Abstract
To evaluate the results of pterygium excision with conjunctival autograft transplantation for primary pterygium performed by trainee ophthalmologists. Design Prospective interventional case series. Setting A tertiary eye care center in northern Thailand. Participants Patients with primary pterygium recruited from July 2011 to August 2012. Intervention In all cases, the affected eye underwent pterygium excision followed by a superior conjunctival autograft carried out by trainee ophthalmologists. Main outcome measure The recurrence of pterygium and other post-operative complications. Results Sixty-two eyes from 54 patients were studied. There were 36 females (66.7 %) and 18 males (33.3 %). The mean age of the patients was 54.5 (±9.8) years with the mean corneal invasion measured at 3.3(±0.8) mm. Pterygium morphologies of Grade 1, Grade 2, and Grade 3 were 33.9, 48.4, and 17.7 %, respectively, with the mean follow-up time of 17.3 (±7.9) months. Pterygium recurred in the cornea of six eyes (9.7 %). All recurrences occurred within 6-month post-operation. Other post-operative complications included conjunctival recurrence (4.8 %), graft retraction (3.2 %), conjunctival cyst (3.2 %), and increased intraocular pressure (1.6 %). The recurrence of pterygium was not associated with the patient age (p = 0.72), occupation (p = 0.23), sun exposure time (p = 0.18), pterygium duration (p = 0.22), pterygium size (p = 0.67), or pterygium morphology (p = 0.85). Conclusion The recurrence rate and post-operative complications of pterygium excision with conjunctival autograft performed by trainee ophthalmologists were within acceptable limits. All recurrence occurred within 6 months after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pterygium is a common degenerative change of the ocular surface caused by multifactorial origins, in which ultraviolet (UV) exposure has been implicated as a major causative factor [1, 2]. The prevalence rates of pterygium are higher in tropics than in temperate regions [3–5]. Even though medical treatment can relieve symptoms of eye irritation or redness, surgery remains the treatment of choice to eliminate the pterygium. The main indications for pterygium surgery are visual impairment and cosmetic problems. In general, the goals of pterygium surgery are to remove the pterygium, to achieve a desirable cosmetic outcome, and to avoid possible complications. There are several surgical modalities for pterygium treatment with a wide degree of achievement rates; however, pterygium recurrence still remains a significant problem.
Simple pterygium excision without adjunctive therapy has been known for its high recurrence rate, and is rarely acceptable in the treatment of pterygium [6–8]. Surgery adjunct with anti-fibrotic agents such as mitomycin-C or beta irradiation can decrease the recurrence rate; however, these therapies may cause visual threatening complications or even eye loss which may occur as late as 20 years later [7, 9, 10]. Conjunctival autograft (CAG) transplantation involves the placement of a free graft, from another part of an eye, covering the bare scleral defect after pterygium removal. This procedure has been shown to be safe and effective [11] even though, it requires more ocular surface disruption, longer surgical time, and more surgical skill than simple excision. At present, pterygium excision with CAG has been considered as the standard treatment for pterygium removal; however, there have been a wide range of surgical techniques and success rates of this operation [6, 7, 11–14]. Amniotic membrane transplantation has been used as an alternative to CAG; however, the success rate has been shown to be inferior to that of CAG and should be considered in the patient who needs a large graft to cover the defect or to preserve the conjunctiva for future glaucoma surgeries [13–15].
Pterygium surgery is the second most common procedure after cataract surgery performed by ophthalmologists in Thailand, a tropical country lying close to the equator, where pterygium is a common eye problem. From a recent survey of pterygium surgery in this country, pterygium excision with CAG was the most preferred procedure [16]. Pterygium surgery adjunct with CAG is a procedure required during ophthalmology training. This study aimed to evaluate the results of pterygium excision with CAG for primary pterygium performed by ophthalmology residents. The results from this study may be beneficial in improving patient care and professional training.
Materials and methods
Approved by the Institute Review Board, this study was initiated and carried out in accordance with the ethical standards stated in the declaration of Helsinki (protocol number 214/2554). Written consent was obtained from all patients enrolled in the study.
Patient selection
The patients undergoing pterygium excision with CAG by ophthalmology residents at Chiang Mai University Hospital, from July 2011 to August 2012, were recruited. The inclusion criteria included primary pterygium, patient age between 20 and 80 years, and corneal invasion of ≥2 mm.
