Abstract
One major challenge to successful aging is the capability to preserve health, or from another perspective to avoid disease. Unfortunately, a large percentage of the elderly people are living with chronic diseases or disabilities. Home care technologies and other emerging technologies have the potential to play a major role in home-based health care approach. The advent of sensor technology, in addition to telecom industry has made this possible. The main goal of the presented research in this paper is to develop a cost-effective user-friendly telehealth system to serve the elderly and disabled people in the community. The research also aims at utilizing the state-of-the-art advances in medical instrumentation technology to establish a continuous communication link between patients and caregivers and allow physicians to offer help when needed. Hence, we are presenting here an integrated user-friendly model of a smart home which provides telemedicine for elderly at home. The general problem addressed in this paper is that of offering a smart environment which monitors the elderly continuously as he moves around at home, and sends an emergency call for help in case of an occurrence of an accident or a severe health problem. The paper focuses on implementation details and practical considerations of integrating the diverse technologies into a working system.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Recently, with the enormous performance improvement and cost drop in embedded systems, we are seeing an explosive growth in the number of internet enabled appliances and mobile devices, including smart phones, wireless PDAs and various internets enabled multimedia devices. Lately, a related technology, ubiquitous or pervasive computing, is exploring ways to make computers disappear or to install smart devices which function without the intervention of the user. Examples of those are smart offices, smart homes and others. Ubiquitous systems may not necessarily be mobile, they ma be fixed in a house or office. They are designed to be “everywhere”. A user may not be aware of the existence of a hundred sensors inside the wall or under the floor, to adjust the light level and the room temperature, and monitor the home safety. Intelligent appliances in a networked home allow the access to a variety of controls from a remote internet browser. For example, Tini web servers in the size of a matchbox could be applied to manage the state of an air conditioning system. Telephones, light switches, refrigerators, and washing machines will be part of a resident network (Crilly et al. 1997; Deni et al. 2005).
In the pervasive computing world, people need to be able to identify or authenticate themselves to computer systems. For payment, tracking, and security applications, computer systems need to be able to identify products, packages, and objects in general. As it turned out, a special breed of computer chips has been developed to fulfill identification and authentication requirements such as these. These chips can be embedded within plastic cards, paper labels, key ring fobs, and many other forms. In the last decade, smart cards or chip cards, evolved from basic memory cards to complex systems on chips with expanding processing power. This has opened the avenue to many applications such as financial transactions, e-commerce, physical access control, health, and transportation services (Dhem and Feyt 2001).
Further more; there has been increasing interest recently in wearable/mobile health monitoring devices, both in research and industry. These devices are particularly important to the world’s increasingly aging population, whose health has to be assessed regularly or monitored continuously. For example, a third or more of the 78 million baby boomers and 34 million of their parents may be at risk for the development of devastating diseases including cardiovascular disease, stroke and cancer. Chronic diseases are becoming the world’s leading causes of death and disability, and will account for almost three-forth of all deaths by 2020. Each year, number of deaths caused by cardiovascular diseases and hypertension is estimated to be 16.7 million and 7.1 million, respectively. Population of diabetic adults is expected to reach 300 million by 2025 (Dresher and Mendelson 2006).
The implications of these wearable health monitoring technologies are paramount, since they could: (1) enable the detection of early signs of health deterioration; (2) notify health care providers in critical situations; (3) find correlations between lifestyle and health; (4) bring healthcare to remote locations and developing countries, and transform health care by providing doctors with multi-sourced real-time physiological data (Hansmann et al. 2003).
In recent years, there has been a proliferation of consumer health monitoring devices. A good portion of these devices have been developed for the sports. These are sophisticated watches available today that provide real-time heart rate information, and let users store and analyze their data on their home PC (Dhem and Feyt 2001; Dresher and Mendelson 2006). Bodymedia has developed an armband that has multiple sensors (galvanic skin response, skin and near-body temperature, two-axis accelerometer and heat flux) to continuously collect physiological data for a few days at a time. Once the data is downloaded to a PC, their software derives what they call “lifestyle” information, such as energy expenditure, duration of physical activity (Hansmann et al. 2003).
