Abstract
The classic NLRP3 inflammasome and NF-κB molecular pathways are activated in many inflammatory-related diseases, such as pleurisy. Because oridonin (Ori) has been indicated as a covalent NLRP3 inhibitor with strong anti-inflammasome activity, we herein aimed to assess the effects of Ori in a mouse model of carrageenan (CAR)-induced pleurisy. The results showed that CAR caused hemorrhaging and exudation of lung tissues and the release of inflammatory factors (TNF-α, IL-6 and IL-1β), effects that were significantly reduced by treatment with Ori. In addition, increased neutrophil infiltration, protein concentrations and volumes were found in the exudates of the CAR group, and these phenomena were suppressed by Ori treatment. Regarding cellular pathways, Ori could alleviate the CAR-activated NF-κB and TXNIP/NLRP3 pathways. Additionally, oxidative stress was shown to be involved in the pathogenesis of pleurisy, but possible mechanisms remain to be explored. Herein, Ori reversed the CAR-induced depletion of GSH and SOD and the CAR-induced increases in ROS, MPO and MDA levels. Furthermore, Ori inhibited NOX-4 levels, initiated the dissociation of KEAP-1 from Nrf2, activated the downstream genes HO-1 and exerted antioxidative effects on CAR-induced pleurisy. In conclusion, Ori conferred protection against CAR-induced pleurisy via Nrf2-dependent antioxidative and NLRP3-dependent anti-inflammatory properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many pathogenic factors, usually viruses and bacteria, stimulate the pleura and cause pleurisy. In pleurisy, neutrophils and exudate accumulate and exacerbate local inflammation, ultimately leading to chest pain and dyspnea (Light 2003). Carrageenan (CAR)-induced pleurisy is a classic animal model of acute inflammation that is used to assess the effects of inflammatory mediators and agents (Ekuadzi et al. 2018). Administration of CAR into the chest can cause polymorphonuclear leukocyte (PMN) accumulation and advance the progression of local inflammation and lung injury (Fusco et al. 2017). The production of inflammatory cytokines, chemokines, and reactive oxygen species (ROS) enhances the inflammatory response. In the occurrence and development of pleurisy, many inflammatory pathways are involved (Ward 2010). The NOD-like receptor NLRP3 inflammasome and its upstream signaling receptor NF-κB are the most important components that enhance the production of the abovementioned inflammatory mediators (Fusco et al. 2017). NF-κB is a heterodimer consisting of P50 and P65 and is normally retained in the cytoplasm. Once stimuli induce the phosphorylation of its inhibitor IκB, NF-κB is activated and translocates to the nucleus to initiate the downstream effectors (Pereira Dos Santos Nascimento et al. 2016; Bayir et al. 2019). Increasing evidence shows that thioredoxin-interacting protein (TXNIP) detaches from thioredoxin (TRX) and binds to NLRP3 in response to ROS (Ye et al. 2017). The NLRP3 inflammasome is an assembled molecular complex that includes NLRP3, the adaptor ASC and the effector pro-caspase-1. Upon activation, pro-caspase-1 converts IL-18 and IL-1β into their active forms to induce inflammation (Hou et al. 2018).
In addition, oxidative stress is also an important component of pleurisy induced by CAR (Yang et al. 2018; Nardi et al. 2007). Once inflammation is established, excessive production of ROS will lead to an imbalance between pro-oxidants and antioxidants, which eventually leads to oxidative stress (Islam 2017). When the levels of glutathione (GSH) and superoxide dismutase (SOD), critical free-radical scavengers in the body, are insufficient to resist the accumulation of pro-oxidants, the products of lipid peroxidation [malondialdehyde (MDA) and myeloperpxidase (MPO)] are increased, thus exacerbating cellular injury (Lv et al. 2017). Among the related molecular pathways, nuclear factor (erythroid-derived 2)-like 2 (Nrf2) plays a vital role (Hybertson et al. 2011). As a transcriptional factor, Nrf2 in its inactive form combines with KEAP-1 in the cytoplasm. Upon activation, Nrf2 regulates the expression of downstream antioxidative enzymes, such as GSH and heme oxygenase-1 (HO-1) (Zhu et al. 2017). Furthermore, the NADPH oxidase system is widely considered important in the production of ROS and induces the activation of Nrf2 (Wu et al. 2017). Many studies have verified that Nrf2 activators exert therapeutic effects on many inflammatory and oxidative-related diseases, such as pleurisy (Hybertson et al. 2011; Yang et al. 2018).
