Abstract
The purpose of this study was to investigate the efficacy and safety of the Toris K silicone hydrogel contact lens (SwissLens; Prilly, Switzerland) in keratoconus patients. A database with information on 50 keratoconus patients (64 eyes) fitted with Toris K soft contact lenses over a 2-year period was retrospectively reviewed. Demographic data, prefitting refraction, the reason for choosing the Toris K soft contact lens, uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BSCVA), best-corrected visual acuity with a rigid gas permeable lens (BCVA RGP), best-corrected visual acuity with the Toris K lens (BCVA Toris K), and complications were evaluated. The mean age ± standard deviation at the time of fitting was 27.92 ± 9.86 years. The mean spherical refractive power was −4.62 ± 6.53 dioptres, and the mean cylinder was −3.78 ± 2.43 dioptres. The most common reason for using Toris K soft contact lenses was an inability to fit the patient with a RGP contact lens. There was a statistically significant difference between UCVA and BCVA Toris K (p = 0.0001), as well as between BSCVA and BCVA Toris K (p = 0.0001). However, there was no statistically significant difference between BCVA Toris K and BCVA RGP (p = 0.20). Superficial punctate keratitis and giant papillary conjunctivitis were the most common complications. The Toris K contact lens is a viable alternative for the optical management of all grades of keratoconus. The Toris K soft contact lens is a promising alternative for the visual rehabilitation of keratoconus patients who cannot tolerate RGP lenses or achieve a good fit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Keratoconus is a progressive noninflammatory disease of the cornea characterized by corneal thinning and ectasia that affects the refractive power of the cornea, resulting in irregular myopic astigmatism [1–3]. The optical correction of keratoconus is a challenging problem because of the abnormal curvature and advancing corneal ectasia [1, 2].
In mild cases of keratoconus, spectacles can be used to help correct vision; however, contact lenses are required for moderate and advanced disease. Many different types of contact lenses are available for keratoconus, such as rigid gas permeable (RGP) contact lenses, intralimbal lenses, scleral lenses, piggyback lenses, hybrid contact lenses, soft lenses, and soft toric lenses [4].
RGP contact lenses are the standard treatment for irregular astigmatism in keratoconus. However, some patients cannot tolerate these lenses because of discomfort. Other patients, particularly those with very steep and/or irregular corneas, experience frequent lens dislocation and decentration [5, 6]. The mechanical interaction of a rigid lens with the corneal surface leads to corneal micro-trauma, epithelial and anterior stroma disruptions, and consequent ocular inflammation [7–9]. Scleral lenses completely clear the corneal surface, provide good centration, and stabilize visual acuity but are associated with worse tear exchange and increased difficulty in application and removal [4]. Hybrid lenses have been associated with oedema, decreased endothelial cell density, increased risk of neovascularization, and other issues regarding resistance to lens handling [10, 11]. Conversely, piggyback systems seem to be effective and have been shown to provide sufficient oxygen to fulfil corneal needs during daily wear, even when conventional lenses are used. However, handling and cleaning 2 different lenses are major inconveniences for many patients [12].
Soft lenses and soft toric lenses may be indicated in early keratoconus, decentred keratoconus, and cases involving RGP contact lens intolerance. The advantages of soft conventional contact lenses include greater comfort and lower cost for noncustom lenses. The disadvantages include low oxygen permeability if the lens is not a silicone hydrogel (SiH) and the inability to mask moderate-to-severe irregular astigmatism [4].
The Toris K soft keratoconus contact lens (SwissLens, Prilly, Switzerland) is a newly designed type of SiH lens with a toric front surface. Both spherical and cylindrical corrections are added to the toric surface of the lens to increase the visual performance. The main purpose of this study was to evaluate the safety and efficacy of the Toris K SiH contact lens for the optical management of patients with keratoconus and patients who underwent penetrating keratoplasty. The second purpose was to compare the optical performances of Toris K SiH contact lenses and RGP contact lenses.
Methods
Clinical data from the records of 50 patients (64 eyes) fitted with Toris K soft contact lenses for visual rehabilitation during the 2-year period between November 2012 and December 2014 at the Contact Lens Unit of the Cerrahpasa Medical Faculty, Department of Ophthalmology were retrospectively analysed. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Istanbul University, Cerrahpasa Medical Faculty, Istanbul, Turkey.
