Abstract
This study aimed to describe the course of early onset eating disorders in a population-based sample followed from 14 to 20 years; identify variables that could account for the persistence of eating disorders from 14 to 20 years; and describe outcome of early onset eating disorders with reference to general and psychological functioning at age 20. Participants (N = 1,383; 49 % male) were drawn from the Western Australian Pregnancy Cohort (Raine) Study, which has followed children from pre-birth to young adulthood. Eating disorder symptoms were assessed using an adapted version of the Eating Disorder Examination-Questionnaire, at ages 14, 17 and 20. At age 14, 70 participants met DSM-IV criteria for a binge eating or purging eating disorder. Nearly half (44 %) of these adolescents ceased to meet criteria for an eating disorders at ages 17 and 20, whilst one-quarter still met criteria for an eating disorder at age 20 and one-fifth met criteria for an eating disorder at all three time points. Purging at age 17 and externalising behaviour problems at age 14 were the strongest predictors of eating disorder persistence to age 20. Participants who experienced a persistent eating disorder were less likely to complete high school than other participants, and reported pronounced depressive and anxiety symptoms at age 20. This study provides new data the course and outcome of early onset eating disorders at a population level. Behavioural difficulties in early adolescence and purging in middle adolescence may predict persistent eating pathology to young adulthood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Population-based studies suggest that up to 15 % of women may experience an eating disorder (anorexia nervosa [AN], bulimia nervosa [BN], or an eating disorder not otherwise specified [EDNOS]) in their lifetime (Kjelsas et al. 2004; Wade et al. 2006). Currently, detailed data regarding the course of these disorders in the community are rare. Outcome has predominantly been examined in treatment-seeking groups, where, on average, full physical and psychological recovery is achieved by 50 % of adult cases and 75 % of adolescent cases, when followed up for 5 to 10 years post-treatment (Ben-Tovim et al. 2001; Berkman et al. 2007; Eisler et al. 2007; Lock et al. 2006; Steinhausen 2002; Steinhausen and Weber 2009). However, treatment-seeking samples are likely to over-represent severe presentations. Additionally, these samples can not provide information on the natural course of eating disorders when treatment is not provided.
Studies on the natural course of eating disorders in adults have utilised two types of participants: those who have received no form of eating disorder treatment, and those who have received treatment in non-specialist (primary care) settings only. Outcome appears to be similar across these two groups (Keski-Rahkonen et al. 2009; Keski-Rahkonen et al. 2007). For BN, reported remission rates range from 50 to 75 % over 5 to 20 year follow-up periods (Fairburn et al. 2000; Grilo et al. 2007; Keel et al. 2010; Keski-Rahkonen et al. 2009). Few studies have followed community-based participants with AN, but two retrospective studies of adult women found remission rates of 67–75 % (Keski-Rahkonen et al. 2007; Wade et al. 2006). The difficulty with these studies is that many adult participants will have developed eating disorder symptoms years before the initial period of observation. This precludes a reliable estimation of the true course of the disorder. As noted by others (Agras et al. 2009; Grilo et al. 2012), studies have also tended to focus on AN and BN to the exclusion of EDNOS. This is problematic when considering that EDNOS cases make up over half of the referrals to eating disorder services, and are broadly comparable to AN and BN cases in symptom severity and functional impairment (Fairburn and Bohn 2005; Hay et al. 2010). Prospective, population-based studies with adolescents, which consider all forms of clinically significant eating disorders, would allow for a more complete investigation of course and outcome.
Several community studies have been conducted using adolescent participants. Collectively, results suggest that adolescent eating disorders may be relatively time limited in a majority of cases, with remission rates ranging from 75 to 100 % over 1 to 10 year follow-up periods (Lewinsohn et al. 2000; Patton et al. 2003; Rastam et al. 2003; Stice et al. 2009). However, adolescents who experience eating disorders may be at risk for subsequent recurrences of eating pathology (Stice et al. 2009), experience persistent sub-clinical eating disorder symptoms (Rastam et al. 2003; Stice et al. 2009), and/or experience non-eating related psychiatric difficulties that persist into young adulthood (Lewinsohn et al. 2000; Patton et al. 2003; Rastam et al. 2003). Depressive and anxiety symptoms appear to be particularly common after eating disorder remission, and may affect half to three-quarters of young adults with an eating disorder history (Lewinsohn et al. 2000; Patton et al. 2003).
To date, only Stice et al. (2009) have considered the course and outcome of the full range of possible eating disorders. Their study followed adolescent females (N = 496) over 8 years and investigated full and partial AN and BN, as well as two forms of EDNOS: purging disorder (PD) and binge eating disorder (BED). High remission rates were observed for BN, BED and PD, but participants with BN and BED were more likely to experience symptom relapses than participants with PD. These results highlight the importance of attending to diagnostic differences when considering eating disorder course and outcome. The relatively new status of PD as a category of interest in DSM-5 (Keel et al. 2005) makes additional research on this disorder important.
Research is also needed to identify predictors of eating disorder outcome. Many adolescents may show natural reductions in eating pathology, but it is clear that not all adolescents will do so. Moreover, even when eating disorder symptoms do remit, other psychiatric difficulties may develop or persist (Lewinsohn et al. 2000). Identifying reliable predictors of these alternate trajectories would facilitate targeted prevention and intervention efforts for adolescents.
Given the above, the current study aimed to extend the evidence base on the natural course and outcome of eating disorders in the community, using prospective data from a population-based sample of male and female Australian adolescents. We focused on adolescent eating disorders that developed by age 14, and considered the full range of clinically significant eating disorders. Specific aims were to:
-
1.
Describe the course of early onset adolescent eating disorders in a population-based sample followed from 14 to 20 years.
-
2.
Identify variables that can account for the persistence of early onset eating disorders to age 20.
-
3.
Describe outcome from early onset eating disorders, in terms of general functioning, eating disorder symptoms, and depressive and anxiety symptoms at age 20.
Methods
Participants
Participants were drawn from the Western Australian Pregnancy Cohort (Raine) Study, a prospective cohort study of 2,868 live birth babies followed to 20 years of age. Details regarding the Raine Study have been published previously (Allen et al. 2009; Newnham et al. 1993). In brief, women (N = 2,900) were recruited from the antenatal booking clinics at King Edward Memorial Hospital for women (KEMH), the only public maternity hospital in Western Australia, between May 1989 and November 1991. Of the 2,900 women enrolled, 2,804 delivered live birth babies. Due to 64 multiple births, the initial cohort included 2,868 children. These children were assessed at birth and ages 1, 2, 3, 5, 8, 10, 14, 17 and 20 years.
