Abstract
Considerable research has focused on youth depression, but further information is needed to characterize different patterns of onset and recurrence during adolescence. Four outcome groups by age 20 were defined (early onset-recurrent, early-onset-desisting, later-onset, never depressed) and compared on three variables predictive of youth depression: gender, maternal depression, and interpersonal functioning. Further, it was hypothesized that the association between maternal depression and youth depression between 15 and 20 is mediated by early-onset depression and interpersonal dysfunction by age 15. Eight hundred sixteen community youth selected for depression risk by history (or absence) of maternal depression were interviewed at age 15, and 699 were included in the 5-year follow-up. Controlling for gender, early onset and interpersonal dysfunction mediated the link between maternal depression and late adolescent major depression. Different patterns for males and females were observed. For males maternal depression’s effect was mediated by early onset but not interpersonal difficulties, while for females maternal depression’s effect was mediated by interpersonal difficulties but not early onset. Maternal depression did not predict first onset of major depression after age 15. The results suggest the need for targeting the impact of maternal depression’s gender-specific effects on early youth outcomes, and also highlight the different patterns of major depression in youth and their likely implications for future course of depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adolescent depression has emerged as a well-described phenomenon and compelling research topic in the past two decades (e.g., Rao 2006; Rudolph et al. 2006). In recent community samples one-third of youth met criteria for major depressive disorder (Kessler and Walters 1998; Lewinsohn et al. 1998). The sheer prevalence suggests that there are multiple pathways to depression, with considerable heterogeneity in etiology, course, and treatment/prevention implications. As Harrington et al. (1996) noted, it is important to identify possible subtypes of adolescent depression for both theoretical and treatment reasons. To meet the challenge of greater understanding of potentially different manifestations of depressive disorders, further longitudinal studies of natural course and predictors of course are needed.
Several studies have reported naturalistic multi-year follow-ups of youth first identified as depressed in adolescence in both clinically ascertained (e.g., Harrington et al. 1990; Weissman et al. 1999) and community or mixed samples (Bardone et al. 1996; Dunn and Goodyer 2006; Fleming et al. 1993; Lewinsohn et al. 1999; Lewinsohn et al. 2000; Pine et al. 1998; Rao et al. 1999). Clinical samples have tended to report recurrent major depression rates of 60% or more, and community samples have generally reported 25–45% recurrence. Thus, while many youth have recurrence of depression in the period of adolescence–early adulthood, a substantial proportion do not, suggesting that identification of factors that distinguish among subgroups could shed light on etiological mechanisms and intervention implications. It is particularly important to distinguish between those youth who have isolated depressive reactions during adolescence that are possibly limited to the developmental demands and turbulent transitions faced by youth (Arnett 1999), and those whose depression may signal a recurrent and highly impairing course.
Unfortunately, few studies have examined predictors of recurrence or course of major depression during adolescence. Most such studies have been relatively small clinical samples, mixed child and adolescent depressions, or focused chiefly on clinical or demographic predictors (e.g., Birmaher et al. 2004; Hankin et al. 1998; Harrington et al. 1990; Kovacs 2001).
Predictors of adolescent depression more generally include female gender (e.g., Nolen-Hoeksema and Girgus 1994), parental depression (Beardslee et al. 1998), stressful events, distressing family and social circumstances, interpersonal factors (Goodman and Gotlib 1999; Hammen et al. 2004; Hammen 2008), and cognitive and emotion regulation dysfunctions (e.g., Lakdawalla et al. 2007). Such variables represent a starting point for prediction of major depression recurrence and course (Rutter et al. 2006).
One factor that has been repeatedly shown to predict recurrence in adolescence or young adulthood is parental depression. Notably, Lewinsohn et al. (2000) found that youth with prior depression were more likely to have recurrence by early adulthood if they had multiple previous episodes, family members with major depressive disorder, and for females, family conflict. Rohde et al. (2005) in the same sample found that maternal major depression was predictive of youth recurrence of depression among those with previous depression. Essau (2004), in a large cross sectional study of adolescents, also found an association between youth reports of recurrent depression and maternal history of depression. Similar findings of recurrent depression in community youth associated with parental depression have been reported (e.g., Lieb et al. 2002; see Weissman et al. 1997 for a clinically ascertained sample), although Daley et al. (2000) found that parental psychopathology and youth chronic stress predicted first onset but not recurrence of MDD.
Within longitudinal studies of offspring of depressed parents, other features of the course of adolescent depression have been examined to a limited extent. Weissman et al. (2006) followed offspring and control samples for 20 years. They reported that among offspring who had major depression there were no differences in rates of recurrence between groups with depressed and nondepressed parents, although offspring of depressed parents had higher rates of depression and other pathology overall. Weissman and colleagues (2006) noted, however, that for both offspring samples the peak age of onset of major depression was in the period of 15–20, but with offspring of depressed parents tending to develop depression younger (age 16) compared to offspring of nondepressed parents (age 19).
