Abstract
Objectives
This review examines the pharmacokinetics, modes of action and therapeutic properties of the anti-malarial drugs, hydroxychloroquine (HCQ) and chloroquine (CQ), in the treatment of systemic lupus erythematosus (SLE), rheumatoid arthritis (RA) and related conditions, as well as osteoarthritis (OA).
Key findings
Both HCQ and CQ have historically been employed successfully for the treatment of SLE and RA for over 70 years. HCQ has been used extensively for SLE where it has a good reputation for controlling the dermatological complications in SLE. It has also been reported to effectively control the symptoms of Sjøgren’s syndrome, as well as preventing thrombosis in phospholipid antibody (aPL) syndrome. In RA and SLE, HCQ is preferred because of the lower incidence of gastrointestinal adverse reactions compared with CQ and it might have a lower risk of ocular adverse reactions. There is increasing evidence that HCQ may reduce atherosclerosis and risks of cardiovascular disease in rheumatic patients. Both HCQ and CQ have been shown to improve glycaemia and reduce the risks of type II diabetes mellitus. Although both HCQ and CQ are effective in low-moderate RA, HCQ is now preferred as part of combination therapy for more severe disease. The advantages of combination therapy are that the doses of the individual drugs may be lowered so reducing adverse reactions. Both HCQ and CQ are diastereoisomers, have basic properties and are given as the sulphate and phosphate salts. While being relatively well absorbed orally and with good bioavailability, they have long and variable plasma terminal elimination half-lives (approximately 40–60 days). This reflects their high volume of distribution, V D (HCQ 44,000L; CQ 65,000L) which extends into aqueous compartments, long mean residence time (HCQ 1300 h; CQ 900 h) and with about half the drugs (metabolites) undergoing renal clearance. The strong binding to melanin reflects the ocular injury and dermatological properties of these drugs. The consensus is that the occurrence of ocular adverse reactions can be minimised by close attention to the dose (which should be set on a body weight basis) with regular (e.g. quarterly) retinal examination. Although HCQ and CQ can pass through the placenta, the use of these drugs during pregnancy does not appear to risk harm to the baby and might be beneficial to the mother with SLE and her child by controlling the SLE disease activity, which is known to be an important factor affecting pregnancy outcome. The modes of action of HCQ and CQ in these arthritides represent somewhat of an enigma. Undoubtedly, these drugs have multiple actions related, in part, their ability to accumulate in lysosomes and autophagosomes of phagocytic cells as well as affecting MHC Class II expression and antigen presentation; actions of the production of pro-inflammatory cytokines [e.g. interleukin-1 (IL-1) tumour necrosis factor-α (TNFα)]; control of toll-like receptor-9 activation; and leucocyte generation of reactive oxygen species (ROS); i.e. antioxidant activity. The actions of these drugs on T and B cells are less clear but may depend on these leucocyte-mediated actions. Anti-malarials also protect against cytokine-mediated cartilage resorption. This and other actions may underlie the potential benefits in treating OA. The exact relationships of these various actions, mostly determined in vitro, have not been specifically defined in vivo or ex vivo in relation to clinical efficacy.
Outcomes
HCQ and CQ have a good reputation for being effective and relatively safe treatments in SLE, mild-moderate RA and Sjøgren’s syndrome. There is need for (a) more information on their mode of action in relation to the control of these diseases, (b) scope for developing formulations that have improved pharmacokinetic and therapeutic properties and safety, and (c) further exploring their use in drug combinations not only with other disease-modifying agents but also with biologics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
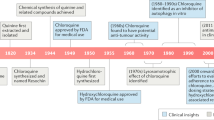
Quinine was the first of the anti-malarials to be used in treating connective tissue disease, following the pioneering observations by Payne (1894) of the effectiveness of this drug for treating skin lesions in systemic lupus erythematosus (SLE) (Payne 1894). Page (1951) reported the successful treating 18 patients with cutaneous SLE with the anti-malarial, mepacrine hydrochloride (quinacrine hydrochloride, Atabrine®). Previously, treatment with anti-malarials (e.g. quinine, quinacrine) had been found to ameliorate rheumatic symptoms in soldiers during World War II who look these drugs for the treatment and prophylaxis of malaria (Rynes 1992). This was quickly followed by interest in the use of anti-malarials in the treatment of systemic or cutaneous lupus with mepacrine until 1961 (Page 1951), but later this was succeeded by chloroquine (CQ) and later hydroxychloroquine (HCQ) (Littler 1990; Rynes 1992; Wallace 1996).
CQ and HCQ were produced as part of the wartime efforts to obtain anti-malarials during World War II by the USA. CQ had been originally synthesised and patented by Andersag, Breitner and Jung in 1937, with the patent being assigned to IG Fabenindustrie AG (quoted in Evans and Williamson 1987; Sneader 2005). Later development during and after World War II was undertaken by the Winthrop Chemical Company in the USA (Sneader 2005). The synthesis of CQ based on both the IG Fabenindustrie patent and Winthrop’s developments involves m-chloraniline being condensed in the presence of acetic acid with ethyl ethoxalylacetate to give the anilinino derivative, which is cyclised by heating to give a mix of the 5- and 7-chloroquinolines; the latter isomer being removed by crystallisation (Sneader 2005). Subsequent decarboxylation of the 5-isomer by heating produces 4,7-dichloroquinoline which is condensed with 4-diethylamino-1-methylbutylamine to give CQ; this is then converted to the diphosphate salt for commercial formulation. A subsequent method of AR Surrey and HF Hammer in 1946 enabled the 5-isomer to be exclusively produced without the unwanted 7-isomer (Sneader 2005). HCQ has an N-hydroxy-ethyl side chain in place of those on the N-diethyl group of CQ. HCQ is prepared by condensing N 1-N-ethyl-N 1-β-hydroxyethyl-1,4-pendanediamine with 4,7-dichloroquinoline to give HCQ (Sneader 2005). HCQ is now the more widely used of these two 4-aminoquinolines (Sneader 2005) following subsequent commercial development by Sterling-Winthrop in the USA and is now marketed as Plaquenil® (Sanofi-Aventis). CQ (Resochin®, Sanoquin®, Nivaquin B®) is available as a generic compound (Sneader 2005).