The study had a primary focus on the 14, 17 and 20-year follow-ups, as detailed eating disorder data were collected at these assessments. Eating disorder data were available for 1,598 participants at age 14; 1,242 participants at age 17; and 1,243 participants at age 20. We focused on participants with data at age 14 and at least one of the subsequent follow-ups, giving an effective sample size of 1,383 (49 % male). This represents 76 % of the participants who completed at least one of the 14 through 20-year assessments (N = 1,878) and 59 % of the participants who were eligible for participation in the 14 through 20-year assessments (i.e., not deceased or lost to follow-up prior to age 14; N = 2,344). The mean age of the sample was 14.01 years (SD = 0.19, range = 13.00–15.08) at the 14-year assessment, 16.92 years (SD = 0.24, range = 15.0–18.2) at the 17-year assessment, and 20.01 years (SD = 0.44, range = 19.00–22.08) at the 20-year assessment.
Procedure
Questionnaire packages were posted to adolescents at the 14, 17 and 20-year assessments, for at-home completion prior to attendance at a face-to-face assessment session. Adolescents’ height and weight were measured during the face-to-face assessment as part of a broader physical examination. Body mass index (BMI) was calculated using the standard formula (weight [kg]/height [m]2). Adolescent assessment measures were selected to assess psychosocial variables previously linked to eating disorder development, maintenance and/or outcome (e.g., see Stice 2002; Wade et al. 2012).
Family sociodemographic characteristics were reported by parents using self-report questionnaires. As with the adolescent questionnaires, these were posted to parents for at-home completion prior to a face-to-face assessment session.
Data collection occurred in accordance with Australian National Health and Medical Research Council Guidelines for Ethical Conduct and was approved by the ethics committees of KEMH and Princess Margaret Hospital for Children. Written consent was obtained from adolescents at age 20, and from parents on behalf of adolescents at ages 14 and 17.
Adolescent Measures
Eating Disorder Symptoms at 14, 17 and 20 Years
Eating disorder symptoms were assessed using 24 self-report items adapted from the Child Eating Disorder Examination (ChEDE) (Bryant-Waugh et al. 1996) and Eating Disorder Examination-Questionnaire (EDE-Q) (Fairburn and Beglin 1994). These 24 items were self-report, as per the EDE-Q, but language was simplified or clarified when there was the possibility of confusion for 14-year-old adolescents. Response options were also simplified and the same four response options were used for all items: 0 (not at all), 1 (some of the time [once per week/a few times a month]), 2 (a lot of the time [a few times a week]), and 3 (most of the time [every day or nearly every day]). Questions referred to the previous month and the same items were used at all assessment points. The validity of a simplified EDE-Q rating scale for youth has been established (Goldschmidt et al. 2007) and support exists for the validity of self-report eating disorder assessment more generally (Berg et al. 2011; Berg et al. 2012a, b; Fairburn and Beglin 1994; Keel et al. 2002).
The 24 self-report items assessed for DSM-IV-TR diagnostic criteria for AN, BN and BED, with the exception that items referred to 1 month rather than 3 to 6 months. Others have found good convergence between EDE-Q assessment with a 1 month time frame and interview assessment with a 3 to 6 month time frame, in terms of eating disorder detection and classification (Berg et al. 2012a). One limitation of the EDE-Q, however, is that it does not assess all of the diagnostic criteria for BED. Specifically, it does not determine whether at least three of the following symptoms are present: rapid eating, eating until uncomfortably full, eating large amounts when not hungry, eating alone, or feeling disgusted, depressed or guilty after overeating. When these criteria are omitted from diagnostic decision making, the prevalence of BED is inflated (Berg et al. 2012b). To address this, we included the over-evaluation of weight and shape as a requirement for BED diagnosis. Others have found over-evaluation to be strongly associated with eating disorder psychopathology and distress about binge eating in samples of binge eaters (Hrabosky et al. 2007; Mond et al. 2007), and to reliably distinguish between individuals with BED and those who report binge eating without clinical impairment.
Table 1 summarises the diagnostic criteria used to define full and partial eating disorders in this study. Additional details are available in Allen et al. (2009). The mean of items relating to dietary restraint and eating, weight and shape concerns was computed as a global index of eating disorder psychopathology (α 0.90, 0.93 and 0.91, at ages 14, 17 and 20 respectively).
Anxiety and Depressive Disorders at 14, 17 and 20 Years
Items regarding diagnosed anxiety and depressive disorders were included in the 14, 17 and 20-year Raine Study questionnaire packages. Adolescents were asked “Do you have now, or have you had in the past, any of the following health professional diagnosed medical conditions or health problems?” (emphasis in the original). “Anxiety problems” and “depression” were listed as two examples. If adolescents endorsed the item, they were asked to indicate when the problem occurred and who diagnosed the difficulties.
Psychological Symptoms at 14 and 17 Years
The self-report Beck Depression Inventory for Youth (BDI-Y) (Beck et al. 2001) was used to assess depressive symptoms at ages 14 and 17. The BDI-Y is an adolescent adaptation of the adult Beck Depression Inventory-2 (Beck et al. 1996) and has established psychometric properties (Beck et al. 2001; Eack et al. 2008). Alpha coefficients in this sample were 0.97 at age 14 and 0.94 at age 17.
The Youth Self-Report (YSR) (Achenbach 1991) was used to assess internalising and externalising behaviour problems at ages 14 and 17. This is a self-report version of the Child Behavior Checklist (CBCL) (Achenbach 1991) and generates Internalising and Externalising Problem scores. These overall scores are formed from eight specific, empirically derived sub-scales: Anxious/Depressed, Withdrawn/Depressed, Somatic Complaints and Social Problems as indices of Internalising Problems, and Thought Problems, Attention Problems, Rule-Breaking Behaviour (Delinquency Problems) and Aggressive Behaviour as indices of Externalising Problems. The YSR is widely used and has been established as psychometrically sound (Achenbach 1991; Johnson et al. 1999). In this sample, alpha coefficients for the overall Internalising and Externalising Problem scales were 0.74 and 0.79 at age 14, and 0.77 and 0.79 at age 17.
