Abstract
The purpose of this study was to compare the keratometry (K) values obtained by the Scheimpflug camera combined with placido-disk corneal topography (Sirius) and optical biometry (Lenstar) for intraocular lens (IOL) power calculation before the cataract surgery, and to evaluate the accuracy of postoperative refraction. 50 eyes of 40 patients were scheduled to have phacoemulsification with the implantation of a posterior chamber intraocular lens. The IOL power was calculated using the SRK/T formula with Lenstar K and K readings from Sirius. Simulated K (SimK), K at 3-, 5-, and 7-mm zones from Sirius were compared with Lenstar K readings. The accuracy of these parameters was determined by calculating the mean absolute error (MAE). The mean Lenstar K value was 44.05 diopters (D) ±1.93 (SD) and SimK, K at 3-, 5-, and 7-mm zones were 43.85 ± 1.91, 43.88 ± 1.9, 43.84 ± 1.9, 43.66 ± 1.85 D, respectively. There was no statistically significant difference between the K readings (P = 0.901). When Lenstar was used for the corneal power measurements, MAE was 0.42 ± 0.33 D, but when simK of Sirius was used, it was 0.37 ± 0.32 D (the lowest MAE (0.36 ± 0.32 D) was achieved as a result of 5 mm K measurement), but it was not statistically significant (P = 0.892). Of all the K readings of Sirius and Lenstar, Sirius 5-mm zone K readings were the best in predicting a more precise IOL power. The corneal power measurements with the Scheimpflug camera combined with placido-disk corneal topography can be safely used for IOL power calculation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Nowadays, cataract surgery not only focuses on visual improvement, but also it is considered as a form of refractive surgery. Final refractive outcomes are important for the success of cataract surgery. Intraocular lens (IOL) power calculation is the first step in preoperative examination to reach the target refraction [1]. Corneal power measurement is required to calculate the IOL power to be implanted at the time of surgery. With the improvement in technology, there have been many devices to measure the corneal power. It can be measured by manual and automated keratometry, placido-disk corneal topography with and without Scheimpflug camera imaging, and optical biometry [2–4].
The use of the rotating Scheimpflug camera to measure the corneal power has some advantages over the placido-disk corneal topography. Scheimpflug camera can measure the central corneal curvature and posterior cornea. Theoretically, this may lead to improved accuracy in IOL power calculation. However, the reports comparing the keratometric values of Scheimpflug camera (Pentacam, Oculus, Inc.) and placido-disk corneal topography (Keratron) gave similar results [5, 6]. The reports that compare the Scheimpflug corneal topography (Pentacam) and optical biometry (IOL Master, Carl Zeiss Meditec) also gave similar results [7]. On the other hand, Shirayama et al. [8] did not find a statistically significant difference between the dual Scheimpflug analyzer and a placido-disk-based corneal topographer in measuring corneal power. On the accuracy of IOL power calculation, the combined topography systems need further investigation.
The purpose of this prospective study was to compare the corneal power measurements of the Scheimpflug camera combined with placido-disk corneal topography (Sirius, CSO Inc, Florence, Italy) and optical biometry (Lenstar LS 900, Haag-Streit AG, Koeniz, Switzerland), and to evaluate the accuracy of IOL power calculation.
Patients and methods
This prospective observational study comprised 50 eyes of 40 patients scheduled for a cataract surgery between June 2014 and January 2015. Each patient was informed about the study and given written consent. The study was approved by the ethics committee of the Bagcilar Training and Research Hospital and the methods adhered to the tenets of the Declaration of Helsinki.
Preoperatively, all patients had a full ophthalmic examination, including visual acuity, Goldmann applanation tonometry, and slit lamp biomicroscopy. Patients with corneal abnormality, previous refractive surgery, and dense cataract were excluded. Keratometry was measured with optical biometry device (Lenstar LS 900, Haag-Streit AG, Koeniz, Switzerland) as well as corneal topography (Sirius, CSO Inc, Florence, Italy). Three measurements were performed with each device. In the case of low reproducibility, the measurements were repeated. The good quality outputs were used for further analysis.
For the IOL power calculation, the measurements of optical biometry device were used including axial length (AL) and keratometry. The IOL power calculations were performed using the same formula SRK/T based on the current Royal College guidelines [26]. Only the eyes with AL between 22.0 mm and 24.5 mm were included in the study to eliminate the errors according to the different formulas. For comparative purposes, corneal power was also measured with Sirius.