Clinical applications of HCQ and CQ in treating rheumatic diseases have been widely reported (Littler 1990; Rynes 1992, 1997; Dubois 1967, 1978; Mackenzie 1970, 1983a, b, c; Laaksonen et al. 1974; Maksymowych and Russell 1987; Adams et al. 1983; Baum 1983; Bellamy and Brooks 1986; Tett et al. 1990; Kruize et al. 1993; Nayak and Esdaile 1996; Fox et al. 1996; Clarke 1998; Avina-Zubieta et al. 1998; Conaghan et al. 1997; Canadian Rheumatology Association 2000; Dawson et al. 2005; Ruiz-Irastorza and Khamashta 2008, 2010; Ruiz-Irastorza et al. 2010; Katz and Russell 2011). Their efficacy in discoid and systemic lupus has been well established (Littler 1990; Rynes 1992, 1997; Dubois 1967; Laaksonen et al. 1974; Maksymowych and Russell, 1987; Tett et al. 1990; Fox et al. 1996; Canadian Rheumatology Association 2000; Das et al. 2002, 2007; Dawson et al. 2005; Ruiz-Irastorza and Khamashta 2008, 2010; Ruiz-Irastorza et al. 2010; Tang et al. 2012). A systematic review of randomised controlled trials and observational studies on the clinical efficacy and safety of anti-malarials (AMs) by Ruiz-Irastorza et al. (2010) showed that (a) high levels of evidence exist for AMs (mainly HCQ) in preventing lupus flares, increased long-term survival of patients and lupus activity in pregnant women without harm to babies; (b) moderate evidence exists for their prevention of irreversible organ damage, prevention of bone destruction, and prevention of thrombosis; and (c) weaker evidence exists for reduction in severe lupus activity, lipid levels and sub-clinical atherosclerosis. The toxicity of AMs is of mild grade, infrequent and usually reversible, with HCQ having the safer profile (Ruiz-Irastorza and Khamashta 2008), particularly where there is attention to dosage (Marmor 2004).
Based on their review, Ruiz-Irastorza et al. (2010) recommended that HCQ should be given to most patients with lupus during the full course of the disease. Indeed, Ruiz-Irastorza and Khamashta (2008) have described HCQ as being the “cornerstone of lupus therapy”. HCQ is a frequent option for the treatment of mild-moderate rheumatoid arthritis (RA) (Rynes 1992; Mackenzie 1983a, b, c; Maksymowych and Russell 1987; Bellamy and Brooks 1986; Tett et al. 1990; Clarke 1998; Avina-Zubieta et al. 1998; Conaghan et al. 1997; Canadian Rheumatology Association 2000; Marmor 2004), Sjøgren’s syndrome (Kruize et al. 1993; Fox et al. 1996; Clarke 1998; Dawson et al. 2005) where its actions have been attributed to reversing hypoactive glandular anti-cholinesterase activity (Dawson et al. 2005), and juvenile rheumatoid arthritis (Laaksonen et al. 1974; Baum 1983). These drugs are amongst the cheapest of the disease-modifying anti-rheumatic agents (DMARDs) that are currently available and appreciably less costly than biologics (Choi et al. 2000; RxFiles Detailing Program (2008); British National Formulary 2009).
In severe RA, it has been long established to employ combinations of AMs with various other DMARDs, azathioprine or biologics (McCarty and Carrera 1982; Csuka et al. 1986; Paulus 1988; Furst 1993; Trnavsky et al. 1993; Lomater et al. 1994; Salaffi et al. 1996; Clegg et al. 1997; O’Dell 1998, 1999; Biasi et al. 2000; O’Dell et al. 2001, 2006; Goekoop et al. 2001; Carmichael et al. 2002; Verstappen et al. 2003; Mottonen et al. 2002; Katchamart et al. 2009; van Vollenhoven et al. 2009). The relative benefits of these combinations have been favourable, but the optimal therapeutic combinations and treatment regimes have not been well established.
Historically, research on the mode of actions of CQ was directed towards understanding its effects in the treatment of malaria (McChesney 1983; McChesney and Fitch 1984; Wallace 1996; Littler 1990; Rynes 1992; Sneader 2005). Coincidentally, the use of anti-malarials other than CQ (quinine, quinacrine, pamaquine) for treating SLE in the 1930s preceded the introduction of CQ for SLE and RA as well as during the latter part of World War II for treating malaria (Wallace 1996). Yet interest in the anti-malarial actions of CQ arose after it was developed and applied clinically with very limited, if any understanding how it might work.
Pharmacokinetics
The pharmacokinetics (PK) properties of HCQ and CQ have posed considerable problems and complexities despite intensive investigations over the years. As a consequence, it has been difficult to relate the pharmacokinetics (PKs) of these drugs to their efficacy in different rheumatic conditions, as well as in relation to their mode of actions and adverse or side effects. There have been a number of reviews published on the PKs of HCQ and CQ in relation to application in rheumatic diseases to which the reader is referred (Rynes 1992; Tett et al. 1993; McChesney and Fitch 1984; McChesney 1983; White 1985; Cutler et al. 1988; Titus 1989; Cutler 1993; Tett 1993; Furst 1996; Davila and Ranganathan 2011).
The complexities in understanding the PKs of these drugs are related to: (a) their intrinsic physico-chemical properties being aqua-soluble basic compounds; CQ having 2 pKa’s comprising pKa1 of 10.2 and pKa2 of 8.1 (Perrin 1965); (b) existence as R(−) and S(+) enantiomers (see Fig. 1) (Witiak et al. 1981; Craig et al. 1988; Titus 1989; Brocks et al. 1992; Brocks and Mehvar 2003) with variable stereo-selective elimination (Iredale et al. 1993; McLachlan et al. 1993, 1994; Tett et al. 1994; Ducharme et al. 1995; Midha et al. 1998; Munster et al. 2002; Brocks and Mehvar 2003; de Oliveira et al. 2007); (c) wide variability in the concentration profiles from sampling of blood or plasma which is possibly due to differences in the sensitivity of analytical methods and calculations of kinetic parameters, especially the terminal elimination plasma half-life (T 1/2) (Cutler et al. 1988; Titus 1989); (d) marked variations of plasma concentrations in relation to dosage as well as differing concentration–response relationships (Cutler et al. 1988; Munster et al. 2002) and variations in responses in patients with RA (Munster et al. 2002) and SLE (Cutler et al. 1988; Carmichael et al. 2003, 2013; Costedoat-Chalumeau et al. 2003) (Fig. 2); (e) variation in steady-state levels (Fig. 3a) or bioavailability (Fig. 3b) in patients with RA or SLE who have received HCQ (Cutler et al. 1988; Munster et al. 2002; Carmichael et al. 2013); (f) the possibility that pharmacogenomic influences affecting drug metabolism and drug transporters may influence responses to the anti-malarials in rheumatic patients (Davila and Ranganathan 2011); and, (g) differences in the ratios of the R(−)/S(+) enantiomers in blood or plasma C max, as well as plasma or urinary values of T 1/2 (Table 1; Figs. 4, 7) (Ducharme et al. 1995; Brocks and Mehvar 2003). These studies show that the S(+) enantiomers of HCQ are eliminated more rapidly than the R(−) antipode.