The Global Self-Worth subscale of the Self-Perception Profile for Adolescents (SPPA) (Harter 1988) was used to assess self-esteem at age 14 (α in this sample 0.84), and the Rosenberg Self-Esteem Scale was used at age 17 (α in this sample 0.89). Both measures are accepted as reliable and valid indices of global self-esteem (Shevlin et al. 1995; Trent et al. 1994).
Psychological Symptoms at 20 Years
The 21-item Depression Anxiety Stress Scale (DASS) (Lovibond and Lovibond 1995) was used to assess depressive, anxiety and stress symptoms at age 20. The DASS has well-established psychometric properties, in clinical and non-clinical samples (Henry and Crawford 2005; Ng et al. 2007), and alpha coefficients in this sample were high (0.79 to 0.89).
General Functioning at 20 Years
The 12-item Short-Form Health Survey-12 (SF-12) (Ware et al. 1996) was used to assess physical and mental quality of life at age 20. The SF-12 is a reliable, valid and practical alternative to the longer SF-36 when assessing quality of life (Salyers et al. 2000; Ware et al. 1996). It makes use of norm-based scoring with a population mean of 50 (SD = 10). Participants also completed questions on health service utilisation, education, and employment status as part of the 20-year Raine Study questionnaire.
Family Measures
Parents (typically mothers) reported on family income, parental employment, parental status (i.e., father living at home), family functioning, parenting style, parent mental health, family exposure to stressful events, parent body mass index, and child internalising and externalising mental health problems (using the parent-report CBCL) at the 5, 8, 10, and 14-year Raine Study follow-ups. Family data from the 5, 8 and 10-year assessments were used for comparisons between participants in the current study and those lost to follow-up prior to adolescence. Family income at age 14 was used as an indicator of sociodemographic status for participants in the current study. Income was dichotomised into low vs. medium-high income categories, where ‘low income’ included the lowest two Australian income quintiles.
Statistical Analysis
Preliminary Analyses
Independent-samples t-tests were used to determine if participants included in this study (N = 1,383) differed in meaningful ways from participants who took part in none (n = 961) or only one (n = 495) of the adolescent assessments. Participants were compared on family, parent and psychosocial variables at ages 5, 8 and 10 years. Adolescent eating disorder symptoms were also compared across participants who provided data at two or more adolescent assessment points and those who took part in only one adolescent assessment.
After data screening, EM imputation using maximum likelihood estimation was used to impute missing eating disorder data for participants who completed two out of three adolescent assessments. Imputation was conducted using established principles and techniques (Kenwood and Carpenter 2007; Schafer and Graham 2002) and is described in greater detail below.
Core Analyses
In recognition of the small group sizes, non-parametric and exact tests were used when possible. We also report 95 % confidence intervals (CI) for percentages. We report mean scores instead of medians for ease of interpretation.
To address Aim 1, participants who met full or partial criteria for an eating disorder at age 14 were classified according to their eating disorder status at ages 17 and 20. Changes in diagnostic status over time were considered at an overall level, for full and partial eating disorder cases separately, and for diagnostic sub-groups separately. Three broad participant groups were created: participants experiencing a persistent, unremitting eating disorder (full/partial disorder at 14, 17, and 20), participants experiencing a relapsing, late remitting or partially remitting eating disorder (full/partial eating disorder at 14 and 20; full/partial eating disorder at 14 and 17; or a full/partial eating disorder at 14 with sub-threshold eating disorder symptoms at 17 and 20), and participants experiencing an early remitting and non-relapsing eating disorder (full/partial disorder at 14 with no eating disorder and no sub-threshold symptoms at 17 and 20).
To address Aim 2, two sets of analyses were undertaken. Both were limited to the participants who met full or partial criteria for an eating disorder at age 14. First, Kruskal-Wallis non-parametric and chi square tests were used to compare the three eating disorder groups identified above on 14 and 17-year eating disorder symptoms, depressive symptoms, internalising and externalising problems, self-esteem, BMI, and demographic information. Identified between-group differences were followed up using Mann-Whitney-U non-parametric tests (for the Kruskal-Wallis comparisons) or Fisher’s Exact tests (for the categorical chi square comparisons). These analyses sought to identify variables that could distinguish between adolescents who did and did not experience persistent eating pathology.
Second, classification tree analysis using the CHAID method (Ripley 1996) was used to identify the 14 and 17-year variables that best accounted for eating disorder status at age 20 (full or partial eating disorder vs. sub-threshold symptoms vs. no disorder). Categorical predictor variables included participant sex; eating disorder status at 14 and 17 years; specific eating disorder diagnosis at 14 and 17 years; and the presence of regular objective binge eating (at least a few times per month), regular fasting, regular hard exercise for weight control, and any purging (any vomiting or laxative misuse) at 14 and 17 years. Continuous predictor variables included scores for global eating disorder symptoms; depressive symptoms; self-esteem; internalising and externalising problems; and BMI at 14 and 17 years. These analyses sought to identify the variables that could best account for eating disorder status at age 20, amongst adolescents who experienced an eating disorder at age 14.
To address Aim 3, Kruskal-Wallis and chi square tests were used to compare functioning at age 20 across the three eating disorder groups described above and two additional control groups. The first control group consisted of participants with a 20-year depressive or anxiety disorder as diagnosed by a health care professional (‘psychiatric control group’). The second control group consisted of participants with no diagnosed depressive or anxiety disorder, currently or in the past (‘general control group’). These groups were created on the basis of responses to the Raine Study questionnaire items on diagnosed depressive and anxiety disorders. Participants who reported a current (20-year) diagnosis of a depressive or anxiety disorder, and who had no identified current or past eating disorder, were included in the psychiatric control group (n = 68). Participants who reported no current or past diagnosis of a depressive or anxiety disorder, and who had no identified current or past eating disorder, were included in the general control group (n = 910). Participants diagnosed with a depressive or anxiety disorder prior to age 20 (but not at age 20) were excluded. Participants who developed an eating disorder after age 14 were also excluded. Participant groups were compared on 20-year eating disorder symptoms, depressive, anxiety and stress symptoms, quality of life, health service utilisation, educational attainment, and employment status. Again, identified between-group differences were followed up using Mann-Whitney-U tests or Fisher’s Exact tests.