Oridonin (Ori), an active diterpenoid compound isolated from the plant Rabdosia Rrubescens, possesses antioxidative, anti-inflammatory and antitumor properties. On one hand, Ori induces the nuclear transcription of Nrf2 and acts as an antioxidative molecule (Lu et al. 2018). On the other hand, Ori forms a covalent bond with the cysteine 279 of NLRP3 to block the interaction between NLRP3 and NEK7, thereby inhibiting NLRP3 inflammasome assembly and activation (He et al. 2018). However, the effects of Ori on CAR-induced pleurisy have not been studied. Therefore, the aim of our study was to investigate whether Ori can inhibit the pleurisy and the related molecular pathways.
Methods and materials
Reagents and antibodies
Ori (purity > 98% tested by HPLC) was obtained from Chengdu Pufei De Biotechnology Company. CAR and Giemsa stain were purchased from Sigma Aldrich. Mouse TNF-α, IL-6 and IL-1β enzyme-linked immunosorbent assay (ELISA) kits were obtained from Biolegend. MPO, MDA, GSH, and SOD determination kits were provided by Nanjing Jiancheng Bioengineering Institute. The ROS assay kit was obtained from Beyotime Biotechnology and the BCA detection kit was provided by Thermo. Primary antibodies against NOX-4, KEAP-1, Nrf2, HO-1, NLRP3, CASPASE-1, IL-1β, ASC, TRX-1, TXNIP, p-p65, p-IκB, IκB and β-actin were purchased from Cell Signaling or Abcam. The horseradish peroxidase-conjugated anti-rabbit and anti-mouse IgG were obtained from Proteintech.
Animal
BALB/c female mice (18–20 g) were obtained from the Liaoning Changsheng Technology Institute (Certificate SCXK2015-0001) and housed at a temperature of 23 ± 1 °C with a light–dark cycle and access to a standard diet and water. This study was approved by the Animal Ethical Committee of First Hospital of Jilin University in 2016 (Protocol no.071).
CAR-induced pleurisy
The mice were randomly divided into six groups: the control, CAR (2%), Ori (20 mg/kg), CAR + Ori (5 mg/kg), CAR + Ori (10 mg/kg) and CAR + Ori (20 mg/kg) groups. Ori (5, 10 and 20 mg/kg) was intraperitoneally injected and 1 h later, CAR (2%) or saline was injected into the right pleural cavity. After 4 h, the mice were euthanized with diethyl ether, and the pleural exudate was collected for measurement of the total volume, protein concentration, the number of neutrophils and ROS levels (Pereira Dos Santos Nascimento et al. 2016; Fusco et al. 2017). The left lung tissues were obtained for formalin fixation and hematoxylin and eosin (HE) staining. The right lung tissues were extracted for the detection of MPO, MDA, GSH, SOD and the related protein expression levels.
Histological examination
The left lung tissues were fixed in formaldehyde solution for 1 week at room temperature and embedded in paraffin blocks. Sections were cut into 5 μm and stained with HE. Then, the lung injury was scored based on leukocyte infiltration, hemorrhage, edema and alveolar wall thickness. A score scaled from 0 to 5 represented the severity: 0 for no damage, 1 for mild damage, 2–3 for moderate damage, 4 for severe damage, and 5 for very severe damage.
Giemsa staining
The pleural exudate was collected and centrifuged at 6000 rpm for 10 min at 4 °C. The supernatant was stored at − 80 °C for later measurement of cytokine levels. The cells were lysed and centrifuged onto glass slides by a cytospin, fixed into methyl alcohol for 1 min, and incubated with Giemsa A and B for 5 min. The neutrophils and macrophages were distinguishable.
Enzyme-linked immunosorbent assay
The corresponding primary antibodies were coated into Maxisorp overnight and blotted with a diluted sample for 1 h. The supernatant of the pleural exudate was added into every well for 2 h, and then the secondary antibodies and horseradish peroxidase were added to the cell plates. Finally, every well was incubated with TMB substrate for 15 min, and the stop solution was fully mixed into every well. The absorbance was read at 450 nm with a microplate reader.
