Abstract
Purpose
To evaluate the corneal topographic changes and postvitrectomy astigmatism after 27-gauge (g) microincision vitrectomy surgery (MIVS) by using Pentacam HR-Scheimpflug imaging system.
Methods
This prospective descriptive study included 30 eyes of 30 patients who underwent 27-g MIVS. All eyes underwent a Pentacam HR examination preoperatively and on the first week, first month and third month postoperatively. The power of the corneal astigmatism, mean keratometry (K m), K 1 and K 2 values and corneal asphericity (Q value) values for the both front and back surfaces of the cornea, index of surface variance (ISV), index of vertical asymmetry (IVA), index of height asymmetry (IHA), index of height decentration (IHD) and higher-order aberrations including coma, trefoil, spherical aberration, higher-order root-mean-square and total RMS were recorded. Additionally, the mean induced astigmatism was estimated by vector analysis.
Results
No statistically significant changes were observed in the mean power of corneal astigmatism, mean keratometry, K 1 and K 2 values, corneal asphericity values, ISV, IVA, IHA, IHD and higher-order aberrations on the first week, first month and third month after the operation. The mean surgically induced astigmatism was calculated as 0.23 ± 0.11 D on the first week, 0.19 ± 0.10 D on the first month and 0.19 ± 0.08 D on the third month postoperatively.
Conclusion
Minor corneal surface and induced astigmatic changes are expected to result in rapid visual rehabilitation after pars plana vitrectomy with the 27-g MIVS system.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Microincision vitrectomy surgery (MIVS) with 23-gauge (g) and 25-g instrumentations has largely replaced with traditional 20-g pars plana vitrectomy (PPV). As increasing the number of the patients who obtain excellent postoperative visual outcomes after MIVS, possible induction of corneal astigmatism could be clinically important. It has been well documented in the literature that utilization of smaller diameter instruments with self-sealing, transconjunctival scleral wounds provides some advantages such as decreased postoperative pain and inflammation, decreased induced astigmatism, faster visual recovery and improved patient comfort [1–4].
In 2010, Oshima et al. [5] firstly described the initial feasibility and safety of a novel 27-g instrument system, reporting excellent visual and anatomic outcomes in a series of 31 patients. They reported that 27-g MIVS is feasible and may reduce concerns about wound sealing-related complications in selected cases. In the last few years, successful results have been documented in a variety of vitreoretinal disorders with 27-g MIVS [6–9].
In this study, we aimed to evaluate the corneal topographic changes and postvitrectomy astigmatism after 27-g MIVS by using Pentacam HR-Scheimpflug imaging system (Oculus, Wetzlar, Germany), which is a reproducible method that measures almost all anterior segment parameters.
Subjects and methods
Study design and patient selection
This clinical prospective descriptive study was performed at the Retina unit of Ankara Ulucanlar Eye Training and Research Hospital from May 2015 to September 2016. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Thirty eyes of 30 patients who underwent 27-g MIVS were enrolled. Twelve eyes of these patients had idiopathic epiretinal membrane (40%), 8 had idiopathic macular hole (26.6%), 7 had diabetic retinopathy with non-clearing vitreous hemorrhage (23.3%), 2 had central retinal vein occlusion with non-clearing vitreous hemorrhage (6.6%), and the remaining 1 had asteroid hyalosis (3.3%). All patients in the study had phakic crystalline lens status in both eyes. Patients with any of the following conditions were excluded: a history of corneal changes prior to the surgery such as corneal trauma, scar, haze, opacities and degeneration, corneal transplant, corneal ectasias such as keratoconus, a history of corneal and ocular surgery, a history of contact lens usage, lens opacities that would like require cataract extraction during the 27-g MIVS and those who were not sufficiently cooperative for Pentacam HR examinations. The patients who required additional surgery were not included. In addition, since the corneal changes associated with silicon oil had been reported [10], the patients who required silicone oil tamponad were also excluded from the study. All cases underwent a comprehensive ophthalmic examination including best-corrected visual acuity (BCVA) using the Snellen chart, intraocular pressure (IOP) measurement with Goldmann applanation tonometry, anterior segment examination with slit lamp biomicroscopy, dilated fundus examination and Pentacam HR examination. All these ocular examinations and measurements were performed preoperatively and on the first week (7th day), first month (30th day) and third month (90th day) postoperatively. In order to calculate and compare visual acuity, Snellen acuity was converted to logMAR.
