Abstract
Purpose
To determine predictors of best-corrected postoperative visual acuity (VA) in patients who underwent surgical intervention for macula-off rhegmatogenous retinal detachment.
Materials and methods
Primary macula-off retinal detachments from the University of Colorado Primary Rhegmatogenous Retinal Detachment Database (2012–2017) were reviewed. The primary outcome measure was a postoperative VA of 20/40 or better at least 6 months after surgery. Patient demographics, medical history, duration of central vision loss before surgery, examination findings, operative technique, and postoperative findings were analyzed as possible predictors of postoperative visual recovery to 20/40 or better. Chi-square or Fisher’s exact test was used to compare categorical variables, and Wilcoxon rank sum test was used for continuous variables. A multivariable logistic regression analysis was used to determine the adjusted odds ratios and 95% confidence intervals for variables that were significant in the univariable analyses. Statistical significance was set at p < 0.05.
Results
One hundred thirty-one patients met inclusion criteria. Eighty-one (61.8%) patients achieved a postoperative VA of 20/40 or better 6 or more months after surgery. Patients with a single retinal break were more likely than patients with more than one break to reach a postoperative VA of 20/40 or better (76.9% vs. 55.4%, p = 0.021). Patients with a better preoperative logMAR VA had better postoperative VA (p = 0.021). Duration of central vision loss prior to surgical repair was not related to final postoperative VA in this particular study.
Conclusion
Postoperative recovery of visual acuity to 20/40 or better was significantly more common in patients with a single retinal break as well as in patients with better preoperative visual acuity. Duration of central vision loss prior to surgical repair was not significantly associated with postoperative VA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary rhegmatogenous retinal detachment (RRD) occurs when a full thickness break in the retina permits separation of the neurosensory retina from the underlying retinal pigment epithelium [1,2,3]. The subsequent accumulation of fluid within the subretinal space extends the area of detachment, causing visual loss [3]. The incidence of this adverse ocular event is between 10.1 and 18.2 per 100,000 individuals, and the macula becomes involved in about 50% of cases [2, 4, 5]. With advancements in surgical visualization and modern surgical techniques, the success rate of complete anatomical attachment of the retina after a single surgery is now estimated to be about 90% [6,7,8,9]. However, despite high rates of successful reattachment of the retina, visual outcomes in macula-off RRDs are not uniform [1, 10].
Previously reported risk factors for poor visual outcomes after macula-off RRD include: worse preoperative visual acuity (VA) [6, 7, 11,12,13], older age [9, 12, 13], duration of macular detachment (DMD) [9, 11,12,13,14,15,16,17,18], choroidal detachment [12], hypotony [12], greater extent of detachment [15], height of detachment [13], preoperative proliferative vitreoretinopathy (PVR) [6], increased number of breaks [6], and large or giant retinal breaks [12, 13, 17]. Many of these risk factors are not modifiable, and thus, further investigation of the predictors of macular function restoration is needed to help guide physicians and adequately counsel patients [16].
The overall objective of our study was to evaluate surgical outcomes of macula-off RRDs at an academic center in Colorado. Our specific objective was to determine factors predictive of good visual outcomes when reattachment was achieved in a single surgery, and to explore the possible effect of high altitude on macular function recovery.
Methods
A retrospective review of records from the University of Colorado, Department of Ophthalmology, Rhegmatogenous Retinal Detachment Registry, was conducted between January 1, 2012, and July 31, 2017. The retinal detachment registry includes information on patients presenting to the UCHealth Sue Anschutz-Rodgers Eye Center for surgical treatment of retinal detachment. Data were collected on the patients’ demographics, medical history, and preoperative and postoperative examinations of the eye. The study adhered to the Declaration of Helsinki and received approval by the Colorado Multiple Institutional Review Board. Some of the patients had follow-up visits with the Department of Ophthalmology at Kaiser Permanente, a healthcare system in Colorado. We collected follow-up data on these patients after the Kaiser Institutional Review Board also approved the study.
