Abstract
Objective
To assess the long-term results of intraoperative mitomycin C (MMC) in external dacryocystorhinostomy (EXT-DCR).
Methods
In this prospective randomized controlled study, 35 patients (40 eyes) with primary acquired nasolacrimal duct obstruction were assigned randomly into two groups. In the control group, a standard EXT-DCR procedure was performed. In the MMC group 0.2 mg/ml MMC was applied to the osteotomy site for 30 min. The results of EXT-DCR in both groups were evaluated by both asking patients about the tearing condition and examining the patency of irrigation at one-year follow up.
Results
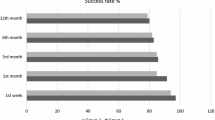
Eighteen (90%) of the 20 eyes in the MMC group remained totally symptom-free and one eye (5%) improved; while 12 (60%) of 20 eyes in the control group were reported to be symptom-free and five (25%) of the eyes to have an improvement in the tearing symptoms (P = 0.087). The success rate in the MMC group was 95% compared with 85% in the control group (P = 0.605). No surgical complications occurred.
Conclusions
The satisfaction and success rates of the MMC group were higher than those of the control group and no deleterious effect was noted with MMC application, however the differences did not reach statistical significance. Intraoperative MMC application seems to be a safe adjuvant that could help in increasing the success rates of EXT-DCR surgery in primary acquired nasolacrimal duct obstruction ,however further studies with larger series are needed to make definite statements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
EXT-DCR has been the standard therapy for nasolacrimal duct obstruction in managing epiphora [1]. A review of the literature reveals a success rate of approximately 90% [2–4]. Obstruction of common canaliculus and osteotomy site by granulation tissue has been reported as the most frequent cause for failure in EXT-DCR [5, 6]. Thus if fibrous tissue growth and scarring over the anastomosed flaps and osteotomy site could be inhibited, the success rate might be increased during DCR surgery.
MMC, derived from Streptomyces caespitosus, is an alkylating antibiotic. It reduces fibroblast collagen synthesis by inhibiting DNA-dependent RNA synthesis. Application of MMC was found to be effective on subconjunctival fibroblasts for the prevention of excessive scar formation [7]. It has been widely used as an antiproliferative agent in pterygium excision and glaucoma surgery [8, 9].
Hu et al. [10] observed the effects of MMC on cultured human nasal mucosa fibroblasts using 0.1–0.4 mg/ml of MMC for 1–5 min. They showed that MMC could inhibit the proliferation of cultured nasal mucosa fibroblasts and also induce apoptosis of fibroblasts. Yalaz et al. [11] evaluated the effects of antiproliferative agents (MMC and 5-flourouracil) on the fibrous tissue responsible for the failure of EXT-DCR at the site of surgical rhinostomy. The light and electron microscopic examination of the cases given antifibroblastic agents revealed a decrease in fibroblastic activity predominantly with hypo- and acellular areas. It might be postulated that adjunctive use of MMC over the osteotomy site and anastomosed flaps in DCR surgery could inhibit scarring and granulation tissue formation around the osteotomy site or common canaliculus and enhance the success of DCR surgery.
In this prospective study, we evaluated the long-term success rate of EXT-DCR surgery with intraoperative MMC application.
Methods
Thirty-five patients with a diagnosis of primary acquired nasolacrimal duct obstruction were assigned randomly into an MMC EXT-DCR group (MMC group) and conventional EXT-DCR group (control group). In five patients with bilateral nasolacrimal duct obstruction, EXT-DCRs were performed in both eyes on separate dates and one eye received MMC application, whereas the other eye did not. All patients had radiological assessment with dacryocystography and underwent endoscopic nasal examination. Only two patients with deviation of nasal septum underwent a deviation operation before the EXT-DCR surgery. Patients who had previous DCR surgery were not included in the study. All patients were followed for more than one year for the evaluation of subjective symptoms and objective findings. Institutional ethical board approval was taken and informed consent was obtained from all the patients.
