Abstract
Purpose To describe the clinical and histopathologic finding of very limited ophthalmic Wegener granulomatosis (WG). Methods Thirteen patients with scleritis, orbitopathy, episcleritis, and panuveitis were studied. They presented without evidence of lung or kidney disease, though eight had sinus involvement. We reviewed the biopsies for histopathologic findings consistent with WG, and tested for antineutrophil cytoplasmic antibodies antineutrophil cytoplasmic antibody (ANCA). Results WG was suggested by granulomatous foci, collagen necrosis, neutrophils/nuclear dust, plasma cells and infiltrating eosinophils. Granular degeneration of the interstitial collagen; mummification of the collagen with disappearance of fibroblastic nuclei; and a polymorphous infiltrate exhibiting plasma cells, lymphocytes, neutrophils, and eosinophils within the epithelioid granulomas should suggest the diagnosis. ANCA test results supported the diagnosis of WG in all cases. Conclusion The described histologic characteristics are highly suggestive of WG. These findings along with clinical or laboratory findings, allow the diagnosis of very limited ophthalmic WG in the absence of systemic involvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Wegener granulomatosis (WG) has been classically described as a systemic vasculitis, with the brunt of the destructive inflammation borne by the sinuses, upper respiratory passages, lungs, and kidneys [1–4]. The classic criteria of generalized focal granulomatous necrotizing vasculitis of both small arteries and veins affecting the lungs, upper respiratory tract, and kidneys (glomerulitis characterized by necrosis and thrombosis) were suggested in 1954 by Godman and Churg [4]. Numerous classification schemes for the various vasculitic syndromes have been proposed, based on different criteria, e.g., vessel type, demographics, immune complexes, organ tropism, and antibodies; but suffice it to say that all have had shortcomings, and that diagnostic criteria have also remained elusive [5]. Carrington and Liebow proposed the term limited WG for patients who presented with pulmonary lesions identical to those seen in patients with WG but without renal involvement [6, 7].
Prior to the advent of antineutrophil cytoplasmic antibody (ANCA) testing, the diagnosis of WG relied entirely on the interpretation of clinical and histologic findings. Based on antibodies against the 29-kd protein found in the α-granules in granulocytes and monocytes, the resultant cytoplasmic staining pattern has been found to be 93% sensitive and 97% specific for WG [8, 9]. The c-ANCA measures antibody to neutrophil serine proteinase; p-ANCA corresponds to antibody directed against lyzosomal enzymes, lactoferrin, or myeloperoxidase. Recent reports indicate that there is increased constitutive expression of neutrophil proteinase in patients with vasculitis; and that this correlates with disease severity and the development of relapses [10].
The prompt diagnosis of WG, even the very limited ophthalmic variant, should lead to the early introduction of appropriate therapy, with the objective of preventing progression of the disease and systematization. We report herein a group of 13 patients who presented initially with a primary focus of inflammation centered in the sclera, episclera, or orbit (including the lacrimal gland), often with accompanying sinus disease. We identified, in a review of the pathologic specimens obtained from our 13 patients, some distinctive histopathologic features which should stimulate strong suspicion for WG, prompt the performance of an ANCA serologic test [7, 11–13], and raise the consideration of therapy appropriate for WG, thus preventing disease progression and systemization.
Materials and methods
IRB approval for this study was obtained; and informed consents were obtained from the patients involved. Then, 25 patients diagnosed with WG through the immunology and the pathology services at the Massachusetts Eye and Ear Infirmary from 1985 to 1992 were reviewed. Seven patients whose signs and symptoms were limited to the eye or orbit at the time of presentation were identified. Two additional patients with similar findings and histories from the University of Iowa, one from the University of South Florida, one from Washington University in Saint Louis, one from the Armed Forces Institute of Pathology, and one from the Medical College of Wisconsin were also reviewed; all of their study specimens were analyzed at the infirmary. The study was conducted as a retrospective case series.