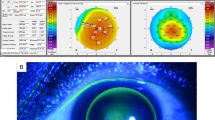
The inclusion criterion was a diagnosis of keratoconus in 1 or both eyes by an ophthalmologist. Keratoconus was diagnosed based on clinical signs of irregular keratometric mires, scissoring of the retinoscopic reflex or irregularity in the red reflex as detected by direct ophthalmoscope, and refractive findings; and biomicroscopic signs such as Vogt’s striae, Fleischer’s ring, Rizutti’s sign, stromal thinning, and apical corneal scarring. Corneal topography was also used in the diagnosis [13].
The collected patient data included sex, date of birth, ocular diagnosis, history of surgeries, manifest refraction, and indication for Toris K soft contact lens fitting. Corneal topographic analyses using the Pentacam HR Eye Scanner (Oculus, Inc., Wetzlar, Germany) were performed. The patients’ previous visual acuities, methods of correction (spectacles, RGP lenses, or Toris K soft contact lenses), and visual acuities after visual rehabilitation were noted. Visual acuity was measured using Snellen charts. All visual acuity measurements were performed by the same practitioner under standard photopic luminance conditions in the same examination room. A statistical analysis of visual acuity was performed after converting the measurements to the logarithm of the minimum angle of resolution (logMAR).
The topographic variables, thinnest corneal thickness, mean astigmatism, axis of astigmatism, mean radius of the anterior corneal curvature (Rm), and mean keratometric values (Km) were recorded using a Pentacam system. The mean radius of the corneal curvature (Rm), mean astigmatism, and axis of astigmatism were also measured and recorded using manual keratometry (Javal-Schoitz keratometer).
There is no generally accepted classification system for keratoconus, but one of the most commonly used is the Amsler-Krumeich classification, which is based on the patient’s mean keratometry readings on the anterior curvature sagittal map, thickness at the thinnest location, corneal opacities, and refractive error [14]. This classification was used in the present study.
The reasons for discontinuing spectacles or RGP contact lenses and for selecting Toris K soft lenses were noted and analysed. These reasons were RGP lens intolerance, inability to fit the patient with an RGP lens, and patient preference (refusal to wear spectacles or RGP lenses).
Subjective complaints included discomfort and unsatisfactory vision. Objective complications included giant papillary conjunctivitis, superficial punctate keratitis, corneal epithelial defects or abrasions, pannus or neovascularization, corneal oedema, corneal ulcers, and contact lens damage. The management and outcomes of complications were also reviewed.
All patients were fitted with Toris K soft keratoconus contact lenses. Table 1 shows the technical parameters of the Toris K soft contact lenses, as indicated by the manufacturer [15]. The initial trial lens was selected according to the protocol as described. The first step was to choose the lens to be applied based on topographic indications. The Toris K12 was chosen for keratoconus grades 1–2, and the Toris K34 was chosen for keratoconus grades 3–4. The first trial lens was used to validate the base curve and diameter. Dynamic stabilization marks are needed to measure the stabilization axis. Lens stabilization and movement were assessed 30 min after lens fitting. The final cylinder corresponds to the residual astigmatism. Measurement of the residual astigmatism is made with an automated refractometer in combination with subjective refractometry. All patients wore their lenses on a daily basis.
The mean values and standard deviations (SDs) of the investigated parameters were calculated. The values presented are the means and SDs for each study variable. Descriptive statistics were analysed to report demographic data, refraction, topography, and contact lens parameters. The paired t test was used to compare mean changes in the visual outcomes of Toris K-fitted eyes without a history of surgery and eyes in the early stages (stages 1 and 2) of keratoconus. The Wilcoxon signed-rank test was used to compare mean changes in the visual outcomes of Toris K-fitted eyes with a history of keratoplasty and in the late stages (stages 3 and 4) of keratoconus. Pillai’s trace test was used to compare visual outcomes among operated and unoperated patients. Differences in mean visual acuity between spectacles, RGP lenses, and Toris K soft contact lenses were assessed with an independent sample t test. Values of p < 0.05 were considered statistically significant.
Results
Sixty-four eyes of 50 patients were included in this retrospective study. The female/male ratio was 26/24. The mean age ± SD at the time of fitting was 27.92 ± 9.86 years (range 10–58 years). The average follow-up duration for these patients was 11.94 ± 7.24 months (range 6–24 months).