A standard surgical technique of EXT-DCR under local anesthesia was used in all patients in both groups. Local infiltrative anesthesia consisting of 2% lignocaine (lidocaine, Pharmaceutical Co. Ltd.), 0.75% bupivacaine and 1:100.000 adrenaline (epinephrine), was administered in the region of the medial canthus and lower eyelid in all patients. The nasal mucosa was anesthetized and vasoconstricted with a pledget saturated with a mixture of approximately 2 ml of 5% cocaine and 1:100.000 adrenaline. An incision of approximately 2 cm in length was marked over the anterior lacrimal crest, starting just below the medial canthal tendon. The skin incision was created and blunt dissection was performed until the periosteum overlying the anterior lacrimal crest was exposed. The periosteum was incised and elevated off the lacrimal sac fossa. The osteotomy was created over the lacrimal sac fossa with an electric drill. The lacrimal sac was opened in a longitudinal fashion to form anterior and posterior flaps. The nasal mucosa was cut with sharp-tipped scissors to form anterior and posterior mucosal flaps. Then, the posterior nasal and lacrimal sac flaps were joined with 5-0 Vicryl sutures. In the MMC group, a piece of 0.5 × 0.5 cm neurosurgical cottonoid with long silk strings saturated with 1 ml of 0.2 mg/ml MMC was placed over the anastomosed posterior flaps and osteotomy site. We let the long silk protrude from the nasal cavity. The anterior nasal and lacrimal sac flaps were closed with 5-0 Vicryl sutures, in addition to closing the periosteum and orbicularis muscle in separate layers. The skin incision was closed with a running 6-0 Prolene suture. The MMC-soaked cottonoid was removed transnasally by pulling out the long silk in the recovery room after an application time of 30 min. In the control group, the same surgical procedures were performed except for the MMC application. Postoperatively both topical and oral antibiotics were used for seven days. The skin sutures were removed in 5–7 days.
The results of EXT-DCR surgery in both groups were evaluated by both asking patients about the tearing condition and examining the patency of irrigation at one-year follow up after the operation. The surgical procedure was considered as successful if the patients had no symptoms or improvement in tearing, and the lacrimal drainage system was proved to be patent by irrigation; whereas no improvement in tearing or constant epiphora and non-patent irrigation was considered as failure. The same physician, who did not know whether the patient received MMC application during the surgery, documentated subjective symptoms and objective findings. In the case of failure, transnasal endoscopy was performed to evaluate the cause of obstruction.
A Student’s t test was used to compare the means and Fisher’s exact χ 2 test was used to compare the results of DCR surgeries for both groups.
Results
A total of 40 primary EXT-DCRs were performed in this study; 20 eyes were in the MMC group and the remaining 20 eyes were in the control group. The mean (± SD) age of the MMC group was 41.2 ± 11.5 years and that of the control group was 39 ± 7.5 years. There was no significant difference in age between the two groups (t test, P > 0.05). The patients were followed up for 12–19 months (mean 15.8 months).
Eighteen eyes (90%) in the MMC group remained symptom-free (no tearing) and one eye (5%) improved after one-year follow up. Only, one eye (5%) in the MMC group had excessive tearing. In the control group, three eyes (15%) had excessive tearing after the surgery, five eyes (25%) improved and 12 eyes (60%) remained symptom-free (Table 1). Although, intraoperative MMC application seemed to improve the subjective symptoms reported by patients, the satisfaction rates did not differ significantly between the two groups (P = 0.087, Fisher’s exact χ 2 test).
All patients except one showed patency of the lacrimal drainage system in the MMC group. In the control group, three eyes revealed non-patency of the drainage system. The success rate in the MMC group was 95% (19/20), and that in the control group was 85% (17/20) (Table 2). Although, the success rate in the MMC group was higher than that of the control group, there was no statistically significant difference between the success rates of MMC and control DCR surgery groups (P = 0.605, Fisher’s exact χ 2 test).
The power calculation of the study was found to be 0.45 for the satisfaction rates and was 0.08 for success rates, both of which were underpowered.
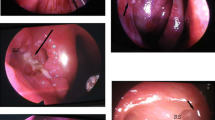
All four failed eyes (one in the MMC group and three in the control group) underwent a revision endoscopic lacrimal surgery secondary to failed primary EXT-DCR. Excessive granulation tissue formation or fibrous tissue growth at the osteotomy site was noted during the endoscopic surgery in all patients.
