Abstract
This study explored the influence of adolescent mood variability on the symptom development of generalized anxiety and depression in the context of parent-adolescent negative interactions. Participants were 456 adolescents (55.7 % male) from a community sample, who were followed from age 13 to 16 years. During 4 annual assessments, adolescents reported on their generalized anxiety and depressive symptoms, and both parents and adolescents on levels of negative interactions with each other. Within each study year, adolescents rated their daily mood states during 5 consecutive days for 3 times per year (total of 9 weeks). The absolute differences between mood states on consecutive days were summed to construct a mood variability score. Results showed that high levels of adolescent mood variability predicted increases in generalized anxiety and depressive symptoms across the studied period. No influence of negative interactions on anxiety and depression development was found, but positive predictive links from mood variability to negative interactions at age 14 and 15 appeared. The study underscores the role of adolescent mood variability in the development of symptoms of generalized anxiety and depression during adolescence, but found little evidence for an influence of parent-adolescent negative interactions on internalizing problem development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adolescence is a period with great challenges. For instance, adolescents have to accommodate to biological changes (Brooks-Gunn and Reiter 1990), develop new emotional skills (Rosenblum and Lewis 2003), and achieve autonomy (Zimmer-Gembeck and Collins 2003). This transitional period may be perceived as emotionally demanding to most adolescents (Phillips and Power 2011) and therefore adolescents might be especially vulnerable to the development of internalizing problems (i.e., symptoms of anxiety and depression). Studies using community samples have found normative increases in the experience of symptoms of generalized anxiety and depression across adolescence (Cole et al. 2002; Van Oort et al. 2009). Moreover, it has been shown that symptoms of anxiety and depression co-occur frequently during adolescence (Lewinsohn et al. 1997). Although the increase in internalizing symptoms seems normative during this period, for some adolescents it might be linked to various negative outcomes, including prolonged anxiety or depressive symptoms into adulthood (Pine et al. 1998), lowered feelings of self-efficacy (Muris 2002), and reduced social competence (Chansky and Kendall 1997; Daley and Hammen 2002).
One key factor that may underlie the development of internalizing symptoms is heightened mood variability, which is characterized by “frequent and extreme changes in mood or emotion over time” (Larsen 1987, p. 1195). During the first years of adolescence, individuals typically show an increase in mood variability (for a review, see Arnett 1999). It has been noted that great fluctuations in mood (i.e., high levels of mood variability) may impair individuals in their ability to function adaptively, thereby provoking depressive and anxious feelings (Gruber et al. 2013). Moreover, when trying to understand the influence of mood variability on the development of internalizing problems, we need to account for the social context of adolescents, because interpersonal difficulties play an important role in generalized anxiety and depression (Borkovec et al. 2004; Rudolph et al. 2008). Regarding this, early adolescence is characterized by significant changes in the parent-adolescent relationship (for a review, see Laursen and Collins 2009) and increased conflicts are often the result (De Goede et al. 2009). Some adolescents might experience this normative increase in conflicts as stressful, which might affect their mood and in turn lead to increases in internalizing symptoms. Despite the hypothesized role of mood variability and parent–child conflicts on adolescent anxiety and depression development, longitudinal studies on these associations are lacking and to our knowledge there is currently no study available that simultaneously addressed these variables in concert. Therefore, using a community sample of adolescents followed from age 13 to 16, the overall aim of the present study was to examine the role of adolescent mood variability and negative interactions in the normative development of both generalized anxiety and depressive symptoms from early to middle adolescence.
Adolescent Mood Variability and Adolescent Internalizing Problems
When entering adolescence, individuals are confronted with a number of developmental changes, which may be perceived as challenging to most of them (Phillips and Power 2011). Especially because adolescents are not acquainted with these multiple changes, they are likely to react with more fluctuating moods than children or adults (Arnett 1999). Studies have shown that adolescents experience more mood variability than adults (Larson et al. 1980) and that their mood swings are more pronounced in early compared to late adolescence (Larson et al. 2002).
Several researchers have hypothesized that mood variability plays an important role in psychological health (Cole and Hall 2008) and individual differences in mood variability might also explain why some individuals show higher levels of internalizing problems. For instance, studies have shown that mood variability is positively related to neuroticism (Murray et al. 2002), which in turn increases the risk for symptoms of anxiety and depression (Kendler and Gardner 2011). Moreover, it has also been hypothesized that heightened mood variability is associated with a greater need to regulate these fluctuations, leading to fewer available capacities for adaptive functioning in other domains (Gruber et al. 2013), therefore possibly leading to anxiety and depressive symptoms. Despite the plausibility of the influence of mood variability on the development of internalizing problems, it is important to note that anxiety and depressive symptoms might also exacerbate mood variability. As Gruber and colleagues (2013) note, psychopathology might make it more difficult to maintain a stable mood state, which might then lead to more mood variability. Therefore, in addition to mood variability evoking feelings of anxiety and depression, such symptoms might also lead to fluctuating emotions, thereby suggesting a possible dynamic interplay between mood variability and internalizing symptoms.
Despite the theoretical plausibility of links between mood variability and symptoms of internalizing problems, most empirical evidence is restricted to cross-sectional studies, which hampers our ability to draw solid conclusions on possible developmental links between these phenomena. One cross-sectional study using a representative community sample of adolescents found that heightened mood variability, as reported by parents and adolescents, was related to an increased likelihood of adolescent anxiety and depressive disorders (Stringaris and Goodman 2009). Likewise, other studies using adolescent and adult samples have found positive associations between heightened mood variability and increased levels of anxiety and depressive symptoms (Gruber et al. 2013; Silk et al. 2003). Studies using clinical samples have found similar relations by showing that mood variability was higher in patients with anxiety (Bowen et al. 2006) and depressive disorders compared to controls (Silk et al. 2011). These studies point out that mood variability is positively associated with both anxiety and depressive symptoms. To our knowledge, there is only one short-term longitudinal study that examined the influence of mood variability on the development of anxiety and depressive symptoms (Neumann et al. 2011). This study used the same sample as the present study, but only examined a one-year interval in early adolescence (age 13 to 14). It was found that adolescents’ day-to-day mood level and mood variability were related to changes in anxiety and depressive symptoms. However, the association between mood variability and depressive symptoms was no longer significant when examining mood level and variability simultaneously. Due to the small time interval, testing for a possible dynamic relationship between mood variability and internalizing problems was impossible. Therefore, using the same sample, we aimed to extend these initial longitudinal findings by investigating the role of adolescent mood variability in the development of adolescent generalized anxiety and depressive symptoms from age 13 to 16 years while taking into account the stability of both constructs and possible reverse paths.