Measurement of ROS generation
Plural effusion was collected and lysed with lysis buffer. Cells were transferred into tubes, washed with 100 μl of PBS three times and stained with 2,7-dichlorodihydrofluorescein diacetate (DCF/DA) for 30 min. Then, 300 μl of PBS was added to every tube and FACS analysis was performed. In addition, 96-well plates were incubated with 100 μl of cell suspension and stained for 30 min. A fluorescence microscopy was used to detect the intensity of every well and the intensity data were analyzed by ImageJ.
MPO, MDA, GSH and SOD levels
The right lung tissues were collected and ground until homogenized in saline. The four oxidative stress markers were examined using their respective detection kits.
Western blotting analysis
Lung tissues were lysed in RIPA buffer with protease inhibitor for 30 min and centrifuged at 12,000 rpm for 10 min at 4 °C. The supernatants were extracted to measure the protein concentrations. Proteins were analyzed by 10–12.5% SDS-PAGE and transferred to a polyvinylidene difluoride membrane. Then, the membranes were incubated with primary antibodies overnight, incubated with the secondary antibody for 1 h, visualized by enhanced chemiluminescence (ECL) and analyzed by ImageJ software.
Statistical analysis
All values are expressed as mean ± standard deviation (S.D.). These data were analyzed by one-way ANOVA or Student’s t test. P < 0.05 or P < 0.01 was considered statistically significant.
Results
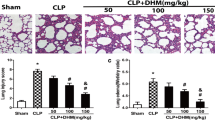
Ori reduced lung injury scores
Compared with the control group, the CAR group showed significant inflammatory granulocyte infiltration, edema, disseminated thickening of alveolar septa and focal hemorrhaging of lung tissues. According to the assessment of lung injury, Ori treatment (5, 10 and 20 mg/kg) contributed to lower lung injury scores compared to those in the CAR group; scores in the 20 mg/kg Ori treatment group were reduced by 50% compared to those in the CAR group.
Ori reduced the release of cytokines
Then, we collected the pleural effusion and examined cytokine levels by ELISA. The results showed that Ori (10 and 20 mg/kg) inhibited the release of inflammatory cytokines (TNF-α, IL-6 and IL-1β). Among all the conditions analyzed, 20 mg/kg Ori showed the best therapeutic effects (Figs. 1, 2).
Ori reduced lung injury scores. a, b After euthanasia, the left lung tissues were collected and examined by HE staining. According to the degree of lung injury, the lung injury score was determined on a five-point scale in the following groups: a control b CAR (2%) c Ori (20 mg/kg) d CAR + Ori (5 mg/kg) e CAR + Ori (10 mg/kg), and f CAR + Ori (20 mg/kg). The error bars represent the standard error from five replicates. **P < 0.01 relative to the control group. #P < 0.05 and ##P < 0.01 relative to the CAR alone group
Ori reduced the release of cytokines. a–c The thorax was washed with PBS and collected for the subsequent experiments. According to the ELISA instructions, the levels of inflammatory cytokines (TNF-α, IL-6 and IL-1β) in the pleural exudate were detected. The error bars represent the standard error from five replicates. **P < 0.01 relative to the control group. #P < 0.05 and ##P < 0.01 relative to CAR alone
Ori decreased the levels of oxidative stress markers
Oxidative stress markers were used to assess the antioxidative effects of Ori on CAR-induced pleurisy. GSH and SOD are free radical scavengers in the human body. As shown in Fig. 3, the levels of these two markers were higher in the Ori group (10 and 20 mg/kg) than in the CAR group. As the degree of lipid peroxidation increased, ROS, MPO and MDA were overexpressed. Consistently, CAR induced the accumulation of ROS and high MPO and MDA expression levels, which were reversed by the injection of Ori (10 and 20 mg/kg). Fundamentally, the largest dose of Ori (20 mg/kg) relieved the CAR-induced oxidative stress imbalance.