A link between parental depression and youth social dysfunction has been commonly observed in families of depressed parents (Goodman and Gotlib 1999; Lovejoy et al. 2000). In support of an interpersonal dysfunction model of youth depression, Hammen et al. (2004) found that the association between maternal depression and adolescent depression at age 15 was accounted for by interpersonal variables that measured family discord and youth interpersonal stress and social competence, although the study was limited to cross sectional analyses. In the same project Hammen and Brennan (2001) observed that the interpersonal functioning profiles of depressed adolescents differed by maternal depression status. The depressed youth of depressed mothers had significantly more evidence of peer and family maladjustment compared to equally depressed offspring of nondepressed mothers (Hammen and Brennan 2001). We speculated that the depressed youth of depressed mothers, because of their greater social dysfunction and its likely contribution to stressful events and circumstances, would be at higher risk for recurrence of depressive episodes during later adolescence than would depressed youth of the nondepressed women. The current study is a longitudinal follow-up to pursue such hypotheses. Gender differences in depression outcomes and their association with maternal depression and interpersonal functioning were explored in view of extensive evidence of gender differences in rates of adolescent depression and their likely predictors (e.g., Nolen-Hoeksema and Girgus 1994; Rudolph 2002; Silberg et al. 2001).
The study has two goals. First, patterns of depression course through late adolescence (age 20) are characterized, based on longitudinal assessments conducted at ages 15 and 20. This period is known to be associated with dramatically increasing rates of depression especially for girls (e.g., Costello et al. 2003; Hankin et al. 1998; Lewinsohn et al. 1993). Four naturally occurring, rationally derived, patterns are described: early onset depression by age 15 that recurs by age 20; early onset depression that does not recur; first onset of depression after age 15; and never depressed. These groups were defined for purposes of comparison on several factors commonly associated with youth depression—gender, maternal depression, and interpersonal dysfunction at age 15. One question, for example, is whether maternal depression continues to predict first onset of depression throughout adolescence, or is it more likely to predict only early onset depression?
Second, following predictions in Hammen and Brennan (2001), we hypothesize and test a pathway to depression recurrence in which maternal depression predicts both early onset depression and interpersonal dysfunction by age 15, and those variables in turn predict depression occurrence after age 15, such that the link between maternal and youth later adolescent depression is mediated by the early onset depression and interpersonal dysfunction. Results supporting this pattern would clarify a mechanism by which maternal depression affects the course of youth depression—by contributing to interpersonal difficulties which may cause the youth to experience depression, and by contributing to the vulnerability to experience early-onset depression which increases risk for depression recurrence.
The present community sample is well-suited to assess the patterns of depression during adolescence. It has the advantages of large size and generalizability to community samples, a longitudinal design, well-characterized clinical and psychosocial functioning, and oversampling of families with maternal depression. Also, all youth are the same ages at the times of study (ages 15 and 20).
Methods
Participants
Participants were 20-year old youth (343 M, 363 F) retained from 816 families previously studied at 15 years of age. The original 816 families were a subset drawn from the Mater-University Study of Pregnancy (MUSP) in Brisbane, Australia (Keeping et al. 1989). The MUSP study originally followed a birth cohort of over 7,000 women during pregnancy and after birth, at 6 months, and 5 years to study health and development. When the children were 15, the present investigators selected families to represent mothers with diverse experiences in severity and chronicity of depressive symptoms (including no or minimal depression) over the child’s early life. Selection was based on scores on administrations of a depression questionnaire given to mothers during pregnancy and three additional times in the first 5 years of the child’s life. Following sample selection, actual diagnostic information was collected as described below. Further details are reported in Hammen and Brennan (2001).
Of the original 816 youth, 706 (87%) were retained in the age 20 follow-up (2 were deceased, 51 refused, and 52 could not be located or scheduled; 5 participants did not complete diagnostic interviews). Those who were included were marginally more likely to have depressed mothers, χ 2 (1, n = 816) = 3.56, p = 0.059. Males were less likely to participate in the follow-up than females, χ 2 (1, n = 816) = 12.63, p = 0.006. Participants did not differ from nonparticipants on their own prior depression status, χ 2 (df = 1, n = 816) = 1.32, p = 0.25, or on any prior diagnosis. Nonparticipants also came from families with lower income, t(783) = 2.11, p < 0.05.
The current study reports on 699 of the 706 retained; 7 are not included in the current analyses because 1 withdrew, 3 were excluded due to maternal bipolar disorders, and 3 youth were excluded because they did not fit the grouping criteria for natural course of depression because they had first onset dysthymic disorder after age 15 but no major depressive disorders.
Procedures
At age 15 the youths and mothers (and fathers if available) were interviewed individually and privately at home, and also completed questionnaires. For the follow-up, the youths were contacted in their 20th year of age, and were interviewed at home or in a convenient location and completed a questionnaire packet. Parental informed consent and youth assent were obtained when the youth was 15, and informed consent was obtained from the youth at age 20. All procedures were reviewed and approved by institutional review boards at UCLA, Emory University, and the University of Queensland. Participants were paid for their time. Interviewers were clinically trained postgraduate students in psychology, trained to proficiency and reliability on all interview procedures. Interviewers in both the age 15 study and the age 20 follow-up were blind to maternal diagnostic status (and in the follow-up, blind to youth prior diagnostic status).
Measures
Maternal diagnostic evaluation
Lifetime and current diagnostic interviews were conducted when the youth was 15, using the Structured Clinical Interview for DSM-IV (SCID; First et al. 1995), which yielded weighted Kappas of 0.87 for current depression diagnoses and 0.84 for past, based on independent judges’ ratings of audiotaped interviews. Mothers were again interviewed with the SCID at youth age 20, covering the prior 5 years. Of the 699 youth retained in the follow-up, 313 mothers had had a diagnosable depression by youth age 15 (dysthymia, major depression, or both), and 386 were never depressed.