Parent-Adolescent Negative Interactions and Adolescent Internalizing Problems—Mood Variability as an Explaining Variable?
When trying to understand the role of mood variability in the development of anxiety and depression, we also have to consider the adolescent’s social context. Worrying, as the core symptom of generalized anxiety, is often concerned with interpersonal relationships (Borkovec et al. 2004) and studies have shown that worry about interpersonal issues is most strongly endorsed in generalized anxiety in both clinical and community samples (Roemer et al. 1997). Moreover, interpersonal problems may induce feelings of low self-esteem and negative self-evaluations (Rudolph et al. 2008), and studies have shown that these feelings are associated with depressive symptoms (Bolton et al. 2009; Sowislo and Orth 2013). Given the importance of interpersonal difficulties in generalized anxiety and depression, it may be that certain aspects of the parent-adolescent relationship constitute a risk factor for anxiety and depressive symptoms during adolescence.
Although peers become increasingly important during adolescence (Brown 2004), the relationship with parents remains an important factor for adolescent development (Laursen and Collins 2009). The first years of adolescence are characterized by a change in the relationship between parents and adolescents (Laursen and Collins 2009) with temporary increases in conflicts (De Goede et al. 2009). These more frequent conflicts may explain the normative increase in generalized anxiety and depressive symptoms during adolescence (Kendall et al. 2006; Rudolph et al. 2008). Studies have confirmed the hypothesized role of negative parent-adolescent relationships in both generalized anxiety and depression. For instance, clinical studies have shown that children and adolescents with anxiety and depressive disorders have more conflict-ridden and less cohesive family environments than controls (Stark et al. 1990). Moreover, community studies have shown that different indices of relationship and attachment quality (e.g., perceived parental rejection and alienation) were concurrently and longitudinally associated with adolescent generalized anxiety (Hale et al. 2006; van Eijck et al. 2012) and depressive symptoms (Branje et al. 2010; Sheeber et al. 1997).
We hypothesize however that mood variability may be a key variable in explaining the link between parent-adolescent conflicts and adolescent generalized anxiety and depressive symptoms. Problems in the parent-adolescent relationship are likely to be perceived as stressful and may therefore increase adolescent mood variability, which in turn may affect levels of adolescent generalized anxiety and depression. Indeed, it has been shown that interpersonal problems and daily stress are associated with higher levels of mood variability (Carels et al. 2000). Despite the theoretical suggestions, there is—to our knowledge—no study that has examined mood variability as the linking factor between parent-adolescent negative interactions and adolescent internalizing symptoms. Therefore, our second objective was to examine the role of parent-adolescent negative interactions in the development of adolescent generalized anxiety and depression, and specifically whether adolescent mood variability acted as a mediator in this link.
The Present Study
The present study addressed the development and interlinkage of adolescent internalizing problems (i.e., generalized anxiety and depressive symptoms) and adolescent mood variability in the context of parent-adolescent negative interactions in 456 adolescents followed from age 13 to 16 years. Specifically, we tested the following hypotheses: (1) high levels of mood variability predict increases in generalized anxiety and depression above and beyond the stability of these problems; (2) high levels of negative interactions predict increases in generalized anxiety and depression above and beyond the stability of these problems, (2b) but these links are indirect and run via high levels of mood variability. Although the primary hypothesis is that symptoms of generalized anxiety and depression are influenced by mood variability and negative interactions, we acknowledge that reverse paths may also be found.
Method
Participants
Data were taken from the RADAR-Y (Research on Adolescent Development and Relationships—Young cohort) study, a longitudinal research project in the Netherlands that followed adolescents, their families and friends from age 13 to 18 years. For the current study, data were used from four waves of measurement (ages 13 to 16 years) in order to represent early to middle adolescence. We had 497 target families available with predominantly middle or high socio-economic status (89.2 %) and Dutch-Caucasian background (96.6 %).
Because we used mothers’, fathers’, and adolescents’ reports to characterize parent-adolescent negative interactions, only families in which data from both parents were available for at least one wave of measurement were used. Of the initial 497 families, 456 were included by virtue of this criterion. Adolescents who were excluded from analyses had a higher probability of being from low SES families compared to the final sample, χ2(1) = 36.79, p < 0.01. However, excluded adolescents did not differ from the final sample on sex, levels of negative interactions, generalized anxiety, or depression scores at Time 1 or mood variability over the first study year. Adolescents’ mean age for the final sample was 13.03 years (SD = 0.48) at Time 1 and adolescent sex was almost equally distributed (55.7 % male).
Procedure
Prior to the start of the study, written information about the study was sent to adolescents and their parents, who provided written informed consent for each of the participating family members. The study was approved by the medical ethical committee of the University Medical Centre Utrecht (the Netherlands). For the present study, data were collected during four home visits (time[T]1, T5, T9 and T13), separated by 1 year. During the annual home visits, both adolescents and their parents were present and completed questionnaires. Research assistants visited the families to supervise the data-collection and to provide verbal instructions in addition to the written instructions that accompanied the questionnaires.