The minimum, maximum, and mean values (±SD) of the refractive error, logMAR uncorrected visual acuity (UCVA), logMAR best spectacle-corrected visual acuity (BSCVA), logMAR best-corrected visual acuity with RGP lenses (BCVA RGP), logMAR best-corrected visual acuity with Toris K lenses (BCVA Toris K), and topographic and keratometric outcomes for all patients are shown in Table 2.
Fifty-six eyes (87.5 %) had no history of eye surgery; 46 were in stages 1–2, and 10 were in stages 3–4. Groups were stratified by stage and compared with each other. Eight (12.5 %) eyes had a history of penetrating keratoplasty surgery. Eyes with and without histories of surgery were also compared with each other.
The mean visual acuities of the 64 eyes enrolled in this study were 0.50 ± 0.53 with spectacles and 0.20 ± 0.19 with Toris K soft lenses, and the difference was statistically significant (p = 0.0001, t test). However, there was no statistically significant difference between BCVA Toris K and BCVA RGP (p = 0.20, t test).
Vision was improved from 0.84 ± 0.52 (UCVA) to 0.20 ± 0.21 with the Toris K lens (paired t test, p = 0.0001) in the unoperated group. Among keratoplasty patients, vision improved from 0.96 ± 0.19 to 0.25 ± 0.7 (Wilcoxon signed-rank test, p = 0.01). When the operated and unoperated groups were compared, there was no statistically significant difference (p = 0.66, Pillai’s trace test).
The mean UCVA was 0.64 ± 0.45, and the mean BCVA Toris K12 was 0.16 ± 0.15 for stages 1–2, representing a statistically significant improvement (paired t test, p = 0.0001). The mean UCVA was 1.38 ± 0.38, and the mean BCVA Toris K34 was 0.46 ± 0.30 for stages 3–4 and showed a statistically significant difference (Wilcoxon signed-rank test, p = 0.005) (Fig. 1).
The reasons for choosing the Toris K contact lens were inability to fit the patient with RGP lenses in 23 eyes (35.9 %), RGP lens intolerance in 21 eyes (32.81 %), and patient preference in 20 eyes (31.25 %). The most common complaint was unsatisfactory vision. This complaint was reported in 10 eyes (15.6 %) and resulted in the discontinuation of contact lens use in 4 eyes (66 % of the failures). Nonspecific discomfort (the patient’s subjective assessment) was reported in 8 eyes (12.5 %).
Table 3 summarizes the complications that were observed. Neither corneal pannus nor neovascularization was observed with Toris K SiH contact lenses. Superficial punctate keratitis was treated by educating the patients in the proper technique for cleaning these lenses and by providing artificial tear drops. Giant papillary conjunctivitis was treated with topical mast cell stabilizers and/or antihistamines. Toris K soft lens wear was discontinued after the occurrence of a sterile corneal ulcer and epithelial corneal oedema in 2 patients. The sterile corneal ulcer and corneal oedema were treated without visual loss.
Discussion
Continuous developments have occurred over the years giving rise to a variety of contact lens materials, designs, and wearing modalities for the successful optical correction of keratoconus [4].
The cause of keratoconus is unknown, although it is probably a genetic disease [1, 2]. A retrospective study that assessed the demographic profiles of patients with keratoconus reported the median age at the time of presentation was 24 years (range 15–36 years) [16]. In the present study, the average age of the patients was 27 years (range 10–58 years).
The process of contact lens fitting for eyes affected by keratoconus is complicated and challenging for both the patient and the fitter. To optimize the quality of life of patients with keratoconus, many different lens designs have been marketed. The advantages of RGP lenses are that they provide a smooth, regular surface that masks the underlying corneal irregularity and also provide good tear exchange. The disadvantages are stability (RGP lenses are more likely to decentre) and the difficulties in adaptation experienced by some patients [17].
Soft contact lenses provide greater comfort and protect the ocular surface in keratoconus [18]. In moderate-to-severe keratoconus, specialty custom soft contact lenses may be considered. These lenses may be manufactured from a hydrophilic material, such as the Soft K lens (Soflex Contact Lens Industries Ltd.; Misgav, Israel), or an SiH material, such as the KeraSoft (UltraVision; Bedfordshire, United Kingdom) and Toris K lenses. The main limitations of Soft K and KeraSoft 3 contact lenses are that they cannot mask high levels of irregular astigmatism. The thickness and hydrogel material are other disadvantages of Soft K lenses. Recently, Soft K contact lenses have begun to be manufactured using an SiH material [18–20].