No complications such as nasal bleeding, mucosal necrosis or infection were noted in any patients during the one-year follow up. No nasal or gastrointestinal irritation had been observed during intraoperative MMC application.
Discussion
There are limited studies concerning the adjunctive use of MMC as a new treatment modality in EXT-DCR surgery to evaluate the long-term success, patient satisfaction and rate of complications. Liao et al. [12] evaluated the long-term results of intraoperative MMC application in EXT-DCR surgery compared with the results of the conventional procedure in a prospective randomized controlled study for a total of 88 primary acquired nasolacrimal duct obstructions. Among the 44 eyes in the MMC group, 95.5% of patients remained totally symptom-free after 10 months of follow up, while in the conventional group 70.5% of patients were reported to be symptom-free and 18% of patients to have an improvement in their symptoms. The non-patency rate in the MMC group was 4.5% compared with 11.4% in the conventional group. They concluded that intraoperative MMC application could improve the satisfaction rate and the success rate of EXT-DCR surgery.
Kao et al. [13] observed the effect of intraoperative MMC on the size of the osteotomy site after EXT-DCR. They showed that the mean actual osteotomy size in MMC group (27.10 ± 5.78 mm2) at the end of the sixth postoperative month was statistically significantly larger than that of the control group (10.63 ± 3.37 mm2). They stated that intraoperative MMC is effective in maintaining a larger osteotomy size. Yeatts and Neves [14] recommended that the adjunctive use of MMC might increase the success rate of repeat DCR.
In this study, patients were assigned randomly to each group, with age between the two groups not being a significant factor. Eighteen eyes in the MMC group remained free from epiphora and one eye improved after one-year follow up. Only one out of 20 eyes failed to respond to EXT-DCR. While in the control group three out of 20 eyes had excessive tearing after the surgery, five eyes improved and 12 eyes remained symptom-free. All patients except one showed patency of the lacrimal drainage system in the MMC group. In the control group three eyes revealed non-patency of the drainage system, and an obstruction over the osteotomy site. The success rate in the MMC group was 95% (19/20), and that in the control DCR group was 85% (17/20). According to the results of this study, the satisfaction and success rates of the MMC group were higher than those of the control group, however the differences were not statistically significant.
You and Fang [15] assessed the efficacy of different dosages of intraoperative MMC in EXT-DCR in 50 eyes. They used 0.2 mg/ml MMC for 5 min in one group and 0.5 mg/ml MMC for 5 min in another group and compared the efficacy with the control group. The patency rate and osteotomy size differences between the patients treated with MMC and the control group was statistically significant, whereas there was no significant difference between the two MMC groups. It has also been shown that 0.5 mg/ml of MMC for 2.5 min favorably affected wound healing in the osteotomy site [16]. However, an MMC exposure time of 30 min with lower concentrations of the drug (0.2 mg/ml) was arbitrarily chosen in our study as an interval to maximally inhibit fibrosis. Moreover, it took about 1 min to perform MMC-soaked cottonoids during the surgery. We removed the MMC-soaked cottonoid after an MMC exposure time of 30 min outside the operating room. Thus, MMC soaking during EXT-DCR did not increase the operating time.
A standard surgical technique of EXT-DCR was used in all patients except for nasolacrimal tube intubation, which could be considered a limitation of this study. Silicone tubes are advised for use in EXT-DCR to ensure patency of the canalicular system, especially in the early postoperative period [1]. We advocate EXT-DCR with silicone tube intubation for congenital, post-traumatic and revision patients. The success rates of 85–95% for EXT-DCR surgery for both control and MMC groups reported in this study are comparable with those achieved with nasolacrimal intubation.
Many complications such as corneal ulcus, corneal perforations, scleral calcification, secondary cataract, endophthalmitis, hypotony and maculopathy have been reported in both pterygium and glaucoma filtration surgeries [17, 18]. No severe complications such as abnormal nasal bleeding, mucosal necrosis or severe infections were reported during MMC soaking in EXT-DCR surgery in this study, consistent with those other studies.