In addition to these annual home visits, a total of nine internet assessments were used. Within each study year, three internet assessments were conducted, for three consecutive years (T2 to T4 in study year 1, T6 to T8 in study year 2, and T10 to T12 in study year 3; see Table 1 for an overview of the design). An internet assessment lasted for 5 days (i.e., Monday to Friday). Each day during an internet assessment, adolescents rated their average mood states for happiness, sadness, anger, and anxiety using online questionnaires over this particular day. In order to remind adolescents to fill out the questionnaire, e-mail invitations were sent at approximately 5:30 pm. In order to complete the assessment, adolescents had to log in to the RADAR website for data collection. When adolescents had not completed the questionnaires 1.5 h after the initial e-mail invitation, they received reminder e-mails. After an additional 1.5 h, adolescents received text messages and, in case adolescents did not respond, phones calls were made. Families received 100 Euros (equivalent to US $133) for each home visit and adolescents received an additional 10 Euros (equivalent to US $13) for each internet assessment.
Measures
Adolescent Generalized Anxiety Symptoms
Adolescents completed the Generalized Anxiety subscale (9 items, e.g., “I am nervous”) of the Screen for Child Anxiety Related Emotional Disorders (SCARED; Birmaher et al. 1997). Items were rated on a three-point scale with response options 0 (almost never), 1 (sometimes), and 2 (often) and were summed into a total generalized anxiety score. Total scores were between 0 and 18 in the present sample and Cronbach’s αs ranged from 0.85 to 0.89 across the four waves of measurement (T1, T5, T9, T13).
Adolescent Depressive Symptoms
Adolescents completed the subscales Dysphoric Mood (8 items; e.g., “I feel like crying”), Negative Self-Evaluation (8 items; e.g., “I feel I am bad”) and Somatic Complaints (7 items; e.g., “I am tired”) of the Reynolds Adolescent Depression Scale—2nd Edition (RADS-2; Reynolds 2002). Response options ranged from 0 (almost never) to 3 (most of the time). The items were summed per subscales and then added up to a total depression score. Total scores were between 0 and 64 in the present sample and Cronbach’s αs ranged from 0.93 to 0.95 across the four waves of measurement (T1, T5, T9, T13).
Adolescent Mood Variability
In order to measure mood variability, adolescents completed the Daily Mood Device, an internet version of the Electronic Mood Device (Hoeksma et al. 2000). Adolescents were asked to rate the intensity of their daily mood for happiness, sadness, anger, and anxiety (“Today I feel …”) on 5 consecutive days at 9 different time-points (T2 to T4, T6 to T8, T10 to T12) using online questionnaires. Each mood state was measured with three items. Happiness using “glad”, “happy”, and “cheerful”, sadness using “sad”, “down”, and “dreary”, anger using “angry”, “cross”, and “short-tempered”, and anxiety using “afraid”, “anxious”, and “worried”. Items were assessed using a 9-point Likert scale (1 = not glad/sad/anxious… to 9 = glad/sad/anxious…). In order to increase reliability, the three items were summed per mood, resulting in a total mood score per day. Cronbach’s αs ranged from 0.86 to 0.96 for happiness, from 0.92 to 0.98 for sadness, from 0.88 to 0.96 for anger, and from 0.73 to 0.94 for anxiety.
In order to calculate adolescent mood variability, that is the day-to-day fluctuation in adolescent mood states, the absolute differences between assessments of consecutive days within 1 week were calculated, separately for each mood. These differences were summed per mood and then divided by the valid number of absolute difference scores per week in order to control for missing data. This resulted in a weekly mood variability score for each mood. Mood variability scores were only calculated when there were at least four valid assessments in total or three consecutive valid assessments per week. We decided to calculate a general mood variability score by summing the four different mood variability scores (happiness, sadness, anger, and anxiety variability) per internet assessment week (the ‘week mood variability’ score). This is because different mood variability scores correlated with a range from 0.37 to 0.75, all ps < 0.001, per internet assessment week and recent studies have shown that the variability of mood states contributes in rather non-specific ways to psychopathology (Neumann et al. 2011; Silk et al. 2003). For instance, Neumann et al. (2011), using the present sample from age 13 to 14, found that the variability of happiness, anger, anxiety, and sadness, and not just the variability of one particular emotion, influenced the development of anxiety and depressive symptoms. The week mood variability scores were used as indicators of a latent mood variability variable for each year. For instance, the week mood variability scores of T2, T3, and T4 loaded on one factor, representing adolescent mood variability between ages 13 and 14 years. These latent year mood variability scores were used in the analyses (for factor loadings see Online Resource 1 in the Supplementary Material).
Adolescent Mood Level
Based on the daily mood ratings from the internet assessments (as described above), we also calculated an adolescent mood level score. This score was only computed when there were at least four valid assessments in total or three consecutive valid assessments per week. In order to calculate the weekly mood level score for each mood, we summed the total daily mood scores within each week, separately for each emotion, and divided them by the valid number of daily mood scores per week. Then, we summed happiness (reverse coded), sadness, anger, and anxiety level scores for each week and calculated the mean of these three weekly scores for each year, resulting in three yearly mood level scores. These yearly mood level scores were used in the analyses as a covariate for mood variability.
Parent-Adolescent Negative Interactions
In order to create a dyadic image of the parent-adolescent relationship, adolescents, fathers, and mothers completed the short subscale Negative Interactions (6 items; e.g., “Do you and your mother/father/child annoy each other and get angry at each other?”) from the Network of Relationship Inventory (NRI; Furman and Buhrmester 1985). Based on these report, we had four measures on negative interactions available per time point (T1, T5, T9, T13): (a) Adolescents’ reports of their negative interactions with the mother and (b) the father, (c) mothers’ reports as well as (d) fathers’ reports of their negative interactions with the adolescent. Items were rated on a 5-point Likert scale with response options ranging from 1 (a little or not at all) to 5 (more is not possible). The mean of the items was used to construct an overall index of negative interactions for each informant. Cronbach’s αs ranged from 0.89 to 0.93 across the four waves of measurement (T1, T5, T9, T13). For the analyses, latent variables with mother-adolescent, adolescent-mother, father-adolescent and adolescent-father reports were constructed, separately for each wave of measurement (for factor loadings see Online Resource 1 in the Supplementary Material).