Patients aged 18 years and older at the time of surgery with primary macula-off RRD (n = 299) were screened for study inclusion. We excluded patients in the following order: (1) Re-detachment or failure to reattach after a single surgery (n = 41); (2) patients with known diabetic retinopathy, glaucoma, uveitis, age-related macular degeneration, history of trauma, giant retinal tear, retinal vascular occlusions, macular hole, macular epiretinal membrane, retinoschisis (n = 59); (3) PVR at the time of presentation (n = 20); and (4) missing visual acuity (VA) data at 6 months or later follow-up (n = 48). Following exclusions, 131 records remained for analysis.
Visual acuity of 20/40 or better at least 6 months after surgery was the primary outcome measure to indicate functional macular recovery. We divided our analysis into two categories: preoperative factors and surgical factors. Preoperative risk factors included age, sex, altitude of the patient’s primary residence, history of smoking, diabetes, sleep apnea, treated hypertension, preoperative logMAR VA, lens status, duration of macular detachment (DMD, defined as the number of days from the loss of central vision until surgical intervention), number of retinal breaks (1 or greater than 1), and break location (superior, inferior, or both). Surgical factors included type of procedure (pneumatic retinopexy, pars plana vitrectomy, scleral buckle, or combined vitrectomy and scleral buckle), use of perfluorocarbon liquid, tamponade agent (gas, oil, air, or none), and the reason for silicone oil use (to avoid altitude restrictions, patient unable to position, monocular, or uncertain) in cases where silicone oil was used.
We recorded the final follow-up data to be within the range of 6 and 48 months; however, if multiple visits occurred during this timeframe, then the date closest to 12 months was selected as the postoperative visual acuity outcome. At the final follow-up, postoperative complications including ocular hypertension, PVR, epiretinal membrane, cystoid macular edema, hemorrhage (retinal and subretinal), development of a new retinal break, and cataract progression were noted.
Statistical analysis utilized Chi-square or Fisher’s exact test to compare categorical variables and the Wilcoxon rank sum test for continuous variables. A multivariable logistic regression was completed to determine the adjusted odds ratios and 95% confidence intervals for variables that were significant in the univariable analyses. A p value < 0.05 was considered statically significant, and all analyses were performed using SAS software (version 9.4, SAS Institute Inc., Cary, NC, USA).
Results
Table 1 lists demographic and medical status data from the 131 patients who met inclusion criteria. Eighty-one (61.8%) patients achieved a postoperative VA of 20/40 or better 6 or more months after surgery. Eighty-five percent of patients had their final follow-up visit between 6 and 18 months. There was no significant difference in baseline patient demographic and medical history parameters (Table 1) between patients with an outcome better or worse than 20/40.
Preoperative factors
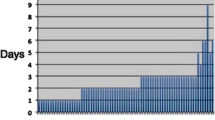
In Table 2, we compare duration of macular detachment symptoms and several preoperative examination findings between patients with VA better than 20/40 and VA worse than 20/40. Patients with a better preoperative logMAR had better postoperative VA (p = 0.021). Patients who achieved the outcome of 20/40 or better had a median preoperative logMAR of 1.3 (Snellen 20/400), compared to a median preoperative logMAR of 2.0 (Snellen 20/2000) for those who did not achieve the desired outcome. Patients with one retinal break were more likely to have a postoperative VA of 20/40 or better than patients with more than one break (76.9% vs. 55.4%, p = 0.021). Half of the patients had a DMD of 0–3 days, but DMD was not related to final postoperative VA in this study (Table 2).
Surgical factors
As shown in Table 3, the most common repair procedure was a combined PPV and SB, which was done in 71 cases (54.2%). This group had the lowest proportion of patients (56.3%) achieving 20/40 or better among all surgical procedures. The least common procedure was pneumatic retinopexy (6.9%), and 8 of these 9 patients (88.9%) achieved postoperative VA of 20/40 or better. A combined PPV and SB was the most commonly performed surgery among both groups regardless of preoperative VA. Thus, preoperative VA did not predict surgical approach (p = 0.066). Twenty-one patients had oil placed as a tamponade agent. Of these patients, the oil was placed in 16 (76.2%) to permit travel to a higher altitude. The average altitude of patients’ residences in the entire cohort was 1738 (standard deviation 236) meters. Neither tamponade nor altitude was associated with a postoperative VA of 20/40 or better.
Postoperative complications
We evaluated postoperative complications at 1 week, 1 month, 3 months, and final follow-up. The most common complications were ocular hypertension and epiretinal membrane formation, none of which were significantly related to type of procedure, postoperative VA, or use of IOP lowering medication at any time following surgery.
