Abstract
Predictors of attrition from individual parent–child interaction therapy were examined for 99 families of preschoolers with disruptive behavior disorders. Seventy-one percent of treatment dropouts were identified by lower SES, more maternal negative talk, and less maternal total praise at pretreatment. Following PCIT, families were randomly assigned to an Assessment-Only or Maintenance Treatment condition. Higher maternal distress predicted 63% of dropouts in the Assessment-Only condition. Lower maternal intellectual functioning predicted 83% of dropouts from Maintenance Treatment. Findings highlight a continuing need for evidence-based retention strategies at various phases of engagement in PCIT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Predicting Treatment and Follow-up Attrition in Parent–Child Interaction Therapy
Disruptive behavior disorders (DBDs) constitute the most common reason for referral to child mental health clinics (Loeber et al. 2000). These conditions include oppositional defiant disorder (ODD) and conduct disorder (CD) and are characterized by disregard for authority and violation of social norms and others’ rights, respectively (American Psychiatric Association [APA] 2000). Disruptive behavior disorders affect as many at 16% of children (APA 2000) and are associated with significant impairments in social, emotional, and educational functioning (Frick and Loney 1999).
Left untreated, DBDs show a high degree of stability over time (Campbell 2002; Farrington 1995; Lahey et al. 1995) and carry a high societal price tag. Children with these disorders account for a larger percentage of health care costs than children with chronic health conditions, such as asthma, diabetes, or epilepsy (Guevara et al. 2003). In young children, DBDs are the most powerful risk factor for subsequent delinquent behavior, including interpersonal violence, substance abuse, and property destruction (Loeber et al. 2000; Gau et al. 2007).
Early intervention for children with DBDs is important. Families of young children are more apt to complete treatment than families of older children (Dishion and Patterson 1992), and positive treatment-related behavior changes in young children with DBDs tend to last over long periods of time (Eyberg et al. 1998; Hood and Eyberg 2003; Reid et al. 2003). In contrast, attrition is likely related to the absence of behavior change during treatment for young children and to maintenance of their disruptive behavior over time (Boggs et al. 2004).
Attrition is difficult to study because families electing not to return to treatment tend not to return for assessment. It also complicates the study of families that complete treatment. Attrition interferes with the random composition of research groups, reduces statistical power, and limits the external validity of findings (Kazdin 1990). The differing operational definitions of attrition also make cross-study comparisons difficult (Armbruster and Kazdin 1994). Broadly defined, attrition is premature termination decided unilaterally by the patient against therapist advice (Kazdin 1996), but the criteria for “premature” vary widely.
By any definition, the methodological and clinical implications of incomplete treatment are of concern. In family theraphy, attrition statistics range from 30 to 65% (Wierzbicki and Pekarik 1993), with families continuing to drop out during follow-up periods at high rates (40% in Cohen et al. 2005; 22% in Flannery-Schroeder et al. 2005; 22% in Webster-Stratton 1990). These very high rates make continued study of attrition essential.
Attrition researchers have cautioned against the “uniformity assumption”—the notion that predictors of dropout are similar, or uniform, across different variables such as child age, clinical diagnosis, treatment program, or treatment modality (Armbruster and Kazdin 1994, p. 100). Several studies refute the uniformity assumption. For example, in treatments for externalizing behaviors, higher problem severity has predicted attrition (Kazdin 1990), whereas for internalizing behaviors, lower severity is related to attrition (Kendall and Sugarman 1997; Flannery-Schroeder et al. 2005). Predictors of attrition may also vary depending on when in the process of engaging in treatment families drop out (McKay and Bannon 2004). Kazdin and Mazurick (1994) found that dropouts from earlier relative to later sessions of treatment for DBDs were significantly more often highly stressed single parents of minority group membership. Nevertheless, among treatments for DBDs certain demographic and maternal characteristics have repeatedly been associated with dropout. Specifically, low socioeconomic status (SES), single motherhood, ethnic minority status, and high maternal stress have been identified across treatments (Armbruster and Fallon 1994; Kazdin et al. 2005; Prinz and Miller 1994; McCabe 2002; Peters et al. 2005).
Researchers have recently formulated a “barriers to treatment model,” which posits a range of obstacles that may interfere with families’ attendance, participation, and continuation in treatment (Nock and Ferriter 2005, p. 154). Variables such as parent perceptions of treatment relevance (Nock and Kazdin 2001), support by the therapist (Harwood and Eyberg 2004), and logistical barriers, such as transportation (Kazdin et al. 1997), have all been implicated in attrition. Furthermore, family variables, such as low SES, may influence parental perceptions of barriers, which then predict attrition (Nock and Kazdin 2001). Similar variables have been implicated in attrition from prevention studies. One universal prevention study found that socioeconomic disadvantage was related to lower initial project participation, and logistical barriers were most frequently cited to explain non-participation in the parent training component (Heinrichs et al. 2005).
Less is known about attrition from follow-up studies of treatments for DBDs. Follow-up studies have focused primarily on child diagnostic rates (Cohen et al. 2005; Flannery-Schroeder et al. 2005) or significant changes from pretreatment (Eyberg et al. 2001), rather than predictors of attrition. However, follow-up studies provide important information on the durability of treatment gains over time and the developmental trajectory of psychopathology. Attrition from follow-up, therefore, prevents acquisition of clinically important information (e.g., need for a booster session) and carries with it similar methodological problems as attrition from treatment.
The DBD treatment research with young children has been mixed regarding differences between follow-up completers and dropouts. Webster-Stratton (1990) found no differences at either pre- or post-treatment on a variety of variables. In contrast, Hood and Eyberg (2003) found that mothers participating in follow-up were older and had higher intellectual screening scores than mothers lost to follow-up. Compared to follow-up completers, follow-up dropouts have also reported less satisfaction with treatment (Brestan et al. 1999; Luk et al. 2001).
This study examined conceptually based predictors of attrition from an evidence-based DBD treatment—individual parent–child interaction therapy (PCIT; Eyberg et al. 2008)—and from two, 2-year follow-up conditions after completion of PCIT. PCIT outcome studies have demonstrated increases in positive parenting behaviors (e.g., praise, reflective listening) and decreases in negative parenting behaviors (e.g., criticism, sarcasm) at treatment completion, as well as increases in child compliance and decreases in deviant child behaviors (Bagner and Eyberg 2007; Eisenstadt et al. 1993; Eyberg et al. 2001). Improvements in parenting stress and parenting locus of control, and high satisfaction with treatment have also been found after PCIT (Bagner and Eyberg 2007; Nixon et al. 2003; Schuhmann et al. 1998). PCIT is not time-limited and continues until parents reach pre-set skill levels and rate their child’s behavior within normal limits. Treatment attrition in PCIT is defined as discontinuing treatment at any point after attending the first treatment session and before meeting the treatment completion criteria. In an earlier study (Werba et al. 2006), attrition from PCIT was 33%.