However, in all cases the physiological data is analyzed on a home PC at a later time. Traditionally, personal medical monitoring systems, such as Holter monitors, have been used only to collect data for offline processing. One of the most popular remote health systems perhaps is the AMON system (Hung et al. 2004), a wearable (wrist worn) medical monitoring and alert system targeting high risk cardiac/respiratory patients. The system includes continuous collection and evaluation of multiple vital signs (blood pressure, SpO2, one lead ECG and two-axis accelerometer), multi-parameter medical emergency detection and cellular connection to a medical centre. Use of wearable monitoring devices that allow continuous or intermittent monitoring of physiological signals is critical for the advancement of both the diagnosis as well as treatment of cardiovascular diseases. The usual clinical or hospital monitoring of physiological events such as the electrocardiogram or blood pressure provides only a brief window on the physiology of the patient because they are likely to fail in sampling rare events that may have profound diagnosis, and they cannot monitor the patient during rest or sleep. The capacity to detect physiologic signals in a non-invasive manner greatly facilitates the application of wearable monitoring devices. The continuous measurement of blood pressure serves as one example. Most ambulatory blood pressure monitoring devices rely on the repeated measurement of systolic and diastolic blood pressure at predetermined intervals but do not provide a continuous reading of blood pressure. Although efforts have been made to supply such information by invasive monitoring schemes, they are limited by the potential of untoward events such as arterial damage and infection. Therefore the development of devices that can acquire such information in a non-invasive manner is essential (Hung et al. 2004).
With the advent of advanced telecommunication technology, long-term home care of elderly, or what we call telehealth, is becoming a rapidly growing area of health care industry. The current trend in long-term care is a shift of the delivery system away from institutional care towards home and community-based care.
The health care is seeking to reduce some of the inefficiencies of home health care by using state-of-the-art two way medical monitors, such that health care providers can conduct a check-up on a home care patient’s vital signs such as pulse rates, blood oxygenation and body temperature. This type of technology could be used round-the-clock with patients suffering from chronicle diseases, including patients with congestive heart failure, pulmonary diseases and permanent disability. Hence, Remote health monitoring has the potential to improve the quality of health services delivered and to reduce the total cost in healthcare by avoiding unnecessary hospitalisations and ensuring that those who need urgent care get it sooner. In addition to cost-effective telehealth, remote health monitoring can significantly contribute to the enhancement of disease prevention, early diagnosis, disease management, treatment and home rehabilitation (Polar watches, http://www.suunto.com; T6, foot pod, n6hr, http://www.bodymedia.com).
In a citizen-centred health system, it is very important to have simultaneous access to different kind of health related data such as patient’s health record and accounting data. Also, remote monitoring of personal health status, through vital signs and video/audio signals, with communication link to the health provider and interoperability with existing patient data could significantly improve disease prevention, diagnosis, treatment and rehabilitation. This paper focuses on a novel web-enabled smart home solution for elderly and disabled.
2 Our smart home scenario
In this section, a possible application scenario for smart home for elderly is proposed, assuming a normal apartment owned and inhabited by an elderly person who might be handicapped in various ways, as senses and capabilities to remember are not good. Also his relatives, who might be spread all over the world, would like to make sure he is alright and perhaps keep an eye on him 24/7. The elderly is not able to see a physician anytime he needs, because he is unable to make his way to the clinic or hospital. Therefore, a solution must be developed to allow a patient to talk to his physician in a user-friendly manner. The physician must have a remote-view of the vital signs that physicians look at like oxygen saturation, blood pressure, heart rate, etc. In case of emergency, a reliable emergency system must call a physician and ambulance for help. Since health is a critical issue, the patient’s profile is stored on a secure smart card. Any physician or relative can use his own smart card to access the home, since the elderly is not in a situation to open for visitors.
2.1 Objectives
For an elderly or handicapped person, the main goal is to overcome the limitations in life and to provide successful aging at home. We can list a set of objectives for a smart home for elderly and disabled. These goals constitute the main building blocks for the research. The first objective is developing a monitoring and sensing system that maintains the elderly capacity and keeps an accurate and updated record of his whereabouts at home for his relatives to make sure he is alright, and to report in case he is in trouble. To capture the elderly vital signs continuously and to allow the physician or caregiver to interact with the smart home and to keep the physician up to date. The detailed architecture then should monitor and control certain functions in the home such as entertainment, lights, heat and security and keep a record of these smart home components in order to provide comfort and ease of life for the elderly at home, and initiate emergency call and provide video/audio communication.
