Abstract
Purpose
We describe cases of dislocation or subluxation of the WIOL-CF® polyfocal full-optics intraocular lens (IOL) and suggest a consistent pattern and possible mechanism for the IOL instability.
Methods
This is a retrospective case series of five consecutive eyes in three patients with WIOL-CF® IOL instability at Keimyung University Dongsan Medical Center and Kimkisan Eye Center from 2012 to 2014. The medical records and ocular exam data for these patients were analyzed.
Results
A 50-year-old male had uneventful phacoemulsification in both eyes with WIOL-CF® IOL implantation. At 27 months after surgery, the patient was referred to our clinic with a dislocated IOL in the left eye. The IOL in the right eye was dislocated in the same pattern 38 months after cataract surgery. Another 50-year-old male, who had phacoemulsification and WIOL-CF® IOL implantation in both eyes, was referred to our clinic following diagnosis of a subluxated IOL. Both IOLs were well centered; however, the infranasal aspect of the IOLs tilted posteriorly, and the supratemporal portion the IOLs tilted anteriorly, with overlying iris atrophy in a symmetric pattern. The inferonasal continuous curvilinear capsulorrhexis (CCC) edge was dragged superotemporally, and the supratemporal CCC edge was identified on the posterior surface of the IOL. A 16-year-old female had uneventful phacoemulsification and WIOL-CF® IOL implantation to treat a cataract in the right eye, and 3 years later, the IOL tilted with the same pattern as the previous case.
Conclusions
Years after uncomplicated phacoemulsification, an implanted WIOL-CF® IOL may tilt and dislocate in the absence of trauma, in a consistent and characteristic pattern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
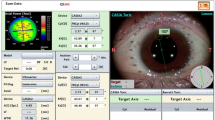
A conventional intraocular lens (IOL) implant is not able to accommodate like the human crystalline lens. To address this shortcoming, in recent years multifocal and accommodating IOLs have been designed and deployed [1, 2]. Among accommodative IOLs, the WIOL-CF® (Gelmed International, Kamenne Zehrovice, the Czech Republic) is a polyfocal, large-optic IOL without haptics, made of hydrogel (Wi-GEL). The WIOL-CF® was designed to be very similar to the human crystalline lens in shape and structure (Fig. 1) [3, 4]. This IOL is distributed throughout Asia, Europe, and Mexico.A The positional instability of the haptic-less WIOL-CF® in a previously vitrectomized eye, with IOL dislocation after neodymium-doped yttrium aluminum garnet (Nd:YAG) capsulotomy was described in a recent report [4].
In this series, we report three cases of WIOL-CF® IOL dislocation/subluxation without Nd:YAG capsulotomy, vitrectomy, or trauma in five eyes of three patients. None of the three patients had conditions predisposing to lens dislocation such as Marfan syndrome, high myopia, or pseudoexfoliation syndrome. We demonstrate a consistent pattern and possible mechanism for IOL instability, which were not fully outlined in the previous report.
Methods and materials
This report includes five consecutive eyes in three patients with WIOL-CF® IOL instability who presented to Keimyung University Dongsan Medical Center and Kimkisan Eye Center from 2012 to 2014. This study was approved by the Keimyung University Institutional Review Board.
No patient endorsed a history of glaucoma, retinal disorder, trauma, or ocular surgery other than uncomplicated phacoemulsification with IOL placement. The medical records and ocular exam data for these patients were analyzed.