Corneal topographic analysis
Corneal topographic analysis was performed by the same masked experienced clinician using the same Pentacam HR-Scheimpflug imaging system (Oculus, Wetzlar, Germany). Three measurements were made per eye, and the one with the best alignment and fixation was selected for data analysis. Corneal refractive map, topometric map and zernike analysis were evaluated for each patient in the study. The power of the corneal astigmatism, mean keratometry (K m), K 1 and K 2 values and corneal asphericity (Q value) values for the both front and back surfaces of the cornea, index of surface variance (ISV), index of vertical asymmetry (IVA), index of height asymmetry (IHA), index of height decentration (IHD) and higher-order aberrations including coma, trefoil, spherical aberration (SA), higher-order root-mean-square (HO-RMS) and total RMS were recorded. ISV describes the deviation of the individual corneal radii from the mean value and is elevated with irregular corneas. IVA gives the degree of symmetry of the corneal radii with respect to the 180° meridian as axis of reflection. IVA is elevated in cases of oblique axes or corneal ectasias such as keratoconus. IHA gives the degree of symmetry of height data with respect to the horizontal meridian as axis of reflection. IHA is analogous to IVA, but sometimes more sensitive. IHD is calculated from first harmonic of Fourier analysis of height and is a measure for vertical decentration.
These all of the topographic measurements were taken preoperatively and on the first week (7th day), first month (30th day) and third month (90th day) postoperatively.
Surgical procedure
In each case, the 27-g MIVS was performed under local anesthesia by retrobulbar injection. Surgical eyes were prepared using 5% povidone-iodine (Betadine; Purdue Fredrick Co, Norwalk, Connecticut, USA). All surgeries were performed using the Constellation Vitrectomy 27+ Total Plus Pak vitrectomy system (Alcon Laboratories) by the same surgeon (K.S). Cannulas were inserted in the inferotemporal, superotemporal and superonasal quadrants 3.0–4 mm posterior to the limbus. The conjunctiva and Tenon’s capsule were displaced over the sclera to avoid communication between conjunctival and scleral entry sites. Trocar cannulas were inserted tangentially at an angle of approximately 30°, parallel to the limbus. All eyes underwent core vitrectomy followed by removal of the posterior hyaloid membrane and vitreous traction. Retinal endophotocoagulation was used in selected eyes. Membrane and/or internal limiting membrane peeling was performed for epiretinal membrane (ERM) or macular hole indications. Air–fluid exchange was performed in eyes with persistent vitreous hemorrhage. Partial air–fluid exchange was performed in eyes with epiretinal membrane. The eyes with macular hole received fluid–gas exchange (16–18% sulfur hexafluoride [SF6]). At the end of the surgery, microcannulas were removed from the eye. The infusion line was clamped during removal of the microcannula and then unclamped after removal. A gentle massage to the sclerotomy site with a muscle hook was performed to avoid leakage. The conjunctiva overlying the sclerotomy was slightly displaced to disrupt the alignment between both entry sites, and the corticosteroid (dexamethasone) was injected into the inferonasal subconjunctival space.
No difficulties were encountered during the insertion of the trocars into any eye. Passage of the 27-g instruments through the microcannula was found to be uncomplicated, and the required procedures were performed with ease in all eyes. No sutures were needed to close the scleral or conjunctival openings, and no intraoperative complications occurred in any eye.