Attrition and Missing Data
Adolescent participant attrition was relatively low at 9.9 % from T1 to T13. The large majority of adolescents had complete data on generalized anxiety (86.6 %) and depressive symptoms (87.3 %) as well as on parent-adolescent negative interactions (87.5 %/86.2 % on negative interactions with the mother/father) at all four annual assessments. Complete data for parental report at all four assessments were available for 87.9 % of the mothers and for 82.2 % of the fathers. Moreover, most of the adolescents included in the study had at least one valid internet assessment within each year (83.6 %). Adolescents with missing data on generalized anxiety or depressive symptoms had higher generalized anxiety scores at T1 than adolescents with complete data at all four annual assessments, F(1,446) = 4.558, p < 0.05, although the effect size of this mean difference was small, η p 2 = 0.01. There were no significant differences regarding sex, socioeconomic status, depressive symptoms and negative interactions at T1, and mood variability measures within year 1 and 2 (T2, T3, T4).
Statistical Analyses
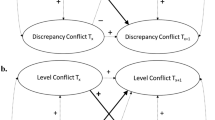
Given the structure of the data (see Table 1), which had yearly parallel assessments of anxiety, depression, and parent-adolescent negative interactions, but within-year assessments of mood variability, we fitted a series of nested structural model as depicted in Fig. 1 to answer our research questions. Models were fitted in Mplus 6.0 (Muthén and Muthén 1998–2010). In order to account for non-normal distributions and missing data in our models, we used the maximum likelihood estimation with robust standard errors (MLR). All models were controlled for adolescent sex to account for level differences between boys and girls. Because mood level and mood variability are significantly correlated, r = 0.32–0.67, p < 0.01, and in order to assess the specific influence of mood variability while controlling for mood level (see also Gruber et al. 2013), we included mood level as a time-varying covariate in the model by regressing mood variability on the associated yearly mood levels per study year. We used the Satorra-Bentler chi-square difference test (Satorra and Bentler 2001) to evaluate the significance of improvement between nested models when allowing for additional regression paths as depicted by our hypotheses. Absolute fit to the data was determined by the Comparative Fit Index and Tucker Lewis Index (CFI and TLI; acceptable values >0.90; Bentler and Bonett 1980) and the Root Mean Squared Error Approximation (RMSEA; acceptable values <0.08; Browne and Cudeck 1992). Presence of indirect paths was tested using the IND command in Mplus (see MacKinnon et al. 2004).
Overview of fitted models. Note: The base model (model 0) contained only autoregressive paths between repeated assessments within constructs (see  ) and cross-sectional correlations between parallel assessed variables (not shown for clarity). In the subsequent models influence paths were added between generalized anxiety and depression, respectively, and mood variability (model 1, see
) and cross-sectional correlations between parallel assessed variables (not shown for clarity). In the subsequent models influence paths were added between generalized anxiety and depression, respectively, and mood variability (model 1, see  ), then between generalized anxiety and depression, respectively, and the parent-adolescent negative interactions (model 2, see
), then between generalized anxiety and depression, respectively, and the parent-adolescent negative interactions (model 2, see  ), and finally between mood variability and parent-adolescent negative interactions (model 3, see
), and finally between mood variability and parent-adolescent negative interactions (model 3, see  ). The Satorra-Bentler chi-square difference test (Satorra and Bentler 2001) was used to evaluate the significance of the improvement in model fit, when adding particular influence paths
). The Satorra-Bentler chi-square difference test (Satorra and Bentler 2001) was used to evaluate the significance of the improvement in model fit, when adding particular influence paths
Results
Descriptive Statistics
Descriptive statistics of the annual measures of adolescent generalized anxiety, depression, and negative interactions are presented in Table 2, whereas the internet assessments of adolescent mood variability can be found in Table 3. Female adolescents scored higher on generalized anxiety and depressive symptoms at all assessments and higher on mood variability at T2, T6, T7, T8, T11, and T12 compared to male adolescents. Moreover, mothers reported more negative interactions with their daughters at T1, T5, and T9 (age 13, 14, and 15). Based on cutoff scores that discriminate between clinical and nonclinical anxiety and depression scores (Muris et al. 2000; Reynolds 2002), 3.5 % of the adolescents experienced clinical levels of depression and 12.5 % (sub)clinical levels of generalized anxiety.
Model Fitting
Our hypotheses were tested using a series of nested model testing. Fit statistics and model comparisons for the nested models are presented in Table 4. We started off with a base model, which contained only autoregressive paths of adolescent generalized anxiety and depressive symptoms, adolescent mood variability, and negative interactions as well as cross-sectional correlations between parallel assessed variables (model 0). The subsequent model tested hypothesis 1 and contained prediction paths from adolescent mood variability to adolescent generalized anxiety and depression and vice versa (model 1). Results showed that model 1 fit significantly better to the data than the base model.
We then moved on to testing hypothesis 2, concerning the role of negative interactions in understanding adolescent generalized anxiety and depression development in the context of mood variability. Model 1 served as the starting point. Allowing for prediction paths from negative interactions to generalized anxiety and depression and vice versa (model 2) did not improve model fit. We then tested for possible indirect effects from parent-adolescent negative interactions to adolescent generalized anxiety and depression, respectively, via adolescent mood variability. To this end, we allowed for paths from negative interactions to mood variability and vice versa, which significantly improved model fit (model 3). Therefore, model 3 was denoted as the best fitting model to the observed data.
Note that variability in anxiety as well as sadness were part of the overall mood variability measure. In order to account for the possibility that associations between mood variability and generalized anxiety and/or depression had been inflated by this inclusion, we tested if exclusion of either anxiety or sadness from the mood variability and level score would affect the longitudinal associations by running additional models. However, all results remained the same. Therefore, the results of the model were reported in which anxiety and sadness were part of the overall mood variability and level measure.