This retrospective study documents clinical experience with the Toris K soft contact lens, a newly designed SiH lens with a toric front surface that causes geometry of spherical with an aspherical flattening, and contains bumps that facilitate dynamic stabilization.
Accordingly, in previous studies, similar lenses were preferred in eyes with mild-to-moderate keratoconus. The Toris K34 lens is a good alternative for patients with keratoconus grades 3–4. In a study by Yavuz et al. [21], the mean UCVA was 0.80 ± 0.40 and the mean BCVA Toris K was 0.14 ± 0.11, representing a statistically significant improvement with Toris K contact lenses. The authors found that Toris K SiH contact lenses were useful for the optical management of patients with keratoconus.
Similar to our study, Gumus et al. [22] determined that BCVA values were significantly better with Toris K lens than with the spectacles (p < 0.001).
Uçakhan et al. [19] studied a group of patients with a mean age of 28 years, which was similar to the mean age in the present study. They evaluated the safety and efficacy of KeraSoft 3 contact lenses (UltraVision), which are specialty custom soft toric lenses made of an SiH material with an aspheric front surface and prism ballast technology for stabilization. RGP lens intolerance was the most common indication. In the present study, an inability to fit the patient with an RGP lens was the most common reason for using a Toris K lens. In the Uçakhan study, 37 % of the participants stopped wearing lenses, and dissatisfaction with vision was the most common reason. In the present study, the discontinuation rate for the Toris K soft contact lens was 9.3 %, and the main reason was unsatisfactory vision.
Our study showed that the use of a Toris K soft keratoconus lens improved visual acuity in all grades of keratoconus and after keratoplasty. The Toris K lens corrected visual acuity to a significantly greater extent than spectacles. To the best of the authors’ knowledge, this is the first study to assess the efficacy of the Toris K soft lens in the optical management of patients with keratoconus after penetrating keratoplasty.
In a review of the literature, no study compared objective and subjective results achieved with Toris K soft contact lenses and RGP lenses in patients with keratoconus. In the current study, there was no statistically significant difference between BCVA Toris K and BCVA RGP. Toris K soft lenses allow many patients who cannot wear RGP lenses to avoid surgery, including patients with mild-to-moderate disease who experience discomfort with RGP lenses and those with advanced disease who cannot be fitted successfully with RGP lenses.
In the current study, the complication rate was 15.6 %, and the most common complications were superficial punctate keratitis (4.6 %) and giant papillary conjunctivitis (4.6 %). In a study by Forister et al., a total of 35.4 % of the eyes examined had a single complication; superficial punctate keratitis occurred in 10.3 % of RGP contact lens wearers, and giant papillary conjunctivitis occurred in 7.3 % [23].
Altun et al. followed 3 keratoconus patients who refused using RGP contact lens because of intolerance. Toris K contact lenses were fitted on all eyes, and during 28 months of follow-up, only one patient had conjunctival hyperemia for a few days in the beginning [24].
The lower complication rates may be explained by the fact that the patients received appropriate treatment when the complications were detected during regular follow-up visits. In the present study, even with regular follow-up visits, sterile corneal ulcers and oedema were reported in 2 eyes (3.1 %). All complications were resolved with medical treatment. Neither corneal pannus nor neovascularization was observed with Toris K soft contact lenses within the follow-up period of 13.80 ± 10.47 months; however, a longer period may be needed for evaluation.
A weakness of the present study is its retrospective nature and the lack of determination of a fixed last check period in all cases. A positive aspect of the present study is the subgroup classifications of patients using Toris K soft contact lenses based on keratoconus grade and history of keratoplasty.
In conclusion, the Toris K SiH contact lens is a viable alternative for the optical management of all grades of keratoconus. In patients with keratoconus who are intolerant of RGP, Toris K soft contact lenses can increase BCVA. Therefore, this type of lens is recommended as an alternative to RGP lenses. Future studies should be performed on larger populations of patients and for longer periods of time to confirm these findings. Moreover, these long-term clinical studies should be conducted with a control group and a double-blinded design.