All analyses were conducted in SPSS Statistics Version 19. Alpha was set at p < 0.05. Whilst a lower alpha level would have reduced the likelihood of Type I error arising from the large number of planned comparisons, it would have increased the likelihood of Type II error due to the small size of the eating disorder sample. Given the clinical significance of identifying predictors of eating disorder outcome, we retain an alpha level of 0.05 and refer to 95 % CI to facilitate the interpretation of the results.
Results
Preliminary Analyses
Participant Characteristics
Compared to participants included in this study (i.e., those who completed two or more adolescent assessments), participants who completed no adolescent assessments were significantly more likely to be from single-parent families at ages 5 (Χ 2 [1] = 17.13, p < .001), 8 (Χ 2 [1] = 23.29, p < .001), and 10 (Χ 2 [1] = 10.51, p < .001) years; were significantly less likely to have employed parents at ages 5 (Χ 2 [1] = 15.51, p < .001), 8 (Χ 2 [1] = 13.96, p < .001), and 10 (Χ 2 [1] = 24.19, p < .001) years; had significantly lower family incomes at ages 5 (t[1,724] = 5.10, p < .001), 8 (t[1,636] = 5.38, p < .001), and 10 (t[1,578] = 4.67, p < .001) years; and had significantly higher CBCL Externalising Problem scores at ages 5 (t[1,738] = 2.76, p = .007), 8 (t[1,656] = 4.22, p < .001), and 10 (t[1,610] = 2.94, p = .003) years. Results were similar for participants who completed one adolescent assessment, with the exception that this group was not more likely to be from a single parent family than participants who completed two or more adolescent assessments. These findings are consistent with the tendency for socially disadvantaged families to be lost to follow-up over time.
When comparing eating disorder data across participants who completed one adolescent assessment (excluded from the current study) and those who completed two or more (included in the current study), there were no significant between-group differences in eating disorder symptom scores, or in the proportion of participants meeting criteria for an eating disorder (ps = .19–.99).
Data Imputation
Missing eating disorder data were imputed for participants who completed two of the three adolescent assessments, using EM imputation with maximum likelihood estimation. Data were screened for patterns of missing variables prior to imputation. No evidence was found to suggest that data were not missing at random and Little’s MCAR test was non-significant (Χ 2 [1,399] = 1,376, p = .66). Data were imputed for 281 participants in total (141 participants at age 17 and 140 participants at age 20). The original raw dataset and imputed EM dataset were highly comparable in terms of estimated means and standard deviations for the eating disorder variables, and in terms of associations between eating disorder variables and psychosocial variables. All subsequent analyses make use of the full, imputed data set. The pattern of results was identical when analyses were conducted using the raw data, with the exception that some results did not reach statistical significance when group sizes were smaller.
Eating Disorder Diagnoses at age 14
There were 74 participants (5.4 % of the sample) who met full (n = 36; 2.6 %) or partial (n = 38; 2.8 %) criteria for an eating disorder at age 14. A further 51 participants (3.7 %) reported sub-threshold eating disorder symptoms at age 14. The remaining 1,258 participants (91.0 %) were classified as non-eating disorder cases. Within the eating disorder group, numbers for each diagnostic category were as follows: AN = 1, BN = 8, BED = 5, PD = 22, partial AN = 3, partial BN = 8, partial BED = 12, and partial PD = 15. Due to the small number of AN-like cases (n = 4), subsequent analyses were limited to participants with BN (n = 16), BED (n = 17) or PD (n = 37) disorders.
The eating disorder (n = 70) and non-eating disorder (n = 1,258) groups did not differ significantly in age (t [1,271] = 6.03, p = .84). As might be expected, female participants were over-represented in the eating disorder group relative to the non-eating disorder group (85 % vs. 45 %) (Fisher’s exact p < .001). Low family income was also over-represented in the eating disorder group, with 26 % of these participants having low family income at age 14 compared to 16 % of the participants without an eating disorder (Fisher’s exact p = .006).
Only 16 % (n = 11) of the eating disorder group reported being treated for an eating disorder by age 20. Rates of treatment did not vary significantly across participants with full and partial eating disorders, across different diagnostic subgroups, or across participants who did and did not experience persistent eating disorder symptoms through to age 17 or 20 (ps = .12–.99).
Aim 1: The Course of Adolescent Eating Disorders
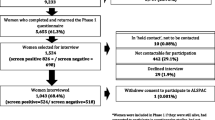
Figure 1 summarises the course of eating disorders from age 14 to age 17, and age 17 to age 20, for those participants with a binge eating or purging disorder at baseline.
Overall, 19 % (n = 13/70; 95 % CI [−10 %, 28 %]) of the 14-year eating disorder sample experienced a persistent eating disorder from 14 to 20 years, whilst 44 % (n = 31; 95 % CI [32 %, 56 %]) experienced an early remitting and non-relapsing course and 37 % (n = 26; 95 % CI [26 %, 48 %]) experienced a late remitting course (eating disorder at 14 and 17 but not 20 years; n = 8) or a partially remitting or relapsing course (n = 18).
Results were similar when analyses were run separately for adolescents with full (n = 35) and partial (n = 35) eating disorders at baseline. For the 14-year full eating disorder cases, 23 % of participants (n = 8; 95 % CI [9 %, 37 %]) experienced a persistent eating disorder from 14 to 20 years whilst 43 % (n = 15; 95 % CI [27 %, 59 %]) experienced an early remitting and non-relapsing course. For the 14-year partial eating disorder cases, 14 % of participants (n = 5; 95 % CI [3 %, 25 %]) experienced a persistent eating disorder from 14 to 20 years whilst 46 % (n = 16; 95 % CI [30 %, 62 %]) experienced an early remitting and non-relapsing course. Differences relative to the full eating disorder cases were not statistically significant (p = .23–.99).
As shown in Fig. 1, the likelihood of symptom remission reduced over time. Whereas 49 % of adolescents moved from an eating disorder at age 14 to no symptoms at age 17 (n = 34/70; 95 % CI [37 %, 61 %]), only 29 % of adolescents with an eating disorder at ages 14 and 17 moved to no symptoms at age 20 (n = 8/28; 95 % CI [12 %, 46 %]) (McNemar Χ 2 [1] = 6.38, p = .01).