The stereochemistry is important for determining the pharmacokinetics of the drug which exists as a racemic mixture of R-(−) and S(+) chloroquine in equal quantities. The pharmacological properties of the individual enantiomers in relation to their anti-rheumatic effects have not yet been fully established
Dose-dependent pharmacokinetics of racemic chloroquine following intravenous administration to healthy volunteers. From Cutler et al. (1988). Reproduced with permission of Springer Basel (AG) owners of Birkhăuser Verlag AG publishers of Agents and Actions
a Steady-state concentrations of racemic hydroxychloroquine in patients with rheumatoid arthritis in relation to dosage. From: Tett et al. (1993); reproduced with permission of Springer Basel AG the publishers of Agents and Actions. b Bioavailability of racemic hydroxychloroquine in normal volunteers (3 left sets of data) and patients with rheumatoid arthritis (right hand group) in relation to conditions of fasting or fed state. Data determined from values of AUC or in the two sets of data in the middle from deconvolution analysis. The fraction of dose absorbed was 30–100 % and this variability could be predicted to be due to high clearance and/pr low bioavailability. From: Tett et al. (1993); reproduced with permission of Springer Basel AG the publishers of Agents and Actions
Variation in blood concentrations of racemic hydroxychloroquine in relation to joint or pain parameters of presence or negative rheumatoid factor. Patients with mild joint symptoms (morning stiffness, pain intensity) or negative rheumatoid factor had higher blood concentrations than those patients with more severe symptoms or positive rheumatoid factor. From: Tett et al. (1993); reproduced with permission of Springer Basel AG the publishers of Agents and Actions
HCQ is administered as the sulphate while CQ is taken as the phosphate salt. Being basic drugs, these salts are principally absorbed in the upper intestinal tract. The lag time before oral absorption of HCQ sulphate 200 mg (taken as Plaquenil® tablets) measured in the blood as the diastereo-isomer ranges from 0 to 0.85 h (mean 0.43 h) (Tett et al. 1989). Despite this variability, the total bioavailability of both HCQ and CQ is 0.7–0.8 and so these values are relatively high (Furst 1996; Tett et al. 1989).
There are marked differences in the PKs of HQ and CQ in humans (Tables 2, 3, 4) (Cutler et al. 1988; Furst 1996; Lim et al. 2009; Munster et al. 2002; Carmichael et al. 2003, 2013; Costedoat-Chalumeau et al. 2003). This is due to variations in the analytical methods used to determine the drug concentrations, whether these were determined in plasma or whole blood, and the differences in the conditions of dosage. Marked variations occur in the PKs with the rate of renal clearance of unchanged HCQ being 21 % of the dose and for CQ 28–47 % of the dose (McChesney 1983; Furst 1996). The terminal elimination half-life of HQ in blood or plasma is highly variable (Titus 1989) (see Tables 2, 3, 4) but in one review is averaged at 50 ± 16 (s.e.m.) days (Furst 1996). Most of the values were at low limits of detection (hence the importance of collecting blood samples to well over the initial decline in values of plasma concentrations, Cp, as noted by Cutler et al. (1988).
The importance of blood concentrations of HCQ for determining responses to therapy of RA is highlighted in Figs. 3, 4 (Tett et al. 1993). It is clear from this graph that morning stiffness, pain intensity and presence of rheumatoid factor can be associated with lower blood levels of HCQ (Tett et al. 1993). The blood concentrations of main metabolite of HCQ, desethyl-hydroxychloroquine (DHCQ), also show a modest association with the efficacy of treatment and gastrointestinal side effects (Munster et al. 2002).
Both HCQ and CQ undergo extensive metabolism to their respective desethyl metabolites (Table 1; Figs. 5, 6) (Churchill et al. 1983; McChesney 1983; White 1985; Brown et al. 1985; Bergqvist et al. 1985; Pussard et al. 1986; Köppel et al. 1987; Iredale et al. 1993; de Oliveira et al. 2007). In laboratory animals, there is a similar pattern of metabolism with ethyl hydroxyl or carboxyl conjugates (e.g. of glucuronic acid) being formed (Aderounmu and Fleckstein 1983; McChesney 1983; McChesney and Fitch 1984).
Metabolic pathways of racemic chloroquine as determined from the urinary excretion over 24 h of the drug and metabolites determined by gas chromatography–mass spectrometry following intake by 5 volunteers of 250 mg chloroquine diphosphate (=150 mg chloroquine base). From: Köppel et al. (1987); reproduced with permission of the publishers of Arzneimittel Forschung (Drug Research) Georg Thieme Verlag KG, Stuttgart, Germany
Metabolic transformation of racemic hydroxychloroquine in humans with data supplemented by studies in laboratory animals. Data from McChesney et al. (1967a, b) and figure which has been redrawn from McChesney (1983). The biotransformation of hydroxychloroquine (HCQ) differs from that of chloroquine (CQ) in that HCQ produces two first-stage metabolites instead of one as observed with CQ. Both the first-stage HCQ metabolites lead in turn to the primary amine, which has a very short half-life (McChesney 1983). The fate of the quinoline nucleus (shown as R- in the figures) is unclear and may include formation of N-oxides
HCQ and CQ also have exceptionally large volumes of distribution (V d) with values around 800 L/kg (Table 2) (Titus 1989; Cutler et al. 1988) reflecting their distribution in aqua-soluble compartments (interstitial fluids, muscle) and binding to pigmented tissues, mononuclear cells, etc. (Varga 1968a, b; Stepien and Wilczok 1982; McChesney 1983; Viala et al. 1983; McChesney and Fitch 1984; Stepien et al. 1987; MacIntyre and Cutler 1986). Most pharmacokinetic parameters fit a three-compartment model (Titus 1989).
The binding to melanin, especially the pigmented cells of the eye, is of particular significance in relation to retinopathy from CQ and HCQ (McChesney 1983; McChesney and Fitch 1984; Rynes 1988; Tehrani et al. 2008; Geamănu-Pancă et al. 2014). There are indications from clinical observations that HCQ may have lower risks of retinopathy than CQ (Finbloom et al. 1985; Salton 1987; Rynes 1988). This is supported by experimental studies in rats in which there appears to be a dose relationship of retinopathy with CQ (Mary and Legros 1987) and HCQ (Furst et al. 1999). Corneal disposition of CQ is greater than HCQ (Easterbrook 1990). There are also indications that the lower V D of HCQ compared with those of CQ (Table 1) might be a factor. However, it should be noted that there are differences in the daily doses employed in rheumatic diseases of CQ (250 mg) compared with HCQ (400 mg) (Rynes 1992), so that the lower retinal toxicity of HCQ compared with CQ may be more apparent in relation to the dose of these drugs.
There are also important physico-chemical features of these drugs governing their uptake into the cytosol from plasma and then their marked accumulation in lysosomes; the latter being a likely candidate organelle for drug action (Fig. 8; Cutler et al. 1988). Such “deep” or tissue/cell specific accumulation of HCQ and CQ is evident in vivo (McChesney 1983; McChesney and Fitch 1984). Marked accumulation of CQ has been found with rat smooth skeletal and cardiac muscle preparations (McChesney and Fitch 1984; Varga 1968a) in which binding to phospholipids has been observed (MacIntyre and Cutler 1986) and this may be a factor in relation to myopathy from these drugs (Abdel-Hamid et al. 2008). Thus, the sites of accumulation of these drugs are likely to be of particular significance in relation to their pharmacological and toxicological effects.