Patients were excluded on the basis of the following criteria: more than one head of pterygium, previous ocular surgery, active ocular surface inflammation or infection, glaucoma or high risk of glaucoma, and severe ocular surface disease.
At the initial evaluation, medical and ocular histories were reviewed and each patient was requested to response to specific questions regarding occupation (indoor or outdoor task), sunlight exposure time per day, and pterygium duration. Each patient underwent a comprehensive ophthalmic examination including visual acuity (VA) assessment, slit-lamp biomicroscopy, intraocular pressure (IOP) measurement, and fundus examination. The clinical features of pterygium were evaluated for location, extension onto the cornea, and grading morphology according to clinical classification based on relative transparency of pterygium tissue [6]. Pterygia were assigned as Grade 1 (atrophic), in which episcleral vessels underlying the body of pterygium was clearly visible, Grade 3 (fleshy), in which episcleral vessels were totally obscured, and Grade 2 (those between grades 1 and 3), with partially obscured episcleral vessels.
Surgical technique
All surgeries were performed by 8 ophthalmology residents who had experienced pterygium excision adjunct with CAG for a minimum of five cases.
The surgical technique was standardized for all surgeons before initiation of the study and the details of the procedure were as follows: all patients received topical anesthesia with tetracaine hydrochloride 0.5 % and xylocaine 2 % with 1:200,000 adrenaline injected into body of the pterygium. Then the pterygium was excised from the cornea, the residual pterygium tissue was removed as much as possible leaving the clear corneal stroma. The episcleral as well as surrounding tenon tissues including the underlie and the conjunctival edge were also removed. Care was taken to avoid damage to rectus muscle and prolapsed orbital fat from excess tenon removal. The bare sclera bed was created and measured in the position that the eye deviated to the opposite site of pterygium to obtain the maximum area of the defect. The graft was measured and harvested from the superior bulbar conjunctiva of the same eye close to the limbus. The free graft was, then, placed and sutured to the episcleral bed with interrupted 8/0 vicryl suture, and was oriented with the limbal side of the graft to the limbal side of the defect. The surgical time, the graft size, number of stitches, and any intra-operative complications were recorded. All patients were asked to rate their discomfort and pain sensation during the operation (score 0–10, from the least to the most).
Post-operative care and follow-up
The regimens for post-operative medications were tobramycin 0.3 % and prednisolone acetate 1 %, four times daily each, and lubricant and oral acetaminophen as required. After 1 month, topical steroid was switched to fluorometholone, then was tapered off, and discontinued within 3 months. Patients were given a post-surgery follow-up at 1 day, 1 week, 1, 3, 6, and 12 months. Patients were recommended to avoid sunlight exposure using UV protective sunglasses and keep their eye from dust, and windy conditions. At each visit, patients were evaluated for VA, IOP, slit-lamp examination, particularly, surgical sites and a graft appearance. Post-operative discomfort and pain score was evaluated at 1 day, 1 week, and 1 month, respectively. Any post-operative complications were also recorded.
Two views of the anterior eye photography were taken including one of the eye in the primary position, and, another was that of the eye deviated to the opposite site of surgery. The photograph was taken before the surgery, and post-operative visits on week 1, month 1, month 3, month 6, and month 12, respectively. The recurrence of pterygium was determined according to those described previously as: “conjunctival recurrence”, in which fibrovascular tissue was present in the surgical area without corneal invasion, and “corneal or true recurrence”, in which a post-operative regrowth of fibrovascular tissue crossing the limbus onto the cornea in the area of previously pterygium excision [13]. The outcome of surgery was evaluated from the photographs and/or slit-lamp biomicroscope by a single investigator (N.T) in a masked fashion.
Statistical analysis
In this study, eyes rather than people were used as a unit for statistical analysis. Quantitative data were calculated as mean and standard deviation. Qualitative data were calculated into frequency. The cumulative proportion of recurrence and recurrent-free time were analyzed by the Kaplan–Meier method. A multivariate logistic regression model was used to determine variables associated with pterygium recurrence. p value of less than 0.05 was considered to be statistically significant. All statistical analyses were performed using the SPSS version 17.0 (SPSS Inc, Chicago, IL).