The second major goal here is to gather data, both vital medical signs and location, analyze the data locally, and make data accessible. The second goal is an ongoing funded research which will utilize LABVIEW and MATLAB tools for the analysis of the vital signs. These objectives require state-of-the-art technology to be utilized in a user-friendly and unobtrusive manner.
2.2 The proposed system architecture
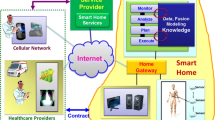
In the following section, a system architecture based on the given objectives is developed. Figure 1 shows an overview of the general layout of the elderly monitoring proposed system using an IP digital camera and the web, in addition to a GSM modem for sending emergency messages or calls to the physician as well as the ambulance. The data base is used to store the information related to the health status of the elderly to be analyzed by a physician or care giver.
The focus in this paper is on an apartment transferred to a smart home. The apartment is equipped with wireless technology as well as sensor technology. The sensors used are divided into two categories. The first category is medical wearable sensors for capturing the vital signs of the elderly to send it upon request to the physician. Two of these sensors included in the proposed design are the pulse oximeter sensor and the blood pressure sensor. These sensors are implanted on a wheel chair, dedicated to help the elderly to move around the smart home. The second category of sensors is the sensors and microcontrollers implanted on surrounding objects in the smart home in a ubiquitous manner. These sensors are used to report the whereabouts of the elderly in the smart home. Example of these sensors is weight sensors and motion detectors, in addition to light sensors. The pervasive smart home should be also context-aware, to allow the elderly to interact comfortably with surrounding objects. For example, if the elderly wakes up at night to fetch something to eat from the kitchen, the lights of the corridor and the kitchen should be switched on, and when he returns to bed the lights should be switched off automatically. See Fig. 2 for the hardware layout of the vital sign sensors. The sensors are connected to a lab top or a PDA on the wheel chair, which sends this data through WIFI to a server for further analysis. There is no doubt that in the context of wearable medical devices, the pulse oximetry represents the greatest advance in wearable patient monitoring in many years, especially for elderly care. It has the unique advantage of continuously monitoring the saturation of haemoglobin with oxygen, easily and no invasively, providing a measure of cardio-respiratory function and extracting breathing rate. By virtue of its ability to quickly detect hypoxemia, it has become the standard of care during anaesthesia as well as in the recovery room and intensive care unit. Pulse oximetry should be used to monitor any patient who is heavily sedated or is likely to become hypoxic (Johnston and Mendelson 2004; Lin et al. 2005; Lopera et al. 2002; Lukowicz et al. 2002; Oliver and Mangas 2005). The blood pressure sensor is off the shelf wearable sensor with USB type interface.
3 Implementations
3.1 Hardware
The main microcontroller used in the developed design is the IP-based Rabbit microcontroller with a built in tiny web server. The Rabbit is chosen due to its small footprint and excellent performance. See Fig. 3 for the proposed layout of the smart home sensors.
Since the focus here is on emergency detection, it is crucial for the smart home for elderly to send alert when water leakage, high temperature or smoke or gas occurs. A wearable fall sensor, which the elderly can wear, will give an alert in case the elderly falls or slips in the bathroom. See Fig. 4 for the proposed layout. For each depicted action of an elderly, we propose a certain scenario of behaviour. The main critical actions required are the frequent times the elderly wakes up at night, in addition to going to the kitchen or bathroom, since in these two places represent source of probable risk for the elderly. In the context of this paper we will only focus on the scenario of the elderly going to the bathroom, and waking up at night. An emergency push button has been added, as shown in Fig. 4 so that the elderly can push it for calling for help by sending an SOS emergency message through the GSM network.
Figure 5 shows an overall proposed model of the smart home for elderly.
If the pressure pad inside the bedroom is activated, it means the elderly is inside the bedroom, and if the pressure sensor of the bed is activated, it implies the elderly wants to sleep.