Table 2 summarises disorder course for BN, BED and PD separately. Full and partial cases were combined for these analyses. There was a significant effect of 14-year diagnosis on eating disorder persistence to age 17 (Χ 2 [2] = 7.01, p = .03) but not to age 20 (Χ 2 [2] = 0.01, p = .99). Follow-up analyses indicated that this overall effect stemmed from BED participants being significantly more likely than PD participants to experience a persistent disorder to age 17 (Fisher’s exact p = .01). Participants with BED also showed a tendency to transition to BN over time, with 45 % of the 14-year participants with a BED-like disorder developing compensatory behaviours, and meeting full or partial criteria for BN, by age 17 (see Table 2).
Aim 2: Predictors of Eating Disorder Persistence
Table 3 summarises between-group differences on 14 and 17-year variables, for participants with a persistent (n = 13), relapsing or late/partial remitting (n = 26), or early remitting and non-relapsing (n = 31) eating disorder. Participants in the persistent eating disorder group were significantly more likely to report externalising problems at age 14, relative to participants without persistent eating pathology, and to report heightened eating disorder symptoms, depressive symptoms, internalising problems, externalising problems, and low self-esteem at age 17. They were also more likely to be female.
Classification tree analysis was conducted to identify the 14 and 17-year variables that could account for eating disorder status at age 20. Purging at age 17 formed the first branch (Χ 2 [1] = 33.03, p < .001), with 73 % of adolescents who reported purging at age 17 going on to meet full or partial criteria for an eating disorder at age 20, compared to 11 % of adolescents who did not report purging (see Fig. 2). Externalising problems at age 14 formed the second and final branch (Χ 2 [1] = 10.24, p = .02), with 29 % of adolescents with an Externalising Problem score >58 at age 14 (and no purging at age 17) going on to meet criteria for an eating disorder at age 20. This compared to 3 % of the adolescents with an Externalising Problem score ≤58 (see Fig. 2). A T-score of 58 on the YSR approximates the 80th percentile against community norms.
This model correctly classified all of the non-eating disorder cases at age 20, and 65 % of the eating disorder cases at age 20 (estimate = 0.20, SE = 0.05). Prediction accuracy was slightly biased to PD participants. For the 14-year BN and BED cases, 50 % of those who continued to meet criteria for an eating disorder at age 20 were correctly classified (n = 2/4 for both BN and BED), whilst for the 14-year PD cases, 78 % of those who continued to meet criteria for an eating disorder at age 20 were correctly classified (n = 7/9).
Follow-up analyses were conducted to identify the specific variables that may account for the Externalising Problem results. As noted, the Externalising Problem scale is made up of four subscales: Thought Problems, Attentional Problems, Rule-Breaking Behaviour, and Aggressive Behaviour. Rule-Breaking Behaviour age 14 distinguished between adolescents who continued to meet criteria for an eating disorder at age 20 and those who did not (Kruskal-Wallis Χ 2 [2] = 7.00, p = .03). Significant effects were not identified for Thought Problems (Kruskal-Wallis Χ 2 [2] = 2.08, p = .267) or Attentional Problems (Kruskal-Wallis Χ 2 [2] = 4.10, p = .189). The effect for Aggressive Behaviour approached significance (Kruskal-Wallis Χ 2 [2] = 6.15, p = .05).
Aim 3: Outcome of Eating Disorders
Between-group differences on 20-year outcome variables are summarised in Table 4. Effect sizes for continuous outcome variables are included in the footnote to Table 4. All identified effects were medium to large in magnitude.
Significant between-group differences remained when analyses were re-run using multivariate analysis of variance with family income at age 14 and BMI at age 20 as covariates.
Discussion
This study had three primary aims: to describe the course of early onset eating disorders in a population-based sample followed from 14 to 20 years; to identify variables that could account for the persistence of early onset eating disorders from 14 to 20 years; and to describe outcome from early onset eating disorders with reference to eating disorder psychopathology and general and psychosocial functioning at age 20. Due to the small number of participants with AN, our results relate to binge eating and purging-type eating disorders. The observed prevalence of these disorders at age 14 (approximately 1 in 20 adolescents) compares well to rates reported elsewhere (e.g., Patton et al. 2003).
Aim 1: The Course of Eating Disorders
Of the participants with a binge eating or purging eating disorder at age 14, nearly half reported no notable eating disorder symptoms at ages 17 and 20. Approximately one-quarter met criteria for an eating disorder at the final assessment point, one-fifth met criteria for an eating disorder at all three assessment points, and one-third reported eating disorder symptoms at all three assessment points. These results are broadly consistent with findings from previous studies of adolescent and young adult participants (Lewinsohn et al. 2000; Stice et al. 2009), and suggest that symptom remission may be relatively common amongst community-based youth with eating disorders. Outcome was also comparable across participants with full and partial eating disorders, lending further support to the clinical significance of ‘EDNOS’ or ‘atypical’ eating disorders (Fairburn et al. 2007). Interestingly, however, eating disorder persistence was more common amongst participants with BED than participants with PD. The likelihood of symptom remission also reduced over time: half of the sample experienced eating disorder remission between 14 and 17 years, but only 29 % of the participants still experiencing an eating disorder at 17 years went on to achieve remission by 20 years.
Aim 2: Accounting for Eating Disorder Persistence
Compared to participants with an early remitting and non-relapsing eating disorder, we found that participants who experienced a persistent eating disorder were more likely to report high levels of externalising behaviour problems at age 14, and to report high levels of eating disorder symptoms, depressive symptoms, internalising problems and externalising problems, and low levels of self-esteem, at age 17. These results were extended in classification tree analyses, where purging at age 17 and externalising behaviour problems at age 14 emerged as the strongest predictors of eating disorder status at age 20.
Aim 3: Outcome from Adolescent Eating Disorders
As might be expected, outcome was least positive for adolescents who experienced a persisting eating disorder from 14 to 20 years. These participants were less likely to finish high school than other participants, and continued to report pronounced eating disorder symptoms at age 20. These participants also reported depressive, anxiety and stress symptoms, and impairments in mental health quality of life, that were equivalent to those for the psychiatric control group. Interestingly, general functioning in the relapsing or late/partial remitting group was not markedly compromised, despite this group continuing to report elevated eating disorder psychopathology. In contrast, the early remitting and non-relapsing eating disorder group reported elevated anxiety and stress symptoms, reduced mental health quality of life, and persisting sub-clinical eating disorder symptoms when compared to the general control group. Thus, as documented previously (e.g., Lewinsohn et al. 2000; Patton et al. 2003), sub-clinical eating disorder symptoms and psychological distress appear to persist at above-average levels amongst adolescents with a history of an eating disorder. The lack of marked psychological distress amongst adolescents in the relapsing or late/partial remitting group is worthy of additional research attention, and suggests that these cases may differ meaningfully from both persisting and fully remitting eating disorder trajectories. Identifying the variables that protect these participants from psychosocial impairment despite their ongoing eating disorder symptoms would be beneficial.