HCQ and CQ exist as diastereoisomers and their pharmacokinetics in humans has been investigated in several studies (Titus 1989; Brocks et al. 1992; Brocks and Mehvar 2003) (Fig. 7). Both the R(−) and S(+) isomers of CQ show equivalent inhibitory effects on smooth muscle contractions in the isolated mouse ileum (Witiak et al. 1981). Anti-malarial activity of the enantiomers against susceptible strains of Plasmodium falciparum is also equivalent in vitro (Fu et al. 1986; Mullié et al. 2012), but the S(+) isomer is more potent against Plasmodium berghei infection in mice (Haberkorn et al. 1979). Embryotoxicity of CQ enantiomers has been investigated in rat whole embryos in culture and the racemic CQ found more toxic than the individual enantiomers, both of which show equivalent toxicity (Tagoe and Ofori-Adjei 1995). Aside from these studies, there does not appear to have been any other investigations on the biological activities of the CQ and HCQ isomers. Clearly, this is an important area for future investigations.
From Ducharme et al. (1995); reproduced with permission of Wiley-Blackwell the publishers of the British Journal of Clinical Pharmacology
Excretion in breast milk and transplacental passage
The issue of the potential for toxicity by CQ and HCQ for the child as well as mother has been of particular concern for patients with SLE and RA (Parke 1993; Borden and Parke 2001; Costedoat-Chalumeau et al. 2003). This could be due to transplacental movement of drug during pregnancy or exposure of the child to the drug from breast milk (Sammaritano and Bermas 2014).
In a number of studies, CQ or its metabolites (Edstein et al. 1986; Ogunbona et al. 1987; Ette et al. 1987a, b, c; Akintonwa et al. 1988) as well as HCQ have been shown to be excreted in breast milk (Nation et al. 1984; Østensen et al. 1985). Transplacental transmission of CQ and HCQ has also been observed (Akintonwa et al. 1988; Costedoat-Chalumeau et al. 2002). It is of interest that the transmission of these anti-malarials in the milk and placenta has been demonstrated in patients with HIV and other viral infections (Chiang et al. 1996; Boelaert et al. 2001a, b; Semrau et al. 2006) and so this may confer protection against these infections upon the foetus or newborn. CQ may afford some neuroprotective effects against brain inflammation as highlighted from studies on the actions of this drug against the HIV-1 viral coat protein in mice (Ashraf et al. 2014).
The amount of HCQ that is secreted in breast milk is limited to the extent that concentrations in cord blood are similar to those in blood (Costedoat-Chalumeau et al. 2002). An issue has been raised about the possible pigmented changes in foetal tissues due to deposits of HCQ and/or its metabolites (Borden and Parke 2001). It is considered that HCQ may be safe for nursing mothers with RA, especially compared with alternatives such as methotrexate or leflunomide (Sammaritano and Bermas 2014). The relative amounts of HCQ that appear in neonatal blood are in the micromolar range (Van Roon et al. 2009). This may not be of toxicological significance, although data in laboratory animals on the feto-toxic actions of HCQ and CQ are lacking.
Drug metabolism and drug interactions
Cytochromes P450
The metabolism of CQ and HCQ to desethyl and other metabolites has been extensively studied in rats and humans (McChesney et al. 1965, 1966, 1967a, b; McChesney 1983; McChesney and Fitch 1984; Furst 1996). CQ and HCQ are rapidly dealkylated by cytochrome P450 enzymes (CYP) to pharmacological active desethyl (DE-CQ) and bis-desethyl CQ (BDE-CQ) in the case of CQ, and the monohydroxyl HCQ (M-HCQ) and desethyl HCQ (D-HCQ) in case of HCQ (McChesney 1983; McChesney and Fitch 1984; Furst 1996; Spaldin et al. 1994; Ducharme and Farinotti 1996; Projean et al. 2003; Kim et al. 2003; Li et al. 2003; Gil and Gil Berglund 2007). The identity of the specific CYP isoforms responsible for these de-alkylation reactions has been explored using rat or human microsomal preparations and human recombinant enzymes (Spaldin et al. 1994; Projean et al. 2003; Kim et al. 2003). A consensus suggests that CYP2C8, CYP 3A4 and CYP 2D6 are the main isoforms responsible for the metabolism of CQ, although CYP1A1 may also be involved (Spaldin et al. 1994; Projean et al. 2003; Kim et al. 2003; Li et al. 2003; Gil and Gil Berglund 2007). The relative contributions of these isoforms to the metabolism of CQ vary according to the kinetic properties, species and enzyme preparation. Thus, Projean et al. (2003) found that human recombinant CYP1A1, CYP2C8, CYP2D9 and CYP3A4 produced DCQ ?DE-CQ, but production of this metabolite was affected by the inhibitors, testosterone (CYP3A4 inhibitor) and paclitaxel (CYP2C8); there was a high correlation with DCQ ?DE-CQ formation in humans. In contrast, human microsomal metabolism of CQ, the metabolism of tacrine was inhibited implying that CYP1A2 was involved. These results suggest that metabolism of CQ may not occur to an appreciable extent via CYP1A2, but this could be a site of inhibition by CQ of those other drugs that are metabolised by this CYP isoform. Studies using the above-mentioned enzyme preparations with modelling of the rates of hepatic or intrinsic clearance indicate that CYP-2C8, CYP-2D6 and CYP-3A4 are the predominant isoforms involved in clearance of CQ (Li et al. 2003).
Drug interactions
Pharmacokinetic drug interactions are important in relation to the safety and efficacy of anti-malarials (Furst 1996; Munster et al. 2002; Carmichael et al. 2003). Some of the drug interactions may be related to the competitive effects of drugs on the activities of the isoforms of the cytochromes P450. The N-de-ethylation of CQ leading to the formation of mono-desethyl form represents one site of action of the CYPs where there may be drug interactions.
Among the potentially important significant drug–drug interactions involving HCQ and CQ, with antibiotics, aspirin, paracetamol, cholestyramine, proton-pump inhibitors or H2 receptor antagonists, imipramine, methotrexate, cyclosporine, caffeine, debrisoquine, metoprolol, and other anti-parasitic agents have received particular attention because of the potential for microsomal P450 interactions or impact on hepato-renal clearance (Gupta et al. 1979; Ali 1985; Ette et al. 1987a, b; McElnay et al. 1985; Gendrel et al. 1990; Kull and Besterman 1990; Onyeji et al. 1993; Raina et al. 1993; Bannwarth et al. 1996; Adedoyin et al. 1998; van den Borne et al. 1998; Oforah and Anyogo 2000; Somer et al. 2000; Vezmar and Georges 2000; Carmichael et al. 2002; Alisky et al. 2006; Cook et al. 2006; Ilo et al., 2006, 2008; Obua et al. 2006; Skinner-Adams et al. 2007; Namazi 2009; Van Roon et al. 2009).
