Abstract
Differentiating between early-onset bipolar disorder (BD) and attention-deficit/hyperactivity disorder (ADHD) can be difficult. Memory problems are commonly reported in BD, and forgetfulness is among the diagnostic criteria for ADHD. We compared children and adolescents with BD (n = 23), ADHD combined type (ADHD-C; n = 26), BD + ADHD-C (n = 15), and 68 healthy controls on memory tests (Digit span, Children’s Verbal Learning Test-II). Further analyses were performed on subgroups of BD (BD-I, BD-II/BD-NOS, with and without previous psychotic symptoms). All clinical groups demonstrated some problems with free recall, but the BD subgroup with a history of psychotic symptoms had a more pervasive problem that also included recognition and semantic clustering. The ADHD-C groups demonstrated the lowest performance on working memory. These data suggest that children and adolescents with BD and previously psychotic symptoms may have inefficient encoding of verbal material, whereas memory problems in ADHD-C appear more characterized by impaired free recall.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The differential diagnosis between attention-deficit/hyperactivity disorder (ADHD) and early-onset bipolar disorder (BD) presents challenges for several reasons. ADHD and the manic episodes of BD overlap regarding symptoms of distractibility, restlessness, talkativeness, and loss of social inhibition (Youngstrom et al. 2010). Cognitive deficits are also reported in both ADHD and BD (Chamberlain et al. 2011; Joseph et al. 2008). ADHD-symptom checklists do not differentiate ADHD from BD because they do not assess the course of the symptoms, which is necessary to discern the episodic presentation of BD from the chronicity of symptoms in ADHD (Robertson et al. 2003). Even so, the specific episodic course of BD may be obscured by inter-episodic instability. There appears to be “a global delay or arrest in the development of appropriate affect regulation” (Carlson and Meyer 2006) in early-onset BD, and the course is often more chronic than that in later onset BD (Birmaher et al. 2006). Lastly, affective symptoms are features of both BD and ADHD (Anastopoulos et al. 2010; Skirrow et al. 2009), and unspecific manic symptoms are not uncommon in children with ADHD (Carlson 1998; Carlson and Meyer 2006; Hazell et al. 2003).
These factors may contribute to misdiagnosis of ADHD as BD and vice versa, as well as to artificially high comorbidity between ADHD and BD (Youngstrom et al. 2010). This is especially the case with the not otherwise specified subtype of BD (BD-NOS), and even more so in the diagnostic construct ‘Juvenile BD’, which include chronic irritability rather than distinct episodes (Biederman et al. 1998). However, evidence from family and outcome studies suggests that the diagnostic categories of BD and ADHD according to the Diagnostic and Statistical Manual (DSM-IV)(American Psychiatric Association 2000) are unrelated (Kent and Craddock 2003). Misdiagnosis is a serious problem because it may lead to unnecessary treatment, with potentially harmful side-effects (Correll et al. 2011). Also, delay of appropriate treatment may be associated with considerable functional impairment and morbidity in both BD and ADHD (Leboyer and Kupfer 2010; Leverich et al. 2007; Rasmussen and Gillberg 2000).
Despite the many overlapping symptoms, few studies have attempted to delimitate BD and ADHD through direct comparison (Mattis et al. 2011; Udal et al. 2009). Most of the existing research has evaluated neuropsychological differences between clinical participants with BD/ADHD comorbidity and clinical participants with a single diagnosis of BD or ADHD. These studies indicate differences in cognitive functioning between the two disorders (Walshaw et al. 2010). A systematic review of neurocognitive impairment in paediatric BD identified the largest effect size for verbal declarative memory (i.e., memory of factual information) (Joseph et al. 2008). In that study, inspection of the studies examining verbal memory indicated that the percentage of participants with ADHD did not moderate this effect. A study that compared neuropsychological functioning in adults with either BD or ADHD found that the ADHD group had significantly better performance than the BD group on memory tests (Torralva et al. 2010). This may imply that verbal memory deficits are more specific to BD, despite forgetfulness being among the diagnostic criteria for ADHD (American Psychiatric Association 2000).
Declarative memory problems in ADHD have often been considered as secondary to executive deficit (Antshel et al. 2010; Seidman et al. 2001). Most studies of declarative memory in ADHD demonstrate impaired free recall and intact recognition, contrary to what would have been expected with a genuine amnestic disturbance (Aycicegi-Dinn et al. 2011; Crocker et al. 2011; Kaplan et al. 1998; Kibby and Cohen 2008; Oie et al. 1999). Working memory (i.e., holding information in the mind while performing a mental operation) is an executive function needed in unstructured tasks such as free recall. Working memory deficits have been reported in children and adolescents with ADHD and in children and adolescents with BD, though most consistently in ADHD (for a review, see Walshaw et al. (2010).
Regarding BD, declarative memory deficits have been reported in both children and adolescents (Joseph et al. 2008; Nieto and Castellanos 2011), and in adults (Kurtz and Gerraty 2009), also in euthymic state (Arts et al. 2008) and in healthy relatives of individuals with BD (Bora et al. 2009; Doyle et al. 2009). Declarative memory deficits in children and adolescents with BD include both recall and recognition of presented word lists (Glahn et al. 2005), indicating a genuine verbal long-term memory deficit. Such deficits are associated with academic difficulties in children and adolescents with BD (Pavuluri et al. 2009) and with functional impairment in adults with BD (Sanchez-Morla et al. 2009). These problems may be reduced by early intervention (Pavuluri et al. 2010).
Young people may be more suited for neuropsychological studies than adults because they are less influenced by illness-related factors such as prolonged use of medication and drug abuse. Also, a stronger influence of genes is hypothesized in early-onset BD (Cahill et al. 2009; Faraone et al. 2004; Mick and Faraone 2009). Though some studies report that much of the cognitive deficit in children and adolescents with BD can be explained by comorbid ADHD (Henin et al. 2007; McClure et al. 2005; Rucklidge 2006), other studies of children and adolescents with BD report memory deficits also in those without comorbid ADHD (Doyle et al. 2005; Pavuluri et al. 2006). These contradictory results may be due to methodological differences regarding how differences in IQ are accounted for (McClure et al. 2005; Meyer et al. 2004), failure to correct for multiple comparisons (Doyle et al. 2005), inclusion of subjects in heterogeneous clinical states and with multiple medications (Dickstein et al. 2004; Doyle et al. 2005; Henin et al. 2007; Mattis et al. 2011; Olvera et al. 2005; Pavuluri et al. 2006), or the inclusion of different subtypes of ADHD and BD (Mattis et al. 2011; Rucklidge 2006).
