Abstract
Objectives
To evaluate the utility of elevated serum P-glycoprotein (P-gp) as a risk marker of therapeutic response failure in rheumatoid arthritis (RA) patients treated with disease-modifying antirheumatic drugs (DMARDs).
Methods
A cross-sectional study was conducted in 151 RA patients. Patients were classified into two groups according to the response achieved in terms of the disease activity score (DAS)28 after ≥ 6 months: (1) patients with a therapeutic response to DMARDs, with DAS28 < 3.2; and (2) patients without a response to DMARDs, with persistent DAS28 ≥ 3.2. We explored a wide group of clinical factors associated with therapeutic resistance. Serum P-gp levels were measured by ELISA. The risk of P-gp elevation as a marker of failure to achieve a therapeutic response to DMARDs was computed using multivariate logistic regression.
Results
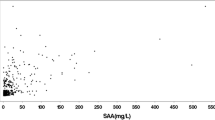
Serum P-gp levels were significantly higher in RA patients (n = 151) than in the controls (n = 30) (158.70 ± 182.71 ng/mL vs. 14.12 ± 8.97 ng/mL, p < 0.001). The P-gp level was correlated with the DAS28 score (r = 0.39, p < 0.001). RA patients with DMARD failure had higher serum P-gp levels than patients with a therapeutic response (206 ± 21.47 ng/mL vs 120.60 ± 15.70 ng/mL; p = 0.001). High P-gp levels increased the risk of DMARD failure (OR 3.36, 95% CI 1.54–7.27, p = 0.001). After adjusting for confounding variables, elevated P-gp remained associated with DMARD failure (OR 2.64, 95% CI 1.29–5.40, p = 0.01).
Conclusion
Elevated serum P-gp is associated with DMARD failure. The P-gp level can be considered a clinical tool for evaluating the risk of DMARD failure in patients; however, future prospective studies should be performed to evaluate the utility of this marker in predicting long-term responses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, clinical practice guidelines consider synthetic disease-modifying antirheumatic drugs (DMARDs) the primary drugs of choice for treating rheumatoid arthritis (RA) (Bombardier et al. 2012; Smolen et al. 2014; Cardiel et al. 2014; Singh et al. 2016). In developing countries, there is an elevated rate of RA patients who undergo long-term treatment with DMARDs (Cardiel et al. 2012). A multicentre survey in Mexico has shown that approximately 93% of patients are treated with synthetic DMARDs, whereas only 6% of patients are treated with biologic DMARDs (Goycochea-Robles et al. 2007). In a previous study, only 23% of RA patients receiving synthetic DMARDs achieved a response after 24 weeks (Machado et al. 2014). An interesting study has shown that nearly 27% of RA subject, including those receiving synthetic or biologic DMARDs, have an inadequate control of the disease (Taylor et al. 2018). Failure to achieve a therapeutic response cannot be explained by a single cause due to the influences of genetic characteristics, comorbidities, disease characteristics (Vasconcelos and Faria 2012) and transporter molecules involved in the therapeutic resistance (Nigam 2014; Silva et al. 2015). P-glycoprotein (P-gp) is a protein transporter that belongs to the ABCB subfamily encoded in humans by the MDR1 gene (Juliano and Ling 1976; Silva et al. 2015). The overexpression of P-gp on lymphocytes is associated with resistance to drugs in RA and systemic lupus erythematosus (SLE). (Tsujimura et al. 2008; Kansal et al. 2015). The overexpression of P-gp on the membrane of lymphocytes in patients with moderate or severe disease activity despite treatment has been described (Tsujimura et al. 2008, 2010, 2017; Agarwal et al. 2009; Prasad et al. 2014). However, the determination of P-gp expression on the cell membrane is used only for research studies, and it is not feasible for the clinical practice because of the associated costs, availability, and technical expertise. Therefore, the quantification of soluble P-gp in sera can be performed by ELISA (Perez-Guerrero et al. 2018), which could facilitate the evaluation of P-gp in clinical practice.
Recently, our group described an association between elevated P-gp level and disease activity resistant to immunosuppressive drugs, including mofetil mycophenolate and azathioprine (Perez-Guerrero et al. 2018). Nevertheless, currently, there is no information regarding whether P-gp levels can be used as a marker of therapeutic resistance in RA receiving DMARDs. This information could be useful for clinicians in identifying a marker of therapeutic resistance with the aim of facilitating clinical decision-making. Therefore, the objective of the present work was to evaluate the utility of elevated serum P-gp as a risk marker of therapeutic failure in RA treated with DMARDs.