Youth diagnostic evaluation
At the age 15 interview, the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Revised for DSM IV (K-SADS-E; Orvaschel 1995) was administered separately to the mother and child, with best-estimate diagnostic decisions for past and current disorders made by the clinical rating team using all available information. Weighted Kappas were 0.82 for current depressive disorders and 0.73 for past, based on independent judges’ ratings of taped interviews. Youth classified in the present study as having depressive disorders at age 15 included those with DSM major depressive disorder or dysthymic disorder or both. At the age 20 interview, diagnoses of major depressive episodes were based on the SCID for DSM IV administered to the youth, covering the period of the past 5 years since the age 15 interview. Independent judges’ ratings of taped interviews yielded significant Kappas for current (0.83) and past 5 years (0.89).
Youth interpersonal functioning at age 15
A semi-structured interview for adolescents was developed from earlier versions of chronic strain/functioning for children and adults (e.g., UCLA Stress Interview; Hammen et al. 1987; Hammen and Brennan 2001). It assesses ongoing conditions, attempting to capture relatively stable features of the person’s life. Probes ask about typical circumstances in the past 6 months. The adolescent version used in the present study at age 15 included four domains relevant to interpersonal functioning: social life, close friendship, romantic relationships (or dating interest), and relations with family members. Each domain was scored by the interviewer on a five-point scale with behaviorally specific anchors such that “1” represented superior functioning and circumstances, and 5 represented severely adverse conditions. For example, regarding close friendship, a score of 1 represents exceptionally close, stable, long-term relationship with no chronic stress; 2 indicates low chronic stress: presence of a good quality, close, confiding friendship, mutual disclosure and support, trustworthy and stable, whereas 4 represents moderate chronic stress: presence of someone the person considers best friend but poor quality—unstable, doubt trustworthiness, or only a moderately close friendship that is somewhat unstable or conflictual. Scores of 1 were rare but represented markedly positive features; scores could be scored at 0.5 increments. In order to capture a range of interpersonal performance, the mean of the four interpersonal functioning scales was computed, with higher scores representing worse conditions. Interrater reliabilities yielded an average intraclass correlation of 0.70 across the four social domains.
Validity is supported for individual domains by comparing interviewer ratings of the youth with independently-obtained information from other sources. For instance, independent interview-based mother-reported relations with the child obtained at the same point in time correlated significantly with the interviewer ratings of child’s relationship with the parents [r(698) = 0.41, p < 0.001]; teacher-reported ratings of youth peer popularity and social functioning at school correlated significantly with social, romantic, and close friend interviewer reports (all p-values < 0.01). Participants’ homeroom teachers had been asked to complete the Teacher Report Form (Achenbach 1991) and supplementary questionnaires on youth’s level of peer rejection and popularity. This measure was developed and reported by Rudolph et al. (1994, 1997). Rejection was rated on a scale of 1 (not at all rejected) to 5 (to a large degree rejected). Popularity was rated on a scale of 1 (extremely popular) to 5 (not at all popular). For example, teacher ratings of youth popularity and perceived rejection were correlated with interview-based ratings of youth social life, r(515) = −0.23 and r(510) = 0.24, p < 0.001, respectively. Maternal ratings of the youth’s age 15 social functioning on the social problems scale of the CBCL correlated significantly with the composite interview chronic social stress ratings [r(683) = 0.32, p < 0.0001]. The correlations are moderate due to method variance across different instruments and use of measures of overlapping but different constructs; nevertheless, all are significant and indicate agreement over different informants.
Results
The analyses first describe four groups of depression outcome patterns during adolescence in terms of maternal depression and early interpersonal functioning, as well as gender. Next we tested the hypothesized predictors of depression occurring during late adolescence, and explored whether maternal depression’s effect on youth depression in late adolescence is mediated by youth early onset depression and early interpersonal adjustment.
Description of Depression Outcomes Between Ages 15–20
Table 1 presents descriptive information on groups defined by major depression patterns. Youth were classified as early-onset recurrent (n = 50) in Table 1 if they had had a diagnosis of major depression and/or dysthymia and also had a new episode of MDE between 15 and 20 (14% also had dysthymic disorder in addition to a major depressive episode after 15). Four of the 50 youth had experienced more than one episode prior to 15. The early-onset nonrecurrent group (n = 49) had experienced major depression and/or dysthymia by age 15 and had no further MDE diagnoses after 15. The later onset group (n = 131) experienced first onset of MDE after age 15; 29 of this group had more than one MDE during the period 15–20. The never-depressed group (n = 469) had no lifetime diagnoses of MDE or dysthymia.
For brevity, the four groups were termed Early-recurrent, Desisting, Later-onset, and Never depressed, and they were compared on gender, maternal depression status to youth age 15, and interpersonal functioning at age 15. In a logistic regression model, gender was significantly predicted by group membership, χ 2(3) = 29.00, p < 0.0001, with percentages of women at 74%, 67%, 61%, and 45% for Early-recurrent, Desisting, Later-onset, and Never depressed respectively, as shown in Table 1. Chi-square comparisons indicated there were no significant differences between the Early-recurrent group and each of the other groups on proportions of females, with the exception that in the Never depressed group compared to the Early-recurrent group the odds of being male were higher, OR = 3.51 (CI 1.82–6.78), p < 0.001. Similar comparisons on maternal depression status indicated an overall significantly different distribution among groups, χ 2(3) = 13.03, p < 0.005. Contrasts indicated no difference in rates of maternal depression between the Early Recurrent and the Desisting groups, but significantly less likelihood of maternal depression in the Later-onset (OR = 0.48, CI 0.24–0.93) and Never depressed (OR = 0.39; CI 0.22–0.72) as compared to the Early-recurrent group. Further, omitting those already depressed by age 15, comparisons indicated that the offspring of depressed women are not more likely to become depressed by age 20 than offspring of nondepressed women, χ 2(1) = 1.12, n.s.