One should be reluctant to interpret inattention as an indication of the inattentive subtype of ADHD in individuals with BD, because inattention is a non-specific symptom typical of several psychiatric disorders (Halperin et al. 1992). Cognitive deficits in adults with BD are found to be associated with a history of psychotic symptoms (Martinez-Aran et al. 2008; Savitz et al. 2009; Simonsen et al. 2011). In children with BD, Glahn et al. (2005) revealed a verbal declarative memory deficit only in those with BD-I disorder, while children with BD-II and BD-NOS did not differ from controls (the diagnostic subgroups of BD are defined later in the methods section). This might be because BD-I includes more of the psychotic subtype of BD. Approximately half of all BD clinical participants had displayed psychotic features on at least one occasion (Benazzi 1999), even more so in early-onset BD (Kowatch et al. 2005; Pavuluri et al. 2004; Tillman et al. 2008). To the best of our knowledge, no former study has compared learning and memory among the four groups of BD, ADHD combined subtype (ADHD-C), concurrent BD and ADHD-C, and controls, and no study has explored the effect of lifetime psychosis on memory function in children and adolescents with BD. The purpose of the present study is therefore to explore memory test performance in children and adolescents with ADHD, BD + ADHD-C, BD, and controls, with further analyses on subgroups of BD. We hypothesized that:
-
1)
The BD group will demonstrate a genuine amnestic deficit affecting all aspects of verbal declarative memory, most pronounced in those with a history of psychotic symptoms.
-
2)
The ADHD-C group will show retrieval problems characterized by impaired working memory and free recall, but normal performance on the more structured recognition task.
-
3)
Those with concurrent ADHD-C and BD will be impaired on both working memory and declarative memory.
-
4)
The different memory profiles may contribute to differentiating between BD and ADHD.
Methods
Clinical Sample
Inclusion Criteria
-
1)
BD defined as BD-I (DSM-IV 296.0-7), BD-II (DSM-IV 296.89), or BD-NOS (DSM-IV 296.80) (American Psychiatric Association 2000). Because the DSM-IV criteria for BP-NOS are vague, these were defined according to the Course of Bipolar Youth Study criteria (Birmaher et al. 2006): “…a minimum of elated mood plus 2 associated DSM-IV symptoms or irritable mood plus 3 DSM-IV associated symptoms, along with a change in the level of functioning, duration of a minimum of 4 hours within a 24-hour period, and at least 4 cumulative lifetime days meeting the criteria”. Cyclothymic disorder (DSM-IV 303.13) was also included in the BD-NOS group.
-
2)
ADHD defined as ADHD combined type (ADHD-C; DSM-IV 314) (American Psychiatric Association 2000). We included ADHD-C only, because data supporting the validity of other subtypes of ADHD are scarce (WHO 1993; Woo and Rey 2005).
-
3)
Concurrent ADHD-C and BD.
Exclusion criteria were age below 6.0 years or above 18.5 years, mental retardation according to DSM-IV or brain injury.
Recruitment Procedure
Clinical participants were recruited from a general child and adolescent unit in Norway from December 2004 to January 2009; 1983 individuals were referred during this period. Whenever BD was suspected (n = 232) by any of the staff, the patients were evaluated for further assessment; of these, 47 were included. In addition, 17 patients were referred from other units; of these, 6 were included. In addition, 18 patients with suspected ADHD-C only were selected from other referred patients to optimize the age and gender match; of these, 11 were included. The remaining assessed patients did not meet the inclusion criteria (n = 189), met the exclusion criteria (n = 4), did not wish to participate (n = 6), or did not complete the memory tests (n = 4). Finally, 64 clinical participants were included in the study: 23 with BD 26 with ADHD-C, and 15 with BD + ADHD-C (Table 1).
Diagnostic Assessment
Psychiatric diagnoses were assessed by a psychiatrist (first author) using the Kiddie-Schedule for Affective Disorders and Schizophrenia Present and Lifetime version (KSADS-PL) (Kaufman et al. 1997). Children and their parents or guardians were interviewed separately. KSADS-PL is a semi-structured interview designed to facilitate DSM-IV diagnostics, including a broad anamnestic interview and a comprehensive diagnostic interview. It has a strong content validity because it includes detailed probes useful in eliciting meaningful information regarding present and lifetime symptoms. Excellent-to-good validity and reliability are reported (Kaufman et al. 1997; Kim et al. 2004). The taped interviews, supplied with condensed medical journals, were validated by a child and adolescent psychiatrist. Inter-rater agreement (kappa) was 1.0 on bipolar disorder and 0.87 on ADHD-C. Information was also obtained from the school via a teacher’s evaluation and in most cases school observation by a clinician. The final inclusion diagnoses were based on all available information from discussions with the main researcher and an experienced child psychiatrist (last author). Information regarding comorbidity was also recorded from KSADS-PL.
A History of Psychotic Symptoms
As in a number of other studies (Rende et al. 2006; Savitz et al. 2009), a history of psychotic symptoms was evaluated during the diagnostic interview. A history of psychotic symptoms was defined as the presence of at least one psychotic symptom (hallucination or delusion) during a manic or a depressive episode. Also, very brief psychotic phenomena were counted as ‘a history of psychotic symptoms’. A history of state-dependent psychotic symptoms was reported in 10 BD clinical participants and 4 BD + ADHD-C clinical participants (6 during depression and 8 during mania or mixed episode). No psychotic symptoms were observed during assessments. Because the BD + ADHD-C group was so small, pair-wise comparisons were performed only in the BD subgroups with and without a history of psychotic symptoms, hereafter named the ‘BD-psychotic subgroup’ and the ‘BD-nonpsychotic subgroup’, respectively. The BD-psychotic subgroup was significantly older and reported more comorbid drug abuse than did the BD-nonpsychotic subgroup.
Medication
When possible, medication was delayed until after the diagnostic and neuropsychological assessment. Only 5 BD-I clinical participants were diagnosed with BD and treated with mood-stabilizer before they were referred to the study (lamotrigine: n = 2, lithium: n = 1, valproate: n = 2, and aripiprazole: n = 1). Medication was not discontinued in these clinical participants.
Other medication (methylphenidate: n = 5) was discontinued for a minimum of five times the elimination half-life before testing.
State
When possible, the clinical participants were assessed in euthymic phase. The neuropsychologist reported mood symptoms according to the following “scale”. 1. No mood symptoms (n = 54). 2. Some mood symptoms (n = 8). 3. Mood symptoms that may affect the validity of the results (n = 2; both BD + ADHD-C) (Table 1).
Controls
Sixty-eight controls were recruited from three secondary schools and one junior high school. The inclusion criterion was attendance of regular school classes at normal grade levels without known learning disorder or psychiatric disorders. The parents confirmed that their child was not using medication, receiving treatment from child and adolescent psychiatric services, diagnosed with a declarative memory disability, or currently receiving any form of special tutoring/education. They were not evaluated by a specific diagnostic interview, but the teacher and parents completed the Achenbach System of Empirically Based Assessment questionnaires (see below), which also measure DSM-IV-oriented symptoms (Spatola et al. 2007). T-scores above 60 indicate a problem. Affective problems were reported from 7 parents and 3 teachers. Anxiety problems were reported by 4 parents and 4 teachers. ADHD problems were reported by 3 parents and 4 teachers. Controls were in common with another study (Egeland et al. 2009).
Checklist-Rated Behaviour
Symptom checklists rated by parents and school were used for a clinical comparison of the sample. Symptom checklists were not used as diagnostic tools; therefore, no cut-off scores are provided (Table 1).