References
Krachmer JH, Feder RS, Belin MW (1984) Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol 28:293–322
Rabinowitz YS (1998) Keratoconus. Surv Ophthalmol 42:297–319
Efron N, Hollingsworth JG (2008) New perspectives on keratoconus as revealed by corneal confocal microscopy. Clin Exp Optom 91:34–55
Barnett M, Mannis MJ (2011) Contact lenses in the management of keratoconus. Cornea 30:1510–1516. doi:10.1097/ICO.0b013e318211401f
Lass JH, Lembach RG, Park SB, Hom DL, Fritz ME, Svilar GM et al (1990) Clinical management of keratoconus: a multicenter analysis. Ophthalmology 97:433–445
Asbell PA, Dunn MJ (1997) Fitting the abnormal cornea. In: Krachmer JH, Mannis MJ, Holland EJ (eds) Cornea: diagnosis and management. Mosby-Year Book Inc, St. Louis, pp 1457–1460
Barr JT, Wilson BS, Gordon MO, Rah MJ, Riley C, Kollbaum PS et al (2006) Estimation of the incidence and factors predictive of corneal scarring in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Cornea 25:16–25
Bergmanson JP, Ruben M, Chu LW (1984) Corneal epithelial response of the primate eye to gas permeable corneal contact lenses: a preliminary report. Cornea 3:109–113
Efron N (2007) Contact lens-induced changes in the anterior eye as observed in vivo with the confocal microscope. Prog Retin Eye Res 26:398–436
Owens H, Watters G, Gamble G (2002) Effect of SoftPerm lens wear on corneal thickness and topography: a comparison between keratoconic and normal corneas. CLAO J 28:83–87
Edmonds CR, Wung SF, Husz MJ, Pemberton B (2004) Corneal endothelial cell count in keratoconus patients after contact lens wear. Eye Contact Lens 30:54–58
Giasson CJ, Perreault N, Brazeau D (2001) Oxygen tension beneath piggyback contact lenses and clinical outcomes of users. CLAO J 27:144–150
Belin MW, Ambrósio R (2013) Scheimpflug imaging for keratoconus and ectatic disease. Indian J Ophthalmol 61:401–406
Kamiya K, Ishii R, Shimizu K, Igarashi A (2014) Evaluation of corneal elevation, pachymetry and keratometry in keratoconic eyes with respect to the stage of Amsler-Krumeich classification. Br J Ophthalmol 98:459–463
Keratoconus soft contact lenses, in: SwissLens product document, 2012, pp. 16–17
Fatima T, Acharya MC, Mathur U, Barua P (2010) Demographic profile and visual rehabilitation of patients with keratoconus attending contact lens clinic at a tertiary eye care centre. Cont Lens Anterior Eye 33:19–22. doi:10.1016/j.clae.2009.09.004
Chou B, Weissman BA (2010) Making sense of the irregular cornea. Rev Cornea Cont Lenses 147:14–21
González-Méijome JM, Jorge J, De Almeida JB, Parafita MA (2006) Soft contact lenses for keratoconus: case report. Eye Contact Lens 32:143–147
Uçakhan OO, Bayraktutar B (2014) KeraSoft 3 contact lenses in corneal ectasia. Eye Contact Lens 40:390–394. doi:10.1097/ICL.0000000000000092
Fernandez-Velazquez FJ (2012) Kerasoft IC compared to Rose-K in the management of corneal ectasias. Cont Lens Anterior Eye 35:175–179. doi:10.1016/j.clae.2012.02.005
Yavuz L, Yilmaz I, Özgür OR, Kandemir B, Calli U, Cabi C (2013) Toris K silicone hydrogel contact lens for the optical management of keratoconus. New J Med 30:174–176
Gumus K, Kahraman N (2015) A New Fitting Approach for Providing Adequate Comfort and Visual Performance in Keratoconus: Soft HydroCone (Toris K) Lenses. Eye Contact Lens, 1–6
Forister JF, Forister EF, Yeung KK, Ye P, Chung MY, Tsui A et al (2009) Prevalence of contact lens-related complications: UCLA contact lens study. Eye Contact Lens 35:176–180
Altun A, Kurna SA, Sengor T, Altun G, Olcaysu OO, Simsek MH (2015) Success of hydrocone (TORIS-K) soft contact lens for keratoconus and traumatic keratopathy. Pak J Med Sci 31:995–998
Funding
There is no funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Sultan, P., Dogan, C. & Iskeleli, G. A retrospective analysis of vision correction and safety in keratoconus patients wearing Toris K soft contact lenses. Int Ophthalmol 36, 799–805 (2016). https://doi.org/10.1007/s10792-016-0200-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-016-0200-0