Ori decreased the levels of oxidative stress markers. a–c Pleural effusion was collected and centrifuged at 6000 rpm for 5 min. Cell pellets were lysed with lysis buffer and stained with DCF/DA. Then, samples were assessed by FACS and fluorescence microscopy. The intensity of fluorescence was analyzed by ImageJ. Scale bars: 50 μM. a Control b CAR (2%) c Ori (20 mg/kg) d CAR + Ori (5 mg/kg) e CAR + Ori (10 mg/kg) f CAR + Ori (20 mg/kg). d–g The MPO activity, MDA formation, GSH content, and SOD content in lung tissues were examined according to the instructions. The error bars represent the standard error from five replicates. **P < 0.01 compared to the control group. #P < 0.05 and ##P < 0.01 compared to the CAR group
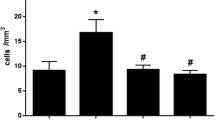
Ori reduced neutrophil infiltration, the exudate volume and the exudate protein concentration
When inflammation occurs, neutrophils continue to exude and activate in the affected area. Therefore, inhibition of leukocyte chemotaxis may be a new way to treat pleurisy. According to Giemsa staining, Ori (10 and 20 mg/kg) alleviated the CAR-induced infiltration of neutrophils. Additionally, we examined the volume and protein concentration of the exudate; the results were consistent with the above findings, as the expression levels in the 20 mg/kg Ori treatment group were reduced by 50% compared to those in the CAR group, and 20 mg/kg Ori showed obvious therapeutic effects.
Ori inhibited the CAR-activated NF-κB pathway
According to the above results, 20 mg/kg Ori significantly suppressed the inflammatory response induced by CAR. Therefore, we used 20 mg/kg Ori to assess the related pathways. In inflammatory signaling pathways, NF-κB plays a vital role in regulating downstream inflammatory cytokines and mediators. Therefore, we detected the activation of the NF-κB pathway by Western blot analysis, revealing that Ori inhibited the phosphorylation of NF-κB and IκB, which may be involved in the altered levels of cytokines and neutrophils.
Ori inhibited the CAR-activated TXNIP/NLRP3 pathways
To investigate the effects of Ori on inflammasome activation, we analyzed NLRP3, ASC, CASPASE-1 and IL-1β expression. In our study, mice in the Ori treatment group exhibited decreased levels compared with those in CAR-treated mice. TXNIP acts as an upstream signal of NLRP3 and participates in the progression of inflammatory-related diseases. Consistently, CAR activated TXNIP and inhibited TRX-1 expression levels, and Ori showed a significant protective role in CAR-induced pleurisy.
Ori activated the KEAP-1/Nrf2 signaling pathway
Oxidative stress occurs during the process of inflammation, and we next assessed the possible mechanisms underlying this phenomenon in an animal model. We mainly focused on the Nrf2 pathway. Ori induced the activation of Nrf2 and HO-1 to exert antioxidative effects. Examination of upstream regulators showed that the expression levels of KEAP-1 and NOX-4 were decreased after Ori treatment.
Discussion
Pleurisy can be caused by infection and infectious pathogens, mainly bacteria and viruses. In the acute phase of pleurisy, vascular permeability is increased and neutrophils infiltrate the inflamed tissues. Furthermore, exudates migrate from injured tissues to the pleural cavity, leading to pleural effusion. The primary clinical symptoms of pleurisy are chest distress, chest pain and dyspnea. Extraction of exudates and the use of antibiotics are common treatments in the clinic (Kass et al. 2007).
CAR-induced pleurisy is a representative model and is widely used to investigate the related mechanisms and effects of inflammatory mediators and agents (Ekuadzi et al. 2018; Fusco et al. 2017). The injection of CAR induces the infiltration of neutrophils and the overproduction of ROS, such as hydrogen peroxide, superoxide, and hydroxyl radicals (Salvemini et al. 1996). Thus, oxidative stress and inflammation jointly participate in the pathological progression of pleurisy. In a phenotypic analysis, our results demonstrated that Ori group (5, 10 and 20 mg/kg) alleviated CAR-induced leukocyte infiltration, hemorrhaging and edema. Assessment of lung injuries and statistical analyses demonstrated that the high dose of Ori showed the best therapeutic effects among all the doses analyzed (Fig. 1). Additionally, CAR induced the release of inflammatory cytokines (TNF-α, IL-6 and IL-1β) (Fig. 2) and increased the protein concentration of exudate (Fig. 4), conditions that were reversed by treatment with Ori (10 ang 20 mg/kg). Furthermore, oxidative stress markers were examined to assess the antioxidative effects of Ori and as expected, Ori injection was associated with decreased levels of MDA and MPO and increased levels of GSH and SOD compared to those in the CAR group. In addition, pleural effusion cells were stained with DCF/DA and assessed by FACS and fluorescence microscopy, revealing that Ori group (10 ang 20 mg/kg) significantly inhibited CAR-induced ROS generation (Fig. 3).