Parent- and teacher-rated behavioural and emotional functioning were recorded from the Achenbach System of Empirically Based Assessment questionnaires (Achenbach 2010), which include 120 behavioural items rated on a three-step scale from 0 to 2. These are grouped in problem areas and converted to T-scores relative to population norms. T-scores above 60 indicate a problem. Multivariate analyses identified two main groups of problems, designated Internalizing (anxious, inhibited behaviour) and Externalizing (aggressive, antisocial behaviour). The questionnaires are validated in a Norwegian sample (Novik 2000).
ADHD rating scale–IV are parent- and teacher-rated checklists of 9 inattentive and 9 hyperactivity/impulsivity symptoms graded from 0 to 3 and linked to the DSM-IV criteria for ADHD-C. The ratings are converted to an inattention percentile and a hyperactivity/impulsivity percentile relative to population norms. Adequate psychometric properties for the screening and assessment of ADHD are reported (Barkley 1990; DuPaul 1998; Szomlaiski et al. 2009), but no study has explored its diagnostic validity for ADHD versus BD. There are no Norwegian norms.
Neuropsychological Tests
IQ: All clinical participants completed the Wechsler Intelligence Scales (1991, 1997). In the control sample, intellectual capacity was estimated from scaled scores of the subtests Similarities and Picture Completion from the Wechsler Intelligence Scales.
Working memory was determined by the Digit Span subtest from WISC-III/WAIS-III (Wechsler 1991, 1997), in which the participant repeats forward and backward random pairs of numbers read aloud. Digit Span is one of the most commonly administered and widely accepted indexes of working memory.
Verbal declarative memory was assessed by the children’s version of the Rey Auditory Verbal Learning Test: the Children’s Auditory-Verbal Learning Test-2, in accordance with the professional manual (Talley 1993). Normative data from 595 public U.S. school pupils are available, and the test is validated in several studies (Talley 1993). There are no Norwegian norms.
The task was to recall an orally presented list of 16 ordinary Norwegian words over five learning trials, followed by presentation and recall of a second interference list. Short- and long-delayed recall of the initial list was then assessed, followed by delayed recognition tests in which words from both lists were mixed with new words. Impaired recognition indicates a genuine amnestic deficit, whereas all the other trials are based on free recall of learned material. In the present study, short- and long-delay recall was adjusted for words recalled in learning trial 5. Because words are grouped into four semantic categories, one can assess the extent to which participants use semantic strategies to recall information.
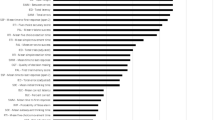
The tests were administered in fixed order by an experienced neuropsychologist. All analyses were performed on raw data because the age variance was larger in the clinical groups than among controls. In addition, the normative data of the Children’s Auditory-Verbal Learning Test-2 are not validated in a Norwegian sample (Fig. 1).
Ethics
The study was carried out in accordance with the Helsinki Declaration and was approved by the Regional Committee for Medical Research Ethics of Southern Norway and the Norwegian Social Science Data Service. Children and their caregivers were given verbal and written information. Caregivers and children aged ≥12 years provided written consent, and younger children provided spoken assent.
Statistical Analysis
Statistical analyses were performed using SPSS software for Windows version 16 (SPSS, Chicago, IL). Significance was set at p < 0.05 (two-sided).
Sample characteristics were analysed using analysis of variance (ANOVA) for continuous variables, and categorical data were analysed by chi-square or Fisher’s exact test as appropriate.
Neurocognitive comparisons were explored using generalized linear models (Nelder and Wedderburn 1972). A generalized linear model is an extension of the linear modelling process that allows models to be fitted to data that follow probability distributions other than a normal distribution, such as a Poisson distribution. Generalized linear models also have a lesser requirement for equality or constancy of variances compared with the hypothesis tests in traditional linear models. We analysed raw scores with covariate age, gender, and estimated IQ. Because we considered simple Bonferroni correction to be too conservative for the multiple groups of the present study, pair-wise post-hoc analyses were performed with sequential Bonferroni adjustments (Holm 1979). The sequential method works as follows: When comparing six pairs with 0.05 as the threshold p value (alpha level), then the most significant of the three p values must be less than 0.05/6 = .008 to be significant; the second most significant p value of the three must be less than .05/5 = 0.010; the third most significant must be less than 0.05/4 = 0.013; the fourth most significant must be less than 0.05/3 = 0.017; the fifth most significant must be less than 0.05/2 = 0.025; and the least significant must be less than 0.05 to be significant. Based on estimated marginal means and corresponding standard errors from the generalized linear models, effect size was expressed as Cohen’s d = ∆ estimated marginal mean/pooled standard deviation (note that effect sizes calculated from generalized linear models with a Poisson distribution must be interpreted with caution). Main group comparisons (BD vs. ADHD-C vs. BD + ADHD-C vs. C) were followed up by analyses of the BD subgroups: BD-psychotic vs. BD-nonpsychotic vs. ADHD-C vs. C, and BD-I vs. BD-II/BD-NOS vs. ADHD-C vs. C.
Because most of the clinical group differences (state, medication, and comorbidity; Table 1) were considered illness-specific, they were not entered as covariates in the neurocognitive comparisons. Instead, follow-up correlation analyses (Spearman’s rho) were used to explore whether neurocognition was associated with mood symptoms, medication, or comorbidity across the clinical groups.
Results
Main Clinical Groups
The mean estimated performance on neuropsychological tests, and differences between the main clinical groups and controls, are presented in Table 2. The ADHD-C group performed significantly below the control group on working memory and free recall (trial 1–5), with normal performance on recognition.
The BD group performed significantly below the control group on six of nine declarative memory measures, but not significantly below controls on working memory. Despite significant differences between the clinical groups and the control group on semantic clustering, the effect sizes of these differences were small. (However, because of the non-parametric distribution of the test results and the corresponding high values of standard errors, the effect size values cannot be relied upon when comparing performance on this test). The BD + ADHD-C group performed significantly below the control group on working memory, free recall (trial 1–5) and recognition. Neither of the clinical groups performed significantly below controls on the short-time and delayed recall trials. The only significant difference between the main clinical groups was the impaired performance of the BD + ADHD-C group compared with the ADHD-C group on recognition.
BD With and Without a History of Psychotic Symptoms
As shown in Table 3, the BD group was split into a BD-psychotic subgroup with a history of psychotic symptoms, and a BD-nonpsychotic subgroup without indications of previous psychotic symptoms. The BD-psychotic subgroup performed significantly below controls on eight of the nine declarative memory measures, including delayed recall and recognition. The BD-psychotic group was also significantly impaired compared with the ADHD-C and BD-nonpsychotic groups on delayed recall and recognition. The BD-nonpsychotic group performed significantly below the control group only on the second learning trial. Neither of the BD groups performed significantly below the control group on working memory.
Diagnostic Subgroups of BD
Verbal learning differences were less pronounced between the diagnostic subtypes of BD than between the BD-psychotic and BD-nonpsychotic subgroups. The BD-II/BD-NOS group performed significantly below controls on more verbal learning trials than did the BD-I group, but only the BD-I group was significantly impaired compared with controls on the semantic clustering, delayed recall and recognition trials (Table 4). None of the BD diagnostic subgroups were significantly impaired compared with controls on working memory.