Planned contrasts between groups on the mean interpersonal functioning variable assessed at age 15 were used to compare the Early-recurrent group with each other group. As shown in Table 1, as hypothesized, the Early-recurrent group had significantly worse interpersonal functioning than each of the other groups, with t-values for the planned comparisons all >3.97 (df = 694), ps < 0.0001.Footnote 1
Mediation of the Effects of Maternal Depression on Depression Status Between Ages 15 and 20
First, a logistic regression was conducted in order to establish a direct effect of maternal depression on the likelihood of offspring experiencing a major depressive episode between ages 15 and 20. Controlling for gender, maternal depression status was a significant predictor of MDE occurring between ages 15 and 20, OR = 1.41 (CI 1.00–1.99), p = 0.05. There was no evidence of an interaction between maternal depression and youth gender (p = 0.67).
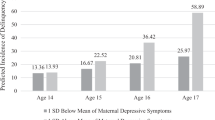
In order to test the hypothesis that depression and social functioning by age 15 would mediate this direct effect of maternal depression on youth depression between ages 15 and 20, a path analysis was conducted using M-Plus statistical software (Muthén and Muthén 1998). Path analysis allowed for simultaneous analysis of the two hypothesized indirect pathways between maternal depression and youth MDE between 15 and 20, thereby eliminating the need for separate mediation regression analyses (Baron and Kenny 1986). Use of M-Plus software for the data analysis allowed for the use of dichotomous mediator variables, namely the presence or absence of youth depression by age 15. For ease of interpretation and comparison to the effects of early onset depression, the interpersonal functioning variable was converted to a dichotomous variable by median split. The mediating pathways tested are depicted in Fig. 1. Weighted least-squares parameter estimates (WLSMV) were used to accommodate the non-normality of the binary variables in the model, yielding probit regression coefficients for each regression relation (Muthén and Muthén 1998).
Results of path analysis showing mediation of the association between maternal depression and youth depressive episodes between ages 15 and 20 by youth history of depression by age 15 and youth interpersonal functioning at age 15, controlling for youth gender. Values given are probit coefficients (and standard errors). Significant pathways are signified by solid lines; non-significant pathways are signified by dotted line
In the initial analysis, we controlled for the effects of gender by directly regressing youth MDE between 15 and 20 onto gender and tested the mediating effects of the two hypothesized indirect pathways. The unstandardized probit coefficients shown in Fig. 1 represent the difference that one unit change in the predictor variable makes in the cumulative normal probability of the direct outcome variable. Overall, the results of the comparisons between the direct and indirect paths suggested that the effect of maternal depression on youth depression in late adolescence was completely mediated by the indirect pathways. While the indirect paths through youth depression (probit coefficient = 0.17, SE = 0.06, p = 0.003) and social functioning (probit coefficient = 0.09, SE = 0.03, p = 0.007) were significant, the direct path from maternal depression to youth depression between 15 and 20 was not significant (probit coefficient = −0.05, SE = 0.12, p = 0.65). A probit coefficient of −0.05 indicated that a one-unit increase in maternal depression (from not depressed to depressed) resulted in a decrease of 0.05 standard deviations in the predicted Z score of cumulative normal probability distribution of youth depression between 15 and 20, a nonsignificant level of change.
In order to further explore the potential impact of gender on these results, separate path analyses were conducted for men and women. The results suggested that while maternal depression was fully mediated for each gender, the specific paths took on differential importance for males and females. For men, the indirect path through chronic social functioning was nonsignificant (probit coefficient = 0.05, SE = 0.07 p = 0.26) while the path through youth depression prior to age 15 was significant (probit coefficient = 0.32, SE = 0.13, p = 0.01). For women, the opposite pattern emerged such that the path through prior youth depression was nonsignificant (probit coefficient = 0.09, SE = 0.06.p = 0.11) while the path through social functioning was significant (probit coefficient = 0.11, SE = 0.05, p = 0.04). These gender differences must be interpreted cautiously given the loss of power associated with dividing the sample by gender. Nonetheless, the probit coefficients paired with the significance data suggest that these two mediating pathways may have differing amounts of importance in explaining youth depression in late adolescence for men and women. In both analyses, the direct pathway from maternal depression to youth depression between 15 and 20 was nonsignificant (all ps > 0.60), suggesting full mediation in both.
Discussion
The study attempted to characterize depression patterns in youth as a way to bring greater clarity to the heterogeneous phenomenon of “adolescent depression.” Patterns were selected based on the combination of depression status at two time points, by age 15 and age 20, and these outcomes were described in relation to three key variables predictive of adolescent depression: maternal depression, youth interpersonal functioning in early adolescence, and gender. Specifically, in keeping with an interpersonal, intergenerational approach to youth depression (Hammen et al. 2004) we tested whether the associations between maternal depression and youth major depression after age 15 are mediated by early onset depression and interpersonal maladjustment, and whether the mediation patterns differ for females and males.