In the Werba et al. (2006) study, potential pretreatment predictors of attrition were explored with multiple logistic regression. Dropouts (n = 17) and completers (n = 33) were compared on numerous variables, including demographic, maternal, and child characteristics, logistical barriers, and observational variables from mother–child interactions. Results indicated that only Maternal Distress (a variable created from scores on the Beck Depression Inventory and the Parenting Stress Index) and Maternal Negative Talk (combining observed criticism and sarcasm toward the child) predicted dropout (approximately 56% reliably predicted). Maternal parenting stress also predicted attrition from PCIT in a study by Capage et al. (2001).
Using a continuous enhancement approach (Nock and Ferriter 2005), changes were made to the PCIT protocol in response to the Werba et al. (2006) findings, to reduce attrition by specifically targeting maternal distress. Prinz and Miller (2004) had previously shown that addressing parents’ life concerns beyond their child during parent training sessions significantly reduced attrition. Although PCIT therapists were required to allot a brief time in each session to address parents’ personal concerns, this enhancement was not implemented in a controlled or highly structured way.
A second change to the protocol was also made to decrease attrition. This change was based on evidence that logistical barriers can predict dropout (Kazdin et al. 1997) and on retrospective parent reports (n = 31) from an earlier PCIT study (Boggs et al. 2004) in which parents reported their primary reasons for dropping out were logistical, specifically inability to obtain transportation or child-care for siblings (n = 11, or 35%). In response, this study protocol included provision of child care for siblings of target children during treatment sessions and monetary reimbursement for transportation (US$3.00 per visit).
The purpose of this study was to examine conceptually based pretreatment predictors of attrition during PCIT and during the follow-up period. Earlier studies had shown that maternal criticism predicted child outcomes from parent training (Webster-Stratton 1996) and also predicted attrition from PCIT (Werba et al. 2006). Therefore, we expected Maternal Negative Talk would predict treatment attrition in this study. Werba et al. (2006) had also examined maternal prosocial behavior, a broad composite category of positive attention, but did not find that it distinguished dropouts from completers. In this study, we narrowed the construct of prosocial behavior to include only Maternal Total Praise, a more salient counterpart to Maternal Negative Talk, and hypothesized this variable would predict dropout.
SES has emerged as a predictor of dropout in many parent training studies (Kazdin 1990; Kazdin et al. 1993; Kazdin and Mazurick 1994; McCabe 2002; Prinz and Miller 1994) and has been related to non-participation in prevention studies as well (Heinrichs et al. 2005). We therefore included SES among our potential predictors of attrition. Finally, we included Maternal Distress to examine whether this variable remained a predictor of attrition from PCIT using the revised PCIT protocol.
This study also examined potential predictors of attrition during the PCIT follow-up period. Treatment completers had been randomized into maintenance treatment (MT) or assessment-only (AO) during the 2-year follow-up period. For both conditions, follow-up completion was defined as participating in the final 2-year assessment. We retained Maternal Distress as a potential predictor of follow-up attrition for families in the AO condition based on findings from earlier studies suggesting that improvements in parenting stress may not be maintained after treatment ends (Eyberg et al. 2001) and that loss of emotional support from therapists when treatment ends might negatively affect maintenance of treatment gains (Bagner and Eyberg 2003). Additionally, because a continuing relationship between therapist and parents during follow-up has been linked to increased retention (Capaldi and Patterson 1987), we expected attrition to be lower for families receiving maintenance treatment in the follow-up period. Finally, we examined maternal age and intellectual functioning as well as treatment satisfaction as potential predictors of attrition from follow-up based on findings from earlier PCIT follow-up studies (Brestan et al. 1999; Hood and Eyberg 2003)
We hypothesized that treatment attrition would be predicted by a linear combination of variables including Maternal Total Praise, Maternal Negative Talk, Maternal Distress, and SES, with Maternal Distress contributing least to the equation. We hypothesized that follow-up attrition would be predicted by a linear combination of variables including Maternal Age, Maternal Intellectual Functioning, Maternal Distress, and Treatment Satisfaction, with Maternal Distress significantly predicting attrition only for families not receiving maintenance treatment in follow-up. Our final hypothesis was that attrition would be lower for families in MT than families in AO.
Method
Participants
Participants were 99 mother–child dyads with 3- to 6-year-old children with DBDs enrolled in a treatment study examining the efficacy of maintenance treatment (aimed at maintaining the changes in child behavior and maternal distress seen at treatment completion). Children (69 boys, 30 girls) were referred to the PCIT laboratory for treatment of difficult-to-manage behavior by pediatricians, child psychiatrists, child neurologists, teachers, and day care providers. The children’s mean age was 4 years, 4 months (SD = 1 year, 1 month), and racial/ethnic composition was 76% Caucasian, 11% Biracial, 8% African American, 4% Hispanic, and 1% Asian. For caregivers, the racial/ethnic breakdown was 84% Caucasian, 7% African American, 5% Biracial, and 4% Hispanic. With all five socioeconomic categories represented, families had a mean SES of 38.44 (SD = 13.98), placing them, on average, in the lower middle SES range (e.g., skilled craftsmen, clerical, sales workers) according to the Hollingshead ((1975). Four-Factor Index of Social Status. Unpublished manuscript, Yale University, New Haven, CT) Index. Maternal caregivers included 92% biological or adoptive mothers, 3% stepmothers, 4% grandmothers, and one foster mother. Maternal caregivers’ mean age was 33 years, 9 months (SD = 9 years, 6 months), and most were married (58%), divorced (17%), single (17%), or separated (6%); one mother was widowed. For inclusion in this study, children had to meet Jensen et al. (1996) criteria for oppositional defiant disorder (ODD), which requires both categorical and dimensional indices of the disorder. The children met diagnostic criteria for ODD on the Diagnostic Interview Schedule for Children-IV-Parent (DISC-IV; Shaffer et al. 2000) and obtained a clinically elevated (T > 61) score on the Aggressive Behavior subscale of the Child Behavior Checklist (CBCL/2–3; Achenbach 1992; CBCL/4–18; Achenbach 1991). Parents also had to obtain a standard score of at least 75 on a cognitive screening measure (Wonderlic Personnel Test [WPT] Dodrill 1981) and children had to obtain a standard score of at least 70 on the Peabody Picture Vocabulary Test-III (PPVT-III; Dunn and Dunn 1997). Children were excluded if parents described severe sensory or mental impairment (e.g., blindness, autism) during the clinical interview. Children taking psychotropic medications to help manage their behavior (29%) had to maintain a consistent medication regimen and dosage schedule for at least one month before enrolling in the study, and caregivers were asked not to alter their child’s medication or dosage during treatment. Parents of children not taking psychotropic medication were asked not to begin medication for their child during treatment. In addition to ODD, children in this study met DISC-IV criteria for attention-deficit/hyperactivity disorder (ADHD; 74%), conduct disorder (CD; 46%), separation anxiety disorder (SAD; 26%), and major depressive disorder (MDD; 4%).