Impact of Mood Symptoms, Medication, and Comorbidity
There were no significantly negative correlations between the main findings (defined as score on Digit span, verbal learning trial 5, and verbal recognition) and mood symptoms, medication, comorbid anxiety disorder, tic disorder, drug abuse, post traumatic stress disorder, or reading problems.
Discussion
The present study compared verbal memory in children and adolescents with BD, ADHD-C, BD + ADHD-C, and controls. In a second step, we compared BD with and without a history of psychotic symptoms, ADHD-C, and controls. In a third step we compared BD-I, BD-II/BD-NOS, ADHD-C, and controls.
All clinical groups performed below controls on verbal learning trials (free recall). The BD-psychotic and BD-I subgroups performed significantly below controls also on delayed recall and recognition, indicating a genuine amnestic deficit. These impairments were driven by the BD-psychotic group, which also performed significantly below the ADHD-C group on delayed recall and recognition. Only the ADHD-C groups performed significantly below controls on working memory. The ADHD-C only group demonstrated performance equal to healthy controls on the recognition trial. Thus, the three first hypotheses were partially verified: 1. Genuine amnestic deficit in BD, most pronounced in those with a history of psychotic symptoms; 2. Free recall and working memory problems in ADHD-C; and 3. Free recall, working memory, and amnestic problems in the BD + ADHD-C group. The fourth hypothesis regarding differential diagnostic usefulness of memory profiles was not verified: With the exception of one area (recognition and to some extent delayed recall) there were no group differences among the clinical groups on any of the areas tested. However, declarative memory deficit cannot be used as a diagnostic marker for BD because only a subgroup of the BD sample was significantly impaired compared with the controls and ADHD-C on delayed recall and recognition. Working memory deficit had no diagnostic value: only the ADHD-C groups performed significantly below controls on this test, but looking at effect sizes, the difference between the clinical groups was marginal.
Findings in BD
The recall and recognition problems in the BD-psychotic subgroup indicate a genuine encoding deficit that may be associated with the extremely low level of semantic clustering in this subgroup. Semantic organization refers to real-world knowledge and is one of the key factors in perception, executive functions, and memory (Chang et al. 2011; Gazzaniga et al. 2009). Inconsistent reports of semantic clustering deficit in BD (Bearden et al. 2006; Chang et al. 2011; Glahn et al. 2005) may reflect different samples studied, because semantic deficits in BD appear to be associated with a history of psychotic mood episode(s) (Kravariti et al. 2009).
Recognition deficit is reported previously in children and adolescents with BD-I, but not in children and adolescents with broader BD phenotypes (Glahn et al. 2005; McClellan et al. 2004). Because our BD-psychotic subgroup comprised mostly BD-I participants and the BD-nonpsychotic subgroup comprised all the BD-NOS participants, there was a partial overlap between a history of psychotic symptoms and the diagnostic subtypes of BD. Difference was more pronounced between the BD-psychotic and BD-nonpsychotic subgroups than between the BD-I and BD-II/BD-NOS subgroups (Tables 3 and 4), indicating that a history of psychosis better explains the neurocognitive variance in the BD group than the BD diagnostic subtypes do, in line with the findings of several studies of adults with BD (Savitz;(Levy and Weiss 2010; Martinez-Aran et al. 2008; Savitz et al. 2009) (Simonsen et al. 2011). Thus, a history of psychotic symptoms may be a marker of a more serious developmental subtype of BD with more cognitive deficits, or may be a sequel of psychotic episodes in BD.
The high prevalence of psychotic mood episodes in our BD sample is consistent with the findings of other studies (Reddy et al. 1997; Rende et al. 2006; Tillman et al. 2008), and supports the suggestion that early-onset BD commonly represents a severe subtype of the disorder (Geller et al. 2008; Pavuluri et al. 2004). However, because it is difficult to evaluate retrospective information of psychotic symptoms in children, false perceptions and drug-related psychotic symptoms may have been misinterpreted as psychotic episodes of BD (Hlastala and McClellan 2005; Reimherr and McClellan 2004). Despite no reports of psychotic symptoms outside a mood episode, our BD-psychotic group may have included some participants misdiagnosed with schizoaffective disorder, which may have contributed to the marked verbal memory deficit (McClellan et al. 2002; McClellan et al. 2004). Nevertheless, a recent meta-analysis found that individuals with paediatric BD suffer from cognitive deficits (including verbal memory) that are milder but similar in nature to those of patients with early-onset schizophrenia (Nieto and Castellanos 2011).
The scarce impairments in the BD-nonpsychotic group are supported by the recent adult BD literature (Savitz et al. 2009; Simonsen et al. 2011). In the present study, the BD-nonpsychotic group included all participants with a diagnosis of BD-NOS, which is a “maybe bipolar” category: some of these may have had mood instability of other aetiology, while others may have had a BD prodrome (Glahn et al. 2005; Sala et al. 2009).
In the present sample, mood symptoms, medication, and comorbidity had no significant impact on performance. Because of the small sample and large intra-group variation, we cannot rule out the effect of these factors on test performance.
Findings in ADHD-C
In line with the findings of most other studies, the ADHD-C group demonstrated impaired working memory and free recall problems compared with the controls, but no recognition deficit (Crocker et al. 2011; Kaplan et al. 1998; Martinussen et al. 2005; Seidman et al. 1998; Walshaw et al. 2010). The ADHD-C group’s efficient recognition indicates that verbal recall problems in ADHD may be due to executive problems rather than a genuine amnestic deficit. Free recall problems may explain why impaired listening comprehension is correlated with working memory deficit and inattention symptoms in ADHD (McInnes et al. 2003).
However, our findings are group results, and the majority of ADHD participants in the present study did not demonstrate significantly worse working memory than controls, in line with the findings of most studies of ADHD-C (Willcutt et al. 2005). Thus, working memory deficits cannot be used as a neurocognitive marker of ADHD-C.
Findings in Concurrent ADHD-C and BD
The BD + ADHD-C group demonstrated declarative memory problems similar to the BD group and working memory problems similar to (but not worse than) the ADHD-C group. This indicates that the BD + ADHD-C group may include some participants with ‘true’ comorbidity. The comorbid group demonstrated pronounced recognition problems, where the contribution from four participants with a history of psychotic symptoms was considerable. These four may belong to a more serious neurodevelopmental subtype of BD that is associated with comorbid ADHD, cognitive deficits, and psychotic symptoms (Duffy 2010). However, the heterogeneous performance and over-representation of BD-NOS in our comorbid group indicate that this group may include several disorders, some of which probably belong to an ADHD-C subtype with substantial mood instability (Sobanski et al. 2010) rather than to a comorbid BD subtype.
Clinical Implications and Further Research
The present data suggest that children and adolescents with BD and a history of psychotic symptoms show inefficient encoding of verbal material (i.e., a genuine amnestic deficit), whereas performance of the ADHD group may be better characterized by inefficient free recall of learned material. To the best of our knowledge, this study is the first to reveal that verbal amnestic problems in children and adolescents with BD characterize those with a history of psychotic symptoms, and not those without previous psychotic symptoms; this is consistent with the findings in adults with BD.