Biopsy specimens, radiologic studies, and ANCA test results from these latter 13 patients with limited ophthalmic/orbit/sinus disease were reviewed, along with biopsy specimens from patients with idiopathic orbital pseudotumor and from patients with necrotizing scleritis secondary to rheumatoid arthritis and relapsing polychondritis. The specimens were evaluated by one of us (FAJ) in a masked fashion in an effort to determine whether or not the histopathological characteristics would consistently be so suggestive of limited ophthalmic WG as to represent a distinctive pattern worthy of reporting. Acid fast and gomori methenamine stains were performed on the biopsies. All patients underwent laboratory evaluations which included chest and sinus X-ray, urine analysis, complete blood count, blood chemistries, erythrocyte sedimentation rate, anti-nuclear antibody titer, rheumatoid factor, and ANCA testing.
Results
The ages of the 13 patients with limited ophthalmic WG at the time of diagnosis ranged from 19 to 82 years (median: 55 years) (Table 1). Seven patients were female. The duration of symptoms ranged from 1 month to 8 years (median = 9 months). Two patients presented with inflammation limited to the sclera. One patient presented clinically with episcleritis and had scleritis in addition to conjunctivitis on biopsy (Fig. 1a). One patient had sinusitis and orbitopathy (Fig. 2a, b) preceding the scleritis; the patient was initially diagnosed as having lethal midline granuloma with severe sinus disease resulting in saddle nose deformity.
Montage of clinical and histopathology illustrations; ANCA positive limited ophthalmic Wegener granulomatosis: (First row, left) This image shows moderate diffuse episcleritis in a patient with limited ophthalmic Wegener granulomatosis. Note additionally, the white peripheral corneal infiltrates superiorly, inferiorly, and temporally, signifying peripheral interstitial keratitis in addition to the episcleritis (case 1). (First row, right) Photomicrograph of conjunctival and episcleral biopsy specimen from case 1, showing granulomatous inflammation, with lymphocytes, plasma cells, epithelioid cells, and multi nucleated giant cells, along with eosinophils. Nuclear dust can also be appreciated. Hematoxylin and eosin 640X. (Second row, left) Histopathology specimen from scleral biopsy from case 1. Note the eosinophilic collagen, the nuclear dust scattered throughout the specimen, and the island of basophilia, typical of collagen necrosis. Hematoxylin and eosin, 640X. (Second row, right) Another biopsy specimen illustrating collagen mummification (*), with loss of nuclear detail from fibroblasts(case 6) Hematoxylin and eosin, magnification 640X. (Third row, left) Illustrated here is another area of the scleral biopsy from case 1, with areas of obvious occlusive vasculitis (black arrows). Hemotoxylin and eosin, magnification 640X. (Third row, right) Scleral biopsy specimen from case 5. Note the granulomatous inflammation and pronounced tissue eosinophilia (black arrow without tail). Note also the multi nucleated giant cell (black arrow with tail), and the ephithelioid cells (red arrow). Hematoxylin and eosin, 640X. (Fourth row, left) Scleral biopsy specimen from case 5. Note the extensive nuclear dust in this area of collagen necrosis. Hemotoxalin and eosin, magnification 640X. (Fourth row, right) Scleral biopsy from case 1. Note the chronic granulomatous inflammation with epithelioid cells and multinucleated giant cells, lymphocytes, plasma cells, and numerous eosinophils. Hemotoxalin and eosin 640X
Computed tomography scans from a patient with ANCA positive limited ophthalmic Wegener granulomatosis: (Top) CT scan of a patient not specifically mentioned. Note the opacification of the ethmoid sinuses and the radio dense inflammatory material in the right orbit. (Bottom) Coronal section, same patient as shown in figure 2A, providing a different view of the ethmoid sinus opacification and the right orbital inflammatory material confined to the medial aspect of the orbit
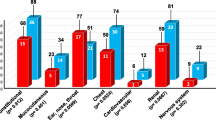
Nine patients had orbital inflammation. Five had orbitopathy without sinus involvement; two of these began as dacryoadenitis, and one presented as an orbital apex mass. Delayed sinus inflammation occurred in a third patient with dacryoadenitis and in two others with orbititis. One patient presented with panuveitis and a rapid evolution of orbital and sinus inflammation. Three patients had orbital inflammation without lacrimal gland or sinus involvement. Two patients had sinusitis without orbital involvement. One of these progressed to massive intraocular inflammation and uveal mass simulating uveal melanoma with extrascleral extension. Anterior segment manifestations included scleritis (six patients), peripheral ulcerative keratitis (five patients), and conjunctivitis (five patients).