The frequently used analgesics, aspirin and paracetamol, would be expected to be of particular concern for the safety of HCQ and CQ. This is especially so when there is pronounced cytokine production in fever and other inflammatory reactions that would be expected to be treated symptomatically with these drugs and which may affect production of cytochromes.
A study in healthy volunteers by Adjepon-Yamoah et al. (1986) showed that CQ increased the peak paracetamol concentration, C max and T max as well as its AUC, but had no effect on paracetamol metabolism. These observations were confirmed in volunteer studies subsequently by Raina et al. (1993). These data suggest that CQ may affect the clearance of paracetamol. However, impairment of urinary and biliary excretion of paracetamol metabolites by CQ has been observed (Oforah and Anyogo 2000), so this may also be an additional site of action of the drug.
Aspirin, in contrast to paracetamol, has not been found to alter the PK of CQ (Raina et al. 1993). However, HCQ has been found to inhibit the activity of serum aspirin esterase in vitro (Gupta et al. 1979) and this inhibitory effect of HCQ might result in increased circulating levels of aspirin compared with its metabolite, salicylate.
Of the antibiotic–anti-malarial drug interactions, the bioavailability of ampicillin has been observed to be reduced by CQ (Ali 1985), while that of ciprofloxacin is less markedly affected by CQ (Ilo et al. 2006, 2008). In contrast, no effects have been observed of CQ on the PK of azithromycin or vice versa (Adedoyin et al. 1998).
Anti-acid secretory agents might be expected to affect the oral absorption of HCQ and CQ as a result of decreased gastric acidity affecting the ionisation of these basic drugs (Perrin 1965). Studies in healthy male volunteers by Ette et al. (1987a) showed that the oral clearance of CQ was reduced by about one-half when co-administered with H2-receptor antagonist cimetidine. These authors also observed that cimetidine reduced the AUC of mono-desethyl CQ, the major metabolite of CQ, while the V D of CQ was increased by nearly twofold. These results suggest that there may be effects of cimetidine on both the gastric absorption and CYP-mediated metabolism of CQ. In contrast, ranitidine does not affect the PK of CQ (Ette et al. 1987b). It is possible that the lack of effects of ranitidine on CYP-mediated metabolism of CQ underlies this negative interaction. Moreover, it has been postulated that proton-pump inhibitors (PPIs; omeprazole, pantoprazole) may affect the immunopharmacological activities of HCQ and CQ (Namazi 2009) raising the possibility that oral bioavailability of these anti-malarials may be affected by the changes in intragastric pH by these potent anti-secretory agents. Alternatively, PPIs may affect accumulation of these anti-malarials in phagolysosomes (Namazi 2009).
Imipramine does not affect the PK of CQ or vice versa (Onyeji et al. 1993). However, the interaction of debrisoquine and CQ as a result of the common actions of these drugs on CYP2D6 (Adedoyin et al. 1998) suggests that there are potential interactions between these two drugs which may result in alterations in their biodisposition and metabolism. HCQ interacts with metoprolol as a consequence of the effects of both of these on CYP2D6 (Somer et al. 2000). This leads to increased maximal plasma concentrations (C max) and thus the bioavailability of metoprolol. No such effects have been observed with dextromethorphan, which is also metabolised via CYP2D6 (Somer et al. 2000).
A study in dogs by McElnay et al. (1985) showed that digoxin serum concentrations were increased by up to two-thirds by CQ. The authors suggested that the mechanism of this drug interaction may be related to that observed with digoxin and quinidine, possibly as a result of increasing concentrations of a CQ metabolite. The effect of HCQ in causing increased levels of digoxin has been noted (RxFiles Detailing Program 2008) and this is clearly an important drug interaction that may result in increased cardiotoxicity of digoxin when used in combination with these anti-malarials (RxFiles Detailing Program 2008). Of related significance is the generalised observation that drugs which increase the QT interval (like quinidine) may increase the risk of cardiac arrhythmia (Van Roon et al. 2009.
Probably, the most significant drug interactions of relevance is the wide spread use of anti-malarials with methotrexate (MTX) (Furst 1993, 1996). A number of PK studies have been performed with these drug combinations (Carmichael et al. 2002, 2003; Bannwarth et al. 1996). Gastric absorption of MTX is reduced by CQ (Bannwarth et al. 1996). Co-administration of HCQ with MTX causes reduced C max and increased T max when co-administered with HCQ (Raina et al. 1993). It has been suggested that this effect of HCQ on the PK of MTX may explain the diminution of acute liver effects due to MTX (Carmichael et al. 2002, 2003). There does not appear to be any significant drug interactions related to effects on the PK of HCQ by MTX (Carmichael et al. 2002, 2003).
Although a less-frequently used drug combination, cyclosporin and anti-malarials may occasionally be employed in severe RA. Use of low doses of both cyclosporin and CQ may improve symptoms of RA but there is a risk of reduced renal function due to cyclosporin which may affect the PK and toxicity of CQ (van den Borne et al. 1998).
Several studies have shown that smoking interferes with the efficacy of anti-malarial therapy in patients with cutaneous lupus (Sams 1967; Homewood et al. 1972; Raghoebar et al. 1986; Fox 1993; Davis and Woolf 1996; Khraishi and Singh 1996). There is a possibility that this is due to effects on the metabolism of the drugs via the cytochrome P-450s. Smoking has been found to affect the clearance and elimination half-life of quinine (Ginsburg and Geary 1987), but the CYP1A catalysed production and urinary excretion of the hydroxylated metabolite, 3-hydroxyquinine, is unchanged in smokers compared with normal subjects (Whitehead and Hager 1954). However, these effects of smoking on the clearance and other PK properties of quinine have not been confirmed in patients with Faciparum malaria (Van Cauwenberge et al. 1958a, b). Moreover, the production of the CYP2C9 isoform is unaffected by smokers or the PK of an experimental naphthoquinone anti-malarial that is metabolised by this isoform (Leoni 1955). Although it seems unlikely that smoking influences the PK of some anti-malarials, this situation has not been resolved with HCQ and CQ.
Cellular disposition: relation to pharmacodynamics
Of particular interest in relation to the anti-inflammatory actions of HCQ and CQ that are leucocyte-mediated is the pronounced accumulation of CQ in polymorphonuclear leucocytes (PMNs) and to a lesser extent mononuclear cells (and red blood cells) (Leoni 1955). The accumulation in PMNs has been suggested to be due to the presence of acidic lysosomal organelles which act as a trap for the weak base, CQ (Leoni 1955). Accumulation of radiolabelled CQ in PMNs was found to vary with extracellular pH: an increase in physiological pH from pH 6.5 to pH 7.4 causing an almost doubling of intracellular concentrations of CQ (Leoni 1955). Also, the acidic drugs, aspirin and salicylic acid markedly reduced the accumulation of radiolabelled CQ (Leoni 1955) suggesting that these acidic drugs could antagonize the leucocyte-mediated actions of CQ by ion pairing.