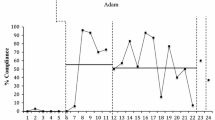
Of the 99 families that participated in PCIT, 63 completed treatment, with a mean of 17 (SD = 5) sessions. Treatment dropouts completed a mean of 9 (SD = 7) sessions (median = 6.5 sessions). Following treatment, 32 families were randomly assigned to an Assessment-Only (AO) follow-up condition and 31 to a Maintenance Treatment (MT) condition (Fig. 1).
Children in the AO condition (22 boys, 10 girls) had a mean age of 4 years, 6 months (SD = 1 year), and their racial/ethnic composition was 81% Caucasian, 13% Biracial, 3% African American, and 3% Asian. In addition to ODD, they met diagnostic criteria for ADHD (65%), CD (46%), SAD (21%), and MDD (6%). Their maternal caregivers included 97% biological or adoptive mothers and 3% stepmothers, with a mean age of 34 years (SD = 9 years). They were 94% Caucasian and 6% Biracial, and most (61%) were married; 23% were divorced, 10% single, and 7% separated. The AO families had a mean Hollingshead ((1995). Four-Factor Index of Social Status. Unpublished manuscript, Yale University, New Haven, (T) SES score of 41.16 (SD = 14.66).
Children in the MT condition (20 boys, 11 girls) had a mean age of 4 years, 4 months (SD = 12 months), and their racial/ethnic composition was 71% Caucasian, 13% Biracial, 10% African American, and 7% Hispanic. In addition to ODD, they met diagnostic criteria for ADHD (78%), CD (43%), SAD (33%), and MDD (3%). Maternal caregivers were 90% biological or adoptive mothers, 7% grandmothers, and 3% stepmothers, with a mean age of 36 years (SD = 9.5 years). They were 77% Caucasian, 10% African American, 7% Hispanic, and 7% Biracial, and 57% were married, 20% divorced, 17% single, 3% separated, and 3% widowed. Their mean Hollingshead SES score was 36.20 (SD = 9.41). Family demographic variables differed between the MT and AO condition only on maternal age, t(52) = −0.83, p < 0.01, such that the mean age of maternal caregivers was significantly higher in the MT group.
Demographic Measures
A demographic questionnaire provided information on age, sex, race/ethnicity, occupation, education level, and marital status of family members. The Hollingshead Four Factor Index of Social Status (Hollingshead 1975. Four-Factor Index of Social Status. Unpublished manuscript, Yale University, New Haven, CT), calculated from parent education, occupation, sex, and marital status reported on the demographic questionnaire, was used to measure family SES.
Diagnostic Measures
Three measures were used to screen for ODD. The Diagnostic Interview Schedule for Children, Fourth Edition, Parent (DISC-IV-P; Shaffer et al. 2000) was administered to assess ODD symptom frequency and duration as well as functional impairment in the home and school settings. In its earlier versions, the DISC was shown to have moderate to substantial test–retest reliability and internal consistency (Fisher et al. 1993; Jensen et al. 1995), and the test–retest reliability of the DISC-IV compares favorably with the earlier versions (Shaffer et al.).
The Child Behavior Checklist for 4 to 18 year olds (CBCL/4–18; Achenbach 1991) consists of 118 items rated by the parent on a three-point scale from (0) not true to (2) very true or often true to assess symptoms of child psychopathology during the past six months. One-week test–retest reliability for the CBCL/4–18 Aggressive subscale has been reported at 0.91 (Achenbach 1991).
The Child Behavior Checklist for 2 to 3 year olds (CBCL/2–3; Achenbach 1992) is similar in format to the CBCL/4–18 and contains 99 items rated by the parent for frequency in the past two months on a three-point scale. Test–retest reliability of the CBCL/2–3 Aggressive subscale has been reported at 0.85 over a 3-week period (Koot et al. 1997).
Cognitive Screening Measures
Cognitive screening of parents was completed using the Wonderlic Personnel Test (WPT; Dodrill 1981), a 12-minute timed test developed to screen adult intellectual ability that correlates with WAIS Full Scale IQ scores at 0.93 (Dodrill 1981). The Peabody Picture Vocabulary Test, Third Edition (PPVT-III; Dunn and Dunn 1997) was used to screen children in this study. The PPVT-III is a well-standardized measure of receptive language, which correlates highly (0.90) with the Wechsler Intelligence Scale for Children III (WISC-III) Full Scale IQ.
Maternal Distress Variable
Consistent with earlier research (Werba et al. 2006), we found a strong correlation (0.58) between total scores on the Beck Depression Inventory, Second Edition (BDI-II; Beck et al. 1996) and the Parenting Stress Index, Short Form (PSI-SF; Abidin 1995). Therefore, scores on these two measures were standardized and combined as in Werba et al. into a composite Maternal Distress variable. The PSI-SF is a 36-item parent self-report scale that measures stress in the parent–child relationship due to parent distress, difficult child behavior, and dysfunctional parent–child interaction. The BDI-II is a 21-item multiple-choice self-report measure of depressive symptomatology. Studies have reported 1-week test–retest reliability at 0.93 (Beck, Steer, & Brown). Internal consistency for the Maternal Distress composite score created for this study was acceptable at 0.72 (Streiner 2003).