Four investigator-defined patterns of major depression by age 20 were characterized. Half of the 99 youth who had diagnoses of depression by age 15 went on to have recurrent MDE (50) and the other half had no further depressive disorders (49). Of the 600 youth who had no depression by 15, 131 had first onset of MDE after 15, and the rest were never depressed (469). Women were over-represented in all of the depression groups (with young men having higher rates than women for “never depressed”). The early onset-recurrent group had significantly poorer interpersonal adjustment at age 15 than each of the other three groups. Also, the early-onset recurrent group was significantly more likely than the later-onset and never-depressed groups to have depressed mothers (but did not differ from the early-onset desisting group). These findings are consistent with the cross sectional findings of Hammen and Brennan (2001) that depressed children of depressed mothers have worse social impairments than the equally depressed children of nondepressed mothers. Results are also consistent with the prediction from the Hammen and Brennan study that, when followed up 5 years later, the interpersonally less well functioning offspring of depressed mothers would have greater likelihood of depression recurrence compared to children of nondepressed women.
The mediation analyses supported the hypothesis that the detrimental effects of maternal depression on youth depression are accounted for by youth early onset depression and interpersonal dysfunction. Overall effects controlling for gender were elaborated by testing the path models separately for sons and daughters. In both models the effect of maternal depression on youth later adolescent depression was fully mediated, but the genders showed different patterns. The indirect effect of early onset depression but not interpersonal problems predicted depression in males, and the reverse pattern was true for females. These path analyses, along with the earlier descriptive analyses of groups, indicate that maternal depression has its ill effects by youth age 15. For girls in particular, maternal depression has its effects on early interpersonal dysfunction predicting later depression, while for boys maternal depression has its effects on early onset depression predicting later depression.
The findings supplement those of follow-up studies of adolescent depression by Bardone et al. (1996); Dunn and Goodyer (2006); Fleming et al. (1993); Harrington et al. (1990); Lewinsohn et al. (1999, 2000); Pine et al. (1998); Rao et al. (1999) and Weissman et al. (1999), who have shown that many but not all of adolescents with major depression experience recurrence in the ensuing few years. The current results shed further light on correlates of the recurrences, and confirm the critical role of interpersonal dysfunction as a risk factor for youth depression (e.g., Hammen et al. 2004; Rudolph et al. 2007)—perhaps especially for adolescent young women. Results are consistent with findings from other studies that indicate girls’ greater depressive reactions to relationship difficulties, greater relationship stress, and importance attached to interpersonal relationships (e.g., Hankin et al. 2007; Rudolph 2002; Shih et al. 2006).
Social difficulties may be an important indicator of risk for future and persistent problems of depression among depressed youth to the extent that they may contribute to stressful family, romantic, and social circumstances that themselves trigger depressive reactions. Moreover, poor functioning in social roles may reduce social support for dealing with negative events and depressive reactions and erode self-esteem, which may exacerbate vulnerability to depression. For all these reasons, we speculate that interpersonal difficulties play a functional role in future depression experiences, especially for females. At the present time the source of poor interpersonal functioning is not known. However, models of the intergenerational transmission of depression have consistently documented dysfunctional parent–child relationships and children’s exposure to a variety of family and marital disturbances, which may predict maladaptive social problem-solving, dysfunctional cognitions about relationships, and insecure attachment bonds (e.g., reviewed in Goodman and Gotlib 1999). Also, of course, genetic pathways may additionally underlie both biological and personality factors that contribute to interpersonal difficulties and stressors.
The results are also consistent with longitudinal studies of offspring of depressed parents that have shown associations of parental depression with recurrent youth depression (e.g., Lieb et al. 2002; Rohde et al. 2005; Weissman et al. 1997). Those studies did not test for mediational effects, however, and the current study is the first to suggest that maternal depression did not have strong direct effects on depression occurring later in adolescence. The present study suggests that the effect of maternal depression may be largely apparent by age 15. In the present sample, if a child was not depressed by that age, the offspring of depressed women were no more likely to become depressed by age 20 than offspring of nondepressed women. In view of the varying patterns for adolescent men and women, the results also are a reminder that gender differences in youth depression affect not only rates of disorder but also its predictors (e.g., Nolen-Hoeksema and Girgus 1994).
While the current study does not go beyond age 20, we might speculate that this subgroup of youth with both early-onset depression and adolescent recurrence may constitute a “life course persistent” (Moffitt 1993) form of the disorder, potentially identifying youth at greatest need for early intervention. Others have hypothesized that early-onset and recurrent depression is associated with worse course and might constitute a subtype of depression marked by greater genetic predisposition (e.g., Bland et al. 1986; Marazita et al. 1997; Weissman et al. 1997). However, most such work has been based on retrospective studies of adults, and uses a wide range of definitions of “early onset.” Further study is needed to learn the outcomes of those who had early onset depression but no further recurrence by age 20. Jaffee et al. (2002) found that their “juvenile-only” depressed youth who did not show later depression included those with high rates of externalizing disorders, suggesting that even if there was no further depression, their adult histories may nonetheless reflect maladjustment (see also Weissman et al. 1997). In further analyses of the clinical features and functional adjustment of the groups of youth described in the present study, those with no further depression after early onset had good overall adjustment in most roles (Hammen 2008). It is also noteworthy that a good many youth developed a first onset of major depression between the ages of 15 and 20. However, this later onset group was not characterized by elevated rates of maternal depression or interpersonal dysfunction. The outcomes of this group over time will be of interest, particularly in comparison with those who had early-onset recurrent depression.
