Abstract
Purpose
To describe the OCT angiography characteristics of flat irregular pigment epithelial detachments (PEDs), an overlapping tomographic feature of various macular disorders.
Methods
Consecutive patients with a dimpled retinal pigment epithelium profile on OCT, referred for a second opinion, were enrolled. Fluorescein (FA) and indocyanine green angiography (ICGA) were performed in all patients and compared to previous examinations, when available. In all patients, enhanced depth imaging-OCT and OCT angiography were performed upon referral and at subsequent follow-ups.
Results
Twenty-five eyes from 25 patients (9 women and 16 men, mean age of 63.4 years) were enrolled. The diagnoses of CSCR were already established by the referring physicians in 10 patients, acute in 15% and chronic in 26%; 48% of patients were referred with a diagnosis of type 1 CNV, and 11% of CSCR complicated by CNV. After performing OCT angiography, 2 masked examiner identified 7 type 1 CNV (29%), 18 eyes with pachychoroid disease of which 31% pachychoroid pigment epitheliopathies (PPEs) at baseline evolved to CSCR, 22% PPE at baseline evolved to pachychoroid neovasculopathy, 18% pachychoroid neovasculopathy stable.
Conclusion
Central serous chorioretinopathy, type 1 CNV, and the pachychoroid spectrum of diseases cause abnormalities in the choroidal circulation that make the overlying RPE dysfunctional, resulting in flat irregular PED. Discrimination between avascular and vascular flat irregular PEDs is crucial for a good visual outcome, but since chronic alterations of the RPE can compromise the diagnostic specificity of FA and ICGA, OCT angiography may become a fundamental tool to differentiate these clinical entities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Flat irregular detachments of the retinal pigment epithelium (PED) [1, 2] is one of the most common optical coherence tomography (OCT) findings of type 1 choroidal neovascularization (CNV) in age-related macular degeneration (AMD) [3]. At the same time, irregular PED is a well-known feature of chronic central serous chorioretinopathy (CSRC) [1, 3], in which it has been described as “RPE with an irregular wave” or “low to flat PED” with an irregular or dimpled surface, and similar PED profiles have also been documented in acute CSCR and have been called “irregular RPE layer” or “RPE irregularities” [1]. The interpretation of this overlapping tomographic feature has been complicated by the possible progression, although rare, of these flat irregular PEDs toward a CNV in eyes with long-term CSCR, while the majority seem to remain avascular, with no evolution toward obvious CNV [4].
Optical coherence tomography enhanced depth imaging (EDI) function has allowed to determine the status of the choroid underlying these flat PEDs [5]. The term pachychoroid pigment epitheliopathy (PPE) [6, 7] has been proposed as a term indicating retinal pigment epithelium (RPE) alterations with no documented subretinal fluid with an underlying abnormal and permanent dilatation of the large Haller’s choroidal vessels compressing the overlying choriocapillaris and Sattler’s layer. Pachychoroid neovasculopathy (PNV) is considered a late complication of PPE [8, 9] with OCT findings similar to those described for PPE but in the presence of sub-RPE neovascular tissue. In the presence of pachychoroid, choroidal hyperpermeability and chronic alterations of the RPE [10] can compromise the diagnostic specificity of fluorescein angiography (FA) and indocyanine green angiography (ICGA) for type 1 neovascularization, leaving the clinician with some uncertainty as to the vascularity of these PEDs.
Recently, new imaging technologies have developed that allow for new insights into the visualization of normal and pathologic vascularization. Specifically, a software called “split-spectrum amplitude-decorrelation angiography” allows for the visualization of both the inner and outer retinal vascular plexi and the choriocapillaris layer without the need for dye injection [11]. It may be at times difficult to visualize these vascular complexes with FA and ICG angiography. This algorithm enables the noninvasive visualization of vessels in the posterior part of the eye with a segmentation of the different layers using the “en face” OCT modality [12].
In this report, we describe the OCT angiography characteristics of these overlapping flat irregular PEDs in patients with an uncertain diagnosis of CSCR or AMD.