Materials and methods
Study design
Cross-sectional study.
Clinical setting
This study included patients with RA from an outpatient rheumatology clinic of a secondary-care hospital [Hospital General Regional 110, Instituto Mexicano del Seguro Social (IMSS)] in Guadalajara, Mexico. Additionally, as healthy controls (HCs), 30 clinically healthy females were recruited as blood donors; these donors were similar to the patients in age (≥ 18 years), and similar exclusion criteria were applied.
Patients and methods
All RA patients met the 1987 ACR criteria (Arnett et al. 1988) along with the following inclusion criteria: (1) age of 18 years or older; (2) currently treated with DMARDs at a stable dosage during the 6 months prior to the study onset; and (3) considered to have active disease at the time of starting DMARD treatment, with a disease activity score (DAS)28 ≥ 5.2. We excluded patients with an overlapping syndrome (characteristics of two autoimmune connective tissue diseases present in the same patient), pregnancy, antecedents of cancer, epilepsy, chronic viral infections (hepatitis C or B virus or human immunodeficiency virus), or acute bacterial, viral, or fungal infections. We excluded patients who were taking a drug acting as a P-gp inhibitor (including analgesics, antiarrhythmics, calcium channel blockers, cyclosporine A, tacrolimus, sirolimus, sertraline, paroxetine, fluoxetine, ketoconazole, and progesterone).
Clinical assessment
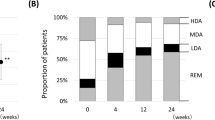
A structured interview was performed to evaluate epidemiological and clinical variables. Disease activity was assessed in all RA patients using the combined DAS28-erythrocyte sedimentation rate (ESR) score (Prevoo et al. 1995). All the included RA subjects were categorized into two groups on the basis of the therapeutic response, as measured by DAS28: group 1, RA patients with a therapeutic response [achieving low disease activity (DAS28 < 3.2–2.6) or remission (DAS28 < 2.6) after a sustained treatment with DMARDs for at least 6 months]; group 2, RA subjects with persistent DAS28 ≥ 3.2 after 6 months of sustained treatment with DMARDs.
Serum determinations of P-gp levels
Peripheral blood samples were collected from patients and controls in the morning. Serum samples were frozen at −20 °C until determination of the P-gp level. All these samples were coded before P-gp level quantification to minimize measurement bias. P-gp measurements were determined by the same researcher, who was unaware to any clinical characteristics and groups. P-gp levels were determined by ELISA (MyBioSource, Inc., San Diego, CA, USA).
Other laboratory determinations
The ESR was determined by the Westergren method, whereas the C-reactive protein (CRP) and rheumatoid factor (RF) titles were measured using nephelometry. Our laboratory applied the following reference values: positive RF > 12 IU/mL and CRP > 10 mg/L.
Statistical analysis
Quantitative variables are shown as the mean ± standard deviation (SD) and qualitative variables as frequencies and proportions (%). Bivariate comparisons of quantitative variables between (a) RA patients and HCs or (b) RA with versus without a therapeutic response were performed using the statistical Student’s t test. For comparisons of proportions, we used the Chi-square test (or Fisher exact test). For identifying the strength of the correlation between the P-gp level, DAS28 and other quantitative variables we used Pearson test.
To estimate the utility of elevated P-gp level for detecting patients at risk for therapeutic failure with DMARDs, we computed the sensitivity, specificity, and predictive values. To build the tetrachoric tables used for computing utility values, the first step was to identify the patients with an elevated P-gp level. We computed the terciles of the serum P-gp values in RA patients. We arbitrarily considered the higher tercile (> 142 ng/mL) as representing patients with a high P-gp level.
Sensitivity was considered as the probability of observing a high P-gp level (> 142 ng/mL) in RA subjects who did not achieve a therapeutic response. Specificity was considered as the probability of observing a non-elevated P-gp level in patients who achieved a therapeutic response. The positive predictive value (PPV) was identified as the probability of a therapeutic response failure in RA subjects with a high P-gp level (> 142 ng/mL), and the negative predictive value (NPV) was considered as the proportion of non-therapeutic response in RA patients with low P-gp level. Additionally, we computed the odds ratios (ORs) and their 95% confidence intervals (95% CIs) for the risk of elevated P-gp levels in RA developing DMARD treatment failure.