Adolescent Internalizing Symptoms, Adolescent Mood Variability, and Parent-Adolescent Negative Interactions
The standardized estimates of the significant paths of the final model (i.e., model 3) are depicted in Fig. 2. With respect to hypothesis 1, it was found that adolescent mood variability positively predicted adolescent generalized anxiety as well as depressive symptoms across ages 14 to 16 years. In contrast, there was only one path from generalized anxiety from age 13 to mood variability between 13 and 14 years and no predictive path from depression to mood variability at any time. In contrast with hypothesis 2, we did not find any direct paths of parent-adolescent negative interactions with adolescent generalized anxiety and depressive symptoms nor did we find any indirect paths via mood variability. Results furthermore show that mood variability led to more negative interactions at ages 14 and 15.
Structural model of adolescent generalized anxiety symptoms, adolescent depressive symptoms, and adolescent mood variability, and parent-adolescent negative interactions (final model 3). Note: Model is controlled for adolescent sex; Adolescent mood variability is controlled for mood level.  = correlations among residual variances of the variables.
= correlations among residual variances of the variables.  = standardized regressions estimates. Only estimates significant at p < 0.05 are provided. *p < 0.05, **p < 0.01, ***p < 0.001
= standardized regressions estimates. Only estimates significant at p < 0.05 are provided. *p < 0.05, **p < 0.01, ***p < 0.001
Discussion
The present study examined the role of adolescent mood variability and parent-adolescent negative interactions in the development of adolescent generalized anxiety and depressive symptoms. Consistently across the period studied, adolescent mood variability predicted increases in adolescent generalized anxiety and depression levels despite sizeable stability paths of these constructs. In contrast, only one reverse path, from adolescent generalized anxiety at age 13 to mood variability was found. No links from negative interactions to anxiety or depressive symptoms were found. However, we found that higher levels of mood variability predicted higher levels of negative interactions at age 14 and 15.
Adolescent Mood Variability and Adolescent Internalizing Problems
Results of the present study agree with and extend previous cross-sectional (e.g., Gruber et al. 2013; Silk et al. 2003) and one short-term longitudinal study (Neumann et al. 2011). This latter study used the same dataset, but was limited to a one-year interval. The present study extends the previous cross-sectional studies by showing that heightened mood variability predicted increases in both adolescent generalized anxiety and depression across the studied period. It extends the—to our knowledge—only longitudinal study by studying depressive and anxiety symptoms simultaneously, and by showing that mood variability, when controlled for mood level, predicts both these outcomes across a prolonged developmental span.
Although possible reverse paths from anxiety and depression to mood variability were theorized, only one path, from generalized anxiety in the first assessment year to mood variability was found. However, this path needs to be interpreted with caution, because mood variability in the first year could not be controlled for previous levels of mood variability. Although some researchers have noted that internalizing problems could themselves lead to increased difficulties in controlling mood states (e.g., Gruber et al. 2013), no longitudinal studies were available that specifically tested this assumption while simultaneously controlling for the stability of internalizing problems and mood variability. Findings of the present study suggest that although heightened mood variability affects the development of generalized anxiety and depressive symptoms, anxious and depressive symptoms in turn do not seem to lead to more mood variability. However, we can only speculate about the underlying mechanism. As noted by several researchers, heightened mood variability may be a sign of ineffective attempts to regulate one’s mood (Cole and Hall 2008; Neumann et al. 2011). Therefore, highly fluctuating moods may provoke feelings of the inability to keep mood between boundaries, which may distress some adolescents and increase symptoms of anxiety and depression. Importantly, the present study controlled for mood level in mood variability, therefore we can be sure that the associations between internalizing symptoms and mood variability are not confounded by individual differences in mood levels.
The fact that mood variability affected anxious and depressive symptoms simultaneously, may suggest that heightened mood variability is a shared vulnerability factor for both forms of internalizing problems. As found in previous studies (Lewinsohn et al. 1997; Seligman and Ollendick 1998), substantial correlations between symptoms of depression and generalized anxiety were found in our study. One explanation for this high co-occurrence could be shared etiological factors (Seligman and Ollendick 1998) and it may be that mood variability represents such an underlying factor. Mood variability might be closely related to the concept of negative affectivity, which has been hypothesized to be one shared risk factor for depression and anxiety (Clark and Watson 1991). Individuals with high negative affectivity experience high levels of aversive emotions and report great subjective distress (Watson and Clark 1984). Similarly, heightened mood variability is also perceived as aversive and is associated with lower well-being (Gruber et al. 2013).
Parent-Adolescent Negative Interactions and Adolescent Internalizing Problems
Our results suggest that the influence of parent-adolescent negative interactions on anxiety and depression development is limited despite previous evidence on such links (Branje et al. 2010; Van der Giessen et al. in press; van Eijck et al. 2012). Several reasons may explain the divergent findings. First, our study used multiple informants (mothers, father, adolescents), while previous studies used adolescent reports on both relationship quality and psychopathology (e.g., van Eijck et al. 2012), which may have inflated associations. Second, some previous studies have used more severe forms of parent–child conflict, such as alienation and parental rejection (e.g., Hale et al. 2006). Finally, it may be that other factors, such as parental over-control, may better account for increases in internalizing problems, such as anxiety symptoms (McLeod et al. 2007). Therefore, our study suggests that the particular and key developmental aspect of the parent–child relationship in adolescence, the likely increase in negative interactions during this period, may not be of particular importance in adolescents’ anxiety and depression development. However, this does not imply that other aspects of the parent–child relationship or parenting may not influence the development of adolescent internalizing problems.
The finding that mood variability predicted increases in parent–child conflicts underscores that the way mood is regulated and expressed is a central requirement for successful interaction (Bell and Calkins 2000). If adolescents have difficulties in controlling their emotions, parent-adolescent interactions may become difficult and conflicts may arise.