At the final follow-up point, 79 (60.3%) patients were pseudophakic, 44 (33.6%) had cataract, and 8 (6.1%) had a clear lens. Among the 18 patients with preoperative lens status of clear, 8 remained clear at the final follow-up point, 8 developed cataract, and 2 patients had artificial lenses implanted. For the 62 patients with preoperative lens status of cataract, 26 (41.9%) were pseudophakic by the final follow-up point. Patients with pseudophakic lens status at the final follow-up had slightly higher rates of postoperative VA of 20/40 or better (68.4%) compared to cataract (54.6%) and clear lens status (37.5%); however, these rates did not significantly differ (p = 0.110).
Multivariable logistic regression
Multivariable logistic regression shown in Table 4 demonstrates that better preoperative logMAR (p = 0.008) and one retinal break (p = 0.027) were statistically significant predictors of postoperative VA of 20/40 or better. Since lens status at end time point could impact postoperative VA outcome, we also analyzed the data with the inclusion of endpoint lens status in the multivariable model. The data in Table 4 are supported by the inclusion of this adjusted model, and the results did not appreciably change the odds ratios or significance values when implemented.
Discussion
Visual outcomes after repair of RRD involving the macula vary greatly. Previous studies have highlighted factors that predict good visual outcomes, but disagreement exists around which factors are useful and to what extent surgeons can use them as predictive tools. In this study, we report our experience treating macula-off RRDs at a large academic referral center. Here, we compare our results with those of previously published studies, as well as comment on the effect of altitude on visual outcomes after surgery in a Colorado cohort.
Of the 131 eyes that achieved reattachment with a single operation, 81 eyes (61.8%) recovered best-corrected VA of 20/40 or better at 6 months or greater follow-up, a proportion within the range of previously reported data [19, 20]. We found that postoperative VA after macula-off RRD is affected by both preoperative VA and the number of breaks. Our finding that preoperative VA is influential in patients’ recovery to achieve good visual outcome is consistent with what has been reported in the established literature [1, 4, 6, 7].
We also found that the presence of more than one retinal break was associated with a lower likelihood of achieving 20/40 or better acuity. To our knowledge, only one other study has associated a higher number of breaks with worse visual outcomes [6]. Doyle et al. found patients with two or more retinal breaks had worse primary success rates than those with less [6]. More breaks may prompt a surgeon to use a longer acting tamponade agent, perform a vitrectomy, or add a scleral buckle. Another possibility is that the presence of more than one break leads to an increased height of detachment, a factor that has previously been shown to indicate a poorer visual outcome [21].
Numerous studies since the late 1970s have shown a clear decline in visual outcomes if surgery is delayed greater than a week, and recent studies have indicated benefits even within the first 3 days after symptomatic loss of central vision [9, 11, 17, 22,23,24]. We found that the DMD had no relationship with visual outcomes in our patient cohort. The reason for this finding is most likely because the vast majority of patients underwent surgery within 1 week of central vision loss. Although the proportion of patients achieving 20/40 or better vision was higher in the group who underwent surgery within 1 week of loss of central vision, the small number of patients with delayed repair may limit the ability to detect statistical significance.
In addition to preoperative factors, we also looked at intraoperative factors and did not find a significant relationship between visual outcome and type of surgical procedure (scleral buckle, vitrectomy, combined buckle/vitrectomy, pneumatic retinopexy), use of perfluorocarbon liquids, or tamponade agent. While our data indicate a greater proportion of patients with optimal visual outcomes underwent pneumatic retinopexy rather than other methods, the small sample limits the statistical significance of this finding. Further, the surgeon’s decision to pursue pneumatic retinopexy depends on ideal case selection which typically includes uncomplicated RRDs, superior breaks of less than one clock hour, and clear view to the retina [24]. It is worth noting the high proportion of cases in our series treated with scleral buckling, either alone or in combination with vitrectomy. While we cannot account for an individual surgeon’s choice of procedure in all cases, one possible reason for the high number of encircling procedures in this series is that several of the surgeons trained at the same institution, leading to high level of commonality in surgical choices among these surgeons.