Statistical analysis
Study data were analyzed using the Statistical Package for Social Sciences (SPSS) for Windows version 22.0 (SPSS Inc., Chicago, IL). Descriptive statistics were presented as mean ± standard deviation, frequency distribution and percentages. Chi-square test was used in the analysis of categorical variables. Normal distribution of the variables was tested by visual (histogram and probability graphs) and analytical methods (Kolmogorov–Smirnov/Shapiro–Wilk test). The preoperative and postoperative measurements were compared using paired-samples t test. Additionally, surgically induced astigmatism was calculated by the vector analysis method, which was described by Jaffe [11].
Results
This study included 30 eyes of 30 patients who underwent 27-g MIVS and followed-up at least 3 months. Overall, 18 (60%) of the patients were male and 12 (40%) were female. The mean age of the patients was 65.47 ± 8.53 (range 55–87) years.
The mean preoperative BCVA was 1.36 ± 0.90 (range 3.10–0.4) logMAR. The mean overall BCVA was 0.62 ± 0.38 (range 1.51–0.10) on the first week, 0.41 ± 0.24 (range 1.00–0.10) on the first month and 0.34 ± 0.25 (range 1.00–0.00) on the third month postoperatively. There was a statistically significant improvement in BCVA on the first week, first month and third month compared to the preoperative BCVA (for each one, p < 0.05). Serial changes in the mean BCVA are shown in Fig. 1.
The mean preoperative IOP was 13.4 ± 5.2 mmHg (range 8–19). The intraocular pressures of all eyes remained within normal limits throughout the postoperative period (range 7–20 mmHg). There were no statistically significant changes in intraocular pressure on any measurement time in the postoperative period compared to preoperative IOP (for each one, p > 0.05). Serial changes in the mean IOP are shown in Fig. 2.
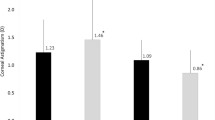
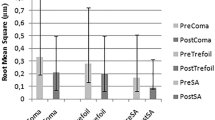
In addition, there were no statistically significant changes in the corneal refractive map, topometric map and zernike analysis of the subjects on any measurement time in the postoperative period compared to preoperatively (p > 0.05). No statistically significant changes were observed in the mean power of corneal astigmatism, mean keratometry, K 1 and K 2 values, corneal asphericity values, ISV, IVA, IHA, IHD and higher-order aberrations on the first week, first month and third month after the operation. Changes in corneal refractive map, topometric map and zernike analysis after 27-g MIVS are given in Tables 1, 2 and 3. The mean preoperative astigmatism of the frontal corneal surface was 0.91 ± 0.50 diopter (D). After the 27-g PPV, it was measured as 0.96 ± 0.68 D on the first week, 1.02 ± 0.73 D on the first month and 0.97 ± 0.42 D on the third month postoperatively (Fig. 3). Additionally, the mean surgically induced astigmatism was calculated as 0.23 ± 0.11 D on the first week, 0.19 ± 0.10 D on the first month and 0.19 ± 0.08 D on the third month postoperatively.
Discussion
In this present study, we evaluated the corneal topographic changes and surgically induced astigmatism after 27-g MIVS by using Pentacam HR-Scheimpflug imaging system. Although corneal topographic changes after 23-g and 25-g transconjunctival sutureless vitrectomy (TSV) have been reported, according to our knowledge, this is the first study that investigating the corneal topographic changes after 27-g MIVS.
The scleral incision in vitreoretinal surgery might affect the corneal curvature and can be an important factor in the visual outcome after the surgery [12]. Central corneal changes are the most important determinant for the optically formation of the macular image and in certain conditions may produce transitory severe refractive impairment of postoperative visual acuity [13]. Although Jampel et al. [12] regard the changes after PPV as slight and transitory, having little long-term clinical consequences, the patients’ visual acuity would be certainly impaired severely by induced changes in corneal shape that are both asymmetric and irregular. Rapid visual rehabilitation is important in patients with potentially good macular function undergoing vitreoretinal surgery, and knowledge of the postvitrectomy response would be useful in guiding postoperative management.