Observational Measures
Two composite variables from the Dyadic Parent–Child Interaction Coding System, Second Edition (DPICS-II; Eyberg et al. 1994) were created for this study. The DPICS is a behavioral coding system that measures the quality of parent–child social interactions during three 5-minute standard situations (Child-Led Play, Parent-Led Play, and Clean-Up) that vary in the degree of parental control required. Four categories of maternal verbalization coded during these parent–child interaction observations were analyzed for this study: Criticism, Smart Talk (sarcasm), Labeled Praise, and Unlabeled Praise. Criticism and Smart Talk were combined into one composite Negative Talk category, and Labeled and Unlabeled Praise were combined into one composite Total Praise category. Kappas for Criticism, Smart Talk, Labeled Praise, and Unlabeled Praise were 0.51, 0.33, 0.64, and 0.87, respectively. Because the Kappa value for Smart Talk was unacceptably low (Fleiss 1981), we examined the Kappa confusion matrix, which indicated that whenever one of two observers coded a Smart Talk and the other coded another category, the other category was Criticism in 100% of occurrences. Similarly, when one of two observers coded Criticism and the other coded another category, that other category was Smart Talk in 100% of occurrences. Thus, by combining these two categories into the single composite Negative Talk category, the data set for Negative Talk contained no inter-coder disagreements and the conceptual overlap of the variables was addressed.
Consumer Satisfaction
Following treatment, caregivers completed the Therapy Attitude Inventory (TAI), a parent-report instrument specifically designed to evaluate consumer satisfaction after parent training, parent–child treatments, and family therapy (Eyberg 1993). The TAI includes 10 items addressing the impact of therapy on parenting skills and child behavior. Parents rate items on a scale from (1) dissatisfaction with treatment or worsening of problems to (5) maximum satisfaction with treatment or improvement of problems. The item ratings are summed to yield a total score between 10 and 50. Earlier studies have demonstrated 4-month test–retest stability (0.85; Brestan et al. 1999) and internal consistency (0.88; Eisenstadt et al. 1993), and TAI scores from different parent training programs have provided evidence of discriminative validity (Eyberg and Matarazzo 1980). Cronbach’s alpha for the TAI in this study was 0.78 at posttreatment.
Procedure
Families were screened for inclusion during the first of two pre-treatment assessment visits. These visits included a clinical interview and child diagnostic interview with the parents, cognitive screening measures, and several questionnaires including a demographic questionnaire, the BDI-II, and the PSI-SF. At each visit, parent–child dyads were also videotaped in three structured play situations later coded using the DPICS. Families were then seen for PCIT by two graduate student co-therapists during weekly one-hour sessions, which were videotaped for later integrity checking. All sessions were conducted according to procedures outlined in the treatment manual (Eyberg and the Child Study Laboratory 1999). Therapists, who were unaware of the hypotheses of this study, were asked to record the reason(s) for dropout for any family that discontinued treatment prematurely.
Following completion of PCIT, families were randomly assigned to either a Maintenance Treatment (MT) or follow-up Assessment-Only (AO) condition. Families receiving MT (n = 31) were called once per month by their PCIT therapist to assess maintenance of change in child behavior and parenting stress and to provide support or advice as indicated. Families in both groups were contacted by phone once every three months by an assessor masked to their follow-up condition (i.e., MT versus AO) to complete measures relating to child behavior and maternal functioning. At 1-year and 2-year follow-up points, families were seen again for full, two-visit assessments that included the questionnaires and behavioral observation measures.
Undergraduate research assistants used session checklists from the treatment manual (Eyberg and Members of the Child Study Laboratory 1999) to code treatment integrity for a randomly selected 50% of session videotapes for each family. Checklist items included both content (e.g., “Coach second parent with child for about 10 min”) and process (e.g., “Discussed or inquired about issue unrelated to child behavior”) items. Treatment integrity, calculated as percent agreement with the session checklist, was 90%. A randomly selected 50% of the coded session tapes were recoded by a second undergraduate research assistant to assess the reliability of the treatment integrity coding. Intercoder percentage agreement reliability was 91%. A similar procedure was used to code audiotapes of maintenance treatment calls and calculate maintenance treatment integrity (97%). Intercoder percentage agreement reliability for maintenance treatment was also 97%.
Analyses of Observational Data
At the pre-treatment, post-treatment, and 1- and 2-year follow up assessments, parents and children were observed in three 5-minute structured play situations (Child-Led Play, Parent-Led Play, and Clean Up) on two occasions, one week apart. For this study, only the pretreatment data from the Parent-Led Play (PLP) and Clean Up (CU) situations were used. Frequency counts for both categories of verbalization, Maternal Negative Talk and Maternal Total Praise, were calculated and averaged across the two pretreatment assessment sessions. Frequencies of each verbalization category were then averaged across the PLP and CU observation situations. When one of the two observations of the same situation was missing due to assessor error in video recording or technical problems with the recording equipment, data from the available observation was substituted for an average of the two observations. Because the observational data were positively skewed, log transformations were performed to normalize distributions. Because there were cases in which no Total Praise or Negative Talk occurred, a nominal value of 0.01 was added to all 0 values prior to transformation because 0 values cannot undergo log transformation. Log transformations resulted in kurtosis and skewness values within acceptable limits (i.e., < | 2 |), except for Total Praise, which remained kurtotic (kurtosis = 3.24).
Results
Treatment Attrition
Treatment attrition was 36% in this study. Primary reasons for dropout were obtained for 31 of 36 (86%) families and are listed in Table 1. The most common reason for dropout was disagreement with the treatment approach (26%), followed by being too busy to participate in treatment (13%), having additional stressors that interfered with treatment participation (13%), or having logistical problems that interfered (13%).
Discriminant function analysis (DFA) was conducted to identify a linear combination of variables predictive of group membership (treatment completers versus dropouts). Total Praise, Negative Talk, SES, and Maternal Distress were included as independent variables. Initial evaluation of the data suggested that SES and Maternal Distress were univariate normal, with skewness and kurtosis estimates less than | 1 |. Intercorrelations among potential predictor variables for treatment attrition are presented in Table 2.
The discriminant function was significant, Wilk’s λ = 0.85, χ2 (4, N = 95) = 14.59, p = 0.006. Examination of standardized canonical discriminant function coefficients suggested that when controlling for the remaining predictors, SES was the best predictor of group membership (0.67), followed by Negative Talk (−0.48), Total Praise (0.35), and Maternal Distress (0.27). Afifi and Clark (1996) recommend a cutoff value of 0.3 for interpreting predictor variables. Therefore, treatment dropout was predicted by lower SES, more Maternal Negative Talk, and less Maternal Total Praise, but not Maternal Distress. Of the 38 caregivers who entered treatment with clinically elevated depression (BDI-II score > 14) and parenting stress (PSI-SF score > 90), 61% (23 of 38) completed treatment. Of these 23 completers, 65% (15 of 23) no longer reported clinically significant levels of distress on either measure at posttreatment.