Biopsy specimens included sclera (7), sinus (4), nasal mucosa (2), lacrimal gland (3), orbital apex (2), and one exenteration. All specimens demonstrated varying degrees of granulomatous inflammation as evidenced by either giant cells or epithelioid cells (Fig. 1b) (Table 2). Many specimens had frank extravascular granulomas. Special stains for bacteria and fungi were negative. Variable amounts of ischemic necrosis in the form of granular collagen necrosis (Fig. 1c) or mummification (Fig. 1d), loss of nuclei with faintness of the matrix eosinophilia, were present in 12 cases. Some specimens had granulomatous inflammation surrounding, but not involving blood vessels. One case had obvious granulomatous vasculitis (Fig. 1e). Four cases demonstrated clear-cut necrotizing vasculitis, some with lumen obliteration (Fig. 3). In three cases, eosinophils were found percolating around and within scattered granulomatous foci (Fig. 1f).
An impressive polymorphous inflammatory infiltrate was present in all cases, with numerous neutrophils or their nuclear dust from degenerated cells (Fig. 1g). All cases had myriad plasma cells, prominently admixed with granulomatous inflammation (Fig. 1h).
The presenting symptoms and visual acuities of most patients improved with therapy (Table 3). The following three case summaries highlight the variable clinical findings and possible progression of the disease.
Selected case reports
Case 1 -- scleritis
A 55-year-old man presented with a two-month history of conjunctival injection of the right eye. At another clinic his scleritis was treated with topical steroids and non-steroidal antiinflammatory drugs. Examination at the Massachusetts Eye and Ear Infirmary revealed necrotizing scleritis in the right eye. The patient's visual acuity was 20/60 in the right eye and 20/20 in the left eye (Fig. 4).
Scleral and conjunctival biopsies revealed numerous multinucleated giant cells and a palisading giant cell. Perivasculitis was seen with epithelioid cells surrounding a vessel. There was evidence of collagen necrosis and nuclear dust suggesting an aggressive ischemic process (Fig. 1c). Eosinophils and mast cells were prominent (Fig. 1h). Lung and renal examinations were normal. The patient’s ANCA level was elevated at 34 SLI units (normal less than 20 SLI units).
The scleritis improved with cyclophosphamide and prednisone treatment. After 3 months of therapy the ANCA level had fallen to two. The scleritis resolved and visual acuity had improved to 20/40 in the affected eye. The patient’s ANCA remained in the normal range over the next year, as the patient continued on cyclophosphamide therapy. Active scleritis developed 1 year after the initiation of therapy, as cyclophosphamide was tapered, with visual acuity falling to 20/400. The patient’s ANCA remained normal during this episode. Indomethacin by mouth was added. The scleritis improved without increasing the dose of cyclophosphamide.
Case 5 – orbitopathy
A 51-year-old man with a history of asthma since age 5, right occipital aneurysm rupture in 1962, and recurrent dacryocystitis (three dacryocystorhinostomies on each side from 1970 to 1984) presented to outside specialists with upper respiratory symptoms and right otitis media. Sinus films were normal.
About 10 days after oral antibiotics were started, the patient returned with pain and proptosis of the right eye. Vision was not affected. Computed tomography revealed orbital inflammation. The patient was hospitalized, and he had minimal response to intravenous corticosteroids and nafcillin (one of six blood cultures grew coagulase negative staphylococcus). One week later new onset pansinusitis with severe ethmoidal involvement was noted on repeat computed tomography. Two weeks after admission to an outside hospital the patient had increased pain, proptosis, and lid edema despite intravenous methylprednisolone and cephazolin.
On transfer to the Massachusetts Eye and Ear Infirmary, the patient’s initial visual acuity was 20/20 in the right eye and count fingers temporally in the left eye, color vision was normal. There was a left exotropia and restriction in adduction in the right eye. The right eye had 3 mm of proptosis, no afferent pupillary defect and marked diffuse conjunctival injection. Computed tomography suggested right ethmoid sinus opacification and medial orbital abscess (Fig. 5).