Surgically induced astigmatism after vitreoretinal surgery has been investigated in many clinical studies after 20-g conventional standard PPV [14–17]. Several authors have reported that the corneal contour is significantly changed after 20-g PPV, inducing surgically induced astigmatism [13, 16–19]. Wirbelauer et al. [13] investigated the changes of corneal shape after conventional PPV and reported a substantial increase in the corneal astigmatism and distinct shape changes in cornea after PPV in the immediate postoperative period. Similarly, Domniz et al. [16] evaluated the changes in corneal shape after conventional PPV by using videokeratography and showed that although the topographic indices were statistically significantly different from baseline at the 2 and 7 days postoperatively, these all indices returned to preoperative values by 1 month postoperatively and remained stable until the final follow-up at 3 months. Weinberger et al. [17] also used videokeratography to investigate the topographic changes of the cornea after 20-g PPV and found that the 20-g PPV induces radial steepening of the central cornea 1.2–1.6 D at 67° and 157°, corresponding to the scleral sutures, and after 3 months, the central cornea flattened in the same meridians, possibly owing to changes in scleral elasticity or loosening of the sutures. It was proposed that the increase in the postoperative astigmatism may be attributed to the scleral cautery and suturing at the entry port after 20-g PPV and the corneal alterations have returned to preoperative values by 1–3 months after the operation, possibly owing to changes in scleral elasticity or loosening of the sutures [16, 17].
Corneal topographic changes also investigated after 23-g and 25-g TSV [20, 21]. Yanyali et al. [22] evaluated the corneal topographic changes after 23-g TSV and revealed the mean surgically induced astigmatism was 0.67 ± 0.7 D at the first day, 0.36 ± 0.2 D at the first week and 0.33 ± 0.17 D at the first month postoperatively. Additionally, in their another study, they investigated those topographic changes after 25-g TSV and disclosed that there were no significant changes in average corneal power, corneal surface cylinder, surface asymmetry index and surface regularity index parameters at the first day, first week and first month after the operation [21]. They also assessed the mean induced astigmatism as 0.38 D at 15°. After this preliminary report, several investigators compared the corneal shape changes and induced astigmatism in 25-g TSV with the 20-g conventional standard PPV and showed that 25-g technique involves a statistically significant reduction in the amount of surgically induced astigmatism compared to 20-g PPV [23–25]. Similarly, Okomato et al. [26] investigated the changes in regular and irregular corneal astigmatism after the 25-g TSV and 20-g PPV and revealed that the 20-g PPV shows significantly greater surgically induced changes than the 25-g TSV for regular astigmatism, asymmetry and higher-order irregularity. They also concluded that 25-g TSV does not induce significant changes in corneal topography and exerts little influence on the optical quality of the cornea in the first postoperative month. Furthermore, Avitabile et al. [27] investigated the corneal shape changes after 25-g TSV and standard 20-g PPV and reported a significant difference in mean surgically induced astigmatism between the eyes that underwent standard 20-g PPV and 25-g TSV. Mean surgically induced astigmatism was reported as 0.8 D after 25-g TSV and 3.0 D after 20-g PPV at second postoperative day. They also suggested that the 25-g TSV system results in faster reduction in surgically induced keratometric astigmatism because of rapid cicatrization of the sclerotomy sites. In a recent study which compared the corneal topographic changes following PPV with the 23-g and 25-g TSV as well as the standard 20-g PPV, it was found that 23-g TSV and 25-g TSV do not induce corneal topographic parameters following surgery, whereas 20-g PPV was found to induce transient topographic corneal changes that had returned to preoperative levels at third month postoperatively [28]. Similarly, in our study no statistically significant changes were observed in the mean power of corneal astigmatism, keratometry, corneal asphericity value, ISV, IVA, IHA, IHD and higher-order aberrations on the first week, first month and third month after the operation. We excepted that if the 23-g and 25-g incisions do not affect the corneal contour and curvature, 27 g, which is about 0.40 mm and smaller than 23 g and 25 g, would not affect those corneal topographic parameters. Additionally, the amount of induced astigmatic changes in our study was about 0.23 D on the first week and 0.19 D on the first month, which are smaller than previously reported values following 25-g TVS surgeries. We also believe that since the reduction in the incision size and self-sealing incisions decrease the amount of surgically induced astigmatism and minor corneal topographic changes that were observed in the current study were thought to be attributable to small sclerotomies that were performed by the 27-g MIVS that allows for completely sutureless vitrectomy. In addition, none of the patients experienced any postoperative ocular hypotony since the 27-g incisions wound healing is expected to be excellent.