Results
Patient demography and operation details
Sixty-two eyes from 54 patients were enrolled in this study. Eight patients had sequential bilateral surgeries. The mean age of the patients was 54.5 (±9.8, range 29–78) years. There were 36 females (66.7 %) and 18 males (33.3 %). The patient occupations were indoor work in 43 (79.6 %) cases, and outdoor work in 11 (20.4 %) cases. Sunlight exposure of ≤3 h/day was found in 45 (72.6 %) eyes, and >3 h/day in 17 (27.4 %) eyes. The duration of pterygium was ≤3 years in 33 (61.1 %) eyes, and >3 years in 21 (38.9 %) eyes. Ocular discomfort was a major indication for surgery in 60 eyes. Among these eyes, 28 eyes also had large-sized pterygium (>3 mm), 6 had cosmetic reason, and 4 had decreased vision. (Figure 1) The affected eye was the right eye for 31 (50 %) eyes, and the left eye for 31 (50 %) eyes. All pterygia located on the nasal side of the cornea with mean corneal extension of 3.3 (±0.8, range 2–6.5) mm. Mean corneal astigmatism was 2.6 (±2.9, range 0.2–12.4) diopters. Pterygium was in Grade 1, 2, and 3 for 21 (33.9 %), 30 (48.4 %), and 11 eyes (17.7 %), respectively.
The mean operation time was 51.5 (±11.6, range 20–75) minutes with a mean graft size of 41.1 (±10.2, range 16–64) sq mm. The mean number of stitches was 8.4 (±1.5, range 4–12) stitches, while the mean discomfort and pain score during intra-operative, at day 1, week 1, and month 1 post-operative was 3.8 ± 2.6, 3.7 ± 2.7, 1.3 ± 1.8, and 0.2 ± 0.6, respectively.
Recurrence rate and factors related to recurrence
The mean follow-up time was 17.3 (±7.9) months. Corneal recurrences of pterygium were found in six eyes (9.7 %), which were observed after surgery at 2, 3, and 6 months in 1, 3, and 2 eyes, respectively. The mean number of operated eyes was 7.8 eyes per surgeon with individual surgeon recurrence rate range from 0 to 25 % (Table 1). For a patient who had pterygium recurrence at 2 months, this patient missed follow-up at 1 month and also ran out of medications, then he never showed up after 2 months. The cumulative non-recurrence rate at 3, 6, and 12 months was 93.5, 90.3, and 90.3 %, respectively. The mean recurrent-free time was 11.2 months (Fig. 2). When using multiple logistic regression analysis, the recurrence of pterygium was not significantly associated with the patient age (p = 0.72), occupation (p = 0.23), sun exposure time (p = 0.18), duration (p = 0.22), size (p = 0.67), and grading of pterygium (p = 0.85).
Other post-operative results and complications
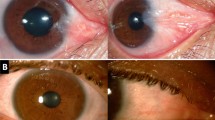
The 12-month post-operative or final best-corrected visual acuity (BCVA) was stable compared to pre-operative BCVA in 48 eyes (77.4 %), gained ≥1 line in 12 eyes (19.4 %), and worsen 1 line in 2 eyes (3.2 %), respectively. No eyes had a loss of ≥2 lines of BCVA from a baseline, and no serious complications were observed. Other post-operative complications were conjunctival recurrence (3), minimal graft retraction without need to re-suture (2), conjunctival epithelial cyst (2), and transient increased IOP (1). From the two eyes with conjunctival cyst, one also had corneal recurrence, and another had conjunctival recurrence (Fig. 3).
Anterior eye photographs of two patients: patient no. 23 (a, b) a pre-operative appearance, b corneal recurrence of pterygium and conjunctival cyst at 3-month post-operation; Patient no. 32 (c, d) c pre-operative appearance, d conjunctival recurrence with a small conjunctival cyst at 12-month post-operation
Discussions
Conjunctival autograft transplantation has become the preferred procedure for pterygium surgery since Kenyon et al. reported its successful results in 1985 [11]. They demonstrated the recurrence rate of 5 % for advanced and recurrent pterygium without serious complications. However, the recurrence rates among studies vary from as low as 2 % to as high as 40 % [6, 8, 17]. The wide range of success rates of this procedure may be due to both patient and surgeon factors. Ti and co-worker found that the success of CAG for pterygium varied widely among surgeons, ranging from 5 to 82 %, and might be related to surgical skill or different surgical technique [17].