Tissue from an anterior orbitotomy on hospital day two revealed only fibrous connective tissue. Cultures for bacteria and fungi were negative, as were stains for acid fast bacteria. Three days later an impressive increase in sphenoid and ethmoid inflammation required ethmoidectomy and sphenoidectomy on hospital day five. Pathology revealed granuloma formation with vessel lumen obliteration, accompanied by neutrophils, multinucleated giant cells, eosinophils and mast cells. Nuclear dust and collagen degeneration were present.
A systemic evaluation conducted during the patient’s rapidly evolving orbital inflammation revealed normal renal function and a normal chest X-ray. ANCA level was elevated (74 with normal less than 20 SLI units). The orbitopathy improved on systemic steroids and cyclophosphamide.
Case 6 – dacryoadenitis
A 55-year-old white man developed conjunctivitis, corneal infiltrates, swelling of the lacrimal gland, and ptosis in the left eye. Two weeks later, he developed a low grade fever, increasing left periorbital edema and erythema unresponsive to antibiotics. A week later upper respiratory symptoms and epistaxis prompted hospital admission at an outside hospital. Computed tomography revealed an air-fluid level in the right maxillary sinus, opacification of the ethmoid air cells, and an enlarged left lacrimal gland.
Ancillary studies demonstrated normal renal function and mild anemia. A liver biopsy obtained to investigate elevated liver alkaline phosphatase revealed only minimal mononuclear cell infiltrate and no evidence of granulomas. Chest radiography showed no evidence of granulomatous disease. Biopsies of right nares, right inferior turbinate, and left conjunctiva and left lacrimal gland were not felt to be diagnostic at the outside institution.
The patient responded dramatically to intravenous steroid therapy and was discharged on prednisone and topical steroid drops. Two months later, in consultation at the Massachusetts Eye and Ear Infirmary, visual acuity was 20/25 in each eye. There was ptosis of the left upper lid, and the left lacrimal gland was enlarged and tender. Slit lamp examination of the left eye revealed episcleritis, mild iritis, corneal pannus and thinning of the peripheral cornea.
Review of the original ethmoid biopsy was suggestive of WG, exhibiting eosinophils, florid granulomatous inflammation in the interstitium and areas of stellate collagen necrosis with nuclear dust suggesting vascular insufficiency. Areas of mummified collagen (loss of fibroblast nuclei and disrupted, poorly staining collagen lamellae) were evident (Fig. 1d). No large caliber vessel with mural vasculitis was found in the available slides. An elevated ANCA test suggested the diagnosis of limited WG (23 with normal less than 20 SLI units).
Three months after diagnosis, the patient had improved on a regimen of prednisone and trimethoprim-sulfamethoxazole. But systemic cyclophosphamide was added for persistence of inflammation, resulting in gradual resolution of dacryoadenitis, sinusitis, orbitopathy, and stabilization of peripheral corneal thinning. Prednisone was discontinued 8 months after its initiation. Cyclophosphamide was discontinued after 1 year of therapy; the patient has been maintained on trimethoprim-sulfamethoxazole alone. The patient’s ANCA normalized with treatment and the patient has remained stable 3 years after the initiation of therapy.
Discussion
Classic WG typically has its onset during the fourth and fifth decades, but has been reported in the elderly and (rarely) in children [11]. There is no sexual or racial predilection [12]. Kuchel and Lee have described a localized cutaneous form of WG, analogous to our report of highy localized ophthalmic WG [14].
Eye involvement is common in patients with WG, and it may be the sole presenting sign, or the feature allowing diagnosis, as it was in each of our cases [13, 15]. In a prospective clinical and therapeutic study of WG, Fauci and others [16] noted 16% of patients had ocular inflammation (conjunctivitis, uveitis, episcleritis, or scleritis) at the time of presentation; seven percent presented with proptosis as an initial sign [16]. Eye involvement eventually developed in 58% of the patients [16].
Sclerouveitis and marginal keratitis (seen in seven of our 13 cases) are frequently the initial ophthalmic manifestation of WG, but are usually accompanied by clinical or radiological evidence of upper and lower respiratory involvement at the time of presentation [1, 17–19]. The orbit may be affected primarily, as in seven of our cases, or may be involved secondary to invasion of granulomatous inflammation from adjacent sinuses, as in two other cases in our series. It is unusual for orbital inflammation to precede respiratory tract involvement by more than a few months [20, 21], even in cases without apparent sinus disease. Lacrimal duct obstruction, although present in 25% of patients, is usually a late manifestation [20, 22]. WG has been reported to present as dacryoadenitis, similar to our cases 6, 7, and 10 [23].