All surgeries were performed by the same surgeon (A.K) using a 2.8-mm clear corneal incision. An acrylic IOL (Acriva UD 613, Istanbul, Turkey) was placed in the capsular bag in all cases. A final evaluation was performed by assessing the subjective refractive outcomes, one month postoperatively, which is when the refractive stability can be expected with small-incision clear corneal surgery. To calculate the mean absolute error (MAE), the measured manifest refractive spherical equivalent was subtracted from the predicted refraction (based on the IOL actually implanted) according to the SRK/T formula. MAE was used for statistical comparisons.
Statistical analysis was performed using SPSS for Windows software (version 21.0, SPSS, Inc, Chicago, Illinois, USA). In the present study, unless otherwise indicated, all data were expressed as the mean ± SD. Normality was checked using the Kolmogorov–Smirnov test. Repeated-measures analysis of variance (ANOVA) was used to compare mean values of corneal power measurements and MAEs. Reliability was determined by calculating the intraclass correlation coefficient (ICC) at % 95 confidence interval, and the limits of agreement by the method of Bland and Altman. The means and 95 % limits of agreement (LoA) were calculated using this method. A P value less than 0.05 was considered statistically significant.
Results
Fifty eyes of 40 patients (22 men, 18 women) were enrolled in the study. The mean age of the patients was 63.1 ± 9.8 (37–80 years). The mean AL was 23.45 ± 0.74 mm (22.0–24.48 mm).
The mean Lenstar K value was 44.05 diopters (D) ±1.93 and the K readings of the topography; SimK, K at 3-, 5-, and 7-mm zones were 43.85 ± 1.91, 43.88 ± 1.9, 43.84 ± 1.9, 43.66 ± 1.85 D, respectively. There was not any statistically significant difference between the K readings. (P = 0.901) (Table 1). The K values of optical biometry and the simK, K values at 3-, 5-, and 7-mm zones of the topography, were significantly correlated and showed a high interclass correlation as shown in Table 2.
Although the MAE obtained from K readings at 5-mm zone showed a trend toward better refractive outcomes (0.36 ± 0.32 D), there was no statistically significant difference between the MAEs obtained with the optic biometry and the topography parameters (P = 0.892) (Table 1). The MAEs of the optical biometry and the simK, K at 3-, 5-, and 7-mm zones of the topography, were significantly correlated and showed a high interclass correlation as shown in Table 2.
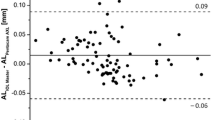
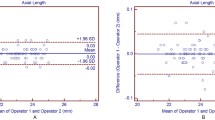
Figure 1 shows a Bland–Altman plot comparing MAE of the optical biometry to MAE of simK, K at 3-, 5-, and 7-mm zones of the topography. There is a high correlation between the methods: (a) MAE of the optical biometry and simK of the topography, with a mean value of 0.14 and a 95 % LoA ranging between 0.55 and −0.26; (b) MAE of the optical biometry and the topography Kat 3 mm, with a mean value of 0.11 and 95 % LoA ranging between 0.53 and −0.31; (c) MAE of the optical biometry and the topography at 5 mm, with a mean value of 0.15 and 95 % LoA ranging between 0.57 and −0.27; and (d) MAE of the optical biometry and the topography at 7 mm, with a mean value of 0.20 and 95 % LoA ranging between 0.73 and −0.34.
Discussion
Our study shows that the corneal power measurements provided by Sirius, a Scheimpflug camera combined with placido-disk corneal topography, can be successfully used for IOL power calculation to achieve the target refraction. The results obtained with the simK, K at 3-, 5-, and 7-mm zones (MAE ranging between 0.36 ± 0.32 and 0.39 ± 0.32 D), were better than those achieved by Lenstar K (0.42 ± 0.33 D), an optical biometry. Although there was no statistically significant difference, K at 5-mm zone gave the better refractive outcome.
Accurate IOL power calculation is the most important point for better visual outcome after cataract surgery. According to Norrby [9], one of the major sources of error in IOL power calculation is keratometry which contributes to the 6 % of total errors. There are many devices that measure the corneal power [10]. The accuracy of Scheimpflug camera on IOL power calculation was evaluated in some studies. Savini et al. [11] reported that the corneal power measurements with Scheimpflug-based corneal topography should be used for IOL power calculation. Shammas et al. [12] compared the K values obtained with an auto keratometer and corneal topograph with Scheimpflug imaging and found that the K values from Scheimpflug photography did not improve accuracy over auto keratometer values. However, Saad et al. [7] compared the K values of the corneal topography and optical biometry and found slightly better results with Scheimpflug images. On the other hand, the accuracy of Scheimpflug camera over placido-disk corneal topography was also evaluated, and they displayed comparable accuracy in IOL power calculation [5].