Methods
The present study was approved by the ethical committee of the Cleveland Clinic Abu Dhabi, UAE; informed consent was obtained from all of the patients, and all research and data collection complied with the Declaration of Helsinki. We enrolled consecutive patients that were referred to our third-level Retina Clinic with an irregular RPE profile with dimpled or irregular surface on SD-OCT and a dubious diagnosis of acute/chronic CSCR or type 1 CNV.
Ophthalmic findings at the time of referral and at each follow-up visit were recorded, including best-corrected visual acuity, slit-lamp and dilated fundus examination. FA and ICGA of the posterior pole and the nine peripheral fields were performed in all patients and compared to previous examinations, when available. In all patients, B-scan and “en face” C-scan EDI-SD-OCT were performed upon referral with a Spectralis-HRA instrument (Spectralis HRA + OCT; Heidelberg Engineering, Heidelberg, Germany). “En face” macular mapping was obtained with 197 transverse sections in a 5.79 × 5.79 mm2 central retinal area. Then, tridimensional reconstruction generated by pooling these sections provided a virtual macular brick, through which 496 shifting sections in the coronal plane result in the C-scan or “en face” OCT. B- and C-scans were repeated during the early and late recovery phase. Optical coherence tomography angiography (3 × 3 mm; 216 × 216 points; 3.8 s) was obtained for all patients upon referral and at subsequent follow-ups using a 70-kHz, 840-nm wavelength commercial spectral OCT (RTVue-XR Avanti; Optovue, Inc, Fremont, CA) using the split-spectrum amplitude-decorrelation angiography algorithm [13]. At a rate of 70,000 A-scans per second, the device produced two OCT volumes consisting of 304 × 304 A-scans each in around 3 s. From these volumes, prototype OCTA software applied a split-spectrum amplitude-decorrelation angiography (SS-ADA) algorithm to produce OCT angiograms. The OCT angiograms are primarily shown in en face views in which each pixel represents the maximum flow value detected within the relevant anatomy layers. Using OCTA software, OCTA volumes of the outer retina were automatically segmented by AngioVue software between Bruch membrane and the inner nuclear layer/outer plexiform layer junction [14]. Normally, this region is devoid of blood vessels; therefore, increased signal likely indicates CNV. Optical coherence tomography angiography angiograms were read by one trained retinal specialist to determine the presence or absence of choroidal neovascularization.
Results
Twenty-five eyes from 25 patients (9 women and 16 men) were enrolled. The patients ranged in age from 45 to 79 years with a mean age of 63.4 years. All of the patients were Caucasian. The diagnoses of CSCR were already established by the referring physicians in 10 patients, acute in 15% and chronic in 26%; 48% of patients were referred with a diagnosis of type 1 CNV, and 11% of CSCR complicated by CNV. Twenty-one study eyes had a history of prior treatment. Nine eyes had received intravitreal anti-VEGF treatment (mean 8.2 injections per eye), 6 eyes had received photodynamic therapy with verteporfin (mean 1.6 treatments per eye), and 6 had been treated with oral eplerenone 50 mg per day for a mean of 3.2 months.
Upon referral, flat irregular PEDs were diagnosed in 25/25 eyes by analyzing multiple SD-OCT scans. Fluorescein angiography was available for 25 study eyes and revealed classic features of type 1 CNV in 5 eyes. In the remaining eyes, type 1 neovascularization could not be diagnosed specifically, since the pattern of hyperfluorescence could not be distinguished from that seen in chronic central serous chorioretinopathy. Indocyanine green angiography was available for 25 eyes and revealed hyperfluorescent neovascular plaques in 4 eyes. Therefore, the detection rate for type 1 neovascularization based on combined FA and ICGA analysis was 5 out of 25 eyes (20%). The mean interval between FA/ICG and OCT angiography for the 25 eyes enrolled in this trial was 6 months. After performing OCT angiography and comparing the information obtained with SD-OCT, FA, and ICGA, the 2 masked examiner identified in the en face OCT angiograms taken through the PEDs, 7 type 1 CNV (29%) with large-caliber feeder vessels and 18 eyes with pachychoroid disease (on the basis of an extrafoveal focus of maximal choroidal thickness exceeding subfoveal choroidal thickness by at least 60 mm or pachy-vessels with distinctive en face OCT morphology) [6, 7]. Of these 18 eyes, 31% PPE at baseline evolved to CSCR, 22% PPE at baseline evolved to pachychoroid neovasculopathy, 18% pachychoroid neovasculopathy remained stable from baseline.