Longitudinal offspring studies are needed to clarify whether verbal long-term memory deficit is a marker of a psychotic subtype of BD or is a consequence of psychotic episodes in BD. Reports of normal cognitive development pre-morbid in BD support the latter suggestion (Lewandowski et al. 2011; Quackenbush et al. 1996), whereas findings of cognitive deficits in two offspring studies indicate the presence of a more serious neurodevelopmental subtype of BD (Maziade et al. 2009; Meyer et al. 2004). If verbal memory deficit is a marker for a more serious developmental subtype of BD, this has importance for diagnostic evaluation, prognosis, and intervention. If verbal memory deficit is a consequence of psychotic episodes, it emphasizes the importance of identification and treatment of early-onset BD, in light of the poor prognosis of those with verbal declarative memory deficit (Bonnin et al. 2010; Torres et al. 2010).
The low level of semantic clustering in the BD-psychotic group indicates that verbal memory deficits in BD may be secondary to semantic organization deficits (Sumiyoshi et al. 2001; Sumiyoshi et al. 2005). Several cognitive domains are largely dependent upon a well-organized network of semantic associations (Rogers et al. 2004), and subtle impairments in semantic organization can bring about considerable changes in cognition and experiences, and also influence delusion formation (Rossell 2006). Follow-up studies may be needed to clarify the interplay among semantic organization, long-term verbal memory, and behavioural characteristics including psychotic symptoms.
Though memory function is not very useful in distinguishing those with BD from individuals with ADHD-C, it may lend insight into the neurobiological systems that are disrupted in childhood psychiatric disorders. In terms of BD, this information can also potentially define endophenotypes for further parsing of BD. In addition, understanding cognitive abnormalities may promote tailored education strategies and perhaps reduce the academic and functional impairment associated with cognitive deficits in both BD and ADHD (Biederman et al. 2004; Martinez-Aran et al. 2007; Miller and Hinshaw 2010; Pavuluri et al. 2009; Thorell 2007).
Limitations and Strengths
The strengths of our study are that most of our clinical participants were drug-free and euthymic, and we did account for estimated IQ. Also, young people may be more suitable for neuropsychological studies than adults because they are less influenced by negative effects of long-term illness.
The small and convenient clinical sample of the present study limits the generalization of our findings. Because of the developmentally insensitive BD criteria and the heterogeneity of the BD groups, the findings in these groups in particular should be interpreted with caution. Also, prior medication exposure may have influenced some of our findings.
The considerable intra-group variation in test performance in the BD groups may be a reflection of the heterogeneity of these groups, but the variance was also considerable in our well-characterized ADHD-C group. However, variable performance is expected in ADHD-C because a failure to engage top-down control, depending on the reward of the task, appears to underlie the shifting cognitive performance in most individuals with ADHD (Casey et al. 2007). Performance on neuropsychological tests is also influenced by various factors, including motivation, stress, and tiredness.
Our results may have been affected by statistical problems. Neuropsychological data on clinical groups are mostly categorical and non-parametrically distributed, and are influenced by several moderators and covariates; these factors, together with our small sample size, make statistical modelling imperfect. This problem is common to most neuropsychological studies.
Conclusions
A genuine amnestic deficit may characterize BD with a history of psychotic symptoms, in contrast to BD with no previously psychotic symptoms. ADHD-C may be better characterized by a deficit in free recall of learned memory. These findings are not useful as diagnostic markers, but may guide our understanding of daily life problems and facilitate tailored educational strategies in children and adolescents with ADHD and BD. Further studies are needed to clarify whether memory problems are primary or secondary to psychotic episodes in BD, and to investigate the interplay among semantic organization, long-term memory, and behavioural characteristics including psychotic symptoms.
References
Achenbach, T. (2010). ASEBA home. Achenbach System of Empirically Based Assessment.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington: American Psychiatric Association.
Anastopoulos, A. D., Smith, T. F., Garrett, M. E., Morrissey-Kane, E., Schatz, N. K., Sommer, J. L., et al. (2011). Self-regulation of emotion, functional impairment, and comorbidity among children with ADHD. Journal of Attention Disorders, 15(7), 583–592.
Antshel, K. M., Faraone, S. V., Maglione, K., Doyle, A. E., Fried, R., Seidman, L. J., & Biederman, J. (2010). Executive functioning in high-IQ adults with ADHD. Psychological Medicine, 40(11), 1909–1918.
Arts, B., Jabben, N., Krabbendam, L., & Van Os, J. (2008). Meta-analyses of cognitive functioning in euthymic bipolar patients and their first-degree relatives. Psychological Medicine, 38(6), 771–785.
Aycicegi-Dinn, A., Dervent-Ozbek, S., Yazgan, Y., Bicer, D. & Dinn, W. M. (2011). Neurocognitive correlates of adult attention-deficit/hyperactivity disorder in a Turkish sample. Attention Deficit Hyperactivity Disorder, 3(1), 41–52.
Barkley, R. A. (1990). Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment. New York: Guilford.
Bearden, C. E., Glahn, D. C., Monkul, E. S., Barrett, J., Najt, P., Kaur, S., et al. (2006). Sources of declarative memory impairment in bipolar disorder: mnemonic processes and clinical features. Journal of Psychiatric Research, 40(1), 47–58.
Benazzi, F. (1999). Psychotic versus nonpsychotic bipolar outpatient depression. European Psychiatry, 14(8), 458–461.
Biederman, J., Klein, R. G., Pine, D. S., & Klein, D. F. (1998). Resolved: mania is mistaken for ADHD in prepubertal children. Journal of the American Academy of Child and Adolescent Psychiatry, 37(10), 1091–1096.
Biederman, J., Monuteaux, M. C., Doyle, A. E., Seidman, L. J., Wilens, T. E., Ferrero, F., et al. (2004). Impact of executive function deficits and attention-deficit/hyperactivity disorder (ADHD) on academic outcomes in children. Journal of consulting and clinical psychology, 72(5), 757–766.
Birmaher, B., Axelson, D., Strober, M., Gill, M. K., Valeri, S., Chiappetta, L., et al. (2006). Clinical course of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry, 63(2), 175–183.
Bonnin, C. M., Martinez-Aran, A., Torrent, C., Pacchiarotti, I., Rosa, A. R., Franco, C., et al. (2010). Clinical and neurocognitive predictors of functional outcome in bipolar euthymic patients: a long-term, follow-up study. Journal of Affective Disorders, 121(1–2), 156–160.
Bora, E., Yucel, M., & Pantelis, C. (2009). Cognitive endophenotypes of bipolar disorder: a meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. Journal of Affective Disorders, 113(1–2), 1–20.
Cahill, C. M., Walter, G., & Malhi, G. S. (2009). Neurocognition in bipolar disorder and juvenile bipolar disorder. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 18(3), 221–230.
Carlson, G. A. (1998). Mania and ADHD: comorbidity or confusion. Journal of Affective Disorders, 51(2), 177–187.
Carlson, G. A., & Meyer, S. E. (2006). Phenomenology and diagnosis of bipolar disorder in children, adolescents, and adults: complexities and developmental issues. Development and Psychopathology, 18(4), 939–969.
Casey, B. J., Nigg, J. T., & Durston, S. (2007). New potential leads in the biology and treatment of attention deficit-hyperactivity disorder. Current Opinion in Neurology, 20(2), 119–124.