Pharmacodynamics
Background
Earlier studies have been considered by Cutler (1993) to indicate that “The actions of CQ in the treatment of malaria have in the past been considered as a possible indicator of anti-rheumatic effects” (Cutler 1993). Yet this author did not specify precisely in what way these actions of CQ were to be an indicator for its anti-rheumatic activity. Cutler (1993) pointed out that an early theory of Homewood et al. (1972) of the action of CQ was that it disrupts functioning of the food vacuole in the malarial organisms by altering pH in this organelle (Homewood et al. 1972). However, this action in an amoebic organism is a long way removed from actions on inflammatory synovia or leucocytes in patients with SLE or RA. It was the serendipitous observations by Page (1951) and shortly afterwards in the 1950s, 1960s and subsequently by others (Newbold 1963; Suzuki et al. 1973; Volastro et al. 1973; Clarke et al. 1975; Teitz and Chrisman 1975; Rainsford 1992; Wallace 1996; Nayak and Esdaile 1996) that set the basis for showing that CQ and HCQ have anti-rheumatic activity, but there was little understanding about the pharmacological mechanisms for this activity.
In this review, we have focussed attention on the mechanisms of action of HCQ and CQ on their anti-inflammatory actions. While some useful information can be gleaned from the studies on the anti-malarial actions of these drugs, we have focussed on the evidence from the cellular and molecular studies relative to their anti-rheumatic activity.
Concepts of modes of action
Rynes (1992) reviewed the mechanisms of the anti-rheumatic effects of anti-malarials based on information available up to 1992. He noted the difficulty of determining drug actions because of the multiplicity of their activities (listed in Table 5 with addition of more recent information). However, Rynes (1992) made two important points about the anti-rheumatic actions of anti-malarials, namely that (a) the anti-rheumatic actions in the treatment of RA develop gradually over time and may not be maximal for 6 months or longer, and (b) after discontinuation of the medication the arthritis may remain well controlled for a number of months thereafter. Rynes (1992) suggested on the basis of these observations that the anti-rheumatic effect of anti-malarials is indirect. He stated that “it is attractive to speculate that primary drug actions indirectly influence various pathogenic disease processes”. He considered that the 2 primary candidates for drug action are the inhibition of enzyme activity (phospholipase A2, lysosomal enzyme release and activity) which precede actions on the immune system (of which there is now extensive data; see later section on sections in the immune and inflammatory cells). Similar views about the effects of anti-malarials on enzymes and the acid vesicle system were expressed by Cutler et al. (1988), Cutler (1993) and in the context of malaria by Ginsburg and Geary (1987). Cutler and colleagues (Cutler et al. 1988; Cutler 1993) considered that there were important pharmacokinetic factors accounting for the prolonged period required for therapeutic actions of anti-malarials to be apparent. In this respect, the long plasma elimination half-lives of HCQ and CQ as well as their dealkylated metabolites (which also probably have pharmacological activity) which amount to up to 50 days allow for appreciable systemic accumulation of these drugs and their pharmacologically active metabolites. Combined with their extensive volumes of distribution and propensity to accumulate in aqua-soluble body compartments raises the issue of whether the accumulation of these drugs/metabolites in some “deep” body compartments (e.g. bone marrow, lymphoid systems) might, inevitably, take some time such that the effects of these agents on the immuno-inflammatory processes in severe arthritic conditions may take considerable time to be affected. This may mean that the postulated slow “deep” body pharmacokinetics with accumulation of the drugs/metabolites in key immunological compartments might account for the slow onset of drug activity in patients with RA and SLE. Furthermore, the slow actions of these drugs may be attributed to the relatively long time dependence of their actions on cells of the immune system and inflamed joints that underlie the arthritic disease.
The importance of the range of effective drug concentrations in vitro in which many of the cellular or molecular processes that can be considered as being pharmacologically effective (in contrast to toxicological effects at high concentrations) is particularly difficult to determine. This is partly because there is little information available on the expected range of drug concentrations in “deep” organs (e.g. lymphoid, immune cells, bone marrow, synovial and other connective tissues) from which to enable pharmacologically related drug concentrations to be established with certainty. The range of plasma/serum/blood concentrations (ca. 0.5–5 μM) as a guide may be wide of the mark when viewed as a guide for potential pharmacological ranges since these may not relate to the concentrations in “deep” compartments. An indication of the possible therapeutic concentration range may be provided by the plasma water concentrations as suggested by Cutler (1993) in which HCQ and CQ have “typical” therapeutic concentrations of 0.5 μM in acidic compartments such as lysosomal or acidic vacuoles (or even synovial fluids) may range as high as 80 mM given the average cell concentration of 1 mM, and in the case of the lysosomal compartment being 1 % of the cell volume (see Fig. 8) (Cutler 1993). As Cutler (1993) pointed out these calculations may be extended to estimate that the final concentration may be in the range of 0.05 μM in the extracellular fluid. Given the possibility of progressive accumulation of the drug/metabolites with time and the kinetics of disease progression (dX/dt = R-k x ; X being the extent of “damage” or inflammatory injury in progression with time, t; R = new damage; k x = rate of repair, k which is in proportion to x, i.e. k x ) (Cutler, 1993) the disease state and the drug metabolites may need to be integrally calculated in an combined pharmacokinetic-pharmacodynamic model in order to understand the dynamics of drug-related actions of HCQ, CQ and for that matter other slow-acting DMARDS.
Postulated pattern of the cellular uptake of hydroxychloroquine (HCQ) or chloroquine (CQ). From: Cutler (1993); reproduced with permission of Springer Basel AG the publishers of Agents and Actions
It is most likely that for slow-acting effects that characterise DMARDs such as HCQ and CQ, their primary site of action will be on the components of the lymphocytes and macrophages that mediate chronic inflammation (Ben-Zvi et al. 2012). These actions of HCQ and CQ are summarised in Table 5. Here, they are reviewed in depth after consideration of some of the associated general anti-inflammatory actions of these drugs.
Anti-inflammatory effects in laboratory animals
During the mid-late 1950s, a number of studies had shown that CQ had in vivo activity in standard models of acute oedema. Thus, Whitehead and Hager 1954 showed that CQ reduced the foot pad oedema induced in rats by the injection of albumin (Whitehead and Hager 1954). Van Cauwenberge and co-workers confirmed these observations and showed that CQ also reduced the dextran-induced paw oedema as well as the cotton-pellet granuloma in rats Van Cauwenberge et al. 1958a, b). Leoni (1955) showed that CQ reduced the erythema in humans induced by phenol. There were indications from these early studies as well as from studies of the protective effects of CQ on the effects on skin following exposure to ultra-violet (UV) radiation (i.e. sunscreen protective effects) that CQ might produce anti-inflammatory effects through its anti-histaminic activity (Sams 1967).
Newbold (1963) observed that CQ and HCQ, in contrast to some NSAIDs, were inactive in the mycobacterial adjuvant-induced arthritis in rats. This has been subsequently confirmed by Rainsford (1992) in studies in which the radiological evidence of joint damage was also measured in addition to joint swelling and clinical observations of disease activity.