Limitations
The sizeable stability coefficients of the studied constructs should be taken into account when interpreting the results. As with many longitudinal studies, high stabilities of constructs may affect the results and suppress possible longitudinal relationships between variables. The constructs of the present study also showed fairly high stabilities. However, despite these fairly high stabilities significant predictive relations were still found.
In addition to this, a number of limitations need to be acknowledged. First, our sample predominantly consisted of Caucasian, middle-class Dutch families in which two parents were present. It is uncertain how results generalize to more diverse populations, including clinical samples or broader socio-economic or ethnic groups. Second, adolescent mood states, generalized anxiety and depressive symptoms were measured by adolescent self-report, which might have affected the associations due to common method variance (Podsakoff and Organ 1986). However, adolescents are accurate reporters of their internal states, because they have an adequate level of insight in their thoughts and feelings (Essau and Barrett 2001). More importantly, internalizing problems and adolescent mood variability were never assessed at the same time, but minimum three months apart from each other. Third, mood variability was assessed at different points in time than the parent-adolescent relationship and internalizing problems. As a consequence, cross-sectional correlations between mood variability and the other variables were not included when estimating the prediction paths to and from mood variability, which might have affected our results.
Implications and Conclusions
The present study used a community sample and only a small subset of adolescents experienced clinically elevated levels of internalizing problems. The results therefore have implications for understanding normative development, but they nonetheless show that mood variability might put adolescents at risk of developing heightened and possibly clinically elevated levels of internalizing symptoms. Therefore, our results suggest that preventive interventions focusing on generalized anxiety and depression may profit from helping adolescents to cope with fluctuating emotions. Such interventions should teach adolescents ways to identify and accept their own emotions and to practice strategies to control these. One such approach is dialectical behavior therapy (Linehan 1993), which combines acceptance and problem solving strategies to help individuals dealing with their emotional instability in reducing depressive and anxiety symptoms (Rathus and Miller 2002).
Findings of the present study also have research implications. First, more empirical studies on the role of mood variability in the development of internalizing problems are needed in order to elucidate the possible explanatory mechanism. Studies should focus on how adolescents become aware of their difficulties in regulating their moods, for instance by studying mood variability in concert with physiological measures of the stress regulation system. Recent cross-sectional studies have shown that mood variability is associated with increased cortisol (Simpson et al. 2008), and that high levels of cortisol are in turn associated with increased worry and stress (Adam 2006). Second, research should focus on whether mood variability not only affects the development of internalizing symptoms in a normative sample, but also in clinically referred adolescents. Third, future studies should study broader contextual factors in the development of adolescent internalizing symptoms, such as peer relations. Also, it would be interesting to examine if mood variability plays a more general role in other forms of psychopathology. In sum, the present study underscores that the ability to keep emotions stable represents an important task for adolescents, and those who have difficulties with that are at increased risk of developing increased levels of internalizing symptoms.
References
Adam, E. K. (2006). Transactions among adolescent trait and state emotion and diurnal and momentary cortisol activity in naturalistic settings. Psychoneuroendocrinology, 31, 664–679. doi:10.1016/j.psyneuen.2006.01.010.
Arnett, J. J. (1999). Adolescent storm and stress, reconsidered. American Psychologist, 54, 317–326. doi:10.1037/0003-066X.54.5.317.
Bell, K. L., & Calkins, S. D. (2000). Relationships as inputs and outputs of emotion regulation. Psychological Inquiry, 11, 160–163. doi:10.1207/S15327965PLI1103_04.
Bentler, P. M., & Bonett, D. G. (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88, 588–606. doi:10.1037/0033-2909.88.3.588.
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., et al. (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 545–553. doi:10.1097/00004583-199704000-00018.
Bolton, C., Barrowclough, C., & Calam, R. (2009). Parental criticism and adolescent depression: does adolescent self-evaluation act as a mediator? Behavioural and Cognitive Psychotherapy, 37, 553–570. doi:10.1017/S1352465809990221.
Borkovec, T. D., Alcaine, O. M., & Behar, E. (2004). Avoidance theory of worry and generalized anixety disorder. In R. G. Heimberg, C. L. Turk, & D. S. Mennin (Eds.), Generalized anxiety disorder: Advances in research and practice (pp. 77–108). New York: The Guilford Press.
Bowen, R., Baetz, M., Hawkes, J., & Bowen, A. (2006). Mood variability in anxiety disorders. Journal of Affective Disorders, 91, 165–170. doi:10.1016/j.jad.2005.12.050.
Branje, S. J. T., Hale, W. W., III, Frijns, T., & Meeus, W. H. J. (2010). Longitudinal associations between perceived parent–child relationship quality and depressive symptoms in adolescence. Journal of Abnormal Child Psychology, 38, 751–763. doi:10.1007/s10802-010-9401-6.
Brooks-Gunn, J., & Reiter, E. O. (1990). The role of pubertal processes. In S. Feldman & G. Elliott (Eds.), At the threshold: The developing adolescent (pp. 16–53). Cambridge: Harvard University Press.
Brown, B. B. (2004). Adolescents’ relationships with peers. In R. M. Lerner & L. Steinberg (Eds.), Handbook of adolescent psychology (2nd ed., pp. 363–394). New York: Wiley.
Browne, M., & Cudeck, R. (1992). Alternative ways of assessing model fit. Sociological Methods Research, 21, 230–258. doi:10.1177/0049124192021002005.
Carels, R. A., Blumenthal, J. A., & Sherwood, A. (2000). Emotional responsivity during daily life: relationship to psychosocial functioning and ambulatory blood pressure. International Journal of Psychophysiology, 36, 25–33. doi:10.1016/S0167-8760(99)00101-4.
Chansky, T. E., & Kendall, P. C. (1997). Social expectancies and self-perceptions in anxiety-disordered children. Journal of Anxiety Disorders, 11, 347–363. doi:10.1016/S0887-6185(97)00015-7.