Scheimpflug camera combined with placido-disk corneal topography system, as we used in our study, provides tangential and axial curvature data of the anterior and posterior corneal surfaces and the global refractive power of the cornea [13]. In our study, K readings of the topography, especially K at 5-mm zone, gave the lowest MAE. These findings reveal that dual topography system seems to give more accurate results for IOL power calculation. Given the findings of the present study, it can be said that the addition of a placido-disk topographer increases the accuracy of the anterior corneal curvature measurements provided by the Scheimpflug cameras. Similarly, Savini et al. [14] compared dual Scheimpflug analyzer and a corneal topography system for IOL power calculation and reported that dual Scheimpflug camera can lead to excellent results for IOL power prediction. The same group also reported the high accuracy of Sirius device over the corneal topographer for IOL power calculation in another study [15].
Since the AL measurement is one of the crucial steps for IOL power calculation, the use of optical biometry provided us a high precision in our study. Although in the previous studies ultrasound (US) immersion biometry was used for the AL measurement, we preferred Lenstar [11, 15, 16]. Comparison of refractive outcomes using optical biometry and US immersion biometry was evaluated in many studies and similar results were found [17–19]. MAE in IOL power prediction has been shown to be small with Lenstar when compared with US immersion biometry [20]. Similarly, Cruysberg et al. [21] reported that the reproducibility of Lenstar was excellent and found the AL measurement and IOL power calculation comparable with the other devices. It should be emphasized that an important factor for using optical biometry is to avoid eyes with dense cataract or in cases of fixation instability, as we did in our study.
We used one of the third generation formulas, SRK/T, for IOL power calculation [22]. In eyes with medium AL, IOL power prediction results have varied depending on the formula, but in many studies, SRK/T formula was recommended for these eyes [16, 23, 24]. A previous study also showed that the use of SRK/T formula with Scheimpflug imaging gave accurate refractive outcomes [25].
The relatively small sample size is one of the limitations of our study. Another limitation is that we selected the patients with particular AL, and we did not use other formulas for calculating the IOL power. Finally, we did not evaluate the patients for dry eye and unstable tear film, which can disrupt the quality of Scheimpflug imaging.
Conclusion
In conclusion, the Sirius 5-mm zone K readings were the best in predicting a more precise IOL power among the other K readings of Sirius and Lenstar. Additionally, our study shows the performances of a new material namely the Sirius and gives similar results gained in different studies providing the different keratometry results. The corneal power measurements with Scheimpflug camera combined with placido-disk corneal topography can be safely used for IOL power calculation and have comparable accuracy on postoperative refraction.
References
Olsen T (2007) Calculation of intraocular lens power: a review. Acta Ophthalmol Scand 85:472–485
Lopez de la Fuente C, Sanchez-Cano A, Segura F, Fuentes-Bruto L, Pinilla I (2014) Repeatability of ocular measurements with a dual-Scheimpflug analyzer in healthy eyes. Biomed Res Int. doi:10.1155/2014/808646
Wang L, Shirayama M, Koch DD (2010) Repeatability of corneal power and wavefront aberration measurements with a dual-Scheimpflug placido corneal topographer. J Cataract Refract Surg 36:425–430
Verhulst E, Vrijghem JC (2001) Accuracy of intraocular lens power calculations using the Zeiss IOL master. A prospective study. Bull Soc Belge Ophthalmol 281:61–65
Savini G, Barboni P, Carbonelli M, Hoffer KJ (2013) Comparison of methods to measure corneal power for intraocular lens power calculation using a rotating Scheimpflug camera. J Cataract Refract Surg 39:598–604
Kawamorita T, Nakayama N, Uozato H (2009) Repeatability and reproducibility of corneal curvature measurements using the Pentacam and the Keratron topography systems. J Refract Surg 25:539–544
