Abstract
We compared subjective and objective sleep patterns and problems, and examined cross-method correspondence across parent reports, child reports, and actigraphy-derived sleep variables in clinically-anxious children and healthy controls. In a multi-site, cross-sectional study, 75 pre-adolescent children (6 to 11 years; M = 8.7 years; SD = 1.4; n = 39/52 % female) were examined including 39 with a diagnosis of primary generalized anxiety disorder (GAD) and 36 controls recruited from university-based clinics in Houston, TX and Washington, DC. Structured interviews, validated sleep questionnaires, and 1 week of actigraphy data were utilized. Despite subjective reports of significantly greater sleep problems among anxious children, actigraphy data revealed no significant differences between the groups. All parents estimated earlier bedtimes and greater total sleep duration relative to actigraphy, and all children endorsed more sleep problems than parents. With few exceptions, subjective reports exhibited low and non-significant correspondence with actigraphy-based sleep patterns and problems. Our findings suggest that high rates of sleep complaints found among children with GAD (and their parents) are not corroborated by objective sleep abnormalities, with the exception of marginally prolonged sleep onset latency compared to controls. Objective-subjective sleep discrepancies were observed in both groups but more apparent overall in the GAD group. Frequent complaints of sleep problems and daytime tiredness among anxious youth might more accurately reflect difficulties prior to the actual sleep period, cognitive-affective biases associated with sleep, and/or poor sleep quality. Findings highlight the importance of considering sleep from multiple perspectives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep patterns characterized by appropriate and regimented bedtimes and wake times, positive parent–child interactions, and adequate total sleep duration contribute to healthy development in children (Bordeleau et al. 2012; Iglowstein et al. 2003; McDonald et al. 2014). A considerable proportion of all children experience problems related to sleep but youth who struggle with anxiety are among the most affected (Gregory and O’Connor 2002; Ivanenko et al. 2004; Johnson et al. 2000). Based on parent and child reports at least one type of sleep-related problem, including delayed sleep onset, frequent nighttime awakenings, nightmares, and/or bedtime resistance, affects nearly all (i.e., 90 %) children diagnosed with generalized anxiety disorder (GAD) (Alfano et al. 2006; Alfano et al. 2007; Alfano et al. 2010; Chase and Pincus 2011; Hudson et al. 2009; Reynolds and Alfano 2015). Even among children with other primary forms of psychopathology, the presence of comorbid anxiety is uniquely linked with sleep complaints (Corkum et al. 1999; Mick et al. 2000). Such problems appear to contribute to overall symptom severity and day-to-day impairment experienced by anxious youth (Alfano et al. 2007, 2010; Chase and Pincus 2011).
Despite high rates of sleep complaints, little is known about the actual sleep patterns of anxiety-disordered children (Cowie et al. 2014), even though such data might directly inform sleep intervention approaches. In the only study to examine sleep diary data collected over 1 week, children with anxiety disorders had later bedtimes (by approximately 20 min) and shorter sleep duration (by 30 min) on weekdays than healthy controls (Hudson et al. 2009). Notably, the mean 9.5 h sleep duration found in the anxious group is below the published mean for this age group (i.e., 10 h; Iglowstein et al. 2003). Also, in both groups, average sleep onset latency fell below the suggested 30 min clinical cut-off (Buysse et al. 2006). A study utilizing actigraphy found children and adolescents with anxiety disorders required more time to initiate sleep (i.e., 5 min on average) but spent the same amount of time in bed and asleep as healthy controls (Cousins et al. 2011). Two studies based on polysomnography (PSG) conducted in a sleep laboratory and the home environment provide equivocal results. Youth with GAD evidenced significantly longer sleep onset latency and reduced latency to rapid eye movement (REM) sleep than controls while in the sleep lab (Alfano et al. 2013) but no differences when studied at home (Patriquin et al. 2014). Thus, despite a wealth of evidence for subjective sleep complaints, objective data raise questions about the presence and nature of sleep problems among anxious children.
Children’s sleep can be measured in different ways but the most frequently used method, in both clinic and research settings, is multi-informant subjective reports (e.g., parent reports and child self-reports) (Alfano et al. 2006, 2007, 2010). Despite advantages of low cost and ease of administration, reports of the same phenomena by different informants are often discrepant both from each other as well as objective measures (De Los Reyes and Aldao 2015; De Los Reyes et al. 2012, 2015; De Los Reyes and Kazdin 2005; De Los Reyes et al. 2013b). In community-based samples, parents typically estimate greater total sleep duration and fewer sleep problems relative to both children’s self-reports and actigraphy (Gregory et al. 2006; Robinson and Richdale 2004; Short et al. 2013). In one study including 3-to-10 year old children, parents overestimated their child’s total sleep time by an average of 113 min compared to concurrent actigraphy (Dayyat et al. 2011). Comparisons between child reports and actigraphy reveal a similarly discrepant pattern and child-reported sleep problems such as prolonged sleep onset are often not corroborated by parents (Arora et al. 2013; Short et al. 2012). For example, Short et al. (2013) found parents reported greater total sleep duration on both weekdays and weekends compared to adolescent reports and actigraphy.
In contrast, findings from a number of studies suggest that parents of anxiety-disordered children may overestimate levels of sleep disruption. In one study, 85 % of parents endorsed the presence of a sleep problem compared to only 53 % of children who reported problems sleeping (Alfano et al. 2010). Another study found a small though significant correlation between parent and anxious child reports of sleep problems but overlap between specific types of problems was minimal (Chase and Pincus 2011). Similar discrepancies have been found following behavioral intervention. In a pilot study, children with GAD but not parents reported significant sleep-based improvements following a 14-week treatment program targeting both anxiety and sleep (Clementi and Alfano 2014). Still, absent from the literature are direct comparisons of subjective and objective sleep measures in anxious children. One study found parents of preschoolers with severe nighttime fears to provide sleep estimates more concordant with actigraphy than parents of non-fearful preschoolers (Kushnir and Sadeh 2013), but parents are typically less involved in school-aged children’s sleep routines. Another study examined associations between parent-reported and objective sleep problems in a sample of youth with and without anxiety disorders (Gregory et al. 2011). However, cross-method concordance was not investigated for clinical and non-clinical youth separately.