Representative case examples
Pachychoroid pigment epitheliopathy evolved to pachychoroid neovasculopathy
Twenty-two percent of the eyes presented to our examination with RPE abnormalities on SD-OCT scans with no subretinal fluid, and no sign of CNV either in FA or in ICGA; enhanced depth imaging showed a focal dilation of the large Haller’s choroidal vessels underlying the RPE disturbance. These 5 eyes, during subsequent follow-ups, displayed a various amount of subretinal fluid, which was interpreted in 3 cases as an acute CSCR (treated with observation and 2 photodynamic therapies with verteporfin) and in 2 cases as a type 1 CNV (treated with 5.2 mean intravitreal anti-VEGF injections). Upon referral to our department, OCT angiography revealed a high-flow choroidal neovessel network corresponding to the flat PEDs notable on SD-OCT, and a persistence of the focal dilation of the large outer choroidal vessels, with obliteration of the overlying choriocapillaris. The final diagnosis of pachychoroid neovasculopathy was made, and the patients were treated accordingly.
Case example
In this 62-year-old man, baseline SD-OCT scans (Fig. 1a) did not reveal, upon review, AMD changes such as drusen, but simply focal RPE changes with a large-caliber choroidal vessel underneath. At the 6-month follow-up, subretinal fluid (SRF) overlying a small PED appeared on OCT. Of significance, there still was focal thickening of the choroid with large dilated vessels directly beneath the flat PED (Fig. 1b). There was also obliteration of the choriocapillaris and Sattler’s layer in the area of the largest vessel caliber. Fluorescein angiography showed staining of the RPE disturbance (Fig. 1c), and ICGA (Fig. 1d) did not show an hyperfluorescent plaque. The diagnosis of CSCR was made, and no treatment was administered. The patient was monitored twice a year. Ten months later, OCT showed fluctuation of the subretinal fluid (Fig. 1e), and the patient was referred to our center for further evaluations. ICGA (Fig. 1g) showed a late macular hyperfluorescent plaque: The suspect of CNV with large dilated vessels beneath the area of neovascular tissue was confirmed by OCT angiography, which showed high flow in a CNV network (Fig. 1h). The diagnosis of PNV was made. The patient was treated with intravitreal anti-VEGF therapy with modest improvement of the SRF.
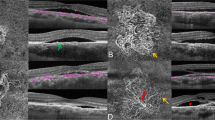
A 62-year-old man with RPE changes on SD-OCT overlying a focally dilated outer choroid (a) and an obliterated choriocapillaris. At the 6-month follow-up, OCT revealed subretinal fluid overlying a small, flat pigment epithelium detachment (b) that stained in fluorescein angiography (c) and was not associated with a neovascular hyperfluorescent plaque in indocyanine green angiography (d). The diagnosis of CSCR was made, and the patient was monitored. 10 months later the patient was referred to our center, where OCT showed reduction in the subretinal fluid (e) and a persistence of the focal dilation of the choroid, and ICGA (g) showed a late macular hyperfluorescent plaque: the suspect of pachychoroid neovasculopathy was confirmed by OCT angiography, which showed high flow in a CNV network (h)
Pachychoroid neovasculopathy
Eighteen percent of the eyes, referred with a type 1 CNV, upon review of the baseline examinations presented with a flat irregular PEDs with variable amount of subretinal fluid, and a focally thick choroid underlying the lesion. All 18% of the eyes had previously been treated with intravitreal anti-VEGF (mean number of injections 4.6, range 2–7), with a complete reabsorption of the fluid in 41% of the eyes, a partial reabsorption (defined as persistence of fluid on OCT) in 38% of the eyes, and no response in 21% of the eyes (defined as a decrease in central macular thickness of less than 10% compared to baseline). When first examined with OCT angiography, all the eyes exhibited a high-flow vascular network in the otherwise avascular outer retina corresponding to the flat irregular PED, and a type 1 CNV was confirmed by ICGA. However, the Haller’s layer remained focally engorged under the CNV in 100% of these eyes with a compression of the overlying choriocapillaris. This feature, associated with the absence of typical AMD findings on fundus examination, pointed toward a diagnosis of pachychoroid neovasculopathy.