A jackknife procedure was used to obtain a cross-validation estimate to account for potential sample bias and provide a more conservative estimate of outcome classification. Using this procedure, 62% of families were classified correctly. For dropouts, 24 of 34 (71%) families were classified correctly and for completers, 35 of 61 (57%) families were classified correctly.
Follow-up Attrition in the Assessment-Only Condition
Follow-up attrition was 53% in the AO condition. A DFA was conducted to identify predictors of follow-up completion versus dropout in AO families. Maternal Distress, Maternal Intellectual Functioning, Maternal Age, and Treatment Satisfaction were included as potential predictor variables. Except for Treatment Satisfaction, the variables were roughly univariate normal, with skewness and kurtosis estimates less than | 1 |. Treatment Satisfaction was negatively skewed (> | 1 |); the distribution was normalized using square root transformation. Table 3 shows the intercorrelations among these four potential predictors. The discriminant function was not significant, Wilk’s λ = 0.76, χ2 (4, N = 26) = 6.10, p = 0.192. Maternal Distress alone predicted 63% of AO attrition.
Follow-up Attrition in the Maintenance Treatment Condition
Attrition was 39% in the MT condition. A separate DFA was conducted in this condition to identify variables predicting follow-up MT attrition. To reduce the potential confound of age emerging as a significant predictor of follow-up status, two participants whose ages represented outliers (defined as three standard deviations from the mean) were excluded from this analysis. Intercorrelations among four potential predictor variables are shown in Table 4.
The MT discriminant function was significant, Wilk’s λ = 0.55, χ2 (4, N = 27) = 13.75, p = 0.008. Standardized canonical discriminant function coefficients suggested that when controlling for remaining predictors, Maternal Intellectual Functioning was the best predictor of attrition versus completion (0.91), followed by Maternal Distress (−0.29), Treatment Satisfaction (0.27), and Maternal Age (0.26). Using 0.3 as the cutoff for interpreting predictor variables, lower intellectual functioning alone predicted dropout in the MT condition. After applying the jackknife procedure, results indicated correct classification for 78% of all MT families. Among MT dropout families, 10 of 12 (83%) were classified correctly, and among MT completers, 11 of 15 (73%) were classified correctly.
Differences in Attrition Between Follow-up Conditions
To test the significance of the difference in dropout rates between AO (53%) and MT (39%) conditions, we calculated a z score by dividing the observed difference between rates by the estimate of the standard error of the difference. The proportion of families that dropped out of MT (12 of 31) did not differ significantly from the proportion that dropped out of AO during follow-up (17 of 32), z = 0.13, p = 0.55.
Discussion
This study identified conceptually based, pretreatment predictors of attrition from PCIT and from a 2-year follow-up period of either maintenance treatment or assessment-only. Family SES and both positive and negative maternal verbalizations during parent–child interactions predicted whether families completed or dropped out of treatment. In the absence of maintenance treatment, maternal distress predicted attrition during the follow-up period. Maternal intellectual functioning predicted attrition from maintenance treatment in follow-up.
Observational data are rarely examined as potential predictors in studies of treatment attrition, despite promising results from several studies (Bischoff and Sprenkle 1993; Harwood and Eyberg 2004). This study found that both negative and positive maternal evaluative statements during pretreatment observations of parent–child interactions were independently predictive of treatment attrition from PCIT. We have previously shown that positive changes in these same parent verbal behaviors mediate the change in child disruptive behaviors during PCIT (Bagner and Eyberg 2007). It may not be surprising that observational measures reflecting maternal attitudes toward the child predict dropout in PCIT; PCIT demands parents’ time and effort in learning and practicing new ways of communicating that may not only be unfamiliar but also incongruent with their current attitudes toward their child. Indeed, 26% of treatment dropouts reported their primary reason was disagreement with the treatment approach.
Our findings underscore the importance of emphasizing in the initial interview the role of positive parent–child interactions in changing children’s behaviors, as well as the sustained efforts required of parents in treatment to master new parent–child communication skills. In addition to conveying the demands of treatment clearly at the outset and clarifying parent expectations (Nock and Kazdin 2001), continued study of the therapeutic alliance (Garcia and Weisz 2002; Kazdin et al. 2005) and therapist verbal behaviors in the initial interview that relate to attrition and retention (Harwood and Eyberg 2004) are essential. Incorporating motivational interventions with families has been found to increase session attendance and retention in parent training (Nock and Kazdin 2005) and to increase retention in PCIT specifically (Chaffin et al. 2008). Fully integrating motivational interviewing into parent training protocols for families of children with disruptive behavior disorders is a particularly promising direction for future research.
Despite efforts to reduce burdens related to socioeconomic adversity (child care and travel costs), SES emerged in this study as the strongest predictor of attrition from PCIT, as it has in other parent training studies (Kazdin and Mazurick 1994; McCabe 2002). Simple logistical supports were insufficient in reducing the greater attrition in lower SES groups. SES is a proxy variable for many specific barriers to treatment associated with socioeconomic disadvantage, and continued research is needed in this area to identify the salient barriers affecting disadvantaged families in treatment.
One intriguing finding in this study was that maternal distress did not emerge as a predictor of dropout from PCIT, despite being implicated in dropout in two earlier PCIT studies examining attrition (Capage et al. 2001; Werba et al. 2006). Approximately 60% of maternal caregivers who reported clinical elevations in depressive symptoms and parenting stress at pretreatment completed PCIT in this study, and 65% of these completers no longer reported clinical elevations in either variable following treatment. The brief parent support component added to PCIT sessions in response to earlier findings may have contributed to the greater retention of distressed maternal caregivers, although this hypothesis was not examined experimentally. That is, families were not randomly assigned to an additional support condition or a no additional support condition during standard treatment; all families received the revised protocol. Thus, we cannot definitively conclude that changes made to the protocol affected our results.
Inclusion of both AO and MT conditions in the follow-up analyses provided additional insight into the role of maternal distress in attrition from follow-up. In families that maintained contact with their therapist during the follow-up period through regular monthly telephone check-ups and assistance when needed, maternal distress remained unrelated to attrition during follow-up. However, maternal distress reappeared as a predictor of dropout for families not receiving therapist contact during the follow-up period.
Ongoing therapist support may represent a successful retention strategy for distressed families after treatment. Still, the format of the maintenance sessions may have been less helpful for caregivers with lower intellectual functioning. Maternal intellectual functioning was the only predictor of dropout versus completion of study follow-up for families receiving maintenance treatment. In telephone sessions, problem-solving is necessarily more abstract than in-session observation and direct modeling and coaching of strategies identified for problem resolution. The development of effective maintenance treatment protocols tailored to individual needs is a critically important direction for intervention research with young children.