Chamberlain, S. R., Robbins, T. W., Winder-Rhodes, S., Muller, U., Sahakian, B. J., Blackwell, A. D., et al. (2011). Translational approaches to frontostriatal dysfunction in attention-deficit/hyperactivity disorder using a computerized neuropsychological battery. Biological Psychiatry, 69(12), 1192–1203.
Chang, J. S., Choi, S., Ha, K., Ha, T. H., Cho, H. S., Choi, J. E., et al. (2011). Differential pattern of semantic memory organization between bipolar I and II disorders. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 35(4):1053–8.
Correll, C. U., Kratochvil, C. J., & March, J. S. (2011). Developments in pediatric psychopharmacology: focus on stimulants, antidepressants, and antipsychotics. Journal of Clinical Psychiatry, 72(5), 655–670.
Crocker, N., Vaurio, L., Riley, E. P., & Mattson, S. N. (2011). Comparison of verbal learning and memory in children with heavy prenatal alcohol exposure or attention-deficit/hyperactivity disorder. Alcoholism, Clinical and Experimental Research, 35(6):1114–21.
Dickstein, D. P., Treland, J. E., Snow, J., McClure, E. B., Mehta, M. S., Towbin, K. E., et al. (2004). Neuropsychological performance in pediatric bipolar disorder. Biological Psychiatry, 55(1), 32–39.
Doyle, A. E., Wilens, T. E., Kwon, A., Seidman, L. J., Faraone, S. V., & Fried, R. (2005). Neuropsychological functioning in youth with bipolar disorder. Biological Psychiatry, 58(7), 540–548.
Doyle, A. E., Wozniak, J., Wilens, T. E., Henin, A., Seidman, L. J., & Petty, C. (2009). Neurocognitive impairment in unaffected siblings of youth with bipolar disorder. Psychological Medicine, 39(8), 1253–1263.
Duffy, A. (2010). The early natural history of bipolar disorder: what we have learned from longitudinal high-risk research. Canadian Journal of Psychiatry, 55(8), 477–485.
DuPaul, G. J. (1998). ADHD rating scale-IV: Checklists, norms, and clinical interpretation. New York: Guilford Press.
Egeland, J., Johansen, S. N., & Ueland, T. (2009). Differentiating between ADHD sub-types on CCPT measures of sustained attention and vigilance. Scandinavian Journal of Psychology, 50(4), 347–354.
Faraone, S. V., Glatt, S. J., Su, J., & Tsuang, M. T. (2004). Three potential susceptibility loci shown by a genome-wide scan for regions influencing the age at onset of mania. American Journal of Psychiatry, 161(4), 625–630.
Gazzaniga, M. S. I., R. B.; Mangun, G. R. (Ed.). (2009). Cognitive neuroscience: the biology of the mind, 3rd Edition. New York, NY: W. W. Nortoan & Company.
Geller, B., Tillman, R., Bolhofner, K., & Zimerman, B. (2008). Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Archives of General Psychiatry, 65(10), 1125–1133.
Glahn, D. C., Bearden, C. E., Caetano, S., Fonseca, M., Najt, P., Hunter, K., et al. (2005). Declarative memory impairment in pediatric bipolar disorder. Bipolar Disorder, 7(6), 546–554.
Halperin, J. M., Matier, K., Bedi, G., Sharma, V., & Newcorn, J. H. (1992). Specificity of inattention, impulsivity, and hyperactivity to the diagnosis of attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 31(2), 190–196.
Hazell, P. L., Carr, V., Lewin, T. J., & Sly, K. (2003). Manic symptoms in young males with ADHD predict functioning but not diagnosis after 6 years. Journal of the American Academy of Child and Adolescent Psychiatry, 42(5), 552–560.
Henin, A., Mick, E., Biederman, J., Fried, R., Wozniak, J., Faraone, S. V., et al. (2007). Can bipolar disorder-specific neuropsychological impairments in children be identified? Journal of consulting and clinical psychology, 75(2), 210–220.
Hlastala, S. A., & McClellan, J. (2005). Phenomenology and diagnostic stability of youths with atypical psychotic symptoms. Journal of Child and Adolescent Psychopharmacology, 15(3), 497–509.
Holm, S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics, 6(2), 65–70.
Joseph, M. F., Frazier, T. W., Youngstrom, E. A., & Soares, J. C. (2008). A quantitative and qualitative review of neurocognitive performance in pediatric bipolar disorder. Journal of Child and Adolescent Psychopharmacology, 18(6), 595–605.
Kaplan, B. J., Dewey, D., Crawford, S. G., & Fisher, G. C. (1998). Deficits in long-term memory are not characteristic of ADHD. Attention Deficit Hyperactivity Disorder. Journal of Clinical and Experimental Neuropsychology, 20(4), 518–528.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988.
Kent, L., & Craddock, N. (2003). Is there a relationship between attention deficit hyperactivity disorder and bipolar disorder? Journal of Affective Disorders, 73(3), 211–221.
Kibby, M. Y., & Cohen, M. J. (2008). Memory functioning in children with reading disabilities and/or attention deficit/hyperactivity disorder: a clinical investigation of their working memory and long-term memory functioning. Child Neuropsychology, 14(6), 525–546.
Kim, Y. S., Cheon, K. A., Kim, B. N., Chang, S. A., Yoo, H. J., Kim, J. W., et al. (2004). The reliability and validity of Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version- Korean version (K-SADS-PL-K). Yonsei Medical Journal, 45(1), 81–89.
Kowatch, R. A., Youngstrom, E. A., Danielyan, A., & Findling, R. L. (2005). Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar Disorder, 7(6), 483–496.
Kravariti, E., Reichenberg, A., Morgan, K., Dazzan, P., Morgan, C., Zanelli, J. W., et al. (2009). Selective deficits in semantic verbal fluency in patients with a first affective episode with psychotic symptoms and a positive history of mania. Bipolar Disorder, 11(3), 323–329.
Kurtz, M. M., & Gerraty, R. T. (2009). A meta-analytic investigation of neurocognitive deficits in bipolar illness: profile and effects of clinical state. Neuropsychology, 23(5), 551–562.
Leboyer, M., & Kupfer, D. J. (2010). Bipolar disorder: new perspectives in health care and prevention. Journal of Clinical Psychiatry, 71(12), 1689–1695.
Leverich, G. S., Post, R. M., Keck, P. E., Jr., Altshuler, L. L., Frye, M. A., Kupka, R. W., et al. (2007). The poor prognosis of childhood-onset bipolar disorder. Journal of Pediatrics, 150(5), 485–490.
Levy, B., & Weiss, R. D. (2010). Neurocognitive impairment and psychosis in bipolar I disorder during early remission from an acute episode of mood disturbance. Journal of Clinical Psychiatry, 71(2), 201–206.
Lewandowski, K. E., Cohen, B. M., & Ongur, D. (2011). Evolution of neuropsychological dysfunction during the course of schizophrenia and bipolar disorder. Psychological Medicine, 41(2), 225–241.
Martinez-Aran, A., Torrent, C., Tabares-Seisdedos, R., Salamero, M., Daban, C., Balanza-Martinez, V., et al. (2008). Neurocognitive impairment in bipolar patients with and without history of psychosis. Journal of Clinical Psychiatry, 69(2), 233–239.