To adjust for confounders, we used multivariate logistic regression analysis. We built the models using failure to respond to DMARDs (dependent variable) including as covariates all the variables with a statistical significance (p < 0.20) in the bivariate analysis. We included in all the models an adjustment by age and disease duration. The results of the forward method are presented as adjusted ORs and the corresponding 95% CIs.
We included multiple regression models to assess those characteristics related with the P-gp level. As covariates, we introduced variables that were significantly correlated with the P-gp level according to the Pearson test (p < 0.20) or have biological plausibility for explaining the P-gp level. The results of the forward method are presented. Statistical significance was considered at the 0.05 level. We used for the statistical analyses the IBM SPSS software ver. 23 (Statistics/IBM Corp., Chicago, IL, USA).
Ethics
We followed the recommendations described by the 64th Declaration of Helsinki to conduct this study. The study protocol was in accordance with the lineaments of the Ethics and Research Board of our Hospital (UMAE Centro Medico Nacional de Occidente del Instituto Mexicano del Seguro Social 13-01). Approval code: R-2014- 1301-77. All the participants signed voluntary written informed consent before the study onset.
Results
One hundred and fifty-one patients with RA and thirty blood donors without chronic diseases were initially compared. Data not shown in tables indicated that the RA patients were similar in age (58.01 ± 13.26 years vs. 55.07 ± 9.88 years; p = 0.89), weight (66.48 ± 11.45 kg vs. 64.75 ± 11.73 kg; p = 0.46), height (154.82 ± 5.68 cm vs. 156.60 ± 6.03 cm; p = 0.46), and smoking proportion (9.7% vs. 13.3%; p = 0.49). RA patients had significantly higher serum P-gp levels than did the HCs (158.70 ± 182.71 ng/mL vs. 14.12 ± 8.97 ng/mL, p < 0.001).
Table 1 shows the general characteristics of the patients with RA included in the study. These patients had a mean age of 58 years and a mean disease duration of 12.7 years. Approximately, 39% of RA patients achieved a response after 6 months of treatment with DMARDs; consequently, 61% of the patients included did not achieve a therapeutic response to DMARDs. Methotrexate was the DMARD most commonly used in these patients (57.6%), followed by sulfasalazine (33.8%) and leflunomide (32.5%); only 8.6% of patients were treated with biologic DMARDs. Fifty-three percent of the patients were treated with a combination of two synthetic DMARDs, and 10.6% of RA patients were treated with a combination of three or more synthetic DMARDs.
Table 2 shows the correlations between the serum P-gp level and other variables. The P-gp levels were positively correlated with the DAS28 score (r = 0.39, p < 0.001), swollen joint count (r = 0.22, p = 0.01), painful joint count (r = 0.37, p < 0.001), and patients’ global health on the visual analog scale (r = 0.22, p = 0.01). The P-gp level was not correlated with acute-phase reactants (ESR or CRP), age, or disease duration.
RA patients with DMARD failure had higher serum P-gp levels than patients with a therapeutic response (206 ± 21.47 ng/mL vs 120.60 ± 15.70 ng/mL; p = 0.001). RA patients with DMARD failure were being treated with slightly higher prednisone doses at the time of the study, and this difference was significant (6.80 ± 3.82 mg/day vs 5.65 ± 2.08 mg/day; p = 0.04). Other variables, including age, disease duration, and specific DMARDs, were not different between RA patients with and without DMARD failure. These results are shown in Table 3. Data not shown in tables revealed similar P-gp levels in patients treated with 1, 2 and ≥ 3 DMARDs (p = 0.48). Differences in the P-gp level were not observed between patients treated with anti-TNF-α agents and patients not treated with biologic DMARDs (p = 0.78).
Sensitivity, specificity, and predictive values of serum P-gp level and risk of therapeutic failure
Data not shown in tables revealed that the presence of P-gp > 142 ng/mL had a sensitivity of 78%, specificity of 48%, NPV of 81.36%, and PPV of 43.48% for discriminating patients with an inadequate therapeutic response to DMARDs. Moreover, higher P-gp levels increased the risk of DMARD failure (OR 3.36, 95% CI 1.54–7.27, p = 0.001).