Clarke et al. (1975) employed the development in rats of a granulomatous reaction elicited by subcutaneous implantation of polyurethane cubes impregnated with dead heat-killed Mycobacterium tuberculosis to determine the anti-inflammatory effects of a range of DMARDs, cytostats and NSAIDs by measuring the dry weight and cellular infiltrates into the cubes following 5 days treatment with these drugs. They observed that although aspirin, phenylbutazone, cyclophosphamide and prednisolone reduced the weights of the cubes in a dose-related manner that HCQ, sodium aurothiomalate and d-penicillamine were without effects on this “liquid phase” of inflammation. In contrast, the cellular infiltrate into the cubes was reduced by HCQ and the other drugs. This suggested that NSAIDs, corticosteroids but not DMARDs can exert anti-oedematous effects, whereas HCQ like the NSAIDs affects cell migration.
Several authors have investigated the effects of CQ or HCQ in models of monoarticular arthritis induced in rabbits or mice by intra-articular injection of antigen or prostaglandin (Volastro et al. 1973; Suzuki et al. 1973; Clarke et al. 1975; Teitz and Chrisman 1975; Colombo et al. 1983; Hunneyball et al. 1986; Crossley et al. 1987). In most of these studies, HCQ or CQ showed protective effects while some studies showed that NSAIDs were without any effects. However, these effects could be variable since in the antigen-induced monoarthritis in BALB/c mice, Hunneyball and co-workers (Hunneyball et al. 1986; Crossley et al. 1987) showed that CQ and several other DMARDs as well as NSAIDs failed to affect destruction of bone and articular cartilage as well as histological grades of pannus formation and cellular infiltration, whereas prednisolone, azathioprine and sulphasalazine were effective in suppressing the symptoms and, in some cases, the histological changes. This model of arthritic disease is particularly slow in manifesting joint changes and treatment with the drug takes a long time to produce therapeutic or significant effects.
Blackham et al. (1975) also observed that the reverse-passive Arthus reaction elicited in guinea pigs by intravenous ovalbumin followed by intra-articular injection of anti-ovalbumin or anti-IgG specific antibody was inhibited by CQ and several NSAIDs and DMARDs. This model demonstrated that these drugs could reduce the infiltration of polymorphonuclear leucocyte- and complement-mediated cellular reactions underlying the joint inflammation.
The main conclusions from these in vivo studies are that CQ and HCQ probably have inhibitory effects on cellular infiltration and activation underlying joint inflammation, but their effects on the other manifestations of joint injury are relatively limited.
Lysosomotropic activity
The effects of CQ and HCQ to accumulate in lysosomes and affect the activities of these intracellular organelles have been suggested as underlying their actions on leucocytes and joint inflammation (Rynes 1992; Cutler 1993). Their actions of accumulation in lysosomes, or lysosomotropic activity, are due to the basic properties of these drugs (MacIntyre and Cutler 1988).
Following the pioneering work by De Duve and co-workers in the mid-late 1950s (Novikoff et al. 1956; De Duve et al. 1962; De Duve 1965) on enzymes that cause autodigestion in lysosomes, there was much interest in the possibility that agents such as vitamin A, endotoxin, streptolysins and lysolecithin or the exposure to UV radiation might enhance the release of these tissue-destructive enzymes from these organelles (Weissmann 1984). It was found that protection against the release of these lysosomal enzymes (typically β-glucuronidase, acid phosphatase) could be obtained with drugs such as corticosteroids and CQ (Weissmann 1984; Ignarro 1971, 1974; Malbica and Hart 1971; Ignarro and Colombo 1972). In isolated rat liver, lysosomal preparations CQ 100–250 μM was found to effectively inhibit release of these inflammogen-induced enzymes (Weissmann 1984). The lysosomotropic effects of CQ in accumulating in lysosomes in isolated rats hepatocytes were evident at therapeutic drug concentrations (120–360 μM) and were found to be in the same order of magnitude as found in vivo in rats (Weissmann 1984). The accumulation of CQ was inhibited by ammonium ions and metabolic inhibitors. It was suggested that since the lysosomal compartment is a relatively acidic environment, that the accumulation of CQ, like other weak bases, is due to an ion-pair trapping mechanism (Weissmann 1984).
These effects of CQ have been investigated for their relevance on the lysosomal enzyme release from the key leucocyte populations (i.e. macrophages and PMNs) that mediate inflammatory reactions (Lowe and Turner 1973; Northover 1977; Smith 1977; Riches et al. 1981; Riches and Stanworth 1982; Wildfeuer 1983; Glaumann et al. 1985; Jones and Jayson 1984; Jones et al. 1984). While CQ did not appear to affect release of enzymes from non-phagocytozing cells (Northover 1977), the stimulation of phagocytosis by serum treated zymosan was found to be inhibited by CQ (Smith 1977; Wildfeuer 1983).
Riches et al. (1981) and Riches and Stanworth (1982) observed that mouse peritoneal macrophages incubated with CQ and quinine showed time-dependent and concentration-dependent inhibition of the release from lysosomes of N-acetyl-β-d-glucosaminidase and β-galactosidase from macrophages; the effective concentration range being 50–300 μM for CQ. These authors suggested that these drug effects are due to their lysosomotropic activity.
The inhibitory effects of CQ 25–500 μM on activation of lysosomal β-galactosidase release from macrophages were found to be independent of the effects on increasing complement activation and appeared to resemble that of various weak bases, e.g. methylamine (Riches et al. 1981).
A further feature of CQ and HCQ is their ability to accumulate in secondary lysosomes, or autophagic vacuoles (AVs) (Glaumann et al. 1985). The effects of CQ (1.56–156 μM) on phagocytic activity and electron microscopic appearance of normal PMNs in vitro were investigated by Jones and Jayson (1984). These authors found that CQ caused a time- and concentration-dependent inhibitory effect on uptake by PMNs of latex particles. After prolonged incubation with CQ (4 h), there was a marked increase in the neutrophil granulation and a concentrated increase in the number of autophagosomes in lymphocytes at concentrations (0.15–15 μM) with fine structural evidence of arylsulphatase in these cells which occurred within the plasma therapeutic concentrations. In a companion paper, Jones et al. (1984) observed that the presence of abnormal lysosomes in lymphocytes and PMNs was observed ultrastructurally in patients with SLE and RA that received CQ and HCQ compared with patients that received corticosteroids or NSAIDs or normal subjects. There was a relatively high variability in appearance of the multi-lamellar inclusion bodies and granules indicating the presence of abnormal lysosomes which varied in individual patients. This might be related to the varying periods of time that the patients received the drugs as well as underlying disease activity. The results suggested, however, that there is evidence for lymphocytes having greater susceptibility to the effects of CQ compared with PMNs. The authors suggested that their ultrastructural evidence of electron dense particles in the leucocytes of RA and SLE patients that received CQ as well as in their earlier study in vitro (Jones and Jayson 1984) reflects the impairment by CQ of the digestion by lysosomal enzymes. Based on their results and published literature, it was postulated by the authors that CQ initially labilizes the lysosomal membrane causing release of digestive enzymes and initiating autophagy. With multiple treatments, there is lysosomal membrane stabilisation and inhibition of lysosomal enzyme activity and release. They suggested that these effects of CQ on lymphocytes may cause impairment of the normal functions of lymphocytes, thus accounting for the apparent immunosuppression by this drug. The inhibitory effects of CQ on phagocytosis and granule release were suggested by the authors as underlying the anti-inflammatory effects of CQ. These observations represent an important basis for the understanding of the actions of anti-malarials on immune activity and inflammatory reactions.
