., & Gadow, K. D. (2017). Informant discrepancy defines discrete, clinically-useful autism spectrum disorder subgroups. Journal of Child Psychology and Psychiatry, 58(7), 829–839. https://doi.org/10.1111/jcpp.12730.
Lewis, K. J., Mars, B., Lewis, G., Rice, F., Sellers, R., Thapar, A. K., … Thapar, A. (2012). Do parents know best? Parent-reported vs. child-reported depression symptoms as predictors of future child mood disorder in a high-risk sample. Journal of Affective Disorders, 141(2), 233–236. https://doi.org/10.1016/j.jad.2012.03.008.
Martin, J. L., Ford, C. B., Dyer-Friedman, J., Tang, J., & Huffman, L. C. (2004). Patterns of agreement between parent and child ratings of emotional and behavioral problems in an outpatient clinical setting: when children endorse more problems. Journal of Developmental and Behavioral Pediatrics, 25(3), 150–155. https://doi.org/10.1097/00004703-200406000-00002.
McCutcheon, A. L. (1987). Latent class analysis. Newbury Park: Sage.
Merikangas, K. R., He, J., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., … Swendsen, J. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. https://doi.org/10.1016/j.jaac.2010.05.017.
Merikangas, K. R., He, J., Burstein, M., Swendsen, J., Avenevoli, S., Case, B., … Olfson, M. (2011). Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCSA). Journal of the American Academy of Child & Adolescent Psychiatry, 50, 32–45. https://doi.org/10.1016/j.jaac.2010.10.006.
Muthén, B., & Muthén, L. (2013). Mplus 7.1. Los Angeles: Muthén & Muthén.
Nelson, B. W., Byrne, M. L., Sheeber, L., & Allen, N. B. (2017). Does context matter? A multi-method assessment of affect in adolescent depression across multiple affective interaction contexts. Clinical Psychological Science, 5(2), 239–258. https://doi.org/10.1177/2167702616680061.
Peña, J. B., Wyman, P. A., Brown, C. H., Matthieu, M. M., Olivares, T. E., Hartel, D., & Zayas, L. H. (2008). Immigration generation status and its association with suicide attempts, substance use, and depressive symptoms among Latino adolescents in the USA. Prevention Science, 9(4), 299–310. https://doi.org/10.1007/s11121-008-0105-x.
Radloff, L. S. (1977). The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306.
Rescorla, L. A., Ewing, G., Ivanova, M. Y., Aebi, M., Bilenberg, N., Dieleman, G. C., … Verhulst, F. C. (2017). Parent–adolescent cross-informant agreement in clinically referred samples: findings from seven societies. Journal of Clinical Child & Adolescent Psychology, 1–14. https://doi.org/10.1080/15374416.2016.1266642.
Richters, J., & Pellegrini, D. S. (1989). Depressed mothers’ judgments about their children: an examination of the depression-distortion hypothesis. Child Development, 60(5), 1068–1075. https://doi.org/10.2307/1130780.
Rivera, C. L., Bernal, G., & Rosselló, J. (2005). The children depression inventory (CDI) and the Beck depression inventory (BDI): their validity as screening measures for major depression in a group of Puerto Rican adolescents. International Journal of Clinical and Health Psychology, 5(3), 485–498.
Roberts, R. E. (1992). Manifestation of depressive symptoms among adolescents: a comparison of Mexican Americans with the majority and other minority populations. Journal of Nervous and Mental Disease, 180(10), 627–633. https://doi.org/10.1097/00005053-199210000-00003.
Roberts, R. E., Alegria, M., Roberts, C. R., & Chen, I. G. (2005). Concordance of reports of mental health functioning by adolescents and their caregivers: a comparison of European, African and Latino Americans. Journal of Nervous and Mental Disease, 193(8), 528–534. https://doi.org/10.1097/01.nmd.0000172597.15314.cb.
Rubio-Stipec, M., Bird, H., Canino, G., & Gould, M. (1990). The internal consistency and concurrent validity of a Spanish translation of the child behavior checklist. Journal of Abnormal Child Psychology, 18(4), 393–406. https://doi.org/10.1007/BF00917642.
Shaffer, D., Fisher, P., Lucas, C. P., Dulcan, M. K., & Schwab-Stone, M. E. (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39(1), 28–38.
Stein, G. L., & Polo, A. J. (2014). Parent-child cultural value gaps and depressive symptoms among Mexican American youth. Journal of Child and Family Studies, 23(2), 189–199. https://doi.org/10.1007/s10826-013-9724-3.
Vega, W. A., Rodriguez, M. A., & Ang, A. (2010). Addressing stigma of depression in Latino primary care patients. General Hospital Psychiatry, 32(2), 182–191. https://doi.org/10.1016/j.genhosppsych.2009.10.008.
Weisz, J. R., Suwanlert, S., Chaiyasit, W., & Walter, B. R. (1987). Over-and undercontrolled problems among Thai and American children and adolescents: the wat and wai of cultural differences. Journal of Consulting and Clinical Psychology, 55, 718–726.
Youngstrom, E. A., & Van Meter, A. (2016). Empirically supported assessment of children and adolescents. Clinical Psychology: Science and Practice, 23(4), 327–347. https://doi.org/10.1111/cpsp.12172.
Youngstrom, E., Loeber, R., & Stouthamer-Loeber, M. (2000). Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. Journal of Consulting and Clinical Psychology, 68, 1038–1050. https://doi.org/10.1037/0022-006X.68.6.1038.
Youngstrom, E. A., Findling, R. L., & Calabrese, J. R. (2004). Effects of adolescent manic symptoms on agreement between youth, parent, and teacher ratings of behavior problems. Journal of Affective Disorders, 82, 5–16. https://doi.org/10.1016/j.jad.2004.05.016.
Funding
This funding was supported in part by the Annie E. Casey Foundation (Grant # 212.0008).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Makol, B.A., Polo, A.J. Parent-Child Endorsement Discrepancies among Youth at Chronic-Risk for Depression. J Abnorm Child Psychol 46, 1077–1088 (2018). https://doi.org/10.1007/s10802-017-0360-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-017-0360-z