Results
Patient 1
A 50-year-old male had uneventful phacoemulsification with WIOL-CF® implantation in each eye. At 27 months after the surgery, the patient was referred to our clinic complaining of a sudden decrease in vision in the left eye. At the time of admission, uncorrected visual acuity (UCVA) was right eye 20/20 and left eye 20/500; intraocular pressure (IOP) was 19 and 18 mmHg, respectively; manifest refraction was right eye +1.50 −1.75 ×90° and left eye +8.00 −0.50 D ×180°; best corrected visual acuity (BCVA) was 20/20 bilaterally. Slit-lamp and dilated fundus examinations in the right eye were normal with a well-centered IOL. Slit-lamp examination in the left eye revealed a relatively centered continuous curvilinear capsulorrhexis (CCC) and a large break in the posterior capsule (PC), which was the presumed route of IOL dislocation (Fig. 2a). A dislocated IOL was identified during fundus examination of the left eye. Pars plana vitrectomy, removal of the dislocated WIOL-CF®, and secondary implantation of three-piece IOL into the sulcus were performed (Video 1).
The IOL in the right eye subsequently dislocated in the same pattern 38 months after the cataract surgery (Fig. 2b).
Patient 2
A 50-year-old male had uneventful phacoemulsification and WIOL-CF® IOL implantation in each eye. The patient was referred to our clinic one year after the surgery following a diagnosis of decreased visual acuity and ocular pain in the left eye with a subluxated IOL in the left eye. UCVA was right eye 20/30 and left eye 20/80; IOP was 18 and 15 mmHg, respectively; manifest refraction was right eye –0.75 −0.75 ×180° and left eye −1.75 −3.00 ×180°; BCVA was right eye 20/20 and left eye 20/80.
In the left eye, the IOL was well centered on slit-lamp examination; however, the inferior portion vaulted posteriorly, and vitreous had prolapsed into the anterior chamber, while the supratemporal portion of the IOL tilted anteriorly. There was mid-peripheral iris atrophy with pigment on the anterior surface of the IOL. The inferonasal CCC edge was dragged superotemporally and located nearly at the center of the IOL with a wrinkled anterior capsule, and the supratemporal CCC margin was identified on the posterior surface of the IOL (Fig. 3a, b).
Slit-lamp photographs of patient 2 (a, b, left eye; c, d, right eye). a The intraocular lens (IOL) was located centrally, but the infranasal part tilted posteriorly through which vitreous (stars) was prolapsed into the anterior chamber and the supratemporal portion tilted anteriorly. The continuous curvilinear capsulorrhexis (CCC) margin (arrows) was dragged superotemporally and located at the center of the IOL with the wrinkled anterior capsule (arrow heads). b The CCC margin (arrows) was dragged superotemporally and located at the center, and the supratemporal iris was atrophied (arrow heads). c The IOL was tilted, and supratemporal portion protruded with iris atrophy (arrow heads). The infranasal portion moved backward without prolapsed vitreous. The CCC margin (red arrows) was dragged superotemporally with wrinkles (stars), and the supratemporal CCC (white arrows) margin on the posterior surface of the IOL was identified. Schematic cross-section image along A–B is shown in (Fig. 5a–c). d The CCC margin (arrows) was dragged superotemporally with wrinkles (stars), and the tilted capsular bag with suspected zonular weakness (arrow heads) was apparent
The patient visited our clinic 6 months later for decreased vision in the right eye, one month after initiating a topical ocular hypotensive. The BCVA in the right eye had decreased to 20/40; manifest refraction was +1.00 −2.75 ×180°; Intraocualr pressure was 16 and 21 mmHg, respectively. The IOL in the right eye tilted in the same symmetrical pattern, though without prolapsed vitreous. The supratemporal portion of the IOL vaulted anteriorly with corresponding iris atrophy and the infranasal portion of the IOL tilted posteriorly (Fig. 3c, d).
The WIOL-CF® IOL was removed without rupturing the posterior capsule. A conventional IOL was implanted in the bag following insertion of a capsular tension ring due to inferonasal zonular dialysis (Video 2).