Purpose and Hypotheses
Examination of cross-method correspondence across sleep measures can inform decisions regarding the most reliable assessment and treatment approaches for different populations of youth. The current study therefore had two primary aims. First, to obtain a better understanding of whether and how the sleep patterns and problems of school-aged children (6 to 11 years) with GAD differ from those of healthy children, we compared parent and child sleep reports as well as 1 week of actigraphy data between the groups. In line with previous research, we expected to find higher rates of total sleep problems based on both subjective reports and later bedtimes and longer sleep onset latency based on actigraphy in the GAD group. Second, to understand the extent to which cross-method correspondence exists for sleep patterns and problems within these groups, we examined agreement/discrepancy across sleep measures. With regard to sleep patterns, we expected parents in the control group to overestimate total sleep duration compared to actigraphy and parents of anxious youth to underestimate total sleep. For child sleep problems, variables derived from actigraphy included bedtime consistency, sleep onset latency, total sleep duration, and number of nighttime awakenings. We expected parents of anxious children to report greater levels of sleep problems than children but the reverse pattern in control families (i.e., children would endorse more sleep problems than parents). We expected similar outcomes for subjective-objective correspondence of sleep problems; specifically, that parents of control children would underestimate sleep problems compared to actigraphy whereas parents of anxious youth would overestimate sleep problems.
Method
Participants
Eighty-four children (6 to 11 years; 39/52 % female) including 44 children with a primary diagnosis of GAD and 40 healthy controls participated in the current study. Community flyers and print advertisements were used to recruit children in both groups. Children were recruited in 2 large metropolitan areas: Houston, TX (n = 41) and Washington, DC (n = 43). All participants resided with a parent/primary caretaker and were enrolled in a regular classroom setting. Exclusion criteria included: (a) current/lifetime history of psychotic, pervasive developmental, mood/bipolar, substance abuse, tic, eating, or conduct disorder; (b) present use of treatment services for emotional, behavioral, or sleep problems; (c) use of any medications known to impact sleep (e.g., anti-histamines, melatonin); (d) chronic medical illness; and (e) full scale IQ < 80. Additionally, control group participants could not meet criteria for any psychiatric or sleep disorders in order to be eligible for participation.
After an initial phone screen, a total of 55 children with significant symptoms of anxiety were evaluated to participate. However, 11 children were found ineligible at the initial assessment due to the presence of other primary disorders (n = 7), suspected/confirmed sleep-disordered breathing (n = 2), or IQ < 80 (n = 2). Of the 44 anxious children who completed the study, data were excluded for five participants due to the use of melatonin (n = 1), a stressful life event (parent was hospitalized during the actigraphy week; n = 1), physical illness (n = 1), or equipment error (n = 2), resulting in a final sample of 39 children with GAD. Children in the control group were administered the same assessment procedures as children in the GAD group, including diagnostic interviews and sleep assessments.
Among the 40 healthy control children who participated, adequate actigraphy data were missing for 4 participants, resulting in a final sample of 36 controls. Across the entire sample (N = 84) we compared those with missing or invalid/excluded actigraphy data (n = 5 with GAD; n = 4 controls) to those children in the final sample (n = 75) on all demographic variables (Table 1). No significant differences were found for any variables. Similarly, as seen in Table 1, the final GAD (n = 39) and control (n = 36) groups did not significantly differ on any demographic variables, body mass index (BMI) or pubertal development. There were no differences in any demographic or clinical variables across the 2 data collection sites.
Procedure
The study protocol was approved by appropriate Institutional Review Boards. Parents and children were required to sign consent/assent forms and were given a copy of the forms. Consenting families included all biological mothers with the exceptions of one adoptive mother and two biological fathers. After completing an initial evaluation that included interviews, questionnaires, calculation of BMI, and IQ testing (Weschler 1983), all children wore an actigraph on their non-dominant wrist during a continuous 7 day period. Further, all children (together with their parent) kept a sleep log during the same 1 week period to verify actigraphy data. The week of actigraphy was completed within 2 weeks of the evaluation in order to minimize the possibility of any significant changes in baseline symptoms and/or functioning.
Measures
Structured Interviews
The Anxiety Disorders Interview Schedule for DSM-IV – Child and Parent Versions (ADIS-C/P; Silverman and Albano 1996) was used to determine diagnoses. The ADIS-C/P is a well-validated measure for assessing child anxiety (Silverman et al. 2001). A Ph.D. level psychologist or trained doctoral level graduate student administered the ADIS-C/P separately to the child and parent. All cases were reviewed with a licensed clinical psychologist prior to assigning final diagnoses. ADIS-C/P clinician severity ratings (CSR; range 0–8) are used to categorize disorders as primary (most severe/disabling) or secondary. Reliability for a GAD diagnosis was excellent, kappa = 1.0 (Cohen 1960; Fleiss 1981). Within the GAD group, 18 (46.2 %) participants had secondary diagnoses including social anxiety disorder (n = 9), separation anxiety disorder (n = 5), attention-deficit/hyperactivity disorder (n = 2), specific phobia (n = 1), and oppositional defiant disorder (n = 1).
Pubertal Development
The Pubertal Development Scale (PDS; Carskadon and Acebo 1993) was used to assess pubertal development. A score of 3 or below is interpreted as pre-pubertal status in both boys and girls. PDS scores in the current sample were all below 3.3, range = 1.0 to 3.2; M = 1.5, SD = 0.51.