There are some shortcomings to our study. The primary limitation of this study is the lack of patients who underwent standard 20-g PPV, 23-g TSV and 25-g TSV. Indeed, a comparison of corneal topographic changes after 27-g MIVS with 23-g and 25-g TSV and 20-g standard PPV would reveal the differences between these four systems more clearly. The second limitation of the study is the modest sample size of the cohort, which may affect the validity of our conclusions and their significance.
In conclusion, to the best of our knowledge, this is the first study demonstrating insignificant changes in corneal refractive and topometric indices in the early postoperative period after 27-g MIVS. Thus, minor corneal surface and induced astigmatic changes are expected to result in rapid visual rehabilitation after PPV with the 27-g MIVS system.
References
Lakhanpal RR, Humayun MS, de Juan E, Jr LJ, Chong LP, Chang TS, Javaheri M, Fujii GY, Barnes AC, Alexandrou TJ (2005) Outcomes of 140 consecutive cases of 25-gauge transconjunctival surgery for posterior segment disease. Ophthalmology 112:817–824
Fabian ID, Moisseiev J (2011) Sutureless vitrectomy: evolution and current practices. Br J Ophthalmol 95:318–324
Spirn MJ (2009) Comparison of 25, 23 and 20-gauge vitrectomy. Curr Opin Ophthalmol 20:195–199
Thompson JT (2011) Advantages and limitations of small gauge vitrectomy. Surv Ophthalmol 56:162–172
Oshima Y, Wakabayashi T, Sato T, Ohji M, Tano Y (2010) A 27-gauge instrument system for transconjunctival sutureless microincision vitrectomy surgery. Ophthalmology 117:93–102
Toygar O, Mi CW, Miller DM, Riemann CD (2016) Outcomes of transconjunctival sutureless 27-gauge vitrectomy with silicone oil infusion. Graefes Arch Clin Exp Ophthalmol 254:2111–2118
Romano MR, Scotti F, Vinciguerra P (2015) 27-Gauge vitrectomy for primary rhegmatogenous retinal detachment: is it feasible? Ann Acad Med Singap 44:185–187
Khan MA, Rahimy E, Gupta OP, Hsu J (2016) Combined 27-gauge pars plana vitrectomy and scleral fixation of an Akreos AO60 intraocular lens using Gore-Tex suture. Retina 36:1602–1604
Khan MA, Shahlaee A, Toussaint B, Hsu J, Sivalingam A, Dugel PU, Lakhanpal RR, Riemann CD, Berrocal MH, Regillo CD, Ho AC (2016) Outcomes of 27 gauge microincision vitrectomy surgery for posterior segment disease. Am J Ophthalmol 161:36–43
Sternberg P Jr, Hatchell DL, Foulks GN, Landers MB 3rd (1985) The effect of silicone oil on the cornea. Arch Ophthalmol 103:90–94
Jaffe NS (1981) Postoperative corneal astigmatism. In: Jaffe NS (ed) Cataract surgery and its complications. Mosby, St Louis, pp 92–110
Jampel HD, Thompson JT, Nunez M, Michels RG (1987) Corneal astigmatic changes after pars plana vitrectomy. Retina 7:223–226
Wirbalauer C, Hoerauf H, Roider J, Laqua H (1998) Corneal shape changes after pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol 236:822–828
Yuen CY, Cheung BT, Tsang CW, Lam RF, Baig NB, Lam DS (2009) Surgically induced astigmatism in phacoemulsification, pars plana vitrectomy, and combined phacoemulsification and vitrectomy: a comparative study. Eye (Lond) 23:576–580