Ori reduced neutrophil infiltration, the exudate volume and the exudate protein concentration. a, d After the lysis of pleural cells, part of the cells was stained with Giemsa and used to highlight different inflammatory cells (red arrows: neutrophils; black arrows: macrophages). a Control b CAR (2%) c Ori (20 mg/kg) d CAR + Ori (5 mg/kg) e CAR + Ori (10 mg/kg) f CAR + Ori (20 mg/kg). b, c The exudate volume was detected, and the protein concentration was measured using a BCA kit. The values are expressed as mean ± SD. n = 5. **P < 0.01 versus the control group. #P < 0.05 and ##P < 0.01 versus the CAR group
Based on the above findings and previous studies on the molecular pathway mechanisms, we mainly focused on KEAP-1/Nrf2, NF-κB and TXNIP/NLRP3 (Fusco et al. 2017; Pereira Dos Santos Nascimento et al. 2016; Yang et al. 2018). Nrf2 is a critical factor that regulates oxidative stress and inflammation. It has been proven that Nrf2 can be activated to promote the expression of downstream genes (HO-1 and GSH) and thus exert antioxidative activity. Many reports have shown that agents such as Nrf2 activators confer protection against inflammatory-related diseases (Yang and Liu 2018; Hu et al. 2018). For example, Pterostilbene could inhibit inflammation and ROS production by activating the Nrf2 pathway (Xue et al. 2017) (Figs. 5, 6). Allicin was also proven to decrease lipopolysaccharide-induced inflammation through Nrf2 (Zhang et al. 2017). In our study, Ori could activate Nrf2 and a downstream gene (HO-1) (Fig. 7). Therefore, we wanted to identify the upstream regulatory factors of Nrf2 to further elucidate the pharmacological effects of Ori. On one hand, Nrf2 combines with KEAP-1 and remains in an inactive form in the cytoplasm. When stimulated, Nrf2 separates from KEAP-1 and translocates into the nucleus (Taguchi and Yamamoto. 2017). The KEAP-1/Nrf2 pathways participate in many disease processes, such as inflammation, and in cancer and neurodegenerative diseases (Deshmukh et al. 2017; Lu et al. 2016). On the other hand, the AMPK and MAPK pathways are regulators of Nrf2 and have strong antioxidative effects (Jeong et al. 2016). A dual AMPK/Nrf2 activator was shown to reduce brain inflammation after stroke (Wang et al. 2018). Additionally, Fluoxetine protected against methamphetamine-induced lung inflammation through the MAPK/Nrf2 pathways (Wang et al. 2017). In our research, CAR activated KEAP-1 and the Ori treatment group showed decreased levels of KEAP-1 (Fig. 7). Furthermore, an increasing number of studies have shown that the NADPH oxidase system participates in the production of ROS and the activation of Nrf2. The system consists of many isozymes, such as NOX1-NOX5, DUOX1 and DUOX2, and their expression levels vary by tissue (Tada and Suzuki. 2016). It has been demonstrated that NOX-4 is overexpressed in pulmonary diseases (Kovac et al. 2015); in our study, CAR activated NOX-4, and the Ori group showed decreased levels of NOX-4 (Fig. 7). Therefore, combined with the protective effects on the oxidative indexes (ROS, GSH, SOD, MDA and MPO), these results suggest that Ori exerts its obvious antioxidative effects through the KEAP-1/Nrf2 pathways.