Parent Report of Child Sleep
The Children’s Sleep Habits Questionnaire (CSHQ; Owens et al. 2000a) is a 33-item parent-report measure of child sleep patterns and problems that yields a total sleep problem score as well as eight subscale scores. Parents respond to questions regarding different types of sleep behaviors and problems that occurred during the past week (e.g., bedtime resistance, sleep-disordered breathing, daytime sleepiness, etc.) using on a three-point scale; 1 = rarely, 2 = sometimes, 3 = usually. Parents are also asked to provide numerical estimates of their child’s 1) bedtime, 2) total sleep duration, and 2) wake-up time. For the current study, these sleep pattern estimates were examined in comparison with corresponding actigraphy-based estimates across a 1 week period.
In order to directly compare parent and child report of sleep problems, we constrained total parent CSHQ scores to contain the same number of items included on a child self-report sleep measure developed by the same authors (i.e., Sleep Self Report; Owens et al. 2000b). To ensure the parallel nature of the parent and child scales, the modified parent measure purposely did not included any items assessing sleep behaviors that would conceivably occur while the child was asleep/outside of the child’s awareness (e.g., “Child talks during sleep”). Thus, we reduced methodological differences between the CSHQ and SSR based on both the number of the items and specific phenomena of interest. Finally, we also examined concordance among parent and child-reports of four unique CSHQ and SSR-assessed sleep problems (i.e., bedtime consistency, sleep onset latency > 20 min, sleeps too little, and wakes up at night) and corresponding actigraphy variables.
We implemented pro-rated mean replacement of missing items on the CSHQ for three participants. One participant had all CSHQ item data missing and another had over half of their item data missing. For these two participants, their item scores were based on sample mean-replacement (i.e., each item replaced with sample’s mean item score for all items). The CSHQ has adequate internal consistency and reliability in both clinical and community samples of children (Owens et al. 2000a). In the current sample, we observed adequate internal consistency estimates for the 23-item scale used, α = 0.84.
Child Sleep Self-Report
The Sleep Self Report (SSR; Owens et al. 2000b) is a 26-item self-report measure of sleep problems in school-aged children. It yields a total sleep problems scores. Only 23 items (as described above) were used in the current study. We implemented pro-rated mean replacement of missing items of the SSR for six participants. The SSR has demonstrated good internal consistency and reliability (Owens et al. 2000b). We observed adequate internal consistency for the 23-item SSR scale used, α = 0.73.
Actigraphy
The Micro Motionlogger Sleep Watch (Ambulatory Monitoring, Inc., Ardsley, NY, USA) was used to provide an objective measure of children’s sleep. The watch is an accelerometer-based sleep monitor that records movement continuously for up to 1 month. Data were stored by the unit until downloaded to a computer. Data were collected in 1 min epochs (sensitivity of 0.05 g in a frequency range of 2 to 3 Hz) using the zero crossing mode and scored using the Sadeh algorithm (Sadeh et al. 1994). Prior to analyzing data they were visually inspected to ensure that epochs where the watch had been removed were omitted. Participants pressed an event marker on the watch when they got into bed at night and when they got out of bed in the morning. To ensure accurate assessment of sleep onset latency, this variable was not calculated for any nights where the event button was not used. Sleep logs were collected in conjunction with actigraphy as an additional means of ensuring the validity of objective sleep data. Actigraphy has an accuracy of 88–93 % and sensitivity of 90–95 % relative to polysomnography (Meltzer et al. 2012a; Meltzer et al. 2012b; Sadeh et al. 1994). Consistent with previous reliability studies, participants were required to have a minimum of 5 nights of valid actigraphy data to be included in analyses (Sadeh 1996). Adequate actigraphy data were missing for four participants.
We examined actigraphy for mean bedtime, bedtime consistency (i.e., SD of nightly bedtimes), total time in bed, total sleep duration, sleep onset latency (i.e., the first contiguous 20 min block of sleep after lights out), number of nighttime awakenings, and wake-up time. We defined time in bed as lights out to lights on, and total sleep duration as the total number of minutes from sleep onset to wake-up time. We measured sleep onset in minutes from the time the event button was pressed (i.e., lights out) to sleep onset, defined automatically as the first 20 min block with > 19 min of sleep. We defined number of nighttime awakenings as the number of 20 min blocks of contiguous wake epochs between sleep onset and wake-up time.
For between-group (GAD vs. control) comparisons, analyses were conducted for weekday and weekend nights separately, using school attendance the next day as the definition of a weekday night. For within-group examinations of correspondence between actigraphy and subjective reports, all seven nights of actigraphy were used since parent and child sleep measures did not differentiate between sleep on weekdays or weekends.
Data-Analytic Plan
Research Aim 1
Parent and child-reported sleep problems and patterns were compared between the groups using analyses of variance (ANOVA) with error correction based on the number of comparisons (0.05/9 = p < 0.006). Objective sleep patterns were compared using independent samples t-tests. For actigraphy variables, between-group comparisons were made for weekday and weekend sleep separately. The number of children who completed actigraphy over the summer/during holidays did not differ between groups, GAD = 6 (14 %); control = 9 (22 %); p = 0.289.
Research Aim 2
Correspondence for parent-reported and actigraphy-based child sleep patterns within groups was examined by computing correlations and paired samples t-tests between each individual parent report item and the actigraphy variable to which it was linked. We examined within-group correspondence between subjective and objective estimates of child sleep problems in several ways. First, we computed a series of bivariate correlations between total CSHQ and SSR scores as well as correlations among 4 overlapping CSHQ and SSR sleep problem items and corresponding actigraphy variables.