If 10 minutes or so elapse without any activity, it is assumed the elderly already slept and the smart home will switch the night alarm sensing around the house and monitor any motion in the surroundings. See Fig. 6 for the bedroom scenario.
3.2 Web enabled interface
The web application is done using.net, and the main purpose of it to allow the physician as well as the elderly relatives to view the status of the elderly 24 h. Figure 7 shows a web browser showing real-time status and actions performed by the elderly with time and date log.
Once the vital sign data captured remotely from the elderly is analyzed by a physician, then he can determine whether his case necessities transferring him to the hospital or subscribing a medicine for him. Figure 8 shows a web based medical report generated as a result of the telecare delivered through the proposed smart home model, for monitoring the patient’s blood pressure.
4 Discussion and conclusion
The increased interest in pervasive computing can adapt to a wide spectrum of new small and easy to use technology. The smart objects, medical sensors, actuators represented by control units and other technologies that are made to be proactive for disabled people have become more and more available and affordable. With the rapidly increasing research and development, soon these objects will become as common as mobile phones and PDAs in this time. Concerning health care, it becomes possible to observe and deliver care to patients while living in their homes, instead of spending months or even years in hospital. The proposed design represents a good approach to research in smart home environments for elderly, keeping in mind that many things have been generalized to a certain extent and the analysis of the vital sign data captured from the medical sensors is still an on going research. Certain crucial issues still have to be resolved regarding the user-friendly ness of the telemedicine system and how does the elderly interact with all of this complex technology. Work is also ongoing in making the smart home design context-aware.
References
Crilly, P. B., Arakawa, E. T., Hedden, D. L., & Ferrell, T. L. (1997). An integrated pulse oximeter system for telemedicine applications. IEEE Proceedings of Instrumentation and measurement Technology Conference, 1, 102–104.
Deni, H., Muratore, D. M., & Malkin, R. A. (2005). Development of a pulse oximeter analyzer for the developing world. IEEE Proceedings of 31st Annual Northeast Bioengineering Conference, pp. 227–228.
Dhem, J. F., & Feyt, N. (2001). Hardware and software symbiosis helps smart card evolution. IEEE Micro, 21(issue 6), 14–25.
Dresher, R. P., & Mendelson, Y. (2006). A new reflectance pulse oximeter housing to reduce contact pressure effects. IEEE Proceedings of 32nd Annual Northeast Bioengineering Conference, pp. 49–50.
Hansmann, U., Merk, L., Nicklous, M. S., & Stober, T. (2003). Pervasive computing. New York: Springer.
Hung, K., Zhang, Y. T., & Tai, B. (2004). Wearable medical devices for tele-home healthcare. IEEE Proceedings of the 26th Annual International Conference of Engineering Medicine and Biology Society, 2, 5384–5387.
Johnston, W. S., & Mendelson, Y. (2004). Extracting breathing rate information from a wearable reflectance pulse oximeter sensor. IEEE Proceedings of the 26th Annual International Conference of the Engineering Medicine and Biology Society, 2, 5388–5391.
Lin, K. J., Yu, T., & Shih, C. Y. (2005). The design of a personal and Intelligent pervasive-commerce system architecture. IEEE proceedings of the second international workshop on mobile commerce and services, pp. 163–173.
Lopera, J. M., Diaz, J., Prieto, M. J., & Nuno, F. (2002). Pulse oximeter for homecare. Proceedings of the 24th Annual Conference and Annual Fall meeting of the Biomedical Engineering Society EMBS/BMED Conference, 2, 1738–1739.
Lukowicz, P., Anliker, U., Ward, J., Troster, G., Hirt, E., & Neufelt, C. (2002). AMON: A wearable medical computer for high risk patients. Proceedings of 6th international symposium on wearable computers, pp. 133–134.
Oliver, N., & Mangas, F. F. (2005). HealthGear: A real-time wearable system for monitoring and analyzing physiological signals. Technical report MSR-TR-2005-182.
Acknowledgements
The author would like to acknowledge the support of King Fahad university Petroleum and Minerals for its support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raad, M.W., Yang, L.T. A ubiquitous smart home for elderly. Inf Syst Front 11, 529–536 (2009). https://doi.org/10.1007/s10796-008-9119-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10796-008-9119-y