Wegener emphasized that the pathologic changes seen in the classic form of the disease are not those of a primary vasculitis [2, 24]. McCluskey and Feinberg observed that independent areas of extravascular necrotizing granulomatous lesions account for much of the tissue destruction, especially in pulmonary disease [25]. Purely granulomatous disease (without classic vasculitis) has been proposed as an early and sometimes the only manifestation of WG [24, 26].
While the discovery of granulomatous vasculitis of muscular vessels and interstitial granulomas are hallmarks of the diagnosis of WG, we emphasize here other histopathologic findings which we believe have been under appreciated in the past. And while not pathognomonic of the disease, the finding of these features ought to heighten one’s suspicion of WG. The first of these features is alteration of the interstitial collagen, which can appear as a granular degeneration, linear or stellate necrosis, or complete mummification of the collagen (effaced fibrillarity and eosinophilia) with loss of the fibroblastic nuclei. We suspect that these findings are the result of a vaso-obliterative focus outside the plane of the section [27].
Another important feature is the richly polymorphous nature of the inflammatory infiltrate, which typically features plasma cells, lymphocytes, neutrophils, eosinophils, and dispersed or clustered epithelioid histiocytes. The polymorphonuclear leukocytes may show dissolution of their outlines (leukocytoclasis), resulting in the formation of “nuclear dust”. The propensity of the eosinophils to be scattered throughout the infiltrate, and most distinctively to be intimately admixed within the formed granulomas and among the scattered epithelioid histiocytes, are findings not encountered in idiopathic orbital inflammations [28–30]. In our 13 cases of limited ophthalmic WG, ischemia was manifested as collagen necrosis in four of the five cases of scleritis and in all of the orbital cases. Remnants of neutrophils in the form of nuclear dust were frequently found in specimens affected by collagen necrosis.
Extravascular granulomas were present in two of the three cases where scleritis was the predominant feature of the disease. All five of the orbitopathy cases demonstrated granuloma formation or giant cells. Granulomatous perivasculitis (granulomas around a thin nonmuscular vessel with a large lumen, probably venular) was observed in one case of scleritis and in three orbital cases. True granulomatous vasculitis was observed in muscular vessels in four orbital specimens.
Our findings depart slightly from those reported by Kalina and associates [31], who reviewed orbital biopsies in 14 patients with systemic WG. They found small-vessel lymphocytic vasculitis in 85% of their patients; granulomatous inflammation of the vessel walls was exceptional. Because of the high frequency of vasculitis, tissue necrosis was also observed in 62% of specimens. While mononucleated epithelioid cells, sufficient to warrant the diagnosis of granulomatous inflammation, were detected in 62% of cases, multinucleated giant cells were found in only 31%; the latter were more apt to be found in nasal and sinus biopsies. The most commonly encountered combination of diagnostic histopathologic features was constituted in 31% of specimens by a triad of vasculitis, tissue necrosis, and granulomatous inflammation without giant cells. Eosinophils were less prominent in their series than in ours. It is virtually impossible to determine whether this represents a sampling difference, or reflects different histopathologic features in the subset of patients we are reporting (very limited ophthalmic WG without systemic involvement of the lungs or kidneys).
Our findings are, however, completely consistent with those reported by Perry and associates [32], who reviewed orbital biopsies in 11 patients with WG. They found a mixed inflammation with perivascular lymphocytes (10 of 11 patients), fat necrosis (11 of 11 patients), lipid-laden macrophages, microabscesses (2 of 11 patients), giant cells (five of 11 patients), and polymorphonuclear leukocytic eosinophilic infiltrates (10 of 11 patients). The authors emphasized the significance of the orbital biopsy in reaching the final diagnosis. However, only five of their patients were ANCA positive (all of our patients were ANCA positive) and five of their 13 patients had systemic symptoms (none of our patients had systemic manifestation of WG).