We also found treatment satisfaction unrelated to follow-up attrition. This finding may have been due to a restricted range of treatment satisfaction scores. With a raw score of 50 representing highest satisfaction, 71% of families scored between 45 and 50 (92% between 40 and 50). Although such high satisfaction ratings limit our understanding of how treatment satisfaction may affect attrition in follow-up, they are consistent with previous findings suggesting that parents who complete PCIT are highly pleased with the process and outcome of their treatment (Brestan et al. 1999). In light of findings indicating less satisfaction among families that drop out of PCIT (Brestan et al. 1999), it may be useful to obtain consumer satisfaction ratings periodically during treatment to address lower satisfaction before families drop out.
Contrary to our hypothesis, attrition rates did not differ significantly between follow-up conditions. The 36% treatment attrition rate in this study was consistent with rates obtained in earlier PCIT studies of children with DBDs (e.g., 35% in Eisenstadt et al. 1993; 33% in Werba et al. 2006), and the follow-up attrition rate was relatively high at 53% in the AO condition and 39% in the MT condition. Future study of PCIT may extend motivational enhancements into the follow-up period as a means of increasing retention during this time.
Sample size limited the number of variables that could be examined as predictors of attrition in this study and precluded inclusion of paternal caregivers in our analyses. In light of findings that suggest father involvement in PCIT may relate to improved long-term outcome, it will be important in future research to consider the unique role that father variables may play in predicting attrition. Although research suggests that predictors may differ depending on the point at which families disengage from the treatment process (Kazdin and Mazurick 1994; McKay and Bannon 2004), our sample size did not permit us to separate dropout families according to their varying points of disengagement.
The strength of this study is the identification of three conceptually based variables related to treatment attrition that together improve upon earlier predictions of PCIT attrition (Werba et al. 2006). The inclusion of observed maternal verbal behaviors during parent–child interactions at pretreatment assessment represents an important contribution to the child treatment attrition literature. The results extend the literature by elucidating predictors of follow-up attrition that led to correct classification of 63% of dropouts in the assessment-only condition and 83% in the maintenance treatment condition. Attrition from both treatment and follow-up presents a significant challenge to researchers and clinicians. Our findings point to the need for continued study of attrition and engagement throughout the process of PCIT.
References
Abidin, R. (1995). Parenting stress index manual (3rd ed.). Odessa, FL: Psychological Assessment Resources.
Achenbach, T. M. (1991). Manual for the child behavior checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry.
Achenbach, T. M. (1992). Manual for the child behavior checklist/2–3 and 1992 profile. Burlington, VT: University of Vermont Department of Psychiatry.
Afifi, A. A., & Clark, V. (1996). Computer-aided multivariate analysis. London: Chapman & Hall.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders. (4th edn., text revision). Washington, DC: American Psychiatric Association.
Armbruster, P., & Fallon, T. (1994). Clinical, sociodemographic, and systems risk factors for attrition in a children’s mental health clinic. The American Journal of Orthopsychiatry, 64, 577–585. doi:10.1037/h0079571.
Armbruster, P., & Kazdin, A. E. (1994). Attrition in child psychotherapy. Advances in Clinical Child Psychology, 16, 81–108.
Bagner, D. M., & Eyberg, S. M. (2003). Father involvement in parent training: When does it matter? Journal of Clinical Child and Adolescent Psychology, 32, 599–605. doi:10.1207/S15374424JCCP3204_13.
Bagner, D. M., & Eyberg, S. M. (2007). Parent–child interaction therapy for disruptive behavior in children with mental retardation: A randomized controlled trial. Journal of Clinical Child and Adolescent Psychology, 36, 418–429.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation.
Bischoff, R. J., & Sprenkle, D. H. (1993). Dropping out of marriage and family therapy: A critical review of research. Family Process, 32, 353–375. doi:10.1111/j.1545-5300.1993.00353.x.
Boggs, S. R., Eyberg, S. M., Edwards, D. L., Rayfield, A., Jacobs, J., Bagner, D., et al. (2004). Outcomes of parent–child interaction therapy: A comparison of treatment completers and study dropouts one to three years later. Child & Family Behavior Therapy, 26, 1–22. doi:10.1300/J019v26n04_01.
Brestan, E., Jacobs, J., Rayfield, A., & Eyberg, S. M. (1999). A consumer satisfaction measure for parent–child treatments and its relationship to measures of child behavior change. Behavior Therapy, 30, 17–30. doi:10.1016/S0005-7894(99)80043-4.
Campbell, S. B. (2002). Follow-up and outcome studies. In Behavior problems in preschool children: Clinical and developmental issues (2nd edn., pp. 241–275). New York: Guilford.
Capage, L. C., Bennett, G. M., & McNeil, C. B. (2001). A comparison between African American and Caucasian children referred for treatment of disruptive behavior disorders. Child & Family Behavior Therapy, 23, 1–14. doi:10.1300/J019v23n01_01.
Capaldi, D., & Patterson, R. (1987). An approach to the problem of recruitment and retention rates for longitudinal research. Behavioral Assessment, 9, 169–177.
Chaffin, M., Valle, L. A., Funderburk, B., Gurwitch, R., Silovsky, J., McCoy, C., et al. (2008). A motivational intervention can improve retention in PCIT for chronic child welfare clients. (provisionally accepted)
Cohen, J. A., Mannarino, A. P., & Knudsen, K. (2005). Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse & Neglect, 29, 135–145. doi:10.1016/j.chiabu.2004.12.005.
Dishion, T. J., & Patterson, G. R. (1992). Age effects in parent training outcome. Behavior Therapy, 23, 719–729. doi:10.1016/S0005-7894(05)80231-X.
Dodrill, C. B. (1981). An economical method for the evaluation of general intelligence in adults. Journal of Consulting and Clinical Psychology, 49, 668–673. doi:10.1037/0022-006X.49.5.668.
Dunn, L. M., & Dunn, L. M. (1997). Examiner’s manual for the PPVT-III: peabody picture vocabulary test (3rd ed.). Circle Pines, MN: American Guidance Services.
Eisenstadt, T. H., Eyberg, S. M., McNeil, C. B., Newcomb, K., & Funderburk, B. (1993). Parent–child interaction therapy with behavior problem children: Relative effectiveness of two stages and overall treatment outcome. Journal of Clinical Child Psychology, 22, 42–51. doi:10.1207/s15374424jccp2201_4.