Patient 3
A 16-year old female with insulin-dependent diabetes mellitus had uneventful phacoemulsification and WIOL-CF® IOL implantation in the right eye three years prior to presentation. She had recently developed decreased visual acuity and ocular discomfort in the right eye. The BCVA in the right eye had decreased to 20/60; manifest refraction was plano −2.50 ×180° with no improvement in acuity. The IOL in the right eye was tilted with prolapsed vitreous. The supratemporal portion of the IOL tilted anteriorly, with corresponding iris atrophy, and the infranasal part had tilted posteriorly. The infranasal CCC edge was dragged to the center of the optic, while the superotemporal IOL edge had escaped out of the capsular bag (Fig. 4). There were no fundus abnormalities. The patient underwent pars plana vitrectomy with IOL and capsular bag explantation, followed by scleral fixation of a three-piece IOL.
Discussion
The WIOL-CF® is a unique IOL without haptics, which requires adhesion between the lens and the anterior and posterior capsules to fixate the IOL in the capsular bag. Although the IOL adheres to the lens capsule both anteriorly and posteriorly, the strength of these bonds is presumed not to be strong enough to prevent subluxation [5–7]. A previous report mentioned positional instability of WIOL-CF® in a previously vitrectomized eye; however, that study did not describe IOL tilt and escape of the superotemporal optic from the capsular bag. A cogent mechanism of IOL tilt leading to dislocation was not explored as Nd:YAG capsulotomy provided a ready explanation for the dislocation of the haptic-less IOL [4].
This report reveals that the WIOL-CF® polyfocal full-optics IOL can tilt and dislocate without trauma in a distinctive pattern. Each time the WIOL-CF® tilted, the infranasal portion of the IOL tilted posteriorly, while the supratemporal portion tilted anteriorly. In conjunction with IOL subluxation, the infranasal CCC edge was dragged supratemporally, and the supratemporal CCC edge was located on the posterior surface of the IOL. In the case where the IOL dislocated into the posterior segment, it dislocated through a PC rupture with a centered CCC. This characteristic morphological pattern is consistent with a previous report [4]. Analyzing these features can help answer the question regarding how the IOL could be centered in the pupil even in situations where the infranasal CCC edge was pulled up to the center of the pupil, and explains the process of tilt and progression to dislocation.
The suggested progression process is as follows (Video 3). First, the supratemporal part of the IOL tilts forward and downward, and the infranasal part tilts backward and upward. The forward tilting supratemporal IOL margin comes out of the capsular bag and the corresponding CCC margin is located behind the IOL, which is why the supratemporal CCC margin was identified on the posterior surface of the IOL (Fig. 5a). Then, the IOL becomes more tilted to make contact with the adjacent iris and chafe it, which explains the supratemporal iris atrophy. The backward tilting infranasal IOL margin slides backward from the capsular bag equator to the posterior capsule, stretching the capsule, which explains why the inferonasal CCC margin is dragged superotemporally with a wrinkle and is located at the center of IOL. At some stage, presumably because the iris acts as a barrier to IOL tilt, the progression of IOL tilt slows, and then the tilted IOL margin chafes the iris supratemporally, and stretches and ultimately causes a rent in the PC inferonasally (Fig. 5b). Iris chafing can cause iris atrophy, pigment dispersion, and secondary glaucoma, and chronic stretching of the PC may stretch and loosen the adjacent zonules to induce vitreous prolapse or a PC rupture inferonasally. After the IOL dislocates from the capsular bag into the posterior segment, the dragged and displaced CCC margin returns to its normal position, though with the possibility of infranasal zonular dialysis (Fig. 5c). Although the current cases did not show that tiling the IOL progresses to IOL dislocation, a previous report revealed serial progression from IOL tilt to dislocation with the same morphological pattern; therefore, it is assumed that IOL tilt can progress to IOL dislocation.