Ori inhibited the CAR-activated NF-κB pathway. a, b The lung tissues were collected 4 h after CAR injection and the total protein was extracted. The protein expression levels of p-p65, p-IκB and IκB were measured by Western blot and β-actin was used as an internal control. The error bars represent the standard error. **P < 0.01 relative to the control group. #P < 0.05 and ##P < 0.01 relative to the CAR alone group
Ori inhibited the CAR-activated TXNIP/NLRP3 pathways. a–c Western blot analyses of NLRP3, CASPASE-1, IL-1β, ASC, TRX-1 and TXNIP in lung tissues are shown; β-actin was used as an internal control. *P < 0.05 and **P < 0.01 relative to the control group. #P < 0.05 and ##P < 0.01 relative to the CAR or Ori alone group
Moreover, the NF-κB and TXNIP/NLRP3 canonical pathways are often involved. TXNIP, stimulated by ROS, dissociates from thioredoxin (TRX) and then activates NLRP3 to promote assembly (Cao et al. 2017). NLRP3 is an intracellular signalling molecule that binds to ASC upon activation. Then ASC interacts with caspase-1 to create a complex referred to as the inflammasome, which leads to the activation of caspase-1 and IL-1β. The NLRP3 inflammasome has been shown to be activated in many inflammatory-related diseases, such as type 2 diabetes, Alzheimer’s disease, lung injury and pleurisy (Gaidt and Hornung 2018). BAY 11–7082 and A438079 acted as pharmacological inhibitors to alleviate neuroinflammation (Jiang et al. 2017). Another small-molecule inhibitor, MCC950, has been used to treat NLRP3-associated autoinflammatory and autoimmune diseases (Coll et al. 2015). In addition, it has been demonstrated that a covalent bond between Ori and the cysteine 279 of NLRP3 blocks the interaction between NLRP3 and NEK7, thereby inhibiting NLRP3 inflammasome assembly and activation (He et al. 2018). As our results showed, Ori treatment alleviated CAR-induced TXNIP/NLRP3 and IL-1β activation (Fig. 6). In addition, NF-κB acts as an upstream regulator of NLRP3 and plays significant roles in the abovementioned diseases (Mangali et al. 2019). Under normal conditions, NF-κB is sequestered in the cytoplasm by its inhibitor IκB. Under stress, NF-κB translocates to the nucleus and regulates the release of inflammatory cytokines and downstream effectors (Nennig and Schank 2017). The natural product Crocin has been shown to attenuate LPS-induced anxiety and depressive-like behaviors by suppressing the NF-κB and NLRP3 pathways (Zhang et al. 2018). Our result showed that CAR induced the phosphorylation of NF-κB and IκB, the levels of which were decreased in the Ori group (Fig. 5). Additionally, the number of neutrophils and the concentrations of inflammatory cytokines (TNF-α, IL-6 and IL-1β) and pleural effusion proteins were reversed by treatment with Ori (Figs. 2, 4).
Taken together, our data demonstrated that Ori could activate the Nrf2 pathway and alleviate the CAR-induced NF-κB and NLRP3 pathways and the release of inflammatory factors, which highlights the role of Ori in inflammatory-related diseases.
Conclusions
This study highlighted potential pathways involved in the antioxidative and anti-inflammatory effects of Ori. The protective effect of Ori on oxidative stress was demonstrated by changes in the levels of the oxidative stress markers ROS, MDA, MPO, SOD and GSH and the proteins NOX-4, KEAP-1, Nrf2 and HO-1. In contrast, the levels of cytokines TNF-α, IL-6 and IL-1β and proteins NF-κB and TXNIP/NLRP3 were associated with the anti-inflammatory activity of Ori. Thus, Ori could be a candidate drug for the treatment of pleurisy.
References
Bayir Y, Un H, Cadirci E, Akpinar E, Diyarbakir B, Calik I, Halici Z (2019) Effects of Aliskiren, an RAAS inhibitor, on a carrageenan-induced pleurisy model of rats. An Acad Bras Cienc 91(1):e20180106