Key Implications
This research provides additional data on the course and outcome of early onset eating disorders in the community, and new data on possible predictors of eating disorder persistence across adolescence. Clinically, five main implications arise from the results.
First, there is a need for better eating disorder identification and targeted intervention for adolescents in the community. Although most of the 14-year eating disorder cases did not experience a persistent eating disorder, one in three reported some form of notable eating pathology at all assessment points and very few had received professional help for eating difficulties. The likelihood of symptom remission also reduced significantly after age 17. This highlights the importance of early intervention for adolescents who are at risk of persistent eating pathology. Achieving this requires that eating disorder cases are better detected, as an initial step, so that tailored management and treatment can occur.
Second, the natural course of full and partial eating disorders appears to be comparable, at least in adolescent samples, but remission rates may vary by diagnosis. In this early onset sample, participants with PD were significantly more likely to experience symptom remission than participants with BED. Stice et al. (2009) found similar results, with participants with PD showing better outcome than participants with BN and BED. This finding has implications for the nosology of PD, which is still a provisionally defined condition. Additional research with longer follow-up periods would help to determine whether adolescents with remitted PD are at risk for later recurrences of eating disorder pathology. Research with treatment-seeking samples would help to determine whether the patterns identified here are specific to community groups or generalise to participants receiving treatment.
Third, adolescents who experience persistent eating pathology appear to be at risk for poor general and psychological functioning at age 20. In this sample, this included lower rates of high school completion and pronounced depressive and anxiety symptoms. Again, these results highlight the importance of detecting high-risk eating disorder cases early, so that general as well as eating-specific difficulties may be addressed. Adolescent eating disorder treatments may also benefit from attending to comorbid difficulties after eating disorder symptoms have been addressed.
Fourth, adolescents who experience a time-limited eating disorder may still report psychological difficulties in other areas, particularly depression, in young adulthood. This may be associated with risk for a subsequent recurrence of an eating disorder, a pattern observed elsewhere (Stice et al. 2009), and/or contribute to ongoing impairments in mental health and general functioning.
Fifth, externalising behaviour problems may prospectively predict persistent eating pathology in youth. Given that these forms of behaviour are likely to draw parental or school-based attention, they may also provide markers for identifying high-risk adolescents in the community. In this sample, six items on the YSR Rule-Breaking Behaviour subscales strongly distinguished between the persisting and remitting eating disorder groups: running away from home, truanting from school, disobeying at school, using alcohol or drugs, spending time with trouble-makers, and destroying one’s own things. Most of these behaviours are observable and measurable. Moreover, similar behaviours, including delinquent behaviour and substance misuse, have previously been linked to eating disorder development in adolescence (Wonderlich et al. 2004). A recent study of adolescent girls also found a significant association between binge eating and purging disorders and later onset of substance misuse (Field et al. 2012). These results suggest that externalising problems should be considered in studies of eating disorder development, persistence and outcome. Research on the mechanisms that may underpin the identified effects would also be beneficial. This study did not assess personality traits, but rule-breaking behaviours may be associated with personality difficulties, particularly those associated with affective instability, mood intolerance and/or impulsivity. Previous studies have found that personality disorders in adults are not associated with the natural course of eating disorders (Grilo et al. 2003), so additional research is needed to determine if personality factors relate differentially to adolescent and adult outcomes. Again, this would have implications for prevention and intervention approaches in adolescence, which may need to be tailored to attend to personality variables and their consequences for behaviour and emotion.
Limitations
This study benefited from prospective, population-based data, attention to the full range of DSM-IV eating disorders, and the use of a psychiatric as well as general control group when evaluating 20-year outcome. Several limitations require consideration, however, including the reliance on self-report data, participant attrition, small group sizes for the eating disorder sub-groups, and large (and overlapping) confidence intervals for some findings. Personality assessment may also have allowed for further investigation of the mechanisms underpinning our externalising problem results.
Regarding attrition, the loss of disadvantaged families is a well-replicated phenomenon in longitudinal cohort studies (Wolke et al. 2009). In the Raine Study, attrition has served to increase the representativeness of the cohort over time, as the study initially over-sampled socially-disadvantaged women. Previous analyses have shown that participants who remained in the study to adolescence are broadly comparable to the Western Australian population on a range of sociodemographic indicators (Li et al. 2008). Despite this, replication of our results in other cohorts is important and would help to strengthen the findings observed here.
Small group sizes contributed to the broad confidence intervals observed for many of our findings. These indicate a lack of statistical certainty regarding the precise size or location of the value in question. Where confidence intervals overlap zero, or overlap between different groups, there is particular difficulty in drawing reliable conclusions about the nature of the data. For these reasons, we recommend a degree of caution when interpreting our results and, again, encourage replication in future studies. Future studies may also wish to collect data at narrower intervals, as episodes of relapse/remission may have occurred between our 3-yearly assessments points. As our results relate to adolescents with an early onset eating disorder, we do not draw conclusions regarding eating disorder course and outcome in participants who develop eating disorders in later adolescence or early adulthood.
Conclusions and Recommendations
In summary, this study adds to the small body of available data on the course of adolescent eating disorders at a population level, and provides new data regarding possible predictors of eating disorder outcome. Persistent eating disorders in this sample were predicted by purging behaviour at age 17, and externalising problem behaviour at age 14. By screening for eating disorders in the community, it may be possible to provide tailored intervention to reduce the likelihood of protracted eating disorder symptoms in adolescents who would otherwise be at risk for these. If an eating disorder is detected, assessment of comorbid difficulties (particularly externalising problems) may help to inform treatment planning, and regular monitoring of symptoms would then allow the intensity of support to be adjusted in accordance with individual need.
References
Achenbach, T. M. (1991). Integrative guide for the 1991 CBCL/4-18, YSR, and TRF profiles. Burlington: University of Vermont, Department of Psychiatry.
