Abstract
The purpose of this study is to determine whether pupillary dilation has any effect on anterior chamber flare measurements using a Kowa laser flare meter (FM-500) in patients with chronic anterior uveitis (CAU). Twenty-five eyes of 25 consecutive patients with CAU were assessed for anterior chamber inflammation by an experienced operator using the Kowa laser flare meter. Ten measurements were taken in total, with the highest and the lowest measurements deducted. The mean value and standard deviation was then recorded. One drop of tropicamide 1% and phenylephrine 2.5% was then applied and after 30 min the measurements were repeated and the results recorded. Sixteen women (64%) and nine men (36%) were recruited. The majority of patients were white Caucasian (68%). Fifteen left and ten right eyes were studied and the median (interquartile range: IQR) visual acuity was 6/9 (6/6–6/18). Iris colour was classified as brown, blue, grey/hazel and hazel. Thirteen eyes (52%) had brown irises, eight (32%) had blue, two had grey and the remainder were grey/hazel and hazel. The mean (SD) age was 50.8 (12.59) years. The median (IQR) flare reading before dilation was 17.93 (8.33–29.93) and after dilation was 15.97 (10.17–29.4). The mean change was −0.74 which was not a statistically significantly different to 0 (P = 0.25) and the 95% limits of agreements ranged from −6.91 to 5.43. This study showed little evidence of any systematic difference between dilated and undilated flare measurements. The measurement of flare was not affected by the dilation of the pupil and measurements could be taken before or after papillary dilation for the purpose of patient follow-up data and clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Establishing the presence of protein particles in the aqueous humour plays an important role in the management of patients with anterior uveitis. The blood–aqueous barrier, a selectively permeable barrier formed by the non-pigmented layer of the epithelium of the ciliary body and the endothelium of the blood vessels of the iris, normally prevents the passage of protein to the aqueous [1]. However, a reduction in the rate of aqueous flow or disruption to the blood–aqueous barrier will cause protein to leak from the blood vessels of the inflamed iris or ciliary body and result in an increase of protein components in the aqueous. This is clinically characterised as flare and in severe cases may give the aqueous a cloudy or milky appearance.
Measuring anterior chamber inflammation is an essential part of assessing any patient with uveitis. Evaluation of flare and cell activity by means of slit-lamp biomicroscopy, is the most commonly used and recognised method available for measuring anterior chamber inflammation, but previous studies have shown results with low levels of reproducibility [2].
The Kowa laser flare meter (FM-500) is a non-invasive method developed for concurrent quantitative determination of protein concentration (flare) in the aqueous humour. The instrument consisting of a diode laser, with a 650 nanometre (nm) wavelength, determines the amount of flare by measurement of light scatter, detected by photomultipliers within the device [3, 4]. The amount of light detected is then scanned across a sampling window (0.3 mm × 0.5 mm), over a 0.5 s interval and records two background readings as the laser scans above and below the window. To obtain results, background measurements are averaged and subtracted from the sampling window to provide a laser flare photometry measurement. The flare is expressed as photon counts per millisecond (ph/ms). This method provides minimal patient co-operation and studies have demonstrated the technique to be fast, highly sensitive and reproducible [2, 5].
Previous studies have, however, demonstrated that laser flare photometry values can be altered and influenced by non-disease factors, which affect aqueous protein levels and the amount of reflective light from the anterior chamber. One such factor is the effect of mydriatic agents and pupil size on aqueous flare [6–12]. These studies have shown a relatively small decrease of 10–20% in laser flare values after dilation in normal subjects. This reduction is also observed in pseudophakic eyes [13].
The objective of this prospective study was to determine whether pupillary dilation has any effect on anterior chamber flare measurements using a Kowa laser flare meter (FM-500) in patients with chronic anterior uveitis (CAU). This is important for the timing of such measurements, i.e. before or after dilation, and may also have implications in research protocols.
Methods
Twenty-five patients were selected from the Uveitis Clinic at Moorfields Eye Hospital. The study was approved by the Local Ethics Committee. All subjects were given a full explanation of the study and a signed consent was obtained from each patient prior to enrolment. All subjects were enrolled according to the Declaration of Helsinki. Inclusion criteria included subjects of either gender, aged 18 years or over and clinically diagnosed with CAU. Exclusion criteria included any significant corneal opacities/abrasions and posterior synechiae.
One eye from each patient affected by CAU was used in the study. If both eyes were diagnosed with CAU, the eye which was recorded as the most effected, was selected for the study. Standardized data collection forms were produced to record age, ethnicity, iris colour, pupil size and measurements of flare pre- and post-dilation.
Anterior chamber inflammation was assessed by an experienced operator, using the Kowa laser flare meter (FM-500) to the non-dilated study eye. Ten measurements were taken in total, with the highest and lowest measurements deducted as detailed in the instruction manual supplied by Kowa Ltd Industries. The mean value and standard deviation was then documented. One drop of tropicamide 1% and phenylephrine 2.5% was applied to the study eye. After a total of 30 min, the measurements were repeated and the results recorded.
Bland–Altman methods were used to assess agreement between flare readings with 95% limits of agreement being computed (mean difference pre- and post-dilation ±1.96 standard deviation of differences). A paired t-test was conducted to assess evidence of systematic bias. All analyses were conducted using Intercooled Stata 9.0 for Windows.