Martinez-Aran, A., Vieta, E., Torrent, C., Sanchez-Moreno, J., Goikolea, J. M., & Salamero, M. (2007). Functional outcome in bipolar disorder: the role of clinical and cognitive factors. Bipolar Disorder, 9(1–2), 103–113.
Martinussen, R., Hayden, J., Hogg-Johnson, S., & Tannock, R. (2005). A meta-analysis of working memory impairments in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 44(4), 377–384.
Mattis, S., Papolos, D., Luck, D., Cockerham, M., & Thode, H. C., Jr. (2011). Neuropsychological factors differentiating treated children with pediatric bipolar disorder from those with attention-deficit/hyperactivity disorder. Journal of Clinical and Experimental Neuropsychology, 33(1), 74–84.
Maziade, M., Rouleau, N., Gingras, N., Boutin, P., Paradis, M. E., & Jomphe, V. (2009). Shared neurocognitive dysfunctions in young offspring at extreme risk for schizophrenia or bipolar disorder in eastern quebec multigenerational families. Schizophrenia Bulletin, 35(5), 919–930.
McClellan, J., McCurry, C., Speltz, M. L., & Jones, K. (2002). Symptom factors in early-onset psychotic disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 41(7), 791–798.
McClellan, J., Prezbindowski, A., Breiger, D., & McCurry, C. (2004). Neuropsychological functioning in early onset psychotic disorders. Schizophrenia Research, 68(1), 21–26.
McClure, E. B., Treland, J. E., Snow, J., Dickstein, D. P., Towbin, K. E., Charney, D. S., et al. (2005). Memory and learning in pediatric bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 44(5), 461–469.
McInnes, A., Humphries, T., Hogg-Johnson, S., & Tannock, R. (2003). Listening comprehension and working memory are impaired in attention-deficit hyperactivity disorder irrespective of language impairment. Journal of Abnormal Child Psychology, 31(4), 427–443.
Meyer, S. E., Carlson, G. A., Wiggs, E. A., Martinez, P. E., Ronsaville, D. S., & Klimes-Dougan, B. (2004). A prospective study of the association among impaired executive functioning, childhood attentional problems, and the development of bipolar disorder. Development and Psychopathology, 16(2), 461–476.
Mick, E., & Faraone, S. V. (2009). Family and genetic association studies of bipolar disorder in children. Child and Adolescent Psychiatric Clinics of North America, 18(2), 441–453.
Miller, M., & Hinshaw, S. P. (2010). Does childhood executive function predict adolescent functional outcomes in girls with ADHD? Journal of Abnormal Child Psychology, 38(3), 315–326.
Nelder, J. A., & Wedderburn, R. W. M. (1972). Generalized linear models. Journal of the Royal Statistical Society. Series A (General) (Blackwell Publishing), 3(135), 370–384.
Nieto, R. G., & Castellanos, F. X. (2011). A meta-analysis of neuropsychological functioning in patients with early onset schizophrenia and pediatric bipolar disorder. Journal of clinical child and adolescent psychology, 40(2), 266–280.
Novik, T. S. (2000). Child behavior checklist item scores in Norwegian children. European Child and Adolescent Psychiatry, 9(1), 54–60.
Oie, M., Sunde, K., & Rund, B. R. (1999). Contrasts in memory functions between adolescents with schizophrenia or ADHD. Neuropsychologia, 37(12), 1351–1358.
Olvera, R. L., Semrud-Clikeman, M., Pliszka, S. R., & O'Donnell, L. (2005). Neuropsychological deficits in adolescents with conduct disorder and comorbid bipolar disorder: a pilot study. Bipolar Disorder, 7(1), 57–67.
Pavuluri, M. N., Herbener, E. S., & Sweeney, J. A. (2004). Psychotic symptoms in pediatric bipolar disorder. Journal of Affective Disorders, 80(1), 19–28.
Pavuluri, M. N., O'Connor, M. M., Harral, E. M., Moss, M., & Sweeney, J. A. (2006). Impact of neurocognitive function on academic difficulties in pediatric bipolar disorder: a clinical translation. Biological Psychiatry, 60(9), 951–956.
Pavuluri, M. N., Passarotti, A. M., Mohammed, T., Carbray, J. A., & Sweeney, J. A. (2010). Enhanced working and verbal memory after lamotrigine treatment in pediatric bipolar disorder. Bipolar Disorder, 12(2), 213–220.
Pavuluri, M. N., Schenkel, L. S., Aryal, S., Harral, E. M., Hill, S. K., Herbener, E. S., & Sweeney, J. A. (2006). Neurocognitive function in unmedicated manic and medicated euthymic pediatric bipolar patients. American Journal of Psychiatry, 163(2), 286–293.
Pavuluri, M. N., West, A., Hill, S. K., Jindal, K., & Sweeney, J. A. (2009). Neurocognitive function in pediatric bipolar disorder: 3-year follow-up shows cognitive development lagging behind healthy youths. Journal of the American Academy of Child and Adolescent Psychiatry, 48(3), 299–307.
Quackenbush, D., Kutcher, S., Robertson, H. A., Boulos, C., & Chaban, P. (1996). Premorbid and postmorbid school functioning in bipolar adolescents: description and suggested academic interventions. Canadian Journal of Psychiatry, 41(1), 16–22.
Rasmussen, P., & Gillberg, C. (2000). Natural outcome of ADHD with developmental coordination disorder at age 22 years: a controlled, longitudinal, community-based study. Journal of the American Academy of Child and Adolescent Psychiatry, 39(11), 1424–1431.
Reddy, Y. C., Girimaji, S., & Srinath, S. (1997). Clinical profile of mania in children and adolescents from the Indian subcontinent. Canadian Journal of Psychiatry, 42(8), 841–846.
Reimherr, J. P., & McClellan, J. M. (2004). Diagnostic challenges in children and adolescents with psychotic disorders. Journal of Clinical Psychiatry, 65(Suppl 6), 5–11.
Rende, R., Birmaher, B., Axelson, D., Strober, M., Gill, M. K., & Valeri, S. (2006). Psychotic symptoms in pediatric bipolar disorder and family history of psychiatric illness. Journal of Affective Disorders, 96(1–2), 127–131.
Robertson, H. A., Kutcher, S. P., & Lagace, D. C. (2003). No evidence of attentional deficits in stabilized bipolar youth relative to unipolar and control comparators. Bipolar Disorder, 5(5), 330–339.
Rogers, T. T., Lambon Ralph, M. A., Garrard, P., Bozeat, S., McClelland, J. L., Hodges, J. R., & Patterson, K. (2004). Structure and deterioration of semantic memory: a neuropsychological and computational investigation. Psychological Review, 111(1), 205–235.
Rossell, S. L. (2006). Category fluency performance in patients with schizophrenia and bipolar disorder: The influence of affective categories. Schizophrenia Research, 82(2–3), 135–138.
Rucklidge, J. J. (2006). Impact of ADHD on the neurocognitive functioning of adolescents with bipolar disorder. Biological Psychiatry, 60(9), 921–928.