Agras, W., Crow, S. J., Mitchell, J. E., Halmi, K. A., & Bryson, S. (2009). A 4-year prospective study of eating disorder NOS compared with full eating disorder syndromes. International Journal of Eating Disorders, 42, 565–570.
Allen, K. L., Byrne, S. M., Forbes, D., & Oddy, W. H. (2009). Risk factors for full- and partial-syndrome early adolescent eating disorders: a population-based pregnancy cohort study. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 800–809.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory (2nd ed.). San Antonio: The Psychological Corporation.
Beck, S., Beck, A. T., & Jolly, J. (2001). Beck youth inventory. New York: Psychological Corporation.
Ben-Tovim, D. I., Walker, K., Gilchrist, P., Freeman, R., Kalucy, R., & Esterman, A. (2001). Outcome in patients with eating disorders: a 5-year study. The Lancet, 357, 1254–1257.
Berg, K. C., Peterson, C. B., Frazier, P., & Crow, S. J. (2011). Convergence of scores on the interview and questionnaire versions of the eating disorder examination: a meta-analytic review. Psychological Assessment, 23, 714–724.
Berg, K. C., Peterson, C. B., Frazier, P., & Crow, S. J. (2012a). Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. International Journal of Eating Disorders, 45, 428–438.
Berg, K. C., Stiles-Shields, E. C., Swanson, S. A., Peterson, C. B., Lebow, J., & Le Grange, D. (2012b). Diagnostic concordance of the interview and questionnaire versions of the eating disorder examination. International Journal of Eating Disorders, 45, 850–855.
Berkman, N. D., Lohr, K. N., & Bulik, C. M. (2007). Outcomes of eating disorders: a systematic review of the literature. International Journal of Eating Disorders, 40, 293–309.
Bryant-Waugh, R. J., Cooper, P. J., Taylor, C. L., & Lask, B. D. (1996). The use of the eating disorder examination with children: a pilot study. International Journal of Eating Disorders, 19, 391–397.
Eack, S. M., Singer, J. B., & Greeno, C. G. (2008). Screening for anxiety and depression in community mental health: the beck anxiety and depression inventories. Community Mental Health Journal, 44, 465–474.
Eisler, I., Simic, M., Russell, G. F. M., & Dare, C. (2007). A randomised controlled treatment trial of two forms of family therapy in adolescent anorexia nervosa: a five-year follow-up. Journal of Child Psychology and Psychiatry, 48, 552–560.
Fairburn, C. G., & Beglin, S. J. (1994). Assessment of eating disorders: interview or self-report questionnaire? International Journal of Eating Disorders, 16, 363–370.
Fairburn, C. G., & Bohn, K. (2005). Eating disorder NOS (EDNOS): an example of the troublesome “not otherwise specified” (NOS) category in DSM-IV. Behaviour Research and Therapy, 43, 691–701.
Fairburn, C. G., Cooper, Z., Doll, H. A., Norman, P., & O'Connor, M. E. (2000). The natural course of bulimia nervosa and binge eating disorder in young women. Archives of General Psychiatry, 57, 659–665.
Fairburn, C. G., Cooper, Z., Bohn, K., O'Connor, M. E., Doll, H. A., & Palmer, R. L. (2007). The severity and status of eating disorder NOS: Implications for DSM-V. Behaviour Research and Therapy, 45, 1705–1715.
Field, A. E., Sonneville, K. R., Micali, N., Crosby, R. D., Swanson, S. A., Laird, N. M., et al. (2012). Prospective association of common eating disorders and adverse outcomes. Pediatrics, 130, e289–e295.
Goldschmidt, A. B., Doyle, A. C., & Wilfley, D. E. (2007). Assessment of binge eating on overweight youth using a questionnaire version of the child eating disorder examination with instructions. International Journal of Eating Disorders, 40, 460–467.
Grilo, C. M., Sanislow, C. A., Shea, M., Skodol, A. E., Stout, R. L., Pagano, M. E., et al. (2003). The natural course of bulimia nervosa and eating disorder not otherwise specified is not influenced by personality disorders. International Journal of Eating Disorders, 34, 319–330.
Grilo, C. M., Pagano, M. E., Skodol, A. E., Sanislow, C., McGlashan, T. H., Gunderson, J. G., et al. (2007). Natural course of bulimia nervosa and of eating disorder not otherwise specified: 5-year prospective study of remissions, relapses, and the effects of personality disorder psychopathology. The Journal of Clinical Psychiatry, 68(5), 738–746.
Grilo, C. M., Pagano, M. E., Stout, R. L., Markowitz, J. C., Ansell, E. B., Pinto, A., et al. (2012). Stressful life events predict eating disorder relapse following remission: Six-year prospective outcomes. International Journal of Eating Disorders, 45, 185–192.
Harter, S. (1988). Manual for the self-perception profile for adolescents. Denver: University of Denver.
Hay, P., Buttner, P., Mond, J., Paxton, S. J., Rodgers, B., Quirk, F., et al. (2010). Quality of life, course and predictors of outcomes in community women with EDNOS and common eating disorders. European Eating Disorders Review, 18(4), 281–295.
Henry, J. D., & Crawford, J. R. (2005). The short-form versions of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44, 227–239.
Hrabosky, J. I., Masheb, R. M., White, M. A., & Grilo, C. M. (2007). Overvaluation of shape and weight in binge eating disorder. Journal of Consulting and Clinical Psychology, 75, 175–180.
Johnson, S., Barrett, P. M., Dadds, M. R., Fox, T., & Shortt, A. (1999). The diagnostic interview schedule for children, adolescents, and parents: initial reliability and validity data. Behaviour Change, 16, 155–164.
Keel, P., Crow, S. J., Davis, T. L., & Mitchell, J. E. (2002). Assessment of eating disorders: comparison of interview and questionnaire data from a long-term follow-up study of bulimia nervosa. Journal of Psychosomatic Research, 53, 1043–1047.
Keel, P. K., Haedt, A., & Edler, C. (2005). Purging disorder: an ominous variant of bulimia nervosa? International Journal of Eating Disorders, 38, 191–199.
Keel, P. K., Gravener, J. A., Joiner, T. E., Jr., & Haedt, A. A. (2010). Twenty-year follow-up of bulimia nervosa and related eating disorders not otherwise specified. International Journal of Eating Disorders, 43, 492–497.
Kenwood, M. G., & Carpenter, J. (2007). Multiple imputation: current perspectives. Statistical Methods in Medical Research, 16, 199–218.