We also conducted tests of the effect of group status on discrepancies between parent and child reports. Since it would be erroneous to assume these measures to be independent observations (De Los Reyes and Kazdin 2005; De Los Reyes et al. 2013b), a key assumption underlying general linear modeling (GLM), we utilized generalized estimating equations (GEE): an extension of the GLM that assumes correlated observations of dependent and/or independent variables (Hanley et al. 2003). For GEE modeling, we used an identity link function with an unstructured correlation matrix given the small number of dependent variables. We modeled sleep problem scores as a nested, repeated-measures (within dyadic subjects) dependent variable and modeled the dependent variable as a function of 3 sets of factors (1 within-subjects informant factor, 1 between-subjects group status factor, and their interaction term). We based factor contrasts on comparisons of factors in descending order. The informant factor (coded in ascending order) was coded Parent and then Child. The group status factor (coded in ascending order) was coded Control and then GAD. In the presence of a significant interaction, we conducted univariate tests. As in prior work (De Los Reyes et al. 2013a; Lipton et al. 2014), we calculated pseudo-R 2 figures by dividing each Wald χ2 estimate by the summation of the three estimates in the GEE model (i.e., 119.58). Lastly, we conducted tests of the relation between children’s group status and actigraphy estimates of children’s sleep using independent samples t-tests.
Results
Preliminary Analyses
Frequency distributions for all variables were first examined to detect possible outliers and deviations from normality. We detected deviations in the form of skewness and kurtosis for several sleep variables based on actigraphy and parent-report. Such findings are consistent with previous research (Szymczak et al. 1993; Wolfson and Carskadon 1998) and data transformations were therefore not conducted. Further, while bootstrapping methods also can be used to reduce non-normality, a potential limitation of this method is under-representation of true variability in smaller sample sizes (Guan et al. 2012). Thus, bootstrapping was not performed. Lastly, we observed non-significant relations between the 23-item parent (CHSQ) and child (SSR) reports and child age and gender.
Aim 1: Comparison of Sleep Patterns and Problems Between Anxious Youth and Controls
Parent and Child-Reported Sleep Problems
Parents of children with GAD (M = 35.0, SD = 6.6) reported significantly greater total sleep problems than parents of controls (M = 26.7, SD = 3.1), F (1, 73) = 47.84, p < 0.001. In addition, parents of anxious youth reported significantly greater problems related to bedtime resistance, F (1, 72) = 12.92, p < 0.001; sleep onset delay, F (1, 72) = 22.91, p < 0.001; sleep duration, F (1, 72) = 15.58, p < 0.001; sleep anxiety, F (1, 71) = 26.57, p < 0.001; parasomnias, F (1, 72) = 15.62, p < 0.001; and daytime sleepiness, F (1, 72) = 10.05, p < 0.002. Children with GAD (M = 39.3, SD = 6.2) also reported significantly greater total sleep problems than controls (M = 34.6, SD = 5.3), F (1, 73) = 9.52, p < 0.003.
Parent Reported Sleep Patterns
Analysis of parent-reported sleep patterns did not reveal significant differences in terms of bedtime, total sleep duration, or wake-up time between groups, ts = −0.30 to 2.42; ps = 0.16 to 0.76. See Table 2.
Actigraphy-Based Sleep Patterns
We present means and standard deviations for actigraphy-based sleep variables for both groups in Table 2. We compared the groups on 6 actigraphy variables (mean bedtime, total time in bed, total sleep duration, sleep onset latency, number of nighttime awakenings, and wake-up time) for weekday and weekend nights separately. We did not detect significant between-group differences on any variable, ts = −1.7 to 1.9; ps = 0.05 to 0.87.
Aim 2: Cross-Method Correspondence within Anxious and Control Groups
Parent-Reported and Actigraphy-Estimated Sleep Patterns
Parents of children with GAD reported significantly earlier bedtimes, t = −3.76, p < 0.01, greater total sleep duration, t = 6.98, p < 0.001, and earlier wake-up times, t = −2.41, p < 0.05, relative to actigraphy-based estimates. For the control group, parents reported significantly earlier bedtimes compared to actigraphy, t = −4.10, p < 0.001, as well as greater total sleep duration, t = −8.26, p < 0.001. See Table 3 for 7 days actigraphy estimates.
We assessed correspondence between these same variables. In the GAD group, we observed relatively weak relations between parent-reported and actigraphy-derived estimates of bedtime, total sleep duration, and wake-up time, rs = 0.27, 0.28, and 0.26, respectively; all ps > 0.08. In the control group, correspondence between parent-reported and actigraphy-derived bedtime and wake-up time was similar, rs = 0.28 and 0.12, respectively; both ps > 0.09; though a significant relation was found for total sleep duration, r = 0.54, p < 0.01.
Parent Reports, Child Reports, and Actigraphy-Estimated Sleep Problems
Consistent with prior work (De Los Reyes et al. 2015; De Los Reyes and Kazdin 2005; De Los Reyes et al. 2013b) parent CSHQ and child SSR (23-item) total scores showed weak correlations in both the GAD group, r = 0.22, ns; and control group, r = 0.02, ns.
We also examined correlations between four specific sleep problems from the CSHQ and SSR that corresponded with actigraphy variables. As shown in Table 4, we observed weak to moderate correlations between these parent and child-reported items in both groups. Within the GAD group, the association between parent and child report of “sleeps too little” was moderate in magnitude and statistically significant. Among control children, parent report of nighttime awakenings was moderately associated with awakenings based on actigraphy.