Eyberg, S. M. (1993). Consumer satisfaction measures for assessing parent training programs. In L. VandeCreek, S. Knapp, & T. L. Jackson (Eds.), Innovations in Clinical Practice: A Sourcebook (Vol. 12). Sarasota: Professional Resource.
Eyberg, S. M., Bessmer, J., Newcomb, K., Edwards, D., & Robinson, E. A. (1994). Manual for the dyadic parent–child interaction coding system-II. Social and Behavioral Sciences Documents (No. 2897). Retrieved April 17, 2005, from the World Wide Web: www.pcit.org.
Eyberg, S. M., & Child Study Laboratory. (1999). Parent child interaction therapy: Integrity checklists and session materials. Retrieved July 25, 2008, from the World Wide Web: www.pcit.org.
Eyberg, S. M., Edwards, D., Boggs, S., & Foote, R. (1998). Maintaining the treatment effects of parent training: the role of booster sessions and other maintenance strategies. Clinical Psychology: Science and Practice, 5, 544–554.
Eyberg, S. M., Funderburk, B. W., Hembree-Kigin, T. L., McNeil, C. B., Querido, J. G., & Hood, K. K. (2001). Parent–child interaction therapy with behavior problem children: One and two year maintenance of treatment effects in the family. Child & Family Behavior Therapy, 23, 1–20. doi:10.1300/J019v23n04_01.
Eyberg, S. M., & Harwood, M. D. (2004). Therapist verbal behavior early in treatment: Relation to successful completion of parent–child interaction therapy. Journal of Clinical Child and Adolescent Psychology, 33, 601–612. doi:10.1207/s15374424jccp3303_17.
Eyberg, S. M., & Matarazzo, R. G. (1980). Training parents as therapists: A comparison between individual parent–child interaction training and parent group didactic training. Journal of Clinical Psychology, 42, 594–606.
Eyberg, S. M., Nelson, M. M., & Boggs, S. R. (2008). Evidence-based treatments for child and adolescent disruptive behavior disorders. Journal of Clinical Child and Adolescent Psychology, 37, 213–235. doi:10.1080/15374410701820117.
Farrington, D. P. (1995). The stability and prediction of aggressive behavior. Gruppendynamik, 26, 23–40.
Fisher, P. W., Shaffer, D., Piacentini, J., Lapkin, J., Kafantaris, V., Leonard, H., et al. (1993). Sensitivity of the diagnostic interview schedule for children, 2nd edition (DISC-2.1) for specific diagnoses of children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 32, 666–673. doi:10.1097/00004583-199305000-00026.
Flannery-Schroeder, E., Choudhury, M. S., & Kendall, P. C. (2005). Group and individual cognitive-behavioral treatments for youth with anxiety disorders: 1-year follow-up. Cognitive Therapy and Research, 29, 253–259. doi:10.1007/s10608-005-3168-z.
Fleiss, J. L. (1981). The measurement of interrater agreement. In Statistical Methods for Rates and Proportions. (2nd edn., pp. 212–304). New York: Wiley.
Frick, P. J., & Loney, B. R. (1999). Outcomes of children and adolescents with oppositional defiant disorder and conduct disorder. In H. C. Quay, & A. E. Hogan (Eds.), Handbook of disruptive behavior disorders (pp. 507–524). Dordrecht, Netherlands: Kluwer Academic.
Garcia, J. A., & Weisz, J. R. (2002). When youth mental health care stops: Therapeutic relationship problems and other reasons for ending youth outpatient treatment. Journal of Consulting and Clinical Psychology, 70, 439–443.
Gau, S. S., Chong, M. Y., Yang, P., Yen, C. F., Liang, K. Y., et al. (2007). Psychiatric and psychosocial predictors of substance use disorders among adolescents: Longitudinal study. The British Journal of Psychiatry, 190, 42–48. doi:10.1192/bjp.bp.106.022871.
Guevara, J. P., Mandell, D. S., Rostain, A. L., Zhao, H., & Hadley, T. R. (2003). National estimates of health services expenditures for children with behavioral disorders: an analysis of the medical expenditure panel survey. Pediatrics, 112, e440–e446. doi:10.1542/peds.112.6.e440.
Harwood, M. D., & Eyberg, S. M. (2004). Therapist verbal behavior early in treatment: Relation to successful completion of Parent–child interaction therapy. Journal of Clinical Child and Adolescent Psychology, 33, 601–612. doi:10.1207/s15374424jccp3303_17.
Heinrichs, N., Bertram, H., Kuschel, A., & Hahlweg, K. (2005). Parent recruitment and retention in a universal prevention program for child behavior and emotional problems: Barriers to research and program participation. Prevention Science, 6, 275–286. doi:10.1007/s11121-005-0006-1.
Hood, K. K., & Eyberg, S. M. (2003). Outcomes of Parent–child interaction therapy: Mothers’ reports of maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology, 32, 419–429. doi:10.1207/S15374424JCCP3203_10.
Jensen, P., Roper, M., Fisher, P., Piacentini, J., Canino, G., Richters, J., et al. (1995). Test–retest reliability of the diagnostic interview schedule for children (DISC 2.1). Parent, child, and combined algorithms. Archives of General Psychiatry, 52, 61–71.
Jensen, P. S., Watanabe, H. K., Richters, J. E., Roper, M., Hibbs, E. D., Salzberg, A. D., et al. (1996). Scales, diagnoses, and child psychopathology II: Comparing the CBCL and the DISC against external validators. Journal of Abnormal Child Psychology, 24, 151–168. doi:10.1007/BF01441482.
Kazdin, A. E. (1990). Premature termination from treatment among children referred for antisocial behavior. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 31, 415–425. doi:10.1111/j.1469-7610.1990.tb01578.x.
Kazdin, A. E. (1996). Dropping out of child psychotherapy: Issues for research and implications for practice. Clinical Child Psychology and Psychiatry, 1, 133–156. doi:10.1177/1359104596011012.
Kazdin, A. E., Holland, L., & Crowley, M. (1997). Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology, 65, 453–463. doi:10.1037/0022-006X.65.3.453.
Kazdin, A. E., Marciano, P. L., & Whitley, M. K. (2005). The therapeutic alliance in cognitive-behavioral treatment of children referred for oppositional, aggressive, and antisocial behavior. Journal of Consulting and Clinical Psychology, 73, 726–730. doi:10.1037/0022-006X.73.4.726.