There are rare cases of primary orbital vasculitis unassociated with systemic disease, in which lymphocytes and eosinophils may be prominently featured (including within blood vessel walls), but in which granulomatous inflammation is not present [33]. An extremely rare entity, granulomatous polymyositis, manifests a multinucleated giant cell attack upon the extraocular striated muscle fibers, along with an infiltration of lymphocytes and eosinophils [33, 34]. In this disease there is also a cardiomyopathy which may be fatal. The closest simulator of limited ophthalmic WG is the Churg-Strauss syndrome, which involved tissues from the ocular adnexa that may be indistinguishable from what we have described in our biopsy material. But this entity, in comparison with WG, rarely affects the ocular adnexa [35] and is always accompanied by an eosinophilic pneumonitis.
It is important to realize in the evaluation of patients with disease limited to the eye or orbit that the sensitivity of ANCA testing has also been found to be dependent on disease severity. Nolle et al. found ANCA was positive in only 67% of active limited WG cases, compared to 96% in patients with active disseminated systemic disease [8]. Woo et al. also reported c-ANCA to be positive in only 32% (six of 19) of patients with limited WG compared to 90% (nine of 10) of patients with generalized disease [36]. We have previously reported on patients with limited WG who progressively evolved to systemic WG over the course of follow-up [15]. This concept of progressive evolution of WG with increased organ involvement is significant, since timely therapeutic intervention can prevent potential morbidity and mortality associated with active disease. A delay in diagnosis, for example, may contribute to a higher rate of severe WG manifestations, such as necrotizing scleritis with resultant loss of eye.
Cyclophosphamide and prednisone, as patient 1 and seven other patients in our study received, are the standard immunosuppressive agents for WG. Hoffman and associates found in their prospective study of 158 patients with WG that 91% of patients on this regimen achieved marked improvement or partial remission; 75% had complete remission [37].
A combination of suggestive biopsy results and ANCA testing as reported herein holds the best promise for accurate and early diagnosis of limited ophthalmic WG. Recognition of the constellation of pathologic findings found in our patients may be helpful in justifying the introduction of immunosuppressive therapy, which can prevent progression and systematization of WG.
References
Straatsma BR (1957) Ocular manifestations of Wegener granulomatosis. Am J Ophthalmol 44:789–799
Wegener F (1939) Uber eine eigenartige rhinogene Granulomatose mit besonderer Beteiligung des Arteriensystems under Nieren. Beitr Pathol 102:36–68
Kornblut AD, Wolff SM, deFries HO, Fauci AS (1982) Wegener’s granulomatosis. Otolaryngol Clin North Am 15:673–683
Godman GC, Churg J (1954) Wegener’s granulomatosis: pathology and review of the literature. AMA Arch Pathol 58:533–553
Saleh A, Stone JH (2005) Classification and diagnostic criteria in systemic vasculitis. Best Pract Res Clin Rheumatol 19:209–221
Carrington CB, Liebow AA (1966) Limited forms of angiitis and granulomatosis of the Wegener’s type. Am J Med 41:497–527
Cassan SM, Coles DT, Harrison EG Jr (1970) The concept of limited forms of Wegener’s granulomatosis. Am J Med 49:366–379
Nolle B, Specks U, Ludeman J et al (1989) Anticytoplasmic autoantibodies: their immunodiagnostic value in Wegener granulomatosis. Ann Intern Med 111:28–40
Tervaert JW, van der Woude FJ, Fauci AS et al (1989) Association between active Wegener’s granulomatosis and anticytoplasmic antibodies. Arch Intern Med 149:2461–2465
van Rossum AP, Limburg PC, Kallenberg CG (2003) Membrane proteinase 3 expression on resting neutrophils as a pathogenic factor in PR3-ANCA-associated vasculitis. Clin Exp Rheumatol 21:S64–S68