Saad E, Shammas MC, Shammas HJ (2013) Scheimpflug corneal power measurements for intraocular lens power calculation in cataract surgery. Am J Ophthalmol 156:460–467
Shirayama M, Wang L, Koch DD, Weikert MP (2010) Comparison of accuracy of intraocular lens calculations using automated keratometry, a placido-based corneal topographer, and a combined placido-based and dual Scheimpflug corneal topographer. Cornea 29:1136–1138
Norrby S (2008) Sources of error in intraocular lens power calculation. J Cataract Refract Surg 34:368–376
Elbaz U, Barkana Y, Gerber Y, Avni I, Zadok D (2007) Comparison of different techniques of anterior chamber depth and keratometric measurements. Am J Ophthalmol 143:48–53
Savini G, Barboni P, Carbonelli M, Hoffer KJ (2009) Accuracy of Scheimpflug corneal power measurements for intraocular lens power calculation. J Cataract Refract Surg 35:1193–1197
Shammas HJ, Hoffer KJ, Shammas MC (2009) Scheimpflug photography keratometry readings for routine intraocular lens power calculation. J Cataract Refract Surg 35:330–334
Akçay BIS, Ozgurhan EB, Bozkurt B, Kurt T, Yıldırım Y, Cosar MG et al (2014) Evaluation of pachymetric measurements with Scheimpflug photography-based system and optical coherence tomography pachymetry at different stages of keratoconus. J Ophthalmol 2014:719205. doi:10.1155/2014/719205
Savini G, Barboni P, Carbonelli M, Hoffer KJ (2011) Accuracy of a dual Scheimpflug analyzer and a corneal topography system for intraocular lens power calculation in unoperated eyes. J Cataract Refract Surg 37:72–76
Savini G, Barboni P, Carbonelli M, Hoffer KJ (2012) Accuracy of corneal power measurements by a new Scheimpflug camera combined with placido-disc corneal topography for intraocular lens power calculation in unoperated eyes. J Cataract Refract Surg 38:787–792
Narvaez J, Zimmerman G, Stulting RD, Chang DH (2006) Accuracy of intraocular lens power prediction using the Hoffer Q, Holladay 1, Holladay 2 and SRK/T formulas. J Cataract Refract Surg 32:2050–2053
BjelošRončević M, Bušić M, Cima I, KuzmanovićElabjer B, Bosnar D, Miletić D (2011) Comparison of optical low-coherence reflectometry and applanation ultrasound biometry on intraocular lens power calculation. Graefes Arch Clin Exp Ophthalmol. 249:69–75
Rajan MS, Keilhorn I, Bell JA (2002) Partial coherence laser interferometry vs conventional ultrasound biometry in intraocular lens power calculations. Eye 16:552–556
Landers J, Goggin M (2009) Comparison of refractive outcomes using immersion ultrasound biometry and IOL master biometry. Clin Exp Ophthalmol 37:566–569
Jasvinder S, Khang TF, Sarinder KKS, Loo VP, Subrayan V (2011) Agreement analysis of LENSTAR with other techniques of biometry. Eye 25:717–724
Cruysberg LPJ, Doors M, Verbakel F, Berendschot TT, De Brabander J, Nuijts RM (2010) Evaluation of the Lenstar LS 900 all-in-one non contact biometry meter. Br J Ophthalmol 94:106–110
Retzlaff JA, Sanders DR, Kraff MC (1990) Development of the SRK/T intraocular lens power calculation formula. J Cataract Refract Surg 16:333–340
Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL (2011) Formula choice: Hoffer Q, Holladay 1, or SRK/T and refractive outcomes in 8108 eyes after cataract surgery with biometry bypartial coherence interferometry. J Cataract Refract Surg 37:63–71
Wang JK, Chang SW (2013) Optical biometry intraocular lens power calculation using different formulas in patients with different axial lengths. Int J Opthalmol 6:150–154
Miyata K, Otani S, Honbou N, Minami K (2013) Use of Scheimpflug corneal anterior–posterior imaging in ray-tracing intraocular lens power calculation. Acta Ophthalmol. 91:546–549
Other cited material
Royal College of Ophthalmologists. Cataract Surgery Guidelines, London, UK, The Royal College of Ophthalmologists 2010. http://www.rcophth.ac.uk/standards-publications-research/clinical-guidelines/Accessed Accessed 6 Mar 2012
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kirgiz, A., Atalay, K., Kaldirim, H. et al. Scheimpflug camera combined with placido-disk corneal topography and optical biometry for intraocular lens power calculation. Int Ophthalmol 37, 781–786 (2017). https://doi.org/10.1007/s10792-016-0330-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-016-0330-4