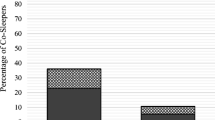
Informant and Group Status Effects on Parent and Child-Reported Sleep Problems
GEE analysis revealed significant main effects for both informant, Wald X 2 = 62.68, Pseudo-R2 = 52.41 %, B = 7.90 (SE = 1.00), 95 % Wald Confidence Interval (CI): [5.95, 9.86], p < 0.001; and group status, Wald X 2 = 51.71, Pseudo-R2 = 43.24 %, B = 8.33 (SE = 1.16), 95 % CI: [6.06, 10.61], p < 0.001. Based on total scores from parent (CHSQ) and child (SSR) reports, children reported greater sleep problems relative to parents, marginal Ms = 36.9 vs. 30.8; and children in the GAD group evidenced larger mean sleep problem scores relative to children in the control group, marginal Ms = 37.1 vs. 30.6. These results were qualified by a significant informant X group interaction, Wald X 2 = 5.19, Pseudo-R2 = 4.34 %, B = −3.66 (SE = 1.60), 95 % CI: [−6.81, −0.51], p < 0.05. Post-hoc univariate analyses revealed that parents of children in the GAD group reported greater levels of sleep problems relative to parents in the control group, 95 % CI: [6.06, 10.61], p < 0.001; and children with GAD reported greater levels of sleep problems relative to controls, 95 % CI: [2.11, 7.23], p < 0.001. However, the discrepancies between parent reports and child self-reports were significantly larger in the control group, 95 % CI: [−9.86,-5.95], p < 0.001; relative to the GAD group, 95 % CI: [−6.71, −1.78]; p < 0.01.
Discussion
Children with anxiety disorders and their parents consistently report high rates of sleep problems. However, the extent to which subjective sleep reports correspond with objective sleep data has rarely been explored. Objective sleep comparisons with typically-developing children are also limited. Thus, our first aim was to compare the sleep of school-aged children with GAD and a healthy control group based on subjective reports and 1 week of actigraphy. With regard to subjective sleep patterns, parents of children in both groups estimated similar bedtimes, total sleep duration, and wake-up times. Objective sleep comparisons produced similar results. On both weekdays and weekends, no differences were detected in terms of what time the groups went to bed, how long they stayed in bed, how long they actually slept, how long it took them to initiate sleep, how many times they woke up during the night, or their morning wake-up time. These results are similar to those from a recent study utilizing home-based PSG among the same two populations of children. In the only other study to incorporate 1 week of actigraphy, youth with various anxiety diagnoses required significantly longer to initiate sleep than controls but the mean difference in sleep onset latency was only 5 min (Cousins et al. 2011). A similar difference was found in the current study whereby weekend sleep onset latency was approximately 7 min longer in the GAD group. Although this result failed to reach statistical significance (p = 0.05), a moderate effect size was detected. However, the clinical meaningfulness of this difference is indeterminate.
Contrary to our findings for sleep patterns, though consistent with other studies of sleep complaints (Alfano et al. 2006, 2007, 2010), both parents and anxious children endorsed significantly more sleep problems than controls. With the exception of sleep-disordered breathing and nighttime awakenings, differences were found for all sleep subscales examined. Discrepancies between children’s sleep patterns and endorsement of sleep problems might be explained by the specific types of ‘problems’ exhibited by children with GAD which have repeatedly been shown to include attempts to delay bedtime, requests to co-sleep, complaints of nightmares, and/or expression of nighttime fears (Alfano et al. 2006, 2007, 2010; Chase and Pincus 2011; Hudson et al. 2009; Reynolds and Alfano 2015). Even though occurring in the context of sleep, such behaviors may not alter actual sleep parameters. Additionally, clinically-anxious children’s perceptions (and complaints) of problems initiating sleep may arise from cognitive-affective biases (e.g., low sleep self-efficacy) or sleep state misperception more so than actual sleep patterns.
A second aim of the current study was to examine cross-method correspondence for child sleep patterns in both groups. Contrary to expectations, all parents endorsed significantly earlier bedtimes and greater total sleep duration in comparison to actigraphy. However, only parents of children with GAD provided significantly-discrepant (i.e., earlier) estimates of child wake-up time. This finding could reflect greater child difficulty getting out of bed in the morning; an interpretation supported by significantly greater levels of daytime sleepiness in the anxious group. Still, because total sleep duration was similar between the groups, morning waking problems and daytime tiredness could be a function of differences in sleep quality or sleep need rather than actual sleep duration. Indeed, parents and children in the GAD group tended to agree that children sleep too little. As sleep processes are shaped by emotional and cognitive inputs (Saper et al. 2005; Walker 2009), persistently increased levels of daytime anxiety/worry might coincide with a stronger homeostatic sleep drive aimed at regulating the physiologic/biochemical effects of stress and arousal. Questions related to sleep quality and need among anxious youth remain important and interesting questions for subsequent studies.
All parents perceived their children to get more sleep than indicated by actigraphy but significant cross-method correspondence for total sleep duration was only found among controls. In the GAD group, relations across all three sleep pattern variables examined were non-significant, suggesting discrepancies between parental perceptions and actual child sleep patterns are somewhat more discordant in anxious samples. Thus, whenever possible, actigraphy should be used in conjunction with subjective reports in order to fully understand children’s actual sleep patterns. We do not wish to imply however that discrepancies between informants’ reports or between subjective and objective sleep indices should be viewed as measurement error and thus a hindrance to drawing empirical conclusions (Alfano et al. 2013; De Los Reyes 2013; De Los Reyes et al. 2011b) or reaching clinical decisions regarding sleep (De Los Reyes et al. 2011a). In fact, interpreting subjective reports as ‘unreliable’ conflicts with findings from the present study where both parents and children provided internally-consistent reports. Among anxious youth in particular this point is worth emphasizing since sleep-related complaints are common and effective intervention approaches rely on input from and motivation from both family members.
We also examined cross-method correspondence for sleep problems across parent and child reports as well as actigraphy. All children reported more sleep problems relative to parents with larger discrepancies found in the control group. Although previous research points toward higher endorsement of sleep problems by parents relative to their anxious children, some methodological differences are noteworthy. In the current study we attempted to ensure that both parent and child reports of sleep problems tapped the same behavioral domains, using the same rating format, and number of items whereas prior studies have tended to rely on non-parallel measures of sleep problems (Chase and Pincus 2011; Short et al. 2013). Variations in key components of measures (e.g., item content, scaling, number and order of items, and response options) can indeed produce drastically different assessment outcomes (Schwarz 1999).