Wolff SM, Fauci AS, Horn RG, Dale DC (1974) Wegener’s granulomatosis. Ann Int Med 81:513–525
Jakobiec FA, Jones IS (1989) Orbital inflammations. In: Tasman W, Jaeger EA (eds) Duane’s clinical ophthalmology, Rev ed., vol 2, chap 35, JB Lippincott, Philadelphia
Coppeto JR, Yamase H, Monteiro MLR (1985) Chronic ophthalmic Wegener’s granulomatosis. J Clin Neuroophthalmol 5:17–25
Kuchel J, Lee S (2003) Cutaneous Wegener’s granulomatosis: a variant or atypical localized form? Australas J Dermatol 44:129–135
Harper SL, Letko E, Samson CM et al (2001) Wegener’s granulomatosis: the relationship between ocular and systemic disease. J Rheumatol 28:1025–1032
Fauci AS, Haynes BF, Katz P, Wolff SM (1983) Wegener’s granulomatosis: prospective clinical and therapeutic experience with 85 patients for 21 years. Ann Intern Med 98:76–85
Austin P, Green WR, Sallyer DC et al (1978) Peripheral corneal degeneration and occlusive vasculitis in Wegener’s granulomatosis. Am J Ophthalmol 85:311–317
Brubaker R, Font RL, Shepherd EM (1971) Granulomatous sclerouveitis. Regression of ocular lesions with cyclophosphamide and prednisone. Arch Ophthalmol 86:517–524
Foster CS, Yee M (1983) Corneoscleral manifestations of Grave’s disease, the acquired connective tissue disorders, and systemic vasculitis. Int Ophthalmol Clin 23:131–157
Bullen CL, Liesegang TJ, MacDonald TJ, DeRemee RA (1983) Ocular complications of Wegener’s granulomatosis. Ophthalmology 90:279–290
Jakobiec FA (1979) Disease of the orbit (pp 216–271). New York, Harper & Row
Hardwig PW, Bartley GB, Garrity JA (1992) Surgical management of nasolacrimal duct obstruction in patients with Wegener’s granulomatosis. Ophthalmology 99:133–139
Leavitt JA, Butrus SI (1991) Wegener’s granulomatosis presenting as dacryoadenitis. Cornea 10:542–545
Wegener F (1936) Über generalisierte, septische Gefässerkrankungen. Verh Dtsch Ges Pathol 29:202–210
McCluskey RT, Fienberg R (1983) Vasculitis in primary vasculitis, granulomatoses, and connective tissue diseases. Hum Pathol 14:305–315
Boudes P (1990) Purely granulomatous Wegener’s granulomatosis: a new concept for an old disease. Semin Arthritis Rheum 19:365–370
Fienberg R (1981) The protracted superficial phenomenon in pathergic (Wegener’s) granulomatosis. Hum Pathol 12:458–467
Sergott RC, Felbert NT, Savino PJ et al (1981) The clinical immunopathology of Graves’ orbitopathy. Ophthalmology 88:484–487
Jellinek EH (1969) The orbital pseudotumor syndrome and its differentiation from endocrine exophthalmos. Brain 92:35–58
Davies GB, Wong PL (1958) Sclerosing lipo-granuloma in the orbit. Br J Ophthalmol 42:697–701
Kalina PH, Lie JT, Campbell RJ, Garrity JA (1992) Diagnostic value and limitations of orbital biopsy in Wegener’s granulomatosis. Ophthalmology 99:120–124
Perry SR, Rootman J, White VA (1997) The clinical and pathologic constellation of Wegener granulomatosis of the orbit. Ophthalmology 104:683–694
Mastaglia FL, Ojeda VJ (1985) Inflammatory myopathies: part 2. Ann Neurol 17:317–323
Kattah JC, Zimmerman LE, Kolsky MP et al (1990) Bilateral orbital involvement in fatal giant cell polymyositis. Ophthalmology 97:520–525
Churg J, Strauss L (1951) Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol 27:277–301
Woo TL, Francis IC, Wilcsek GA, Coroneo MT, McNab AA, Sullivan TJ (2001) Australasian orbital and adnexal wagener’s study group. Australasian orbital and adnexal Wegener’s granulomatosis. Ophthalmology 108:1535–1543
Hoffman GS, Kerr GS, Leavitt RY et al (1992) Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 15(116):488–498
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahmed, M., Niffenegger, J.H., Jakobiec, F.A. et al. Diagnosis of limited ophthalmic wegener granulomatosis: distinctive pathologic features with ANCA test confirmation. Int Ophthalmol 28, 35–46 (2008). https://doi.org/10.1007/s10792-007-9109-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-007-9109-y