Multivariate assessment of variables associated with DMARD therapeutic failure
Table 4 shows the results of the logistic regression analysis used for identifying factors associated with DMARD failure. After adjusting for age, disease duration, and anti-TNF agents, P-gp > 142 ng/mL (OR 2.64, 95% CI 1.29–5.40, p = 0.01) and the glucocorticoid dose (OR 1.20, 95% CI 1.01–1.41, p = 0.03) remained associated with DMARD failure.
We then performed a multivariate multiple regression analysis. After adjusting for age, disease duration, and glucocorticoid dose, the P-gp level remained associated with the DAS28 score (B coefficient: 52.68, 95% CI 32.59–72.76, p < 0.001). These data are not shown in tables.
Discussion
This work revealed a strong relation between elevated serum P-gp and failure to DMARDs in RA patients. A high P-gp level was associated in the multivariate analysis with a threefold greater risk of DMARD failure independent from the glucocorticoid dose.
Several studies have observed an association between an overexpression of P-gp on the membrane of leukocytes and disease activity assessed by DAS28 in RA subjects (Tsujimura et al. 2008, 2010; Agarwal et al. 2009; Prasad et al. 2014). Nevertheless, this is the first study to evaluate the clinical value of elevated serum P-gp as a biomarker for an increased risk of failure to achieve a therapeutic response to DMARDs. Some reports have associated the elevated serum P-gp level with the expression of this transporter on the membrane surface (Chu et al. 1994; Chiampanichayakul et al. 2010). Kato et al. observed that P-gp is transported to the serum by exosomes (Kato et al. 2015). Chiampanichayakul et al. reported the use of monoclonal antibodies directed against surface P-gp and soluble P-gp, demonstrating that these autoantibodies are useful for identifying leukemia patients with P-gp expressed on the cell membrane (Chiampanichayakul et al. 2010). Currently, serum P-gp levels can be quantified by ELISA, and we have identified a relation of serum P-gp level with therapeutic resistance in SLE (Perez-Guerrero et al. 2018).
Studies evaluating P-gp expression on the surface of the cell membrane are limited in their applicability to regular clinical assessments by being requiring a hospital with adequate equipment and technical training. Serum P-gp quantification by ELISA might serve as an adequate strategy regarding cost, availability, and clinical value for identifying patients at risk for failing to achieve a therapeutic response to treatments for RA. To the best of our knowledge, this is the first study to assess the clinical value of P-gp in RA patients with therapeutic failure. According to our results, elevated P-gp has a sensitivity of 78% for detecting patients with therapeutic failure and confers a threefold greater risk of therapeutic failure.
Our results revealed an association between the serum P-gp level and more active disease in RA. These findings are in accordance with those of several works that have identified P-gp is overexpressed on the cell membrane of lymphocytes (Tsujimura et al. 2008, 2010, 2017; Agarwal et al. 2009). Moreover, similar to our findings, other authors have observed a correlation of P-gp overexpression and increased DAS28 scores (Tsujimura et al. 2008, 2010, 2017; Agarwal et al. 2009). Additionally, this overexpression of P-gp on the surface of the cell membrane is associated with resistance to DMARDs and glucocorticoids (Tsujimura et al. 2008; Agarwal et al. 2009).
In vitro, glucocorticoids can stimulate the expression of P-gp (Bauer et al. 2004; Callaghan et al. 2008). Kansal et al. have reported that high glucocorticoid doses are associated with increased P-gp expression (Kansal et al. 2015). Compared with previous studies, in this work, a high rate of RA subjects received low doses of corticosteroids. Even with these low corticosteroid doses, the dose of prednisone was related with the P-gp level in the multivariate analysis.
Our study has several limitations. First, since this is the first study to assess the clinical value of the serum P-gp level in terms of the risk of DMARD therapeutic failure, we have no other studies with which to evaluate the consistency of our findings; thus, we supported our findings with previously described observations of P-gp membrane expression. New studies with clinical objectives evaluating P-gp serum levels are required. Second, since this was a cross-sectional work of RA individuals with different disease durations, we were unable to calculate relative risk, a strong measure for identifying the conferred risk of therapeutic failure. Therefore, future studies should be performed using prospective cohorts of subjects with early RA to identify the risk of long-term failure in patients starting DMARD treatment.