In relation to the more specific sleep problems examined, we found weak correlations overall between subjective and objective measures. The only exception was a moderate, significant association between parent and actigraphy-based nighttime awakenings among controls. This result is somewhat surprising since anxious more so than non-anxious children would be expected to seek out parental attention and support at night. It is possible that parents of anxious youth simply presume nighttime awakenings to occur based on subsequent child complaints rather than actual middle of the night interactions. Specific factors that inform parents’ understanding of these nighttime problems, especially among anxious youth, nonetheless remain to be clarified.
There are limitations to the present study. First, although a key strength of this study was the collection of data from two separate informants and an objective sleep measure, the response formats were not completely parallel. This could have impacted the magnitudes of observed relations between subjective and objective measures. Unfortunately, we did not assess perceived sleep quality or true sleep need which may be critical factors to consider. It should also be noted that actigraphy has been shown to identify sleep onset sooner than PSG when utilized concurrently (Schwarz 1999) and may have underestimated sleep onset latency and overestimated total sleep duration. Actigraphy was collected over a 1 week period but our subjective measures were retrospective in nature. Thus, we cannot rule out the possibility that sleep measures captured different ‘snapshots’ of children’s sleep resulting in lower-magnitude correlations.
One might also question whether the low level of correspondence observed between subjective and objective sleep measures might reflect inadequate psychometric properties of subjective measures. However, both informants’ subjective sleep reports were found to be internally consistent and differentiated the anxious and control groups. Moreover, the low correspondence estimates observed between subjective and objective sleep measures is consistent with the mental health field in general (De Los Reyes and Aldao 2015; De Los Reyes et al. 2015; De Los Reyes and Kazdin 2005; De Los Reyes et al. 2013b) and sleep research in general (Edinger et al. 2000; Rosa and Bonnet 2000).
Several interesting findings emerged from the current study including non-significant differences in the objective sleep patterns of children with GAD compared to a matched, healthy control group. To date, evidence for objective sleep abnormalities among clinically-anxious youth comes from one study where anxious youth were studied in a sleep laboratory (Alfano et al. 2013) and another showing anxious youth to require 5 min longer than controls, on average, to initiate sleep at home (Cousins et al. 2011). We nonetheless caution against interpreting findings as evidence for the absence of sleep-related problems among anxious youth. Sleep-related problems in children can occur prior to the actual sleep period and/or take place outside of the bedroom. Objective estimates would not be expected to capture these behaviors despite a potential need for intervention services. Such problems may also engender sleep disorders over time.
Finally, although we examined a relatively homogeneous anxious group of children (e.g., primary GAD, a restricted age range), the possibility of within-group differences based on other factors needs to be considered. As an example, distinction can be drawn between adult insomniacs with and without normal sleep patterns, with consistent findings of mood disturbance and dysfunctional beliefs about sleep in the former (Edinger et al. 2000). Evolving questions for child researchers therefore include possible sleep-based differences as a function of cognitive-affective biases and processes. In clinical settings, consideration of such factors among children presenting with insomnia may be more valuable than objective sleep assessments and better inform treatment planning.
References
Alfano, C. A., Beidel, D. C., Turner, S. M., & Lewin, D. S. (2006). Preliminary evidence for sleep complaints among children referred for anxiety. Sleep Medicine, 7, 467–473. doi:10.1016/j.sleep.2006.05.002.
Alfano, C. A., Ginsburg, G. S., & Kingery, J. N. (2007). Sleep-related problems among children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 224–232. doi:10.1097/01.chi.0000242233.06011.8.
Alfano, C. A., Pina, A. A., Zerr, A. A., & Villalta, I. K. (2010). Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatry and Human Development, 41, 156–167. doi:10.1007/s10578-009-0158-5.
Alfano, C. A., Reynolds, K., Scott, N., Dahl, R. E., & Mellman, T. A. (2013). Polysomnographic sleep patterns of non-depressed, non-medicated children with generalized anxiety disorder. Journal of Affective Disorders, 147, 379–384. doi:10.1016/j.jad.2012.08.015.
Arora, T., Broglia, E., Pushpakumar, D., Lodhi, T., & Taheri, S. (2013). An investigation into the strength of the association and agreement levels between subjective and objective sleep duration in adolescents. PloS One, 8, e72406. doi:10.1371/journal.pone.0072406.
Bordeleau, S., Bernier, A., & Carrier, J. (2012). Longitudinal associations between the quality of parent − child interactions and children’s sleep at preschool age. Journal of Family Psychology, 26, 254. doi:10.1037/a0027366.
Buysse, D. J., Ancoli-lsrael, S., Edinger, J. D., Lichstein, K. L., & Morin, C. M. (2006). Recommendations for a standard research assessment of insomnia. Sleep: Journal of Sleep and Sleep Disorders Research, 29, 1155–1173.
Carskadon, M. A., & Acebo, C. (1993). A self-administered rating scale for pubertal development. Journal of Adolescent Health, 14, 190–195. doi:10.1016/1054-139X(93)90004-9.
Chase, R. M., & Pincus, D. B. (2011). Sleep-related problems in children and adolescents with anxiety disorders. Behavioral Sleep Medicine, 9, 224–236. doi:10.1080/15402002.2011.606768.
Clementi, M. A., & Alfano, C. A. (2014). Targeted behavioral therapy for childhood generalized anxiety disorder: a time-series analysis of changes in anxiety and sleep. Journal of Anxiety Disorders, 28, 215–222. doi:10.1016/j.janxdis.2013.10.006.
Cohen, J. (1960). A coefficient of agreement of nominal scales. Educational and Psychological Measurement, 20, 37–46.