Case example
This 70-year-old patient was referred for the diagnosis of CSCR not respondent to oral eplerenone. On SD-OCT, the choroidal vessel caliber was largest under the flat PED (Fig. 2b), which proved to be vascularized on OCT angiography that showed details of the CNV structure (Fig. 2a). Of note, the neovasculopathy in this patient is accompanied at baseline on OCT angiography by a “darker halo” encircling the lesion, indicating a region of severe choriocapillaris alteration (Fig. 2a). A diagnosis of PNV was made, and the patient received intravitreal anti-VEGF therapy (a total of 4 injections given every 6 weeks over the course of 6 months) with improvement of the SRF (Fig. 2d, f). At the same time, the network density decreased on OCT angiography (Fig. 2c, e), with residual flow more visible close to the afferent trunk, and circumferential anastomosis border reduction all around the PNV (Fig. 2e).
A 70-year-old patient, referred for CSCR, on SD-OCT revealed subretinal fluid, and a focally dilated choroidal vessels under a flat PED (b), which proved to be vascularized on OCT angiography (a). A diagnosis of pachychoroid neovasculopathy was made, and the patient received 4 intravitreal anti-VEGF injections with improvement of the subretinal fluid (d, f) and disappearance on OCT angiography of the darker halo of ischemia surrounding the neovessels at baseline (c, e)
Type I neovascular membrane
Of the 48% eyes referred with a diagnosis of type I CNV secondary to AMD, only 29% had an actual pure type I CNV on OCT angiography, without any hypertrophic changes of the underlying choroid.
Case example
When this 65-year-old patient was referred to us, review of the baseline SD-OCT showed an area of subretinal fluid, combined with a flat irregular PED (Fig. 3a). Fluorescein angiography revealed a ring of late leakage (Fig. 3b), and ICGA a staining of a choroidal plaque (Fig. 3c). Nine intravitreal injections had been administered over the previous 12 months, initially resulting in a flattening of the serous retinal detachment (SRD) (Fig. 3d), but the SRF continuously relapsed thereafter (Fig. 3e). The treatment was then discontinued, and the patient referred for a possible misdiagnosis. However, OCT angiography (Fig. 3f) showed details of the CNV structure, with a central feeder vessel from which radiated thick core vessels ending in fine vascular fronds. His old scans were examined, and no pachychoroid changes were detected.
A 65-year-old patient was diagnosed with type 1 choroidal neovascular membrane based on an SD-OCT showing subretinal fluid with a flat irregular PED (a), on a ring of pooling hyperfluorescence on fluorescein angiography with surrounding speckled staining (b), and staining of a choroidal plaque in indocyanine green angiography (c). After 9 intravitreal anti-VEGF injections, with a temporary response (d), the treatment was discontinued, more fluid recurred (e) and the patient was referred for a second opinion. OCT angiography (f) showed details of the CNV structure, with a central feeder vessel from which radiated thick core vessels ending in fine vascular fronds. His old scans were examined, and no pachychoroid changes were detected
Pachychoroid pigment epitheliopathy evolved to central serous chorioretinopathy
Of the eyes which had a baseline a flat irregular PED with no SRF but a thickened outer choroidal layer, 31% developed during the course of their follow-up a neurosensory detachment. The multimodal imaging, however, did not reveal a frank vascularized PED, and upon referral, OCT angiography did not show a high-flow neovascular net in any of these patients, confirming the diagnosis of a CSCR.