Some P-gp inhibitors have been evaluated as adjuvants for the treatment of cancer (Binkhathlan and Lavasanifar 2013). Among RA patients, Suzuki et al. observed that after low doses of tacrolimus or cyclosporine, a small sample of RA refractory to DMARDs achieved improved disease activity after 2 weeks of treatment with P-gp inhibitors (Suzuki et al. 2010). These interesting data are promising for further studies evaluating whether other P-gp inhibitors, such as fluoxetine or verapamil, might be used to improve the clinical response.
Conclusion
In conclusion, the serum P-gp level is associated with the failure to achieve a therapeutic response to DMARDs in RA patients. Although multiple factors are associated with this failure, with this knowledge, the P-gp level can be considered an useful clinical tool, as this level can be modified. Further studies are needed to identify the consistency of our findings and determine the potential clinical utility of P-gp inhibitors in RA subjects who fail to achieve a response to conventional therapies.
References
Agarwal V, Mittal SK, Misra R (2009) Expression of multidrug resistance-1 protein correlates with disease activity rather than the refractoriness to methotrexate therapy in rheumatoid arthritis. Clin Rheumatol 28:427–433. https://doi.org/10.1007/s10067-008-1071-1
Arnett FC, Edworthy SM, Bloch DA et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324. https://doi.org/10.1002/art.1780310302
Bauer B, Hartz AMS, Fricker G, Miller DS (2004) Pregnane X receptor up-regulation of P-glycoprotein expression and transport function at the blood-brain barrier. Mol Pharmacol 66:413–419. https://doi.org/10.1124/mol.66.3
Binkhathlan Z, Lavasanifar A (2013) P-glycoprotein inhibition as a therapeutic approach for overcoming multidrug resistance in cancer: current status and future perspectives. Curr Cancer Drug Targets 12:326–346. https://doi.org/10.2174/15680096113139990076
Bombardier C, Hazlewood GS, Akhavan P et al (2012) Canadian Rheumatology Association recommendations for the pharmacological management of rheumatoid arthritis with traditional and biologic disease-modifying antirheumatic drugs: part II safety. J Rheumatol 39:1583–1602. https://doi.org/10.3899/jrheum.120165
Callaghan R, Crowley E, Potter S, Kerr ID (2008) P-glycoprotein: so many ways to turn it on. J Clin Pharmacol 48:365–378. https://doi.org/10.1177/0091270007311568
Cardiel MH, Pons-Estel BA, Sacnun MP et al (2012) Treatment of early rheumatoid arthritis in a multinational inception cohort of latin american patients. J Clin Rheumatol 18:327–335. https://doi.org/10.1097/rhu.0b013e31826d6610
Cardiel MH, Díaz-Borjón A, del Mercado Vázquez, Espinosa M et al (2014) Update of the mexican college of rheumatology guidelines for the pharmacologic treatment of rheumatoid arthritis. Reumatol Clín (English Ed). 10:227–240. https://doi.org/10.1016/j.reumae.2013.10.006
Chiampanichayakul S, Anuchapreeda S, Chruewkamlow N et al (2010) Production of monoclonal antibodies to P-glycoprotein: its application in detection of soluble and surface P-glycoprotein of leukemia patients. Int J Hematol 92:326–333. https://doi.org/10.1007/s12185-010-0668-8
Chu TM, Lin TH, Kawinski E (1994) Detection of soluble P-glycoprotein in culture media and extracellular fluids. Biochem Biophys Res Commun 203:506–512. https://doi.org/10.1006/bbrc.1994.2211
Goycochea-Robles MV, Arce-Salinas CA, Guzmán-Vázquez S, Cardiel-Ríos MH (2007) Prescription rheumatology practices among mexican specialists. Arch Med Res 38:354–359. https://doi.org/10.1016/j.arcmed.2006.11.008
Juliano RL, Ling V (1976) A surface glycoprotein modulating drug permeability in chinese hamster ovary cell mutants. Biochim Biophys Acta 455:152–162. https://doi.org/10.1016/0005-2736(76)90160-7
Kansal A, Tripathi D, Rai MK, Agarwal V (2015) Persistent expression and function of P-glycoprotein on peripheral blood lymphocytes identifies corticosteroid resistance in patients with systemic lupus erythematosus. Clin Rheumatol. https://doi.org/10.1007/s10067-015-3079-7