Corkum, P., Moldofsky, H., Hogg-Johnson, S., Humphries, T., & Tannock, R. (1999). Sleep problems in children with attention‐deficit/hyperactivity disorder: impact of subtype, comorbidity, and stimulant medication. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1285–1293. doi:10.1097/00004583-199910000-00018.
Cousins, J. C., Whalen, D. J., Dahl, R. E., Forbes, E. E., Olino, T. M., Ryan, N. D., & Silk, J. S. (2011). The bidirectional association between daytime affect and nighttime sleep in youth with anxiety and depression. Journal of Pediatric Psychology, 36, 969–979. doi:10.1093/jpepsy/jsr036.
Cowie, J., Alfano, C. A., Patriquin, M. A., Reynolds, K. C., Talavera, D., & Clementi, M. A. (2014). Addressing sleep in children with anxiety disorders. Sleep Medicine Clinics, 9, 137–148. doi:10.1016/j.jsmc.2014.02.001.
Dayyat, E. A., Spruyt, K., Molfese, D. L., & Gozal, D. (2011). Sleep estimates in children: parental versus actigraphic assessments. Nature and Science of Sleep, 3, 115. doi:10.2147/NSS.S25676.
De Los Reyes, A. (2013). Strategic objectives for improving understanding of informant discrepancies in developmental psychopathology research. Development and Psychopathology, 25, 669–682. doi:10.1017/S0954579413000096.
De Los Reyes, A., & Aldao, A. (2015). Introduction to the special section. Toward implementing physiological measures in clinical child and adolescent assessments. Journal of Clinical Child and Adolescent Psychology, 44, 221–237. doi:10.1080/15374416.2014.891227.
De Los Reyes, A., & Kazdin, A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131, 483–509. doi:10.1037/0033-2909.131.4.483.
De Los Reyes, A., Alfano, C. A., & Beidel, D. C. (2011a). Are clinicians’ assessments of improvements in children’s functioning “global”? Journal of Clinical Child and Adolescent Psychology, 40, 281–294. doi:10.1080/15374416.2011.546043.
De Los Reyes, A., Kundey, S., & Wang, M. (2011b). The end of the primary outcome measure: a research agenda for constructing its replacement. Clinical Psychology Review, 31, 829–838. doi:10.1016/j.cpr.2011.03.011.
De Los Reyes, A., Aldao, A., Thomas, S. A., Daruwala, S., Swan, A. J., Van Wie, M., & Lechner, W. V. (2012). Adolescent self-reports of social anxiety: Can they disagree with objective psychophysiological measures and still be valid? Journal of Psychopathology and Behavioral Assessment, 34, 308–322. doi:10.1007/s10862-012-9289-2.
De Los Reyes, A., Lerner, M. D., Thomas, S. A., Daruwala, S., & Goepel, K. (2013a). Discrepancies between parent and adolescent beliefs about daily life topics and performance on an emotion recognition task. Journal of Abnormal Child Psychology, 41, 971–982. doi:10.1007/s10802-013-9733-0.
De Los Reyes, A., Thomas, S. A., Goodman, K. L., & Kundey, S. M. A. (2013b). Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology, 9, 123–149. doi:10.1146/annurev-clinpsy-050212-185617.
De Los Reyes, A., Augenstein, T. M., Wang, M., Thomas, S. A., Drabick, D., Burgers, D., & Rabinowitz, J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin. doi:10.1037/a0038498.
Edinger, J. D., Fins, A. I., Glenn, D. M., Sullivan, R. J., Jr., Bastian, L. A., Marsh, G. R., & Shaw, E. (2000). Insomnia and the eye of the beholder: Are there clinical markers of objective sleep disturbances among adults with and without insomnia complaints? Journal of Consulting and Clinical Psychology, 68, 586. doi:10.1037/0022-006X.68.4.586.
Fleiss, J. (1981). Statistical methods for rates and proportions (2nd ed.). New York: Wiley.
Gregory, A. M., & O’Connor, T. G. (2002). Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 964–971. doi:10.1097/00004583-200208000-00015.
Gregory, A. M., Rijsdijk, F. V., & Eley, T. C. (2006). A twin‐study of sleep difficulties in school‐aged children. Child Development, 77, 1668–1679. doi:10.1111/j.1467-8624.2006.00966.x.
Gregory, A. M., Cousins, J. C., Forbes, E. E., Trubnick, L., Ryan, N. D., Axelson, D. A., & Dahl, R. E. (2011). Sleep items in the child behavior checklist: a comparison with sleep diaries, actigraphy, and polysomnography. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 499–507. doi:10.1016/j.jaac.2011.02.003.
Guan, N.C., Yusoff, M.S.B., Zainal, N.Z., & Yun, L.W. (2012). Analyses of two independent samples with non normailty using non parametric method, data transformation and bootsrapping method. International Medical Journal, 19 (3). 227-229.
Hanley, J. A., Negassa, A., & Forrester, J. E. (2003). Statistical analysis of correlated data using generalized estimating equations: an orientation. American Journal of Epidemiology, 157, 364–375. doi:10.1093/aje/kwf215.
Hudson, J. L., Gradisar, M., Gamble, A., Schniering, C. A., & Rebelo, I. (2009). The sleep patterns and problems of clinically anxious children. Behaviour Research and Therapy, 47, 339–344. doi:10.1016/j.brat.2009.01.006.
Iglowstein, I., Jenni, O. G., Molinari, L., & Largo, R. H. (2003). Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics, 111, 302–307. doi:10.1542/peds.111.2.302.
Ivanenko, A., Barnes, M. E., Crabtree, V. M., & Gozal, D. (2004). Psychiatric symptoms in children with insomnia referred to a pediatric sleep medicine center. Sleep Medicine, 5, 253–259. doi:10.1016/j.sleep.2004.02.001.
Johnson, E. O., Chilcoat, H. D., & Breslau, N. (2000). Trouble sleeping and anxiety/depression in childhood. Psychiatry Research, 94, 93–102. doi:10.1016/S0165-1781(00)00145-1.