Park DH, Shin JP, Kim SY (2009) Surgically induced astigmatism in combined phacoemulsification and vitrectomy; 23-gauge transconjunctival sutureless vitrectomy versus 20-gauge standart vitrectomy. Graefes Arch Clin Exp Ophthalmol 247:1331–1337
Domniz YY, Cahana M, Avni I (2001) Corneal surface changes after pars plana vitrectomy and scleral buckling surgery. J Cataract Refract Surg 27:868–872
Weinberg D, Lichter H, Loya N, Axer-Siegel R, Muzmacher L, Gabbay U, Yassur Y (1999) Corneal topographic changes after retinal and vitreous surgery. Ophthalmology 106:1521–1524
Azar-Arevalo O, Arevalo JF (2001) Corneal topography changes after vitreoretinal surgery. Ophthalmic Surg Lasers 32:168–172
Slusher MM, Ford JG, Busbee B (2002) Clinically significant corneal astigmatism and pars plana vitrectomy. Ophthalmic Surg Lasers 33:5–8
Kim YK, Hyon JY, Woo SJ, Park KH, Yu YS, Chung H (2010) Surgically induced astigmatism after 23-gauge transconjunctival sutureless vitrectomy. Eye (Lond) 24:799–804
Yanyali A, Celik E, Horozoglu F, Nohutcu AF (2005) Corneal topographic changes after transconjunctival (25-gauge) sutureless vitrectomy. Am J Ophthalmol 140:939–941
Yanyali A, Horozoglu F, Macin A, Bozkurt KT, Aykut V, Acar BT, Nohutcu AF (2011) Corneal topographic changes after transconjunctival 23-gauge sutureless vitrectomy. Int Ophthalmol 31:277–282
Citirik M, Batman C, Bicer T, Zilelioglu O (2009) Keratometric alterations following the 25-gauge transconjunctival sutureless pars plana vitrectomy versus the conventional pars plana vitrectomy. Clin Exp Optom 92:416–420
de Paula AC, Nassaralla Júnior JJ, Rodrigues FW, da Silva RE, Correa e Silva RS, Barbosa Junior DR (2012) Alterations in the corneal topography after pars plana vitrectomy with the standard system of 20-gauge and the 25-gauge transconjunctival sutureless vitrectomy. Semin Ophthalmol 27:11–14
Galway G, Drury B, Cronin BG, Bourke RD (2010) A comparison of induced astigmatism in 20- vs 25-gauge vitrectomy procedures. Eye (Lond) 24:315–317
Okamoto F, Okamoto C, Sakata N, Hiratsuka K, Yamane N, Hiraoka T, Kaji Y, Oshika T (2007) Changes in corneal topography after 25-gauge transconjunctival sutureless vitrectomy versus after 20-gauge standard vitrectomy. Ophthalmology 114:2138–2141
Avitabile T, Castiglione F, Bonfiglio V, Castiglione F (2010) Transconjunctival sutureless 25-gauge versus 20-gauge standard vitrectomy: correlation between corneal topography and ultrasound biomicroscopy measurements of sclerotomy sites. Cornea 29:19–25
Grandinette AA, Kniggendorf V, Moreira LB, Moreira Junior CA, Moreira AT (2015) A comparison study of corneal topographic changes following 20-, 23-, and 25-G pars plana vitrectomy. Arq Bras Oftalmol 78:283–285
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Rights and permissions
About this article
Cite this article
Tekin, K., Sonmez, K., Inanc, M. et al. Evaluation of corneal topographic changes and surgically induced astigmatism after transconjunctival 27-gauge microincision vitrectomy surgery. Int Ophthalmol 38, 635–643 (2018). https://doi.org/10.1007/s10792-017-0507-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-017-0507-5