Sala, R., Axelson, D., & Birmaher, B. (2009). Phenomenology, longitudinal course, and outcome of children and adolescents with bipolar spectrum disorders. Child and Adolescent Psychiatric Clinics of North America, 18(2), 273–289. vii.
Sanchez-Morla, E. M., Barabash, A., Martinez-Vizcaino, V., Tabares-Seisdedos, R., Balanza-Martinez, V., Cabranes-Diaz, J. A., et al. (2009). Comparative study of neurocognitive function in euthymic bipolar patients and stabilized schizophrenic patients. Psychiatry Research, 169(3), 220–228.
Savitz, J., van der Merwe, L., Stein, D. J., Solms, M., & Ramesar, R. (2009). Neuropsychological status of bipolar I disorder: impact of psychosis. British Journal of Psychiatry, 194(3), 243–251.
Seidman, L. J., Biederman, J., Monuteaux, M. C., Doyle, A. E., & Faraone, S. V. (2001). Learning disabilities and executive dysfunction in boys with attention-deficit/hyperactivity disorder. Neuropsychology., 15(4), 544–556.
Seidman, L. J., Biederman, J., Weber, W., Hatch, M., & Faraone, S. V. (1998). Neuropsychological function in adults with attention-deficit hyperactivity disorder. Biological Psychiatry, 44(4), 260–268.
Simonsen, C., Sundet, K., Vaskinn, A., Birkenaes, A. B., Engh, J. A., & Faerden, A. (2011). Neurocognitive dysfunction in bipolar and schizophrenia spectrum disorders depends on history of psychosis rather than diagnostic group. Schizophrenia Bulletin, 37(1), 73–83.
Skirrow, C., McLoughlin, G., Kuntsi, J., & Asherson, P. (2009). Behavioral, neurocognitive and treatment overlap between attention-deficit/hyperactivity disorder and mood instability. Expert Review Neurotherapeutics, 9(4), 489–503.
Sobanski, E., Banaschewski, T., Asherson, P., Buitelaar, J., Chen, W., & Franke, B. (2010). Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51(8), 915–923.
Spatola, C. A., Fagnani, C., Pesenti-Gritti, P., Ogliari, A., Stazi, M. A., & Battaglia, M. (2007). A general population twin study of the CBCL/6-18 DSM-oriented scales. Journal of the American Academy of Child and Adolescent Psychiatry, 46(5), 619–627.
Sumiyoshi, C., Matsui, M., Sumiyoshi, T., Yamashita, I., Sumiyoshi, S., & Kurachi, M. (2001). Semantic structure in schizophrenia as assessed by the category fluency test: effect of verbal intelligence and age of onset. Psychiatry Research, 105(3), 187–199.
Sumiyoshi, C., Sumiyoshi, T., Nohara, S., Yamashita, I., Matsui, M., Kurachi, M., & Niwa, S. (2005). Disorganization of semantic memory underlies alogia in schizophrenia: an analysis of verbal fluency performance in Japanese subjects. Schizophrenia Research, 74(1), 91–100.
Szomlaiski, N., Dyrborg, J., Rasmussen, H., Schumann, T., Koch, S. V., & Bilenberg, N. (2009). Validity and clinical feasibility of the ADHD rating scale (ADHD-RS) A Danish Nationwide Multicenter Study. Acta Paediatrica, 98(2), 397–402.
Talley, J. L. (1993). Children’s auditory verbal learning test-2. Proffesional manual. In I. Psychological Assessment Resources (Ed.). Odessa, Florida.
Thorell, L. B. (2007). Do delay aversion and executive function deficits make distinct contributions to the functional impact of ADHD symptoms? A study of early academic skill deficits. Journal of Child Psychology and Psychiatry and Allied Disciplines, 48(11), 1061–1070.
Tillman, R., Geller, B., Klages, T., Corrigan, M., Bolhofner, K., & Zimerman, B. (2008). Psychotic phenomena in 257 young children and adolescents with bipolar I disorder: delusions and hallucinations (benign and pathological). Bipolar Disorder, 10(1), 45–55.
Torralva, T., Gleichgerrcht, E., Torrente, F., Roca, M., Strejilevich, S. A., Cetkovich, M., et al. (2010). Neuropsychological functioning in adult bipolar disorder and ADHD patients: A comparative study. Psychiatry Research, 186(2-3):261–6.
Torres, I. J., Defreitas, C. M., Defreitas, V. G., Bond, D. J., Kunz, M., Honer, W. G., et al. (2010). Relationship between cognitive functioning and 6-month clinical and functional outcome in patients with first manic episode bipolar I disorder. Psychological Medicine, 41(5):971–82.
Udal, A. H., Malt, U. F., Lovdahl, H., Gjaerum, B., Pripp, A. H., & Groholt, B. (2009). Motor function may differentiate attention deficit hyperactivity disorder from early onset bipolar disorder. Behavioral and brain functions, 5, 47.
Walshaw, P. D., Alloy, L. B., & Sabb, F. W. (2010). Executive function in pediatric bipolar disorder and attention-deficit hyperactivity disorder: in search of distinct phenotypic profiles. Neuropsychology Review, 20(1), 103–120.
Wechsler, D. (1991). Wechsler Intelligence Scale for Children -Third Edition (WISC-III). San Antonio: The Psychological Corporation. Wechsler, D. (1997). Wechsler Adult Intelligence Scale-III. San Antonio: The Psychological Corporation.
WHO. (1993). The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. Geneva: World Health Organization.
Willcutt, E. G., Doyle, A. E., Nigg, J. T., Faraone, S. V., & Pennington, B. F. (2005). Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biological Psychiatry, 57(11), 1336–1346.
Woo, B. S., & Rey, J. M. (2005). The validity of the DSM-IV subtypes of attention-deficit/hyperactivity disorder. Australian and New Zealand Journal of Psychiatry, 39(5), 344–353.
Youngstrom, E. A., Arnold, L. E., & Frazier, T. W. (2010). Bipolar and ADHD comorbidity: both artifact and outgrowth of shared mechanisms. Clinical psychology: a publication of the Division of Clinical Psychology of the American Psychological Association, 17(4):350–359.
Acknowledgements
Thanks to the children and their parents, my colleagues at Sörlandet Hospital, Hans Løvdahl, and statistician Are Pripp.
Financial support
Sorlandet Hospital, the South-Eastern Norway Regional Health Authority, and the Centre for Child and Adolescent Mental Health, Eastern and Southern Norway
Authors contribution
AHU (main author): Conception, design, and the acquisition, analysis, and interpretation of data. Drafting, revising, and final approval of the manuscript.
BØ and JE: Design and acquisition and interpretation of data. Drafting, revising, and final approval of the manuscript.
UFM: Conception, planning, and design of the study. Supervised the first application for financial support. Important intellectual revisions and final approval of the manuscript.
BG: Conception, design, and interpretation of data. Drafting, important intellectual revisions, and final approval of the manuscript.
Competing interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Udal, A.H., Øygarden, B., Egeland, J. et al. Memory in Early Onset Bipolar Disorder and Attention-Deficit/Hyperactivity Disorder: Similarities and Differences. J Abnorm Child Psychol 40, 1179–1192 (2012). https://doi.org/10.1007/s10802-012-9631-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-012-9631-x