Kushnir, J., & Sadeh, A. (2013). Correspondence between reported and actigraphic sleep measures in preschool children: the role of a clinical context. Journal of Clinical Sleep Medicine, 9, 1147–1151. doi:10.5664/jcsm.3154.
Lipton, M. F., Augenstein, T. M., Weeks, J. W., & De Los Reyes, A. (2014). A multi-informant approach to assessing fear of positive evaluation in socially anxious adolescents. Journal of Child and Family Studies, 23, 1247–1257. doi:10.1007/s10826-013-9785-3.
McDonald, L., Wardle, J., Llewellyn, C. H., van Jaarsveld, C. H. M., & Fisher, A. (2014). Predictors of shorter sleep in early childhood. Sleep Medicine, 15, 536–540. doi:10.1016/j.sleep.2014.01.005.
Meltzer, L. J., Montgomery-Downs, H. E., Insana, S. P., & Walsh, C. M. (2012a). Use of actigraphy for assessment in pediatric sleep research. Sleep Medicine Reviews, 16, 463–475. doi:10.1016/j.smrv.2011.10.002.
Meltzer, L. J., Walsh, C. M., Traylor, J., & Westin, A. M. L. (2012b). Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep, 35, 159.
Mick, E., Biederman, J., Jetton, J., & Faraone, S. V. (2000). Sleep disturbances associated with attention-deficit hyperactivity disorder: the impact of psychiatric comorbidity and pharmacotherapy. Journal of Child and Adolescent Psychopharmacology, 10, 223–231. doi:10.1089/10445460050167331.
Owens, J. A., Maxim, R., Nobile, C., McGuinn, M., & Msall, M. (2000a). Parental and self-report of sleep in children with attention-deficit/hyperactivity disorder. Archives of Pediatrics and Adolescent Medicine, 154, 549. doi:10.1001/archpedi.154.6.549.
Owens, J. A., Spirito, A., & McGuinn, M. (2000b). The Children’s sleep habits questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep, 23, 1043–1052.
Patriquin, M. A., Mellman, T. A., Glaze, D. G., & Alfano, C. A. (2014). Polysomnographic sleep characteristics of generally-anxious and healthy children assessed in the home environment. Journal of Affective Disorders, 161, 79–83. doi:10.1016/j.jad.2014.02.037.
Reynolds, K., & Alfano, C. A. (2015). Things that go bump in the night: Frequency and predictors of nightmares in anxious and non-anxious children. Behavioral Sleep Medicine. in press.
Robinson, A. M., & Richdale, A. L. (2004). Sleep problems in children with an intellectual disability: parental perceptions of sleep problems, and views of treatment effectiveness. Child: Care, Health and Development, 30, 139–150. doi:10.1111/j.1365-2214.2004.00395.x.
Rosa, R. R., & Bonnet, M. H. (2000). Reported chronic insomnia is independent of poor sleep as measured by electroencephalography. Psychosomatic Medicine, 62, 474–482.
Sadeh, A. (1996). Evaluating night wakings in sleep-disturbed infants: a methodological study of parental reports and actigraphy. Sleep, 19, 757–762.
Sadeh, A., Sharkey, K. M., & Carskadon, M. A. (1994). Activity-based sleep—wake identification: an empirical test of methodological issues. Sleep, 17, 201–207.
Saper, C. B., Cano, G., & Scammell, T. E. (2005). Homeostatic, circadian, and emotional regulation of sleep. Journal of Comparative Neurology, 493, 92–98. doi:10.1002/cne.20770.
Schwarz, N. (1999). Self-reports: How the questions shape the answers. American Psychologist, 54, 93. doi:10.1037/0003-066X.54.2.93.
Short, M. A., Gradisar, M., Lack, L. C., Wright, H., & Carskadon, M. A. (2012). The discrepancy between actigraphic and sleep diary measures of sleep in adolescents. Sleep Medicine, 13, 378–384. doi:10.1016/j.sleep.2011.11.005.
Short, M. A., Gradisar, M., Lack, L. C., Wright, H. R., & Chatburn, A. (2013). Estimating adolescent sleep patterns: parent reports versus adolescent self-report surveys, sleep diaries, and actigraphy. Nature and Science of Sleep, 5, 23. doi:10.2147/NSS.S38369.
Silverman, W. K., & Albano, A. M. (1996). The anxiety disorders interview schedule for children (ADIS-C/P). San Antonio, TX: Psychological Corporation.
Silverman, W. K., Saavedra, L. M., & Pina, A. A. (2001). Test-retest reliability of anxiety symptoms and diagnoses with the anxiety disorders interview schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 937–944. doi:10.1097/00004583-200108000-00016.
Szymczak, J. T., Jasińska, M., Pawlak, E., & Zwierzykowska, M. (1993). Annual and weekly changes in the sleep-wake rhythm of school children. Sleep, 16, 433–435.
Walker, M. P. (2009). The role of sleep in cognition and emotion. Annals of the New York Academy of Sciences, 1156, 168–197. doi:10.1111/j.1749-6632.2009.04416.x.
Weschler, D. (1983). Wechsler Abbreviated Scale of Intelligence (WASI). San Antonio: Psychological Corporation.
Wolfson, A. R., & Carskadon, M. A. (1998). Sleep schedules and daytime functioning in adolescents. Child Development, 69, 875–887. doi:10.1111/j.1467-8624.1998.tb06149.x.
Acknowledgments
This work was supported by NIH grant #K23MH081188 awarded to the first author.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alfano, C.A., Patriquin, M.A. & De Los Reyes, A. Subjective – Objective Sleep Comparisons and Discrepancies Among Clinically-Anxious and Healthy Children. J Abnorm Child Psychol 43, 1343–1353 (2015). https://doi.org/10.1007/s10802-015-0018-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-015-0018-7