Cao Z, Fang Y, Lu Y, Tan D, Du C, Li Y, Ma Q, Yu J, Chen M, Zhou C, Pei L, Zhang L, Ran H, He M, Yu Z, Zhou Z (2017) Melatonin alleviates cadmium-induced liver injury by inhibiting the TXNIP-NLRP3 inflammasome. J Pineal Res 62(3):e12389
Coll RC, Robertson AA, Chae JJ, Higgins SC, Munoz-Planillo R, Inserra MC, Vetter I, Dungan LS, Monks BG, Stutz A, Croker DE, Butler MS, Haneklaus M, Sutton CE, Nunez G, Latz E, Kastner DL, Mills KH, Masters SL, Schroder K, Cooper MA, O'Neill LA (2015) A small-molecule inhibitor of the NLRP3 inflammasome for the treatment of inflammatory diseases. Nat Med 21(3):248–255
Deshmukh P, Unni S, Krishnappa G, Padmanabhan B (2017) The Keap1-Nrf2 pathway: promising therapeutic target to counteract ROS-mediated damage in cancers and neurodegenerative diseases. Biophys Rev 9(1):41–56
Ekuadzi E, Biney RP, Benneh CK, Osei Amankwaa B, Jato J (2018) Antiinflammatory properties of betulinic acid and xylopic acid in the carrageenan-induced pleurisy model of lung inflammation in mice. Phytother Res 32(3):480–487
Fusco R, Gugliandolo E, Biundo F, Campolo M, Di Paola R, Cuzzocrea S (2017) Inhibition of inflammasome activation improves lung acute injury induced by carrageenan in a mouse model of pleurisy. FASEB J 31(8):3497–3511
Gaidt MM, Hornung V (2018) The NLRP3 Inflammasome Renders Cell Death Pro-inflammatory. J Mol Biol 430(2):133–141
He H, Jiang H, Chen Y, Ye J, Wang A, Wang C, Liu Q, Liang G, Deng X, Jiang W, Zhou R (2018) Oridonin is a covalent NLRP3 inhibitor with strong anti-inflammasome activity. Nat Commun 9(1):2550
Hou Y, Wang Y, He Q, Li L, Xie H, Zhao Y, Zhao J (2018) Nrf2 inhibits NLRP3 inflammasome activation through regulating Trx1/TXNIP complex in cerebral ischemia reperfusion injury. Behav Brain Res 336:32–39
Hu Q, Zhang T, Yi L, Zhou X, Mi M (2018) Dihydromyricetin inhibits NLRP3 inflammasome-dependent pyroptosis by activating the Nrf2 signaling pathway in vascular endothelial cells. BioFactors 44(2):123–136
Hybertson BM, Gao B, Bose SK, McCord JM (2011) Oxidative stress in health and disease: the therapeutic potential of Nrf2 activation. Mol Aspects Med 32(4–6):234–246
Islam MT (2017) Oxidative stress and mitochondrial dysfunction-linked neurodegenerative disorders. Neurol Res 39(1):73–82
Jeong YH, Park JS, Kim DH, Kim HS (2016) Lonchocarpine increases Nrf2/ARE-mediated antioxidant enzyme expression by modulating AMPK and MAPK signaling in brain astrocytes. Biomol Ther (Seoul) 24(6):581–588
Jiang W, Li M, He F, Zhou S, Zhu L (2017) Targeting the NLRP3 inflammasome to attenuate spinal cord injury in mice. J Neuroinflammation 14(1):207
Kass SM, Williams PM, Reamy BV (2007) Pleurisy. Am Fam Physician 75(9):1357–1364
Kovac S, Angelova PR, Holmstrom KM, Zhang Y, Dinkova-Kostova AT, Abramov AY (2015) Nrf2 regulates ROS production by mitochondria and NADPH oxidase. Biochim Biophys Acta 1850(4):794–801
Light RW (2003) Pleural diseases. Curr Opin Pulm Med 9(4):251–253
Lu MC, Ji JA, Jiang ZY, You QD (2016) The Keap1-Nrf2-ARE Pathway As a Potential Preventive and Therapeutic Target: An Update. Med Res Rev 36(5):924–963
Lu Y, Sun Y, Zhu J, Yu L, Jiang X, Zhang J, Dong X, Ma B, Zhang Q (2018) Oridonin exerts anticancer effect on osteosarcoma by activating PPAR-gamma and inhibiting Nrf2 pathway. Cell Death Dis 9(1):15
Lv H, Liu Q, Wen Z, Feng H, Deng X, Ci X (2017) Xanthohumol ameliorates lipopolysaccharide (LPS)-induced acute lung injury via induction of AMPK/GSK3beta-Nrf2 signal axis. Redox Biol 12:311–324
Mangali S, Bhat A, Udumula MP, Dhar I, Sriram D, Dhar A (2019) Inhibition of protein kinase R protects against palmitic acid-induced inflammation, oxidative stress, and apoptosis through the JNK/NF-kB/NLRP3 pathway in cultured H9C2 cardiomyocytes. J Cell Biochem 120(3):3651–3663