Keski-Rahkonen, A., Hoek, H. W., Susser, E. S., Linna, M. S., Sihvola, E., Raevuori, A., et al. (2007). Epidemiology and course of anorexia nervosa in the community. The American Journal of Psychiatry, 164, 1259–1265.
Keski-Rahkonen, A., Hoek, H., Linna, M., Raevuori, A., Sihvola, E., Bulik, C., et al. (2009). Incidence and outcomes of bulimia nervosa: a nationwide population-based study. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences, 39, 823–831.
Kjelsas, E., Bjornstrom, C., & Gotestam, K. (2004). Prevalence of eating disorders in female and male adolescents (14–15 years). Eating Behaviors, 5, 13–25.
Lewinsohn, P. M., Striegel-Moore, R., & Seeley, M. S. (2000). Epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 1184–1292.
Li, J., Kendall, G. E., Henderson, S., Downie, J., Landsborough, L., & Oddy, W. H. (2008). Maternal psychosocial wellbeing in pregnancy and breastfeeding duration. Acta Paediatrica, 97, 221–225.
Lock, J., Couturier, J., & Agras, W. S. (2006). Comparison of long-term outcomes in adolescents with anorexia nervosa treated with family therapy. American Academy of Child and Adolescent Psychiatry, 45, 666–672.
Lovibond, S. H., & Lovibond, P. F. (1995). Manual for the depression anxiety stress scales (2nd ed.). Sydney: Psychology Foundation.
Mond, J. M., Hay, P., Rodgers, B., & Owen, C. (2007). Recurrent binge eating with and without the “undue influence of weight or shape on self-evaluation”: implications for the diagnosis of binge eating disorder. Behaviour Research and Therapy, 45, 929–938.
Newnham, J. P., Evans, S. F., Michael, C. A., Stanley, F. J., & Landau, L. I. (1993). Effects of frequent ultrasound during pregnancy: a randomised controlled trial. Lancet, 342, 887–891.
Ng, F., Trauer, T., Dodd, S., Callaly, T., Campbell, S., & Berk, M. (2007). The validity of the 21-item version of the depression anxiety stress scales as a routine clinical outcome measure. Acta Neuropsychiatrica, 19, 304–310.
Patton, G. C., Coffey, C., & Sawyer, S. (2003). The outcome of adolescent eating disorders: findings from the Victorian adolescent health cohort study. European Child & Adolescent Psychiatry, 12(Suppl1), i25–i29.
Rastam, M., Gillberg, C., & Wentz, E. (2003). Outcome of teenage-onset anorexia nervosa in a Swedish community-based sample. European Child & Adolescent Psychiatry, 12(Suppl 1), 78–90.
Ripley, B. D. (1996). Pattern recognition and neural networks. Cambridge: Cambridge University Press.
Salyers, M. P., Bosworth, H. B., Swanson, J. W., Lamb-Pagone, J., & Osher, F. C. (2000). Reliability and validity of the SF-12 health survey among people with severe mental illness. Medical Care, 38, 1141–1150.
Schafer, J. L., & Graham, J. W. (2002). Missing data: our view of the state of the art. Psychological Methods, 7, 141–177.
Shevlin, M. E., Bunting, B. P., & Lewis, C. A. (1995). Confirmatory factor analysis of the Rosenberg self-esteem scale. Psychological Reports, 76, 707–710.
Steinhausen, H. C. (2002). The outcome of anorexia nervosa in the 20th century. The American Journal of Psychiatry, 159, 1284–1293.
Steinhausen, H. C., & Weber, S. (2009). The outcome of bulimia nervosa: findings from one-quarter century of research. The American Journal of Psychiatry, 166, 1331–1341.
Stice, E. (2002). Risk and maintenance factors for eating pathology: a meta-analytic review. Psychological Bulletin, 128, 825–848.
Stice, E., Marti, C., Shaw, H., & Jaconis, M. (2009). An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. Journal of Abnormal Psychology, 118, 587–597.
Trent, L. M. Y., Russell, G., & Cooney, G. (1994). Assessment of self-concept in early adolescence. Australian Journal of Psychology, 46, 21–28.
Wade, T. D., Bergin, J. L., Tiggemann, M., Bulik, C. M., & Fairburn, C. G. (2006). Prevalence and long-term course of lifetime eating disorders in an adult Australian twin cohort. The Australian and New Zealand Journal of Psychiatry, 40, 121–128.
Wade, T. D., Wilksch, S., & Lee, C. (2012). A longitudinal investigation of the impact of disordered eating on young women’s quality of life. Health Psychology, 31, 352–359.
Ware, J. E., Kosinski, M., & Keller, S. D. (1996). A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220–233.
Wolke, D., Waylen, A., Samara, M., Steer, C., Goodman, R., & Ford, T. (2009). Selective drop-out in longitudinal studies and non-biased prediction of behaviour disorders. The British Journal of Psychiatry, 195, 249–256.
Wonderlich, S. A., Connolly, K. M., & Stice, E. (2004). Impulsivity as a risk factor for eating disorder behavior: assessment implications with adolescents. International Journal of Eating Disorders, 36, 172–182.
Acknowledgments
We are extremely grateful to the Raine Study participants and their families who took part in this study and to the Raine Study team for cohort management and data collection.
Financial Support
The first author is supported by an early career research fellowship from the National Health and Medical Research Council (NHMRC) of Australia. Core funding for the Western Australian Pregnancy Cohort (Raine) Study is provided by the Raine Medical Research Foundation; The University of Western Australia (UWA); the Faculty of Medicine, Dentistry and Health Sciences at UWA; the Telethon Institute for Child Health Research; the Women’s and Infant’s Research Foundation; and Curtin University. Funding for the 14-year Raine Study follow-up was provided by the Raine Medical Research Foundation and NHMRC project grants. Funding for the 17-year follow-up was provided by NHMRC programme grant 35314. Funding for the 20-year follow-up was provided by the Canadian Institutes of Health Research and NHMRC project grants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Allen, K.L., Byrne, S.M., Oddy, W.H. et al. Early Onset Binge Eating and Purging Eating Disorders: Course and Outcome in a Population-Based Study of Adolescents. J Abnorm Child Psychol 41, 1083–1096 (2013). https://doi.org/10.1007/s10802-013-9747-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-013-9747-7