The location of our surgery center at high altitude distinguishes this patient cohort from previous studies of macula-off visual outcomes. Our patients tended to reside in or travel from the surrounding region, where altitudes typically range from 1219 meters to over 3048 meters above sea level. The effect of altitude on visual recovery following RRD repair has been reported previously, but previous studies have focused on complications from intraocular gas tamponade agents [25]. We used silicone oil in 16 eyes specifically to avoid altitude-induced ocular hypertension, and we did not find any differences in visual outcome or complication rates in this subset of patients. One additional consideration is the lower partial pressure of oxygen at higher elevation, with the hypothesis that lower ambient oxygen tension could limit visual recovery. However, we did not find any difference in outcome for our cohort relative to other reported studies.
This study has several limitations. The strength of our conclusions is limited by the retrospective nature of the study. Data on DMD are inherently imprecise because they rely on the patient’s self-reported history. It is possible the visual acuity results we present here underestimate the true postoperative vision in those patients based on possible cataract progression. We did not routinely obtain optical coherence tomography or ultrasound preoperatively, and so we did not measure height of macular detachment, a factor thought to influence visual outcome [21]. Preoperative macular imaging (either with ultrasound or optical coherence tomography) and its correlation to visual acuity outcomes would be an ideal addition to a study of this type, but real-world case series seldom include macular imaging because it is not normally necessary in diagnosis or management of acute retinal detachment. A prospective study with preoperative imaging would be a logical next step to enhance understanding of these cases.
In this study, we examined a cohort of patients who underwent surgery to repair primary macula-involving RRD. We found that duration of macular detachment did not influence final VA, nor did systemic medical comorbidities, altitude, location of retinal breaks, or type of surgical procedure. We did find that preoperative VA and number of retinal breaks were associated with postoperative visual outcomes. Further study is needed to determine the significance of the number of breaks and its influence on macular recovery after RRD.
References
D’Amico DJ (2008) Clinical practice. Primary retinal detachment. N Engl J Med 359(22):2346–2354. https://doi.org/10.1056/nejmcp0804591
Mitry D, Charteris DG, Fleck BW, Campbell H, Singh J (2010) The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol 94(6):678–684. https://doi.org/10.1136/bjo.2009.157727
Mitry D, Fleck BW, Wright AF, Campbell H, Charteris DG (2010) Pathogenesis of rhegmatogenous retinal detachment: predisposing anatomy and cell biology. Retina 30(10):1561–1572. https://doi.org/10.1097/IAE.0b013e3181f669e6
Wilkes SR, Beard CM, Kurland LT, Robertson DM, O’Fallon WM (1982) The incidence of retinal detachment in Rochester, Minnesota, 1970–1978. Am J Ophthalmol 94(5):670–673
Van de Put MA, Hooymans JM, Los LI (2013) The incidence of rhegmatogenous retinal detachment in The Netherlands. Ophthalmology 120(3):616–622. https://doi.org/10.1016/j.ophtha.2012.09.001
Doyle E, Herbert EN, Bunce C, Williamson TH, Laidlaw DA (2007) How effective is macula-off retinal detachment surgery. Might good outcome be predicted? Eye (London, England) 21(4):534–540. https://doi.org/10.1038/sj.eye.6702260
Ross WH (2002) Visual recovery after macula-off retinal detachment. Eye (London, England) 16(4):440–446. https://doi.org/10.1038/sj.eye.6700192
Thelen U, Amler S, Osada N, Gerding H (2012) Outcome of surgery after macula-off retinal detachment—results from MUSTARD, one of the largest databases on buckling surgery in Europe. Acta Ophthalmol 90(5):481–486. https://doi.org/10.1111/j.1755-3768.2010.01939.x
Hassan TS, Sarrafizadeh R, Ruby AJ, Garretson BR, Kuczynski B, Williams GA (2002) The effect of duration of macular detachment on results after the scleral buckle repair of primary, macula-off retinal detachments. Ophthalmology 109(1):146–152