Results
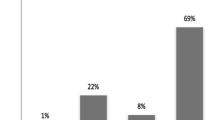
Sixteen women (64%) and nine men (36%) were recruited. The majority of patients were white Caucasian (68%). Fifteen left and 10 right eyes were studied and the median (interquartile range: IQR) visual acuity was 6/9 (6/6–6/18). Iris colour was classified as brown, blue, grey/hazel and hazel. Thirteen eyes (52%) had brown irises, eight (32%) had blue, two had grey and the remainder were grey/hazel and hazel. The mean (SD) age was 50.8 (12.59) years.
The median (IQR) flare reading before dilation was 17.93 (8.33–29.93) and the one after dilation was 15.97 (10.17–29.4). Two patients had extremely high readings both before and after dilation, as shown in Fig. 1.
Figure 2 shows that some patients’ flare readings decreased after dilation, whilst for others, readings increased. The mean change was −0.74 which was not statistically significantly different to 0 (P = 0.25) and the 95% limits of agreements ranged from −6.91 to 5.43.
Discussion
Previous studies have shown that anterior chamber flare measurements, performed by the laser flare meter, provide validity and reproducibility when using this technique.
One study by El-Harazi et al., where measurements were taken by two experienced operators on eyes with varied degrees of inflammation, together with eyes with no pathology, concluded that the intra-observer and inter-observer reproducibility was excellent. However, the results did not determine whether these findings would be applicable in eyes with much higher flare readings.
Studies conducted by Shah et al. have shown that the slight decrease in flare photometry readings after papillary dilation may be an artefact. They demonstrated that readings taken by the flare meter reduced in value due to the reduction of light scatter when the iris was moved away from the scanning window.
Other evidence given to explain this reduction in photometry values have focused on pharmacological effects of the mydriactic agent. Oshika et al. concluded from their study that photometry values continue to decrease after maximal pupil dilation had already occurred, due to reduction in blood–aqueous barrier permeability.
No evidence has been offered to suggest that either pupil size or colour influences these readings.
Our study has shown little evidence of any systematic difference between dilated and undilated flare measurements. Some patients showed an increase in flare after dilation whilst others showed a decrease with an average change of just −0.74 ph/ms. The limits of agreement ranged from −6.91 to 5.43, so that for the majority of patients the difference between measurements will be no greater than 7 ph/ms, which offers no clinical significance.
In conclusion, the flare measurements taken on our cohort of patients was not affected by the dilation of the pupil, proving that measurements could be taken before or after papillary dilation. However, the median flare measurement for the study group was relatively low. Further studies are needed to assess the degree and significance of change in subjects with a much higher recorded level of flare pre- and post-dilation.
References
Hogan MJ, Kimura SJ, Thygeson P (1959) Signs and symptoms of uveitis. I. Anterior uveitis. Am J Ophthalmol 47:155–170
El-Harazi SM, Feldman RM, Chuang AZ, Ruiz RS, Villanvera G (1998) Reproducibility of the laser flare meter and laser cell counter in assessing anterior chamber inflammation following cataract surgery. Ophthalmic Surg Lasers 29:380–384
El-Maghraby A, Marzouki A, Matheen TM, Souchek J, Van der Karr M (1992) Reproducibility and validity of laser flare/cell meter measurements as an objective method of assessing intraocular inflammation. Arch Ophthalmol 110:960–962
El-Harazi SM, Ruiz RS, Feldman, Chuang AZ, Villanuera G (2002) Quantitative assessment of aqueous flare; the effect of age and papillary dilation. Ophthalmic Surg Lasers 33:379–382
Ladas JG, Wheeler NC, Morhun PJ, Rimmer SO, Holland GN (2005) Laser flare-cell photometry: methodology and clinical applications. Surv Ophthalmol 50:27–47
Oshika T, Kato S, Inamochi K, Mori M, Araie M (1989) Aqueous flare and cells after mydriasis in normal human eyes. Nippon Ganka Gakkai Zasshi 93:698–704
Osogera T, Gimbal HV, DeBroff BM (1993) Aqueous flare and cell number on healthy eyes of Caucasians. Jpn J Ophthalmol 37:447–451
Oshika T, Kato S (1989) Changes in aqueous flare and cell after mydriasis. Jpn J Ophthalmol 33:271–278
Oshika T, Nish M, Mochizuki M et al (1989) Quantitative assessment of aqueous flare and cells in uveitis. Jpn J Ophthalmol 33:279–287
Petternel V, Findl O, Kruger A et al (2000) Effect of tropicamide on aqueous flare before and after cataract surgery. J Cataract Refract Surg 26:382–385
Sawa M, Tsurimaki Y, Tsura T et al (1988) New quantitative methods to determine protein concentration and cell numbers in aqueous in vivo. Jpn J Ophthalmol 32:132–142
Shah SM, Spalton DJ, Smith SE (1991) Measurement of aqueous cell and flare in normal eyes. Br J Ophthalmol 7:57
Chin PK, Cuzzani OE, Gimbel HV, Sun RE (1996) Effect of commercial dilating agents on laser flare-cell measurements. Can J Ophthalmol 31:362–365
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ikeji, F., Pavesio, C., Bunce, C. et al. Quantitative assessment of the effects of pupillary dilation on aqueous flare in eyes with chronic anterior uveitis using laser flare photometry. Int Ophthalmol 30, 491–494 (2010). https://doi.org/10.1007/s10792-010-9373-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-010-9373-0