In conclusion, in the present study the satisfaction and success rates of the EXT-DCR with MMC application were found to be higher than those of standard EXT-DCR, however the differences did not reach statistical significance. No deleterious effect was noted with MMC treatment. Although the sample size and power of the study were too small to make definite statements, intraoperative MMC application seems to be a safe adjuvant that could help to increase the success rate of EXT-DCR surgery in primary acquired nasolacrimal duct obstruction. Application of a wound-healing inhibitor is a new treatment modality in EXT-DCR surgery and more studies with larger series must be done on this topic before one can make further conclusions. A rationale for the duration and method of MMC application should also be determined.
References
Tarbet KJ, Custer PL (1995) External dacryocystorhinostomy: surgical success, patient satisfaction and economic cost. Ophthalmology 102:1065–1070
Zolli CL, Shannonn GM (1982) Dacryocystorhinostomy: a review of 119 cases. Ophthalmic Surg 13:905–910
Burns JA, Cahill KV (1985) Modified Kinosian dacryocystorhinostomy: a review of 122 cases. Ophthalmic Surg 16:710–716
Walland MJ, Rose GE (1994) Factors affecting the success rate of open lacrimal surgery. Br J Ophthalmol 78:888–891
McLachlan DL, Shannonn GM, Flanagan JC (1980) Results of dacryocystorhinostomy: analysis of the reoperations. Ophthalmic Surg 11:427–430
Allen K, Berlin AJ (1989) Dacryocystorhinostomy failure: association with nasolacrimal silicone intubation. Ophthalmic Surg 20:115–119
Bergstrom TJ, Wilkinson WS, Skuta GL, Watnick RL, Elner VM (1991) The effects of subconjunctival mitomycin C on glaucoma filtration surgery in rabbits. Arch Ophthalmol 109:1725–1730
Singh G, Wilson MR, Foster CS (1988) Mitomycin eye drops as treatment for pterygium. Ophthalmology 95:813–821
Megevand GS, Salmon JF, Scholtz RP, Murray AD (1995) The effect of reducing the exposure time of mitomycin C in glaucoma filtering surgery. Ophthalmology 102:84–90
Hu D, Sires BS, Tong DC, Royack GA, Oda D (2000) Effect of brief exposure to mitomycin C on cultured human nasal mucosa fibroblasts. Ophthal Plast Reconstr Surg 16:119–125
Yalaz M, Firinciogullari E, Zeren H (1999) Use of mitomycin C and 5-fluorouracil in external dacryocystorhinostomy. Orbit 18:239–245
Liao SL, Kao SCS, Tseng JHS, Chen MS, Hou PK (2000) Results of intraoperative mitomycin C application in dacryocystorhinostomy. Br J Ophthalmol 84:903–906
Kao SCS, Liao CL, Tseng JHS, Chen MS, Hou PK (1997) Dacryocystorhinostomy with intraoperative mitomycin C. Ophthalmology 104:86–91
Yeatts RP, Neves RB (1999) Use of mitomycin C in repeat dacryocystorhinostomy. Ophthal Plast Reconstr Surg 15:19–22
You YA, Fang CT (2001) Intraoperative mitomycin C in dacryocystorhinostomy. Ophthal Plast Reconstr Surg 17:115–119
Ugurbas SH, Zilelioglu G, Sargon MF, Anadolu Y, Akiner M, Aktürk T (1997) Histopathologic effects of mitomycin C on endoscopic transnasal dacryocystorhinostomy. Ophthalmic Surg Lasers 28:300–304
Dunn JP, Seamone CD, Ostler BH, Nickel BL, Beallo A (1991) Development of scleral ulceration and calcification after pterygium excision and mitomycin therapy. Am J Ophthalmol 112:343–345
Zacharria PT, Depperrman SR, Schuman JS (1993) Ocular hypotony after trabeculectomy with mitomycin C. Am J Ophthalmol 116:314–336
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yildirim, C., Yaylali, V., Esme, A. et al. Long-term results of adjunctive use of mitomycin C in external dacryocystorhinostomy. Int Ophthalmol 27, 31–35 (2007). https://doi.org/10.1007/s10792-007-9057-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-007-9057-6