Clark, L. A., & Watson, D. (1991). Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100, 316–336. doi:10.1037/0021-843X.100.3.316.
Cole, P. M., & Hall, S. E. (2008). Emotion dysregulation as a risk factor for psychopathology. In T. P. Beauchaine & S. P. Hinshaw (Eds.), Child and adolescent psychopathology (pp. 265–298). New Jersey: John Wiley & Sons Inc.
Cole, D. A., Tram, J. M., Martin, J. M., Hoffman, K. B., Ruiz, M. D., Jacquez, F. M., et al. (2002). Individual differences in the emergence of depressive symptoms in children and adolescents: a longitudinal investigation of parent and child reports. Journal of Abnormal Psychology, 111, 156–165. doi:10.1037/0021-843x.111.1.156.
Daley, S. E., & Hammen, C. (2002). Depressive symptoms and close relationships during the transition to adulthood: perspectives from dysphoric women, their best friends, and their romantic partners. Journal of Consulting and Clinical Psychology, 70, 129–141. doi:10.1037/0022-006x.70.1.129.
De Goede, I., Branje, S. J. T., & Meeus, W. H. J. (2009). Developmental changes in adolescents’ perceptions of relationships with their parents. Journal of Youth and Adolescence, 38, 75–88. doi:10.1007/s10964-008-9286-7.
Essau, C. A., & Barrett, P. (2001). Developmental issues in the assessment of anxiety. In C. A. Essau & F. Petermann (Eds.), Anxiety disorders in children and adolescents: Epidemiology, risk factors and treatment (pp. 75–110). New York: Taylor & Francis.
Furman, W., & Buhrmester, D. (1985). Children’s perceptions of the personal relationships in their social networks. Developmental Psychology, 21, 1016–1024. doi:10.1037/0012-1649.21.6.1016.
Gruber, J., Kogan, A., Quoidbach, J., & Mauss, I. B. (2013). Happiness is best kept stable: positive emotion variability is associated with poorer psychological health. Emotion, 13, 1–6. doi:10.1037/a0030262.
Hale, W. W., III, Engels, R., & Meeus, W. H. J. (2006). Adolescent’s perceptions of parenting behaviours and its relationship to adolescent generalized anxiety disorder symptoms. Journal of Adolescence, 29, 407–417. doi:10.1016/j.adolescence.2005.08.002.
Hoeksma, J. B., Sep, S., Vester, F., Groot, P., Sijmons, R., & De Vries, J. (2000). The electronic mood device: design, construction, and application. Behavior Research Methods, 32, 322–326. doi:10.3758/BF03207801.
Kendall, P. C., Hedtke, K. A., & Aschenbrand, S. G. (2006). Anxiety disorders. In D. A. Wolfe & E. J. Mash (Eds.), Behavioral and emotional disorders in adolescents. Nature, assessment, and treatment (pp. 259–299). New York: The Guilford Press.
Kendler, K. S., & Gardner, C. O. (2011). A longitudinal etiologic model for symptoms of anxiety and depression in women. Psychological Medicine, 41, 2035–2045. doi:10.1017/S0033291711000225.
Larsen, R. J. (1987). The stability of mood variability: a spectral analytic approach to daily mood assessments. Journal of Personality and Social Psychology, 52, 1195–1204. doi:10.1037/0022-3514.52.6.1195.
Larson, R. W., Csikszentmihalyi, M., & Graef, R. (1980). Mood variability and the psychosocial adjustment of adolescents. Journal of Youth and Adolescence, 9, 469–490. doi:10.1007/BF02089885.
Larson, R. W., Moneta, G., Richards, M. H., & Wilson, S. (2002). Continuity, stability, and change in daily emotional experience across adolescence. Child Development, 73, 1151–1165. doi:10.1111/1467-8624.00464.
Laursen, B., & Collins, W. A. (2009). Parent—child relationships during adolescence. In R. M. Lerner & L. Steinberg (Eds.), Handbook of adolescent psychology (3rd ed., pp. 3–42). Hoboken, NJ: Wiley.
Lewinsohn, P. M., Zinbarg, R., Seeley, J. R., Lewinsohn, M., & Sack, W. H. (1997). Lifetime comorbidity among anxiety disorders and between anxiety disorders and other mental disorders in adolescents. Journal of Anxiety Disorders, 11, 377–394. doi:10.1016/S0887-6185(97)00017-0.
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press.
MacKinnon, D. P., Lockwood, C. M., & Williams, J. (2004). Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. doi:10.1207/s15327906mbr3901_4.
McLeod, B. D., Wood, J. J., & Weisz, J. R. (2007). Examining the association between parenting and childhood anxiety: a meta-analysis. Clinical Psychology Review, 27, 155–172. doi:10.1016/j.cpr.2006.09.002.
Muris, P. (2002). Relationships between self-efficacy and symptoms of anxiety disorders and depression in a normal adolescent sample. Personality and Individual Differences, 32, 337–348. doi:10.1016/S0191-8869(01)00027-7.
Muris, P., Merckelbach, H., Mayer, B., & Prins, E. (2000). How serious are common childhood fears? Behaviour Research and Therapy, 38, 217–228. doi:10.1016/S0005-7967(98)00204-6.
Murray, G., Allen, N. B., & Trinder, J. (2002). Longitudinal investigation of mood variability and the FFM: neuroticism predicts variability in extended states of positive and negative affect. Personality and Individual Differences, 33, 1217–1228. doi:10.1016/S0191-8869(01)00217-3.
Muthén, L. K., & Muthén, B. O. (1998–2010). Mplus user’s guide. Sixth Edition. Los Angeles, CA: Muthén & Muthén.
Neumann, A., van Lier, P. A. C., Frijns, T., Meeus, W. H. J., & Koot, H. M. (2011). Emotional dynamics in the development of early adolescent psychopathology: a one-year longitudinal study. Journal of Abnormal Child Psychology, 39, 657–669. doi:10.1007/s10802-011-9509-3.