Lecleire-Collet A, Muraine M, Ménard J-F, Brasseur G (2006) Evaluation of macular changes before and after successful retinal detachment surgery using stratus-optical coherence tomography. Am J Ophthalmol 142(1):176–179. https://doi.org/10.1016/j.ajo.2006.01.080
Burton TC (1982) Recovery of visual acuity after retinal detachment involving the macula. Trans Am Ophthalmol Soc 80:475–497
Tani P, Robertson DM, Langworthy A (1981) Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol 92(5):611–620
van de Put MA, Croonen D, Nolte IM, Japing WJ, Hooymans JM, Los LI (2014) Postoperative recovery of visual function after macula-off rhegmatogenous retinal detachment. PLoS ONE 9(6):e99787. https://doi.org/10.1371/journal.pone.0099787
Frings A, Markau N, Katz T, Stemplewitz B, Skevas C, Druchkiv V, Wagenfeld L (2016) Visual recovery after retinal detachment with macula-off: is surgery within the first 72 h better than after? Br J Ophthalmol 100(11):1466–1469. https://doi.org/10.1136/bjophthalmol-2015-308153
Park DH, Choi KS, Sun HJ, Lee SJ (2018) Factors associated with visual outcome after macula-off rhegmatogenous retinal detachment surgery. Retina (Philadelphia, Pa) 38(1):137–147. https://doi.org/10.1097/iae.0000000000001512
van Bussel EM, van der Valk R, Bijlsma WR, La Heij EC (2014) Impact of duration of macula-off retinal detachment on visual outcome: a systematic review and meta-analysis of literature. Retina (Philadelphia, Pa) 34(10):1917–1925. https://doi.org/10.1097/iae.0000000000000296
Ross WH, Kozy DW (1998) Visual recovery in macula-off rhegmatogenous retinal detachments. Ophthalmology 105(11):2149–2153. https://doi.org/10.1016/s0161-6420(98)91142-3
Liu F, Meyer CH, Mennel S, Hoerle S, Kroll P (2006) Visual recovery after scleral buckling surgery in macula-off rhegmatogenous retinal detachment. Ophthalmologica Journal International d’ophtalmologie International Journal of Ophthalmology Zeitschrift fur Augenheilkunde 220(3):174–180. https://doi.org/10.1159/000091761
Salicone A, Smiddy WE, Venkatraman A, Feuer W (2006) Visual recovery after scleral buckling procedure for retinal detachment. Ophthalmology 113(10):1734–1742. https://doi.org/10.1016/j.ophtha.2006.03.064
Kim JD, Pham HH, Lai MM, Josephson JW, Minarcik JR, Von Fricken M (2013) Effect of symptom duration on outcomes following vitrectomy repair of primary macula-off retinal detachments. Retina (Philadelphia, Pa) 33(9):1931–1937. https://doi.org/10.1097/IAE.0b013e3182877a27
Ross W, Lavina A, Russell M, Maberley D (2005) The correlation between height of macular detachment and visual outcome in macula-off retinal detachments of < or = 7 days’ duration. Ophthalmology 112(7):1213–1217. https://doi.org/10.1016/j.ophtha.2005.01.040
Greven MA, Leng T, Silva RA, Leung L-SB, Karth PA, Moshfeghi DM, Sanislo SR, Schachar IH (2018) Reductions in final visual acuity occur even within the first 3 days after a macula-off retinal detachment. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2018-313191
Diederen RM, La Heij EC, Kessels AG, Goezinne F, Liem AT, Hendrikse F (2007) Scleral buckling surgery after macula-off retinal detachment: worse visual outcome after more than 6 days. Ophthalmology 114(4):705–709. https://doi.org/10.1016/j.ophtha.2006.09.004
Mowatt L, Shun-Shin GA, Arora S, Price N (2005) Macula off retinal detachments. How long can they wait before it is too late? Eur J Ophthalmol 15(1):109–117
Batman C, Cekic O, Totan Y, Aslan O, Ozalp S (1999) Intraocular pressure changes in the vitreon study. Ophthalmic Surg Lasers 30(9):721–726
Acknowledgements
The University of Colorado Retina Research Group: Marc T. Mathias, MD, Frank S. Siringo, MD, Paula E. Pecen, MD, Jeffery L. Olson, MD, James S. Snitzer, BS.
Funding
Support from a Challenge Grant to the Department of Ophthalmology from Research to Prevent Blindness, Inc.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Geiger, M., Smith, J.M., Lynch, A. et al. Predictors for recovery of macular function after surgery for primary macula-off rhegmatogenous retinal detachment. Int Ophthalmol 40, 609–616 (2020). https://doi.org/10.1007/s10792-019-01219-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01219-0