Case example
A 59-year-old patient presented with a baseline PPE (Fig. 4a) and retuned after one year with decreased vision and an unusual hyperreflectivity of the subfoveal RPE surrounded by SRF (Fig. 4b). Indocyanine green angiography showed an area of hyperfluorescence located overlying a large dilated choroidal vessel (Fig. 4e). She underwent 2 intravitreal injections of anti-VEGF, but in March 2014 the fluid was unchanged. On OCT angiography (Fig. 4f), no signs of a CNV were detected, and dilated deeper choroidal vessels proved to have a perfect correspondence to the ICG findings: The diagnosis of a CSCR was confirmed, and the patient was treated with half-fluence photodynamic therapy.
A 59-year-old patient with a baseline PPE (a) on SD-OCT retuned after one year with decreased vision and an RPE irregularity with SRF (b). Differential diagnosis at this time point included CSCR and neovasculopathy from the previous pachychoroid disease. The patient was observed for 3 additional months with no SD-OCT changes (c), and fluorescein angiography was not helpful in differentiating between the two entities (d). Indocyanine green angiography showed the area of hyperfluorescence corresponding to a large dilated choroidal vessel (e). On OCT angiography (f), no signs of a CNV were detected, and dilated deeper choroidal vessels proved to have a perfect correspondence to the ICG findings: The diagnosis of a CSCR was confirmed
Discussion
Flat irregular PED [1] resides within a spectrum of disease [15, 16], including type 1 CNV [4, 6], CSRC [8], PPE and PNV [17,18,19], and occurs due to abnormalities in the choroidal circulation that make the overlying RPE dysfunctional, resulting in focal RPE alterations. Choroidal ischemia and inflammation [10] have been proposed as instigating processes in CSCR, resulting in increased choroidal vascular hyperpermeability and eventually resulting in the leakage of serous fluid into the subretinal space. However, not just overall choroidal thickness but even large focal choroidal vessels may be implicated in the pathogenesis flat, irregular PEDs [1]. A pachychoroid-driven process [7] involving focal choroidal dilation and hyperpermeability manifested by choroidal thickening and dilated choroidal vessels is the pathophysiology underlying PPE, which represents a “forme fruste” of CSCR and falls within the same pathophysiologic spectrum [18], with localized areas of choroidal thickening tomographically visible directly below the RPE alterations.
An early discrimination between these avascular and vascular flat irregular PEDs is crucial for a good visual outcome [20]. The earlier a type 1 CNV is diagnosed and treated, the better is the final visual acuity that can be achieved [21]. The relationship is also valid for CNV complicating chronic CSCR and for sub-RPE pachychoroid neovasculopathy [6]. Knowledge of the presence of pachychoroid neovasculopathy becomes especially important when photodynamic therapy is being considered in patients with chronic CSCR [4], given the potential for photodynamic therapy to upregulate vascular endothelial growth factor expression and activate clinically silent neovascularization. Distinguishing avascular flat irregular PED from type 1 CNV of low-grade activity can, however, be challenging because the signs of CNV can overlap with those of chronic CSCR, and we lack accurate tomographic criteria to distinguish avascular flat irregular PEDs from early stages of type 1 CNV. FA usually shows a stippled early hyperfluorescence with ill-defined late staining, which is consistent with both type 1 CNV and widespread RPE changes in chronic CSCR. ICGA in CSCR shows focal or multifocal “plaques” of choroidal staining progressively spreading but vanishing at the latest phase; these plaques persist in the late phase of angiography if type 1 CNV is complicating chronic CSCR. Unfortunately, in the context of RPE atrophy these 2 patterns of ICGA fluorescence cannot be easily distinguished.
In the present study, the presence of CNV in cases with irregular RPE profiles was detected with the help of OCT angiography [22]. Split-spectrum amplitude-decorrelation angiography [23] analysis showed that 70% of the shallow irregular PEDs in our study harbored type 1 tangled vascular networks. Fluorescein angiography and ICGA underestimate the prevalence of neovascularization in this setting (48%), probably because neovascular tissue may be of an insidious and/or indolent nature. The frequency with which quiescent neovascularization evolves to clinical significance is unknown, but our results indicate that flat irregular PEDs point toward a closer follow-up of the patient, employing dye-based traditional angiography as well as OCT angiography. Whether pachychoroid neovasculopathy that is undetectable by conventional imaging warrants the same anti-VEGF treatment thresholds and regimens as neovascular age-related macular degeneration remains undetermined.