In general, pterygium surgery is considered as a minor ocular procedure. During training, pterygium surgery can be performed by eye resident doctors before intraocular surgery such as cataract surgery. There have been only few studies regarding the results of pterygium surgery done by ophthalmology trainees. Sebban’s study found that the recurrence rate of pterygium excision done by trainees was 46 % [18]. Farrah and colleagues compared the outcomes of CAG for primary pterygium excision when performed by consultants and trainees, and found that the recurrent rate was 6.8, and 19.4 %, respectively [19]. While Chalioulias et al. found no different results of CAG for primary pterygium removal of those performed by the consultants and trainees (26.3 and 24.3 %, respectively) [20]. The different results of both studies might be due to expertise and background experience of the surgeon. This is because Farrah’s study was done in a country where pterygium was common. However, all previous works were retrospective which might promote confounding factors. This study is a prospective study on results of CAG for primary pterygium performed by ophthalmology residents. Even though, the recurrence of this procedure performed by trainees (9.7 %) was higher than that those by consultants (4.8 %) within the same institute and had similar inclusion criteria for patient recruitment [15], this recurrence rate was acceptable when compared to previous studies [7, 14]. The reasons may be partly due to the fact that all of the surgeons in this study have become accustomed to at least five cases using this technique, and the surgery was controlled for primary pterygium without any ocular surface problems. In addition, the protocol of the procedure and the post-operative care were standardized in all patients to minimize variation in the results.
To prevent the under-reported recurrence rate after surgery, this study also included a patient with corneal recurrence at 2-month post-operation who did not attend a follow-up at 1 month and lost to follow-up after 2 months. The recurrence in this case might be related to patient compliance to use medication and come for follow-up visit. All recurrent pterygium in this study occurred within 6-month post-surgery, which is the period that pterygium commonly recurs [15, 17]. Data from prevalence surveys suggested that pterygium was associated with multifactorial causes including living in a rural region, increasing in age, male gender, and occupation linked to outdoor work and other exposure [3–5, 21]. These evidences suggest pterygium is a result of ocular sun exposure in dose-related manner; therefore, sunlight exposure might also affect the outcome after surgery. Two previous studies found that increasing in age was significantly associated with less risk for recurrence [8, 22]. Tan et al. found that pterygium morphology was associated with the pterygium recurrence as fleshy pterygium was a significant risk factor for both primary and recurrent pterygium if bare sclera excision was performed; however, they did not identify risk factors associated with recurrence in CAG group [6]. These points are of consequence even though this study was unable to identify the factors associated with the pterygium recurrence. Nonetheless, we recommend all patients avoid sunlight and environmental factors (i.e., dust, wind) during the post-operative period. In this study, two eyes with conjunctival cyst also had corneal and conjunctival recurrence in each case. Even though conjunctival cyst and conjunctival recurrence are not counted as serious complications after pterygium surgery, they may pose unpleasant eye appearance.
The main strengths of this study are the prospective design, which minimized the selection bias, and the outcomes were evaluated by single independent observer, minimizing inter-observer errors. However, there were some limitations of this study. First, multiple surgeons involved in this study might affect the outcome of surgery due to various degrees of surgical skills. Second, varied number of cases in each surgeon might cause a wide range of recurrence rate among surgeons. Last but not least, this study could not address risk factors for pterygium recurrence, which may be due to a relatively small sample size. Therefore, further studies with larger sample size looking at the pterygium recurrence are required.
We conclude that pterygium excision with CAG done by ophthalmology trainees was safe and effective with a short learning curve. The recurrence rate was within acceptable limits with appropriate criteria for patient selection and proper surgical techniques. Even though this study did not demonstrate enough evidence, preventive strategy to avoid UV exposure and environmental factors is highly recommended in all patients, especially during the first 6 months after surgery in order to achieve effective results, particularly patients who live in tropical area.
References
Coroneo MT (1993) Pterygium as an early indicator of ultraviolet insolation: a hypothesis. Br J Ophthalmol 77:734–739
Taylor HR (1980) Aetiology of climatic droplet keratopathy and pterygium. Br J Ophthalmol 64:154–163
McCarty CA, Fu CL, Taylor HR (2000) Epidemiology of pterygium in Victoria, Australia. Br J Ophthalmol 84:289–292
Gazzard G, Saw SM, Farook M, Koh D, Widjaja D, Chia SE et al (2002) Pterygium in Indonesia: prevalence, severity and risk factors. Br J Ophthalmol 86:1341–1346
Wong TY, Foster PJ, Johnson GJ, Seah SK, Tan DT (2001) The prevalence and risk factors for pterygium in an adult Chinese population in Singapore: the Tanjong Pagar survey. Am J Ophthalmol 131:176–183
Tan DT, Chee SP, Dear KB, Lim AS (1997) Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol 115:1235–1240
Hirst LW (2003) The treatment of pterygium. Surv Ophthalmol 48:145–180
Chen PP, Ariyasu RG, Kaza V, LaBree LD, McDonell PJ (1995) A randomized trial comparing mitomycin C and conjunctival autograft after excision of primary pterygium. Am J Ophthalmol 120:151–160
Ti SE, Tan DT (2003) Tectonic corneal lamellar grafting for severe scleral melting after pterygium surgery. Ophthalmology 110:1126–1136
Tarr KH, Constable IJ (1980) Late complications of pterygium treatment. Br J Ophthalmol 64:496–505
Kenyon KR, Wagoner MD, Hettinger ME (1985) Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology 92:1461–1470
Ma DH, See LC, Liau SB, Tsai RJ (2000) Amniotic membrane graft for primary pterygium: comparison with conjunctival autograft and topical mitomycin C treatment. Br J Ophthalmol 84:973–978
Prabhasawat P, Barton K, Burkett G, Tseng SC (1997) Comparison of conjunctival autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology 104:974–985
Luanratanakorn P, Ratanapakorn T, Suwan-Apichon O, Chuck RS (2006) Randomised controlled study of conjunctival autograft versus amniotic membrane graft in pterygium excision. Br J Ophthalmol 90:1476–1480
Tananuvat N, Martin T (2004) The results of amniotic membrane transplantation for primary pterygium compared with conjunctival autograft. Cornea 23:458–463
Chaidaroon W, ThongKhao-Om M, Wiwatwongwana D, Wiwatwongwana A (2013) A survey of pterygium surgery in Thailand 2010. J Med Assoc Thail 96:64–68
Ti SE, Chee SP, Dear KB, Tan DT (2000) Analysis of variation in success rates in conjunctival autografting for primary and recurrent pterygium. Br J Ophthalmol 84:385–389
Sebban A, Hirst LW (1991) Pterygium recurrence rate at the Princess Alexandra Hospital. Aust NZ J Ophthalmol 19:203–206
Farrah JJ, Lee GA, Greenrod E, Vieira J (2006) Outcomes of autoconjunctival grafting for primary pterygia when performed by consultant compared with trainee ophthalmologists. Clin Exp Ophthalmol 34:857–860
Chalioulias K, Dwarika D, Thakur S (2007) Pterygium excision with conjunctival autograft: consultant versus trainee. Clin Exp Ophthalmol 35:396 (author reply)
Ma K, Xu L, Jie Y, Jonas JB (2007) Prevalence of and factors associated with pterygium in adult Chinese: the Beijing Eye Study. Cornea 26:1184–1186
Lewallen S (1989) A randomized trial of conjunctival autografting for pterygium in the tropics. Ophthalmology 96:1612–1614
Acknowledgments
This study was supported by the Faculty of Medicine Endowment Fund, Faculty of Medicine, Chiang Mai University (Grant number 16/2555). All authors declare no conflict of interest. The authors are grateful to Mrs. Rodjana Peugchanteug, MSc, for assisting in statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest is declared.
Rights and permissions
About this article
Cite this article
Kositphipat, K., Tananuvat, N. & Choovuthayakorn, J. Results of pterygium excision adjunct with conjunctival autograft transplantation for primary pterygium by ophthalmology trainees. Int Ophthalmol 36, 615–621 (2016). https://doi.org/10.1007/s10792-016-0175-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-016-0175-x