Schematic drawing demonstrating cross-section along a–b shown in (Fig. 3c). a The forward tilting supratemporal intraocular lens (IOL) margin (star) comes out of the capsular bag, and the continuous curvilinear capsulorrhexis (CCC) margin becomes located behind the IOL (arrow head). b As the IOL tilts forward and downward, the tilted IOL chafes the iris (star) and stretches the inferior posterior capsule (arrows) and the zonules (arrow head). c Dislocated IOL (star) in the vitreous cavity through the ruptured inferior posterior capsule, and the CCC margin returned to the normal position (arrow)
The cataract extractions described in the above cases were performed by two experienced surgeons, in eyes without prior trauma or predisposition to zonular incompetence. There were no intra- or perioperative complications in any of the cases, until the patients became symptomatic with late tilt and dislocation. As such, we may conclude that the full-optic IOL is vulnerable to positional instability. Its lack of haptics allows for tilting, displacement of the IOL from its centered position between the anterior and posterior capsules, and ultimately dislocation through an induced posterior capsule tear. In the past, the original Ridley lens implanted in the sulcus was also a haptic-less, full-optic IOL, and complications such as anterior uveitis and IOL decentration were frequent because of the IOL’s heavy weight, thickness, and design [8, 9]. After 1975, when Shearing introduced polypropylene haptics designed for capsular bag insertion, the full-optic IOL fell into disuse until its reintroduction with the WIOL-CF® [9, 10].
Although we have described the serial progression of WIOL-CF® IOL instability, questions remain. What induces the IOL to begin tilting, why does it tilt along the same infranasal to supratemporal axis, and how can the problem be overcome? Perhaps the ciliary muscles exert forces along this same axis during accommodation, which over time overcomes the IOLs adhesion to the anterior and posterior capsules, setting the process of induced instability in motion.
In conclusion, WIOL-CF® polyfocal full-optics IOL may tilt and dislocate in the absence of trauma, and the process has a consistent and characteristic pattern.
References
Vanderschueren I, Zeyen T, D’Heer B (1991) Multifocal IOL implantation: 16 cases. Br J Ophthalmol 75(2):88–91
Sen HN, Sarikkola AU, Uusitalo RJ, Laatikainen L (2004) Quality of vision after AMO Array multifocal intraocular lens implantation. J Cataract Refract Surg 30(12):2483–2493. doi:10.1016/j.jcrs.2004.04.049
Kim HJ, Seo JW, Shin SJ, Chung SK (2011) Visual outcome and stability of hydrogel full-optics accommodative intraocular lens. J Korean Ophthalmol Soc 52(12):1448–1454. doi:10.3341/jkos.2011.52.12.1448
Kang KT, Kim YC (2013) Dislocation of polyfocal full-optics accommodative intraocular lens after neodymium-doped yttrium aluminum garnet capsulotomy in vitrectomized eye. Indian J Ophthalmol 61(11):678–680. doi:10.4103/0301-4738.119335
Liu CS, Wormstone IM, Duncan G, Marcantonio JM, Webb SF, Davies PD (1996) A study of human lens cell growth in vitro. A model for posterior capsule opacification. Invest Ophthalmol Vis Sci 37(5):906–914
Ishibashi T, Hatae T, Inomata H (1994) Collagen types in human posterior capsule opacification. J Cataract Refract Surg 20(6):643–646
Nagamoto T, Tanaka N, Fujiwara T (2009) Inhibition of posterior capsule opacification by a capsular adhesion-preventing ring. Arch Ophthalmol 127(4):471–474. doi:10.1001/archophthalmol.2009.63
Ridley H (1957) Intra-ocular acrylic lens. Trans Ophthalmol Soc UK 71:617–621
Williams HP (2001) Sir Harold Ridley’s vision. Br J Ophthalmol 85(9):1022–1023
Shearing S (1979) Mechanism of fixation of the Shearing posterior chamber intra-ocular lens. Contact Intraocul Lens Med J 5:74–77
Funding
There was no financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 86136 kb)
Supplementary material 2 (MP4 116694 kb)
Supplementary material 3 (MP4 73275 kb)
Rights and permissions
About this article
Cite this article
Kim, Y.C., Kang, K.T., Yeo, Y. et al. Consistent pattern in positional instability of polyfocal full-optics accommodative IOL. Int Ophthalmol 37, 1299–1304 (2017). https://doi.org/10.1007/s10792-016-0398-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-016-0398-x