While the analyses provide a picture of the predictive importance of several variables (gender, early-onset depression, interpersonal dysfunction, and maternal depression), it is acknowledged that it is not a model of prediction of youth depression. Such a model would include a variety of factors that were not included in the present article, such as features of maternal depression, stress, family functioning, and related variables and the transactions among them, which we hope to pursue in a separate paper. Obviously, fuller explication of the complex mechanisms leading to early-onset recurrent depression is needed in future work, including integration of biological-genetic, environmental, and personal factors.
It is emphasized that the four groups described in the current study were rationally derived, and do not address the same issues of the empirically derived number, shape, and gender differences in statistical trajectory analyses of depressive symptoms that have been presented in the literature (e.g., Dekker et al. 2007; Stoolmiller et al. 2005). Similarly, the proportions of youth in each diagnosis outcome group are not directly comparable to proportions reported in other longitudinal studies derived from clinical samples, nor to community samples because of the over-representation of youth at risk due to maternal depression.
In addition to gaps in our understanding of the mechanisms, several limitations of the methodology of the study are acknowledged. Because the initial study occurred when youth were age 15, this age was used as the benchmark for “early-onset.” It is possible that a sample that had numerous childhood-onset, rather than adolescent-onset, cases, would have yielded different results. Use of age 15 to mark early onset is somewhat arbitrary, but is consistent with work by Silberg et al. (2001), who suggested that depressions occurring before and after age 14 may be etiologically distinct syndromes, at least in females. It is also acknowledged that diagnoses at age 20 were based on participants’ recall of experiences over the past 5 years, and such a lengthy period may have reduced accurate recall of the occurrence and timing of depressive episodes.
It could be argued that social dysfunction at age 15 may largely reflect impairment due to depressive disorder, suggesting that it is simply worse depression that predicts recurrence. It is likely true that some of the dysfunction reflects symptomatology, but our measure of interpersonal functioning assessed relatively stable circumstances including those covering periods when the youth was not in an episode, and corresponded to teacher and mother reports of various indicators of social functioning. Moreover, exploratory analyses in which youth with current diagnoses of major depression at the time of interpersonal functioning assessments were removed—a conservative test of hypotheses—did not change the results reported. Research on interpersonal functioning in depression generally suggests that social impairments persist even when the person is not currently in an episode (e.g., Hammen and Brennan 2002). Many questions about the nature of specific types of interpersonal maladjustment remain and need to be addressed with a variety of well-validated measures of social behavior.
Maternal depression was defined as diagnoses occurring by the time the youth was 15, on the assumption that later first onsets of maternal depression might have less of an effect owing to less exposure due to emotional and perhaps physical independence of youth. However, exploratory analyses were conducted that included maternal depression occurring at any point by youth age 20, and the results were unchanged. Further studies of the timing, severity, and chronicity of maternal depression on youth outcomes by age 20 will be pursued, along with further efforts to understand the mechanisms of the link between maternal and youth depression.
The study was based on a birth cohort of a particular period in Queensland, Australia. Accordingly, generalization to cohorts born in different decades—or to US samples—may be questioned. However, the cultures of Australia and the US are highly similar, and there is no clear reason to expect that the maternal depression variables would operate differently in Australia than elsewhere. The high risk sample was selected based on depressed mothers. Elsewhere we and others (Brennan et al. 2002; Klein et al. 2005; Marmorstein et al. 2004) have evaluated the role of depressed fathers on offspring outcome, but specific contributions of fathers’ depression to adolescent depression recurrence need to be explored.
The results of the present study suggest guidelines for enhancing prevention and treatment efforts aimed at adolescent depression. The results imply that children who have onset of depression in the early teens, accompanied by chronic difficulties in their social relationships, especially girls, are at particular risk for recurrent depression. Children of depressed mothers may be especially at risk for early-onset depression with social maladjustment. These youth may benefit from treatment of both their social impairments and depressive disorders, with the goal of reducing recurrence during the transition to adulthood.
Notes
Within the first onset group some individuals had more than one major depressive episode during the period 15–20 years of age. To clarify the effects of early onset-recurrence vs. later onset-recurrence, a planned comparison between the groups indicated that the early-onset recurrent MDE group had significantly worse social functioning (M = 2.55, SD = 0.35) compared to those with more than one episode in the later onset group (M = 2.25, SD = 0.26), t(693) = 4.44, p < 0.0001. Thus, onset after age 15, even if associated with more than one major depressive episode by age 20, was not associated with earlier interpersonal impairment.
References
Achenbach, T. (1991). Integrative guide to the 1991 CBCL, YSR, and TRF. Burlington: University of Vermont, Department of Psychiatry.
Arnett, J. J. (1999). Adolescent storm and stress, reconsidered. American Psychologist, 54, 317–326.
Bardone, A., Moffitt, T., Caspi, A., Dickson, N., & Silva, P. (1996). Adult mental health and social outcomes of adolescent girls with depression and conduct disorder. Development and Psychopathology, 8, 811–829.
Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182.
Beardslee, W. R., Versage, E. M., & Gladstone, T. R. (1998). Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 1134–1141.
Birmaher, B., Williamson, D. E., Dahl, R. E., Axelson, D. A., Kaufman, J., Dorn, L. D., et al. (2004). Clinical presentation and course of depression in youth: Does onset in childhood differ from onset in adolescence? Journal of the American Academy of Child and Adolescent Psychiatry, 43, 63–70.
Bland, R. C., Newman, S. C., & Orn, H. (1986). Recurrent and nonrecurrent depression: A family study. Archives of General Psychiatry, 43(11), 1085–1089.