Actions on the immune system and cytokines
Treatment of RA patients with HCQ (200–400 mg/day) for relatively long periods of time (months/years) has been found to reduce those biomarkers that are regulated by the cytokines IL-1 and IL-6, namely ESR and plasma levels of acute phase reactants and haptoglobin, coincident with improvement of physical signs and disease symptoms (Klinefelter and Achurra 1973; Dixon et al. 1981; Pavelka et al. 1989). Furthermore, plasma IgG concentrations were increased while the IgM decreased after 1 year’s treatment with HCQ 200 or 400 mg/day (Kalmanson and Guze 1963). These changes in pathognomonic of disease activity reflect potential for changes in cytokine activity that underlies control of immune cell functions.
Early studies indicated that HCQ and CQ administered orally to rabbits did not reduce the primary and secondary responses in antibody production (Kalmanson and Guze 1963; Thompson and Bartholomew 1964) but HCQ did increase the reactions to BCG and prolonged the skin reaction (Kalmanson and Guze 1963). These results contrast with studies using popliteal lymph node cells isolated from rats immunised against horseradish peroxidase (HRP) and then incubated with CQ 0.88 mM in which anti-HRP antibodies were reduced; a similar effect being noted with lysosomotropic amines (Antoine et al. 1985). It was suggested that these effects were due to their lysosomotropic action. CQ has been found to inhibit antibody-mediated enhancement of yellow fever virus growth as well as viral replication (Brandriss and Schlesinger 1984), indicating that in viral infections the antibody production may be enhanced by CQ. In contrast, the immune reactions accompanying malaria infection may be more related to inhibitory effects on growth of plasmodia in infected cells as a result of vesicular increase in concentrating CQ rather than influences on antibody production (Fox 1993). There are, however, indications that in malaria, CQ and other anti-malarials alter the processing of auto-antigenic proteins via intracytoplasmic vesicles and their assembly into complexes with MHC class II proteins (Fox 1993). According to Fox (1993), this leads to decreased stimulation of CD4+-T cells reactive with self peptides/proteins, decreased release of cytokines and subsequent diminution of the autoimmune process.
Early indications of supposed immunosuppressive effects of CQ were provided from studies by Panayi et al. (1973) in lymphocytes isolated from 14 patients with RA who had received 250 mg CQ daily for 1–10 years together with high doses of soluble aspirin (3.23–5.2 g/day). The incorporation of tritiated-thymidine after PHA stimulation and mitotic index was reduced with these treatments by about one-half compared with those cells from 12 RA patients or 11 with degenerative joint disease osteoarthritis that had received aspirin alone (Panayi et al. 1973). In an accompanying study which may have involved the similar patients who received the same drug treatments, various types of chromosomal damage (stable chromosome breaks and fragments or dicentrics) were observed in the PHA-stimulated B cells of patients with RA that had received either CQ with aspirin but not those which had aspirin alone or in patients that had degenerative joint diseases that received aspirin (Neill et al. 1973). The appearance of unstable chromosomal abnormalities in B cells was not regarded as being of cytologic significance since these cells would inevitably die at subsequent mitosis, and would not require discontinuation of the drug, except in pregnant patients. The significance of these changes in relation to immunological activity of B cells might be related to impairment by CQ of their immunological activity rather than replication of these cells (Neill et al. 1973; Panayi et al. 1973).
Cellular immune reactions
The in vitro inhibitory effects of 0.01 mg/mL CQ were observed on phytohaemagglutinin (PHA) stimulated lymphocytes; these effects were shown to be time-dependent (Hurvitz and Hurschhorn 1965). CQ >10 μM inhibited the proliferation of PHA-stimulated T cells and was less potent than azathioprine (Klinefelter and Achurra 1973). The IC50 for CQ inhibition of T-cell proliferation was found to be 19.50 ± 2.24, which was comparable to tamoxifen but less potent than steroids (Kamal and Jusko 2004). CQ in combination with the immunosuppressants, dehydro-epiandrosterone and 2-chloro-2′-deoxyadenosine, showed additivity in suppressing PHA stimulation, in contrast to combinations of some other immunosuppressants which showed synergistic inhibition (Klinefelter and Achurra 1973). Other studies confirmed the effects of CQ 3 μM on PHA-stimulated tritiated thymidine or deoxyuridine incorporation using salicylate 1 mM (a known inhibitor of lymphocyte proliferation) as a reference standard (Pavelka et al. 1989). In view of the latter observation, the earlier comparison by Panayi and co-workers of the effects of treatment with CQ with aspirin and aspirin alone may require revision on the basis of interpreting the potential effects of salicylate from ingested aspirin alone in diminishing lymphocyte proliferation in patients with RA (Neill et al. 1973; Panayi et al. 1973).
The combined results of these two studies would suggest that long-term treatment with CQ has additional inhibitory effects on PHA-induced lymphocyte proliferation compared with that of high dose aspirin alone.
CQ 0.25–0.75ug/ml like that of some other anti-malarials has been found to inhibit Plasmodium falciparum merozoite-stimulated lymphocyte proliferation in concentration-related manner similar to that observed with PHA (Williams and Davidson 1983; Bygbjerg et al. 1986) suggesting that similar intracellular events might be affected by CQ in response to these stimuli.
In chemoprophylaxis of malaria in Javanese men who received 300 mg CQ base once weekly, mitogen- or antigen-stimulated lymphocyte proliferation was increased by treatment with this and other anti-malarials over a 12-month period in relation to a stimulation index for responder status, but varied according to the nature of the antigen or mitogen (Fryauff et al. 1996). While the T and B cell responses during chemoprophylaxis with anti-malarials in malaria would be expected to be different than those in autoimmune diseases, these studies highlighted variability in lymphocyte proliferation in relation to stimuli which may be of therapeutic significance for treatment of patients with autoimmune diseases—very important point.
In vitro studies have shown the role of complement in enhancing the inhibitory effects of CQ (Fosdyke 1975). CQ is thought to inhibit T cell proliferation and generation of immunoglobulin cells by affecting the accessory functions of monocytes and interleukin-1 secretion (Salmeron and Lipsky 1983).
Of the other lymphocyte subsets affected by anti-malarials, that involving natural-killer (NK) cell activity has attracted much interest. This action has been related to the lysosomotropic effects of CQ, in a manner to other such lysosