Abstract
To compare the accuracy of the predictions of SRK/T and Haigis formulae, incorporating all the parameters calculated using Zeiss IOLMaster Scan, based on partial coherence interferometry, and to analyse the effect of updating or optimisation of the constants on the post-operative result. A retrospective study was done on 51 consecutive patients, who underwent phacoemulsification by a single surgeon with a temporal corneal incision and a standard Alcon Acrysof MA30 implant in the bag. The pre-operative data were measured using Zeiss IOLMaster scan, and the IOL power calculations were done using both SRK/T and Haigis formulae. The final implant power selection was based on SRK/T predictions. The patients were divided into three groups depending on the axial length, and the post-operative results were analysed at 4 weeks. The difference between the predicted value and the post-operative spherical equivalent was calculated for both the formulae, and a paired t test used for significance. The axial length ranged from 20.93 to 25.16 mm. The error for Haigis was less compared to SRK/T overall and SRK/T resulted in an average hypermetropia 0.69 D and Haigis resulted in an average myopia of 0.16 D. The comparison between SRK/T and Haigis and the updated version of both using the paired t test shows a statistically significant difference, the p values being <0.03 and <0.01, respectively. The updated Haigis Formula with the optimised constants was significantly more accurate than SRK/T formula.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Implant power calculation formulae attempt to provide a predictable refractive outcome based on preoperative assessments. Achieving the predicted post-operative refraction is a challenge for every cataract surgeon. Although partial coherence interferometry (PCI) has greatly improved biometry [1, 2], the issue of the choice of intraocular lens (IOL) formula to be used for calculation is debatable. While the SRK/T formula (2 variables) is commonly used [3] for all axial lengths, we compared its accuracy with that of the Haigis formula [4, 12] which uses 3 variables to calculate the effective lens position (A or ACD for SRK/T, and A or ACD and/or A0, A1 and A2 for Haigis). The Haigis formula uses 3 variables for IOL calculation, but only uses 2 for ELP prediction: AXL and ACD (K is only used in the optical calculation). The constants used in both the formulae can be optimised to improve the predictive accuracy. We also analysed the effect of optimising the constants for both SRK/T and Haigis formulae on the post-operative result.
Materials and methods
A total of 51 eyes of 51 consecutive patients were measured preoperatively by Zeiss IOLMaster system based on partial coherence interferometry to measure the axial length (AL), corneal radius of curvature (K-reading) and the anterior chamber depth. The SRK/T and Haigis formulae combined with IOLMaster were used to calculate the pre-operative IOL power in all patients. The constants were updated/optimised using the user group for laser interference biometry (ULIB). All patients underwent phacoemulsification with 3-mm temporal corneal non-sutured incisions by a single surgeon. Based on the predictions of SRK/T formula, a single style, standard Alcon Acrysof MA30 lens was implanted in the capsular bag. Exclusion criteria included (1) patients unable to undergo PCI biometry due to the density of the cataract, (2) patients who had a complicated surgery including a posterior capsular tear, and (3) implants other than Acrysof MA30. Post-operative refractive assessment was performed 4 weeks after surgery. The post-operation prediction for the same implant power was retrospectively calculated for updated SRK/T and Haigis formulae. The difference between the predicted value and the actual post-operative spherical equivalent was calculated for all the four formulae and the results analysed using paired t test for statistical significance. The entire series as well as subdivisions of axial length ranges were analysed.
Results
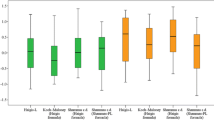
The axial length ranged from 20.93 to 25.16 mm. For analytical purposes, we divided the patients into three groups as shown by Fig. 1. Those with axial length less than 22.0 mm (9 of 51 cases), 22–24 mm (37 of 51 cases), and more than 24.0 mm (5 of 51).
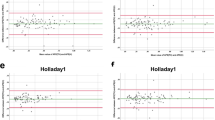
Table 1 shows the mean absolute error (MAE) for the four formulae. Updated Haigis performed better than the other three. Comparisons between the SRK/T and Haigis and the updated version of both using the paired t test show statistically significant differences, the p values being <0.03 and 0.01, respectively. Figure 2 shows the comparison of errors for the four formulae in the entire series as well as in the subdivisions of axial length. The error for Haigis is less compared to SRK/T other than the group with more than 24 mm axial length. This was found to be statistically significant overall and for the eyes of 22–24 mm. In the longer and the shorter groups, statistical significance could not be assessed due to low subject numbers. Overall, Haigis resulted in an average myopia of −0.22 and SRK/T in hypermetropia of 0.6 D sphere. The scatter plots show that the regression line for the Haigis formula (Fig. 4) is less steep than that for SRK/T (Fig. 3). The SRK/T seems to be more dependant on the axial length. However, in the group with >24 mm axial length, the error seems to be least with SRK/T, updated SRK/T (Fig. 5) and updated Haigis (Fig. 6). In the group with <22 mm axial length, the Haigis seems to predict more accurately.
(For Figs. 3, 4, 5, 6: x-axis is axial length in mm and y-axis is error in dioptres)
Discussion
Successful IOL implantation depends partly on the ability to predict post-operative refraction with accuracy. Errors in predicted refraction after IOL implantation are mostly a result of axial length measurement error. With the advent of partial coherence interferometry, the axial length determination has become 5 times more accurate compared with classical ultrasound biometry [2]. Therefore, a need has arisen for even more precise IOL formulae. The higher accuracy of the newer generation theoretical formulas lies in their improved prediction of the pseudophakic anterior chamber depth [5]. Possible explanations of the differences between the formulae maybe the use of different refractive indices in the IOLMaster software, the effect of corneal power and post-operative anterior chamber depth which would also affect the results.
Post-operative refractive assessment was performed at 4 weeks post-operatively in our study, as done by Verhulst and Vrijghem [6] in their study for calculating IOL power using Zeiss IOLMaster. We chose the SRK/T formula because it is the most commonly used formula [3] in UK and includes many users throughout the world. Hoffmann et al. [7]. suggested that newer generation formulae like SRK/T, Holladay and Haigis should be used. This is especially true for short and long eyes. According to the National biometry audit [3], the Haigis formula was not being used in Ophthalmology departments in UK. There are several studies [8–10] comparing IOL power formulae like Binkhrost, SRK II, SRK/T, Hoffer Q, and Holladay. But we could not locate a study which compared the use of SRK/T and Haigis and therefore we decided to perform one.
Implant power calculation formulae typically derive from either an empirical or a theoretical background. However, all formulae use a constant that can be updated or optimised for an individual surgeon or IOL type. This update can be achieved by taking pre-operative parameters and post-operative outcomes of a subset of patients and back calculating the constant. Hoffer’s study [11] has strongly supported the importance of optimisation of A constants. As few as 30 operations are required to optimise the A constants for a particular IOL and surgeon [11]; and can be rapidly done using several software programs [4, 12–14] or the Zeiss IOLMaster software. We therefore also studied the SRK-T and Haigis with their updated constants.
In this study, using this approach, we found that the smallest errors by subset was updated Haigis for the overall and axial length 22–24 mm group, Haigis for <22 mm, and SRK-T and updated version of both for >24 mm (Fig. 3). The updated Haigis formula with optimised constants was significantly more accurate than the SRK-T formula. It is possible to limit post-operative refractive outcome within ±1.00 D in 86 % cases and ±2.00 D in 100 % eyes using updated Haigis formula with IOLMaster. In Haigis et al.’s, study [15], PCI was carried out by Zeiss IOLMaster and IOL calculation by Haigis formula with and without optimisation of constants was done. Their post-operative predicted outcome was within ±1.00 D in 85.7 % and ±2.00 D in 96 % of cases [15]. The results of this study are similar to ours.
In our study, we found MAE of 0.56 D for Haigis and 0.75 D for SRK/T and thus the Haigis formula was more accurate than SRK-T.
Findl et al. [16] used PCI biometry with 4 IOL formulae SRK II, Olsen, SRK/T and Holladay 1. In Findl’s study, the SRK/T and Holladay 1 yielded an MAE in prediction of 0.44 D. Olsen and SRK II were less accurate with MAE 0.49 D and 0.47 D, respectively [16]. In our series, MAE for SRK-T was 0.75 D and updated SRK-T was 0.62 D. Findl et al.’s series found MAE of 0.44 D for SRK/T and 0.42 D for updated SRK/T. In both studies, optimisation of constants showed further improvement in predicting the post-operative outcome. Thus, optimisation or updating the constants reduces the predictive MAE with both SRK/T and Haigis. We therefore strongly recommend optimisation of constants to improve the predictive accuracy. Also, in our present study, updated Haigis performed best overall in all the axial length subgroups except the >24 mm subset.
The limitation of this study is the small sample size. The authors have included eyes ranging from 20.93 to 25.16 mm and divided them into three groups for subgroup analysis. This lends the study to both type I and II errors when testing for statistical significance.
There is a need to conduct more studies with a larger sample size, especially patients with extreme axial length, to assess the predictability of these formulae better.
Due to the retrospective nature of the study and the relatively small sample of the patients included in the study with limited range of axial length, the results may only hold true for the central group of axial length. More patients with shorter and longer axial lengths would had added more strength to this paper.
References
Eleftheriadis H (2003) IOLMaster biometry: refractive results of 100 consecutive cases. Br J Ophthalmol 87:960–963
Schachar RA, Levy NS, Bonney RC (1980) Accuracy of intraocular lens powers calculated from A-scan biometry with the echo-oculometer. Ophthalmic Surg 11:856–858
Gale RP, Saha N, Johnston RL (2004) National biometry audit. Eye 18:63–66
Haigis http://www.augenklinik.uni-wuerzburg.de/uslab/ioltxt/haie.htm XALDON Technologies
Olsen T, Thim K, Corydon L (1991) Accuracy of the newer generation intraocular lens power calculation formulas in long and short eyes. J Cataract Refract Surg 17:187–193
Verhulst E, Vrijghem JC (2001) Accuracy of intraocular lens power calculations using the Zeiss IOLMaster. A prospective study. Bull Soc Belge Ophtalmol 281:61–65
Hoffman PC, Hütz WW, Eckhardt HB (1997) Significance of optic formula selection for postoperative refraction after cataract operation. Klin Monatsbl Augenheilkd 211:168–177
Retzlaff JA, Sanders DR, Kraff MC (1990) Development of the SRK/T intraocular lens implant power calculation formula. J Cataract Refract Surg 16:333–340
Sanders DR, Retzlaff JA, Kraff MC, Gimbel HV, Marsha G, Raanan MS (1990) Comparison of the SRK/T formula and other regression formulas. J Cataract Refract Surg 16:341–346
Richards SC, Oslen RJ, Richards WL, Brodstein RS, Hale PN (1985) Clinical evaluation of six intraocular lens calculation formulas. J Am Intraocul Implant Soc 11:153–158
Hoffer KJ (1980) Biometry of 7500 cataractous eyes. Am J Ophthalmol 90:360–368
Medisoft ophthalmology electronic patient record. www.medisoft.co.uk, Leeds
Holladay IOL Consultant IOL calculation software for ophthalmologists. www.docholladay.com/iolprogram
Hoffer Eye Lab Inc. KDHofferMD@aol.com
Haigis W, Lege B, Miller N, Schneider B (2000) Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol 238:765–773
Findl O, Drexler W, Menapace R, Heinzl H, Hitzenberger CK, Fercher AF (2001) Improved prediction of intraocular lens power using partial coherence interferometry. J Cataract Refract Surg 27:861–867
Acknowledgments
Mr. Alan Rotchford SpR, Queens Medical Centre, Nottingham, for statistical assistance.
Conflict of interest
The authors have no financial or proprietary interests and have not received research funding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharma, R., Maharajan, P., Kotta, S. et al. Prediction of refractive outcome after cataract surgery using partial coherence interferometry: comparison of SRK/T and Haigis formulae. Int Ophthalmol 34, 451–455 (2014). https://doi.org/10.1007/s10792-012-9671-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-012-9671-9