Brennan, P., Hammen, C., Katz, A., & LeBrocque, R. (2002). Maternal depression, paternal psychopathology, and adolescent diagnostic outcomes. Journal of Consulting and Clinical Psychology, 70, 1075–1085.
Costello, E. J., Mustillo, S., Erklani, A., Keeler, G., & Angold, A. (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60, 837–844.
Daley, S. E., Hammen, C., & Rao, U. (2000). Predictors of first onset and recurrence of major depression in young women during the 5 years following high school graduation. Journal of Abnormal Psychology, 109, 525–533.
Dekker, M., Ferdinand, R., van Lang, N., Bongers, I., van der Ende, J., & Verhulst, F. (2007). Developmental trajectories of depressive symptoms form early childhood to later adolescence. Gender differences and adult outcomes. Journal of Child Psychology and Psychiatry, 48, 657–666.
Dunn, V., & Goodyer, I. (2006). Longitudinal investigation into childhood- and adolescence-onset depression: Psychiatric outcome in early adulthood. British Journal of Psychiatry, 188, 216–222.
Essau, C. A. (2004). The association between family factors and depressive disorders in adolescents. Journal of Youth and Adolescence, 33, 365–372.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1995). Structured clinical interview for DSM-IV Axis I disorders. Washington: American Psychiatric Press.
Fleming, J. E., Boyle, M. H., & Offord, D. R. (1993). The outcome of adolescent depression in the ontario child health study follow-up. Journal of the American Academy of Child and Adolescent Psychiatry, 32, 28–33.
Goodman, S., & Gotlib, I. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490.
Hammen, C. (2008). Stress exposure and stress generation in adolescent depression. In S. Nolen-Hoeksema & L. Hilt (Eds.), Handbook of adolescent depression. New Jersey: Lawrence Erlbaum Associates (in press).
Hammen, C., Adrian, C., Gordon, D., Burge, D., Jaenicke, C., & Hiroto, D. (1987). Children of depressed mothers: Maternal strain and symptom predictors of dysfunction. Journal of Abnormal Psychology, 96, 190–198.
Hammen, C., & Brennan, P. (2001). Depressed adolescents of depressed and nondepressed mothers: Tests of an interpersonal impairment hypothesis. Journal of Consulting and Clinical Psychology, 69, 284–294.
Hammen, C., & Brennan, C. (2002). Interpersonal dysfunction in depressed women: Impairments independent of depressive symptoms. Journal of Affective Disorders, 72, 145–156.
Hammen, C., Brennan, P., Keenan-Miller, D., & Herr, N. (2008). Early onset recurrent subtype of adolescent depression: Clinical and psychosocial correlates. Journal of Child Psychology and Psychiatry, 49(4), 433–440.
Hammen, C., Shih, J., & Brennan, P. (2004). Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology, 72, 511–522.
Hankin, B. L., Abramson, L. Y., Moffitt, T. E., Silva, P. A., McGee, R., & Angell, K. E. (1998). Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology, 107, 128–140.
Hankin, B. L., Mermelstein, R., & Roesch, L. (2007). Sex differences in adolescent depression: Stress exposure and reactivity models in interpersonal and achievement contextual domains. Child Development, 78, 279–295.
Harrington, R., Fudge, H., Rutter, M., Pickles, A., & Hill, J. (1990). Adult outcomes of childhood and adolescent depression: Psychiatric status. Archives of General Psychiatry, 47, 465–473.
Harrington, R., Rutter, M., & Fombonne, E. (1996). Developmental pathways in depression: Multiple meanings, antecedents, and endpoints. Development and Psychopathology, 8, 601–616.
Jaffee, S. R., Moffitt, T. E., Caspi, A., Fombonne, E., Poulton, R., & Martin, J. (2002). Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of General Psychiatry, 59, 215–222.
Keeping, J. D., Najman, J. M., Morrison, J., Western, J. S., Andersen, M. J., & Williams, G. M. (1989). A prospective longitudinal study of social, psychological, and obstetrical factors in pregnancy: Response rates and demographic characteristics of the 8,556 respondents. British Journal of Obstetrics and Gynecology, 96, 289–297.
Kessler, R. C., & Walters, E. E. (1998). Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depression and Anxiety, 7, 3–14.
Klein, D., Lewinsohn, P., Rohde, P., Seeley, J., & Olino, T. (2005). Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychological Medicine, 35, 353–365.
Kovacs, M. (2001). Gender and the course of major depressive disorder through adolescence in clinically referred youngsters. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1079–1085.
Lakdawalla, Z., Hankin, B. L., & Mermelstein, R. (2007). Cognitive theories of depression in children and adolescents: A conceptual and quantitative review. Clinical Child and Family Psychology Review, 10, 1–24.
Lewinsohn, P. M., Hops, H., Roberts, R. E., Seeley, J. R., & Andrews, J. A. (1993). Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology, 102, 133–144.
Lewinsohn, P. M., Rohde, P., Klein, D. N., & Seeley, J. R. (1999). Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 56–63.
Lewinsohn, P. M., Rohde, P., & Seeley, J. R. (1998). Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review, 18, 765–794.
Lewinsohn, P. M., Rohde, P., Seeley, J. R., Klein, D. N., & Gotlib, I. H. (2000). Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. American Journal of Psychiatry, 157, 1584–1591.