Kato T, Mizutani K, Kameyama K et al (2015) Serum exosomal P-glycoprotein is a potential marker to diagnose docetaxel resistance and select a taxoid for patients with prostate cancer. Urol Oncol 33:385.e15–385.e20. https://doi.org/10.1016/j.urolonc.2015.04.019
Machado DA, Guzman RM, Xavier RM et al (2014) Open-label observation of addition of etanercept versus a conventional disease-modifying antirheumatic drug in subjects with active rheumatoid arthritis despite methotrexate therapy in the latin american region. J Clin Rheumatol 20:25–33. https://doi.org/10.1097/rhu.0000000000000055
Nigam SK (2014) What do drug transporters really do? Nat Rev Drug Discov 14:29–44. https://doi.org/10.1038/nrd4461
Perez-Guerrero EE, Gamez-Nava JI, Muñoz-Valle JF et al (2018) Serum levels of P-glycoprotein and persistence of disease activity despite treatment in patients with systemic lupus erythematosus. Clin Exp Med 18:109–117. https://doi.org/10.1007/s10238-017-0459-0
Prasad S, Tripathi D, Rai MK et al (2014) Multidrug resistance protein-1 expression, function and polymorphisms in patients with rheumatoid arthritis not responding to methotrexate. Int J Rheum Dis 17:878–886. https://doi.org/10.1111/1756-185x.12362
Prevoo MLL, Van’T Hof MA, Kuper HH et al (1995) Modified disease activity scores that include twenty-eight-joint counts development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48. https://doi.org/10.1002/art.1780380107
Silva R, Vilas-Boas V, Carmo H et al (2015) Modulation of P-glycoprotein efflux pump: induction and activation as a therapeutic strategy. Pharmacol Ther 149:1–123. https://doi.org/10.1016/j.pharmthera.2014.11.013
Singh JA, Saag KG, Bridges SLJ et al (2016) 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 68:1–25. https://doi.org/10.1002/acr.22783
Smolen JS, Landewé R, Breedveld FC et al (2014) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 73:492–509. https://doi.org/10.1136/annrheumdis-2013-204573
Suzuki K, Saito K, Tsujimura S et al (2010) Tacrolimus, a calcineurin inhibitor, overcomes treatment unresponsiveness mediated by P-glycoprotein on lymphocytes in refractory rheumatoid arthritis. J Rheumatol 37:512–520. https://doi.org/10.3899/jrheum.090048
Taylor PC, Alten R, Gomez-Reino JJ et al (2018) Clinical characteristics and patient-reported outcomes in patients with inadequately controlled rheumatoid arthritis despite ongoing treatment. RMD Open 4:e000615. https://doi.org/10.1136/rmdopen-2017-000615
Tsujimura S, Saito K, Nawata M et al (2008) Overcoming drug resistance induced by P-glycoprotein on lymphocytes in patients with refractory rheumatoid arthritis. Ann Rheum Dis 67:380–388. https://doi.org/10.1136/ard.2007.070821
Tsujimura S, Saito K, Nakayamada S, Tanaka Y (2010) Etanercept overcomes P-glycoprotein-induced drug resistance in lymphocytes of patients with intractable rheumatoid arthritis. Mod Rheumatol 20:139–146. https://doi.org/10.1007/s10165-009-0247-0
Tsujimura S, Adachi T, Saito K et al (2017) Relevance of P-glycoprotein on CXCR4+ B cells to organ manifestation in highly active rheumatoid arthritis. Mod Rheumatol. https://doi.org/10.1080/14397595.2017.1341458
Vasconcelos C, Faria R (2012) Therapeutic resistance in autoimmune diseases. Lupus. https://doi.org/10.1177/0961203312462266
Funding
This project was financed by a grant from the Mexican Institute for Social Security (IMSS), Fondo de Investigación en Salud (FIS), Grant no. FIS/IMSS/PROT/G14/1296.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest to disclose.
Ethical approval
Comité Local de Investigación y Ética en Salud 1301. Hospital de Especialidades, Centro Médico Nacional de Occidente LIC. IGNACIO GARCIA TELLEZ, Jalisco. Date when the study was approved: April 11th, 2014. Reference Number of approval: R-2014-1301-77.
Rights and permissions
About this article
Cite this article
Perez-Guerrero, E.E., Gonzalez-Lopez, L., Muñoz-Valle, J.F. et al. Serum P-glycoprotein level: a potential biomarker of DMARD failure in patients with rheumatoid arthritis. Inflammopharmacol 26, 1375–1381 (2018). https://doi.org/10.1007/s10787-018-0529-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-018-0529-2