Nardi GM, Siqueira Junior JM, Delle Monache F, Pizzolatti MG, Ckless K, Ribeiro-do-Valle RM (2007) Antioxidant and anti-inflammatory effects of products from Croton celtidifolius Bailon on carrageenan-induced pleurisy in rats. Phytomedicine 14(2–3):115–122
Nennig SE, Schank JR (2017) The Role of NFkB in drug addiction: beyond inflammation. Alcohol Alcohol 52(2):172–179
Pereira Dos Santos Nascimento MV, Arruda-Silva F, Gobbo Luz AB, Baratto B, Venzke D, Mendes BG, Frode TS, Geraldo Pizzolatti M, Dalmarco EM (2016) Inhibition of the NF-kappaB and p38 MAPK pathways by scopoletin reduce the inflammation caused by carrageenan in the mouse model of pleurisy. Immunopharmacol Immunotoxicol 38(5):344–352
Salvemini D, Wang ZQ, Bourdon DM, Stern MK, Currie MG, Manning PT (1996) Evidence of peroxynitrite involvement in the carrageenan-induced rat paw edema. Eur J Pharmacol 303(3):217–220
Tada Y, Suzuki J (2016) Oxidative stress and myocarditis. Curr Pharm Des 22(4):450–471
Taguchi K, Yamamoto M (2017) The KEAP1-NRF2 system in cancer. Front Oncol 7:85
Wang Y, Gu YH, Liu M, Bai Y, Wang HL (2017) Fluoxetine protects against methamphetamineinduced lung inflammation by suppressing oxidative stress through the SERT/p38 MAPK/Nrf2 pathway in rats. Mol Med Rep 15(2):673–680
Wang Y, Huang Y, Xu Y, Ruan W, Wang H, Zhang Y, Saavedra JM, Zhang L, Huang Z, Pang T (2018) A Dual AMPK/Nrf2 activator reduces brain inflammation after stroke by enhancing microglia M2 polarization. Antioxid Redox Signal 28(2):141–163
Ward PA (2010) Oxidative stress: acute and progressive lung injury. Ann N Y Acad Sci 1203:53–59
Wu Q, Yao B, Li N, Ma L, Deng Y, Yang Y, Zeng C, Yang Z, Liu B (2017) Nrf2 mediates redox adaptation in NOX4-overexpressed non-small cell lung cancer cells. Exp Cell Res 352(2):245–254
Xue EX, Lin JP, Zhang Y, Sheng SR, Liu HX, Zhou YL, Xu H (2017) Pterostilbene inhibits inflammation and ROS production in chondrocytes by activating Nrf2 pathway. Oncotarget 8(26):41988–42000
Yang CP, Liu YC (2018) Therapeutics for inflammatory-related diseases based on plasmon-activated water: a review. Int J Mol Sci 19(6):1589
Yang Z, Guan Y, Li J, Li L, Li Z (2018) Chrysin attenuates carrageenan-induced pleurisy and lung injury via activation of SIRT1/NRF2 pathway in rats. Eur J Pharmacol 836:83–88
Ye X, Zuo D, Yu L, Zhang L, Tang J, Cui C, Bao L, Zan K, Zhang Z, Yang X, Chen H, Tang H, Zu J, Shi H, Cui G (2017) ROS/TXNIP pathway contributes to thrombin induced NLRP3 inflammasome activation and cell apoptosis in microglia. Biochem Biophys Res Commun 485(2):499–505
Zhang M, Pan H, Xu Y, Wang X, Qiu Z, Jiang L (2017) Allicin decreases lipopolysaccharide-induced oxidative stress and inflammation in human umbilical vein endothelial cells through suppression of mitochondrial dysfunction and activation of Nrf2. Cell Physiol Biochem 41(6):2255–2267
Zhang L, Previn R, Lu L, Liao RF, Jin Y, Wang RK (2018) Crocin, a natural product attenuates lipopolysaccharide-induced anxiety and depressive-like behaviors through suppressing NF-kB and NLRP3 signaling pathway. Brain Res Bull 142:352–359
Zhu C, Dong Y, Liu H, Ren H, Cui Z (2017) Hesperetin protects against H2O2-triggered oxidative damage via upregulation of the Keap1-Nrf2/HO-1 signal pathway in ARPE-19 cells. Biomed Pharmacother 88:124–133.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant No. 81870030) and the General Financial Grant from the China Postdoctoral Science Foundation (Grant No. 2018T110257).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, H., Huang, J., Gao, Y. et al. Oridonin attenuates carrageenan-induced pleurisy via activation of the KEAP-1/Nrf2 pathway and inhibition of the TXNIP/NLRP3 and NF-κB pathway in mice. Inflammopharmacol 28, 513–523 (2020). https://doi.org/10.1007/s10787-019-00644-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-019-00644-y