Lieb, R., Isensee, B., Hofler, M., & Wittchen, H.-U. (2002). Parental depression and depression in offspring: Evidence for familial characteristics and subtypes? Journal of Psychiatric Research, 36, 237–246.
Lovejoy, C. M., Graczyk, P. A., O’Hare, E., & Neuman, G. (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20, 561–592.
Marazita, M. L., Neiswanger, K., Cooper, M., Zubenko, G., Giles, D. E., Frank, E., et al. (1997). Genetic segregation analysis of early-onset recurrent unipolar depression. American Journal of Human Genetics, 61, 1370–1378.
Marmorstein, N., Malone, S., & Iacono, W. (2004). Psychiatric disorders among offspring of depressed mothers: Associations with paternal psychopathology. American Journal of Psychiatry, 161, 1588–1594.
Moffitt, T. E. (1993). Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychological Review, 4, 674–701.
Muthén, L. K., & Muthén, B. O. (1998). Mplus User’s Guide. Los Angeles: Muthén & Muthén.
Nolen-Hoeksema, S. N., & Girgus, J. S. (1994). The emergence of gender differences in depression during adolescence. Psychological Bulletin, 115, 424–443.
Orvaschel, H. (1995). Schedule for affective disorder and schizophrenia for school-age children- epidemiologic version-5. Ft. Lauderdale: Center for Psychological Studies, Nova Southeastern University.
Pine, D. S., Cohen, P., Gurley, D., Brook, J. S., & Ma, Y. (1998). The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry, 55, 56–64.
Rao, U. (2006). Development and natural history of pediatric depression: Treatment implications. Clinical Neuropsychiatry, 3, 194–204.
Rao, U., Hammen, C., & Daley, S. (1999). Continuity of depression during the transition to adulthood: A 5-year longitudinal study of young women. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 908–915.
Rohde, P. L., Lewinsohn, P. M., Klein, D. N., & Seeley, J. R. (2005). Association of parental depression with psychiatric course from adolescence to young adulthood among formerly depressed individuals. Journal of Abnormal Psychology, 114, 409–420.
Rudolph, K. D. (2002). Gender differences in emotional responses to interpersonal stress during adolescence. Journal of Adolescent Health, 30, 3–13.
Rudolph, K. D., Flynn, M., & Abaied, J. L. (2007). A developmental perspective on interpersonal theories of youth depression. To appear in J. R. Z. Abela & B. L. Hankin (Eds.), Child and adolescent depression: Causes, treatment, and prevention (pp. 79–102). New York: Guilford.
Rudolph, K., Hammen, C., & Burge, D. (1994). Interpersonal functioning and depressive symptoms in childhood: Addressing the issues of specificity and comorbidity. Journal of Abnormal Child Psychology, 22, 355–371.
Rudolph, K., Hammen, C., & Burge, D. (1997). A cognitive-interpersonal approach to depressive symptoms in preadolescent children. Journal of Abnormal Child Psychology, 25, 33–45.
Rudolph, K., Hammen, C., & Daley, S. (2006). Adolescent mood disorders. In E. J. Mash, & D. A. Wolfe (Eds.), Behavioral and Emotional Disorders in Adolescence (pp. 300–342). New York: Guilford.
Rutter, M., Kim-Cohen, J., & Maughan, B. (2006). Continuities and discontinuities in psychopathology between childhood and adult life. Journal of Child Psychology and Psychiatry, 47, 276–295.
Shih, J. H., Eberhart, N. K., Hammen, C. L., & Brennan, P. A. (2006). Differential exposure and reactivity to interpersonal stress predict sex differences in adolescent depression. Journal of Clinical Child and Adolescent Psychology, 35, 103–115.
Silberg, J. L., Rutter, M., & Eaves, L. (2001). Genetic and environmental influences on the temporal association between earlier anxiety and later depression in girls. Biological Psychiatry, 49, 1040–1049.
Stoolmiller, M., Kim, H. K., & Capaldi, M. (2005). The course of depressive symptoms in men from early adolescence to young adulthood: Identifying latent trajectories and early predictors. Journal of Abnormal Psychology, 114, 331–345.
Weissman, M. M., Warner, V., Wickramaratne, P., Moreau, D., & Olfson, M. (1997). Offspring of depressed parents: 10 years later. Archives of General Psychiatry, 54, 932–940.
Weissman, M. M., Warner, V., Wickramaratne, P., Nomura, Y., Warner, V., Pilowsky, D., & Verdeli, H. (2006). Offspring of depressed parents: 20 years later. American Journal of Psychiatry, 163, 1001–1008.
Weissman, M. M., Wolk, S., Goldstein, R. B., Moreau, D., Adams, P., Greenwald, S., et al. (1999). Depressed adolescents grown up. Journal of the American Medical Association, 281, 1707–1713.
Acknowledgement
This research was supported by NIMH R01MH52239. We are grateful to the MUSP, M900, and M20 Research Teams, and to the parents and youth in the Mater Cohort for their participation in this study. Particular thanks to project coordinators Robyne LeBrocque, Cheri Dalton Comber, and Sascha Hardwicke. The cooperation of Professor Jake Najman of the University of Queensland and head of the MUSP program is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hammen, C., Brennan, P.A. & Keenan-Miller, D. Patterns of Adolescent Depression to Age 20: The Role of Maternal Depression and Youth Interpersonal Dysfunction. J Abnorm Child Psychol 36, 1189–1198 (2008). https://doi.org/10.1007/s10802-008-9241-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-008-9241-9