The present study was designed with a consecutive recruitment strategy to estimate the prevalence of vascularized shallow irregular PEDs within the spectrum of type 1 CNV and CSCR. As such, several limitations should be considered when interpreting the data we presented. First of all, a possible selection bias, given that we recruited patients referred to our third-level retina clinic for a second opinion and non-responsiveness to treatment. A second limitation is certainly represented by the different time points in the multimodal imaging, especially between dye- and OCT angiography [24,25,26]. Furthermore, the number of eyes recruited was too small to provide statistically significant data. Finally, the patients we recruited were not naïve to treatment and had heterogeneous treatment histories.
In conclusion, we found an OCT angiography detection rate for type 1 neovascularization under shallow irregular PEDs to be relatively high at 70%. Patients with shallow irregular PEDs neovascularization may be misinterpreted as having AMD, pachychoroid, or chronic CSCR neovascularization and may in fact be avascular. The information provided by this new technology [27] should be combined with different imaging modalities to detect low-activity type 1 CNVs, in order not to rely on observation or even response to anti-VEGF treatment response to diagnose these ambiguous cases.
References
Hage R, Mrejen S, Krivosic V, Quentel G, Tadayoni R, Gaudric A (2015) Flat irregular retinal pigment epithelium detachments in chronic central serous chorioretinopathy and choroidal neovascularization. Am J Ophthalmol 159(5):890–903
Karatepe Hashas AS, Göktas A, Atas M (2014) Isolated multiple pigment epithelial detachments with unknown cause. Case Rep Ophthalmol Med 2014:289107
Mukai R, Sato T, Kishi S (2014) A hyporeflective space between hyperreflective materials in pigment epithelial detachment and Bruch’s membrane in neovascular age-related macular degeneration. BMC Ophthalmol 14:159
Bonini Filho MA, de Carlo TE, Ferrara D, Adhi M, Baumal CR, Witkin AJ, Reichel E, Duker JS, Waheed NK (2015) Association of choroidal neovascularization and central serous chorioretinopathy with optical coherence tomography angiography. JAMA Ophthalmol 133(8):899–906
McClintic SM, Kim DY, Fingler J, Garcia S, Zawadzki RJ, Morse LS, Park SS, Fraser SE, Werner JS, Ruggiero JP, Schwartz DM (2015) Detection of pigment epithelial detachment vascularization in age-related macular degeneration using phase-variance OCT angiography. Clin Ophthalmol 15(9):1299–1305
Gallego-Pinazo R, Dolz-Marco R, Gómez-Ulla F, Mrejen S, Freund KB (2014) Pachychoroid diseases of the macula. Med Hypothesis Discov Innov Ophthalmol 3(4):111–115
Warrow DJ, Hoang QV, Freund KB (2013) Pachychoroid pigment epitheliopathy. Retina 33(8):1659–1672
Pang CE, Freund KB (2015) Pachychoroid neovasculopathy. Retina 35(1):1–9
Miyake M, Ooto S, Yamashiro K, Takahashi A, Yoshikawa M, Akagi-Kurashige Y, Ueda-Arakawa N, Oishi A, Nakanishi H, Tamura H, Tsujikawa A, Yoshimura N (2015) Pachychoroid neovasculopathy and age-related macular degeneration. Sci Rep 5:16204
Yannuzzi NA, Mrejen S, Capuano V, Bhavsar KV, Querques G, Freund KB (2015) A central hyporeflective subretinal lucency correlates with a region of focal leakage on fluorescein angiography in eyes with central serous chorioretinopathy. Ophthalmic Surg Lasers Imaging Retina 46(8):832–836
Spaide RF, Fujimoto JG, Waheed NK (2015) Optical coherence tomography angiography. Retina 35(11):2161–2162