Phillips, K., & Power, M. (2011). Emotion regulation. In R. J. R. Levesque (Ed.), Encyclopedia of adolescence (pp. 825–832). New York: Springer.
Pine, D. S., Cohen, P., Gurley, D., Brook, J., & Ma, Y. (1998). The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry, 55, 56–64. doi:10.1001/archpsyc.55.1.56.
Podsakoff, P. M., & Organ, D. W. (1986). Self-reports in organizational research: problems and prospects. Journal of Management, 12, 531–544. doi:10.1177/014920638601200408.
Rathus, J. H., & Miller, A. L. (2002). Dialectical behavior therapy adapted for suicidal adolescents. Suicide and Life-Threatening Behavior, 32, 146–157. doi:10.1521/suli.32.2.146.24399.
Reynolds, W. M. (2002). Reynolds adolescent depression scale—2nd edition: Professional manual. Lutz, FL: Psychological Assessment Resources.
Roemer, L., Molina, S., & Borkovec, T. D. (1997). An investigation of worry content among generally anxious individuals. Journal of Nervous and Mental Disease, 185, 314–319. doi:10.1097/00005053-199705000-00005.
Rosenblum, G. D., & Lewis, M. (2003). Emotional development in adolescence. In G. R. Adams & M. Berzonsky (Eds.), Blackwell handbook of adolescence (pp. 269–289). Oxford: Blackwell Publishing Ldt.
Rudolph, K. D., Flynn, M., & Abaied, J. L. (2008). A developmental perspective on interpersonal theories of youth depression. In J. R. Z. Abela & B. L. Hankin (Eds.), Handbook of depression in children and adolescents (pp. 79–102). New York: Guilford Press.
Satorra, A., & Bentler, P. M. (2001). A scaled difference chi-square test statistic for moment structure analysis. Psychometrika, 66, 507–514. doi:10.1007/BF02296192.
Seligman, L. D., & Ollendick, T. H. (1998). Comorbidity of anxiety and depression in children and adolescents: an integrative review. Clinical Child and Family Psychology Review, 1, 125–144. doi:10.1037/0033-2909.111.2.244.
Sheeber, L., Hops, H., Alpert, A., Davis, B., & Andrews, J. (1997). Family support and conflict: prospective relations to adolescent depression. Journal of Abnormal Child Psychology, 25, 333–344. doi:10.1023/a:1025768504415.
Silk, J. S., Steinberg, L., & Morris, A. S. (2003). Adolescents’ emotion regulation in daily life: links to depressive symptoms and problem behavior. Child Development, 74, 1869–1880. doi:10.1046/j.1467-8624.2003.00643.x.
Silk, J. S., Forbes, E. E., Whalen, D. J., Jakubcak, J. L., Thompson, W. K., Ryan, N. D., et al. (2011). Daily emotional dynamics in depressed youth: a cell phone ecological momentary assessment study. Journal of Experimental Child Psychology, 110, 241–257. doi:10.1016/j.jecp.2010.10.007.
Simpson, E. E., McConville, C., Rae, G., O’Connor, J. M., Stewart-Knox, B. J., Coudray, C., et al. (2008). Salivary cortisol, stress and mood in healthy older adults: the Zenith study. Biological Psychology, 78, 1–9. doi:10.1016/j.biopsycho.2007.12.001.
Sowislo, J. F., & Orth, U. (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological Bulletin, 139, 213–240. doi:10.1037/a0028931.
Stark, K. D., Humphrey, L. L., Crook, K., & Lewis, K. (1990). Perceived family environments of depressed and anxious children: child’s and maternal figure’s perspectives. Journal of Abnormal Child Psychology, 18, 527–547. doi:10.1007/BF00911106.
Stringaris, A., & Goodman, R. (2009). Mood lability and psychopathology in youth. Psychological Medicine, 39, 1237–1245. doi:10.1017/S0033291708004662.
Van der Giessen, D., Branje, S., & Meeus, W. Perceived autonomy support from parents and best friends: Longitudinal associations with adolescents’ depressive symptoms. Social Development. (in press)
van Eijck, F., Branje, S., Hale, W. W., III, & Meeus, W. (2012). Longitudinal associations between perceived parent-adolescent attachment relationship quality and generalized anxiety disorder symptoms in adolescence. Journal of Abnormal Child Psychology, 40, 871–883. doi:10.1007/s10802-012-9613-z.
Van Oort, F. V. A., Greaves-Lord, K., Verhulst, F. C., Ormel, J., & Huizink, A. C. (2009). The developmental course of anxiety symptoms during adolescence: the TRAILS study. Journal of Child Psychology and Psychiatry, 50, 1209–1217. doi:10.1111/j.1469-7610.2009.02092.x.
Watson, D., & Clark, L. A. (1984). Negative affectivity: the disposition to experience aversive emotional states. Psychological Bulletin, 96, 465–490. doi:10.1037/0033-2909.96.3.465.
Zimmer-Gembeck, M. J., & Collins, W. A. (2003). Autonomy development during adolescence. In G. R. Adams & M. D. Berzonsky (Eds.), Blackwell handbook of adolescence (pp. 174–204). Oxford: Blackwell Publishing Ldt.
Acknowledgments
Data of the RADAR study were used. RADAR has been financially supported by main grants from the Netherlands Organisation for Scientific Research (GB-MAGW 480-03-005), and Stichting Achmea Slachtoffer en Samenleving (SASS), and various other grants from the Netherlands Organisation for Scientific Research, the VU University Amsterdam and Utrecht University.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 64 kb)
Rights and permissions
About this article
Cite this article
Maciejewski, D.F., van Lier, P.A.C., Neumann, A. et al. The Development of Adolescent Generalized Anxiety and Depressive Symptoms in the Context of Adolescent Mood Variability and Parent-Adolescent Negative Interactions. J Abnorm Child Psychol 42, 515–526 (2014). https://doi.org/10.1007/s10802-013-9797-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-013-9797-x