Kazdin, A. E., & Mazurick, J. L. (1994). Dropping out of child psychotherapy: Distinguishing early and late dropouts over the course of treatment. Journal of Consulting and Clinical Psychology, 62, 1069–1074. doi:10.1037/0022-006X.62.5.1069.
Kazdin, A. E., Mazurick, J. L., & Bass, D. (1993). Risk for attrition in treatment of antisocial children and families. Journal of Clinical Child Psychology, 22, 2–16. doi:10.1207/s15374424jccp2201_1.
Kazdin, A. E., Stolar, M. J., & Marciano, P. L. (1995). Risk factors for dropping out of treatment among White and Black families. Journal of Family Psychology, 9, 402–417. doi:10.1037/0893-3200.9.4.402.
Kendall, P. C., & Sugarman, A. (1997). Attrition in the treatment of childhood anxiety disorders. Journal of Consulting and Clinical Psychology, 65, 883–888. doi:10.1037/0022-006X.65.5.883.
Koot, H. M., Van Den Oord, E. J., Verhulst, F. C., & Boomsma, D. I. (1997). Behavioral and emotional problems in young preschoolers: Cross-cultural testing of the validity of the Child Behavior Checklist/2–3. Journal of Abnormal Child Psychology, 25, 183–196. doi:10.1023/A:1025791814893.
Lahey, B. B., Loeber, R., Hart, E. L., & Frick, P. J. (1995). Four-year longitudinal study of conduct disorder in boys: Patterns and predictors of persistence. Journal of Abnormal Psychology, 104, 83–93. doi:10.1037/0021-843X.104.1.83.
Loeber, R., Burke, J. D., Lahey, B. B., Winters, A., & Zera, M. (2000). Oppositional defiant and conduct disorder: A review of the past 10 years, part I. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 1468–1484. doi:10.1097/00004583-200012000-00007.
Loeber, R., Green, S. M., Lahey, B. B., Frick, P. J., & McBurnett, K. (2000). Findings on disruptive behavior disorders from the first decade of the Developmental Trends Study. Clinical Child and Family Psychology Review, 3, 37–60. doi:10.1023/A:1009567419190.
Luk, E. S., Staiger, P. K., Mathai, J., Wong, L., Birleson, P., & Adler, R. (2001). Children with persistent conduct problems who dropout of treatment. European Child & Adolescent Psychiatry, 10, 28–36. doi:10.1007/s007870170044.
McCabe, K. M. (2002). Factors that predict premature termination among Mexican–American children in outpatient psychotherapy. Journal of Child and Family Studies, 11, 347–359. doi:10.1023/A:1016876224388.
McKay, M. M., & Bannon, W. M. (2004). Engaging families in child mental health services. Child and Adolescent Psychiatric Clinics of North America, 13, 905–921. doi:10.1016/j.chc.2004.04.001.
Nixon, R. D., Sweeney, L., Erickson, D. B., & Touyz, S. W. (2003). Parent–child interaction therapy: A comparison of standard and abbreviated treatments for oppositional defiant preschoolers. Journal of Consulting and Clinical Psychology, 71, 251–260. doi:10.1037/0022-006X.71.2.251.
Nock, M. K., & Ferriter, C. (2005). Parent management of attendance and adherence in child and adolescent therapy: A conceptual and empirical review. Clinical Child and Family Psychology Review, 8, 149–166. doi:10.1007/s10567-005-4753-0.
Nock, M. K., & Kazdin, A. E. (2001). Parent expectancies for child therapy: Assessment and relation to participation in treatment. Journal of Child and Family Studies, 10, 155–180. doi:10.1023/A:1016699424731.
Nock, M. K., & Kazdin, A. E. (2005). Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology, 73, 872–879. doi:10.1037/0022-006X.73.5.872.
Peters, S., Calam, R., & Harrington, R. (2005). Maternal attributions and expressed emotion as predictors of attendance at parent management training. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 46, 436–448. doi:10.1111/j.1469-7610.2004.00365.x.
Prinz, R. J., & Miller, G. E. (1994). Family-based treatment for childhood antisocial behavior: Experimental influences on dropout and engagement. Journal of Consulting and Clinical Psychology, 62, 645–650. doi:10.1037/0022-006X.62.3.645.
Reid, M. J., Webster-Stratton, C., & Hammond, M. (2003). Follow-up of children who received the Incredible Years intervention for Oppositional Defiant Disorder: Maintenance and prediction of 2-year outcome. Behavior Therapy, 34, 471–491. doi:10.1016/S0005-7894(03)80031-X.
Schuhmann, E. M., Foote, R. C., Eyberg, S. M., Boggs, S. R., & Algina, J. A. (1998). Efficacy of parent–child interaction therapy: Interim report of a randomized trial with short-term maintenance. Journal of Clinical Child Psychology, 27, 34–45. doi:10.1207/s15374424jccp2701_4.
Shaffer, D., Fisher, P., Lucas, C. P., Dulcan, M. K., & Schwab-Stone, M. E. (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 28–38. doi:10.1097/00004583-200001000-00014.
Streiner, D. L. (2003). Starting at the beginning: An introduction to coefficient alpha and internal consistency. Journal of Personality Assessment, 80, 99–103. doi:10.1207/S15327752JPA8001_18.
Webster-Stratton, C. (1990). Long-term follow-up of families with young conduct problem children: From preschool to grade school. Journal of Clinical Child Psychology, 19, 144–149. doi:10.1207/s15374424jccp1902_6.
Webster-Stratton, C. (1996). Early-onset conduct problems: Does gender make a difference? Journal of Consulting and Clinical Psychology, 64, 540–551. doi:10.1037/0022-006X.64.3.540.
Werba, B., Eyberg, S. M., Boggs, S. R., & Algina, J. (2006). Predicting the outcome of parent–child interaction therapy: Success and Attrition. Behavior Modification, 30, 618–646. doi:10.1177/0145445504272977.
Wierzbicki, M., & Pekarik, G. (1993). A meta-analysis of psychotherapy dropout. Professional Psychology, Research and Practice, 24, 190–195. doi:10.1037/0735-7028.24.2.190.
Author information
Authors and Affiliations
Corresponding authors
Additional information
This study was funded by the National Institute of Mental Health (RO1 MH60632). We thank the members of the UF Child Study Laboratory for their contributions to this study.
Rights and permissions
About this article
Cite this article
Fernandez, M.A., Eyberg, S.M. Predicting Treatment and Follow-up Attrition in Parent–Child Interaction Therapy. J Abnorm Child Psychol 37, 431–441 (2009). https://doi.org/10.1007/s10802-008-9281-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-008-9281-1