El Ameen A, Cohen SY, Semoun O, Miere A, Srour M, Quaranta-El Maftouhi M, Oubraham H, Blanco-Garavito R, Querques G, Souied EH (2015) Type 2 neovascularization secondary to age-related macular degeneration imaged by optical coherence tomography angiography. Retina 35(11):2212–2218
Palejwala NV, Jia Y, Gao SS, Liu L, Flaxel CJ, Hwang TS, Lauer AK, Wilson DJ, Huang D, Bailey ST (2015) Detection of nonexudative choroidal neovascularization in age-related macular degeneration with optical coherence tomography angiography. Retina 35(11):2204–2211
Bonnin S, Mané V, Couturier A, Julien M, Paques M, Tadayoni R, Gaudric A (2015) New insight into the macular deep vascular plexus imaged by optical coherence tomography angiography. Retina 35(11):2347–2352
Rahimy E, Freund KB, Larsen M, Spaide RF, Costa RA, Hoang Q, Christakopoulos C, Munch IC, Sarraf D (2014) Multilayered pigment epithelial detachment in neovascular age-related macular degeneration. Retina 34(7):1289–1295
Dansingani KK, Balaratnasingam C, Klufas MA, Sarraf D, Freund KB (2015) Optical coherence tomography angiography of shallow irregular pigment epithelial detachments in pachychoroid spectrum disease. Am J Ophthalmol 160(6):1243–1254
Dansingani KK, Balaratnasingam C, Naysan J, Freund KB (2015) En face imaging of pachychoroid spectrum disorders with swept-source optical coherence tomography. Retina 36(3):499–516
Pang CE, Freund KB (2014) Pachychoroid pigment epitheliopathy may masquerade as acute retinal pigment epitheliitis. Investig Ophthalmol Vis Sci 55(8):5252
Lehmann M, Bousquet E, Beydoun T, Behar-Cohen F (2015) Pachychoroid: an inherited condition? Retina 35(1):10–16
Chen FK, Viljoen RD, Bukowska DM (2015) Classification of image artefacts in optical coherence tomography angiography of the choroid in macular diseases. Clin Exp Ophthalmol. doi:10.1111/ceo.12683 (Epub ahead of print)
Zago Filho LA, Moreira AT, Malafaia O, Matias JE (2014) Grid laser photocoagulation in the treatment of serous avascular pigment epithelial detachment in age-related macular degeneration. Arq Bras Oftalmol 77(5):315–320
Hoerster R, Muether PS, Sitnilska V, Kirchhof B, Fauser S (2014) Fibrovascular pigment epithelial detachment is a risk factor for long-term visual decay in neovascular age-related macular degeneretion. Retina 34(9):1767–1773
Huang D, Jia Y, Rispoli M, Tan O, Lumbroso B (2015) Optical coherence tomography angiography of time course of choroidal neovascularization in response to anti-angiogenic treatment. Retina 35(11):2260–2264
Dansingani KK, Freund KB (2014) Optical coherence tomography angiography reveals mature, tangled vascular networks in eyes with neovascular age-related macular degeneration showing resistance to geographic atrophy. Ophthalmic Surg Lasers Imaging Retina 46(9):907–912
Chen FK, Viljoen RD, Bukowska DM (2015) Classification of image artefacts in optical coherence tomography angiography of the choroid in macular diseases. Clin Exp Ophthalmol. doi:10.1111/ceo.12683 (Epub ahead of print)
Cheng Y, Guo L, Pan C, Lu T, Hong T, Ding Z, Li P (2015) Statistical analysis of motion contrast in optical coherence tomography angiography. J Biomed Opt 20(11):116004
Spaide RF, Fujimoto JG, Waheed NK (2015) Image artifacts in optical coherence tomography angiography. Retina 35(11):2163–2180
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pichi, F., Morara, M., Veronese, C. et al. The overlapping spectrum of flat irregular pigment epithelial detachment investigated by optical coherence tomography angiography. Int Ophthalmol 38, 975–983 (2018). https://doi.org/10.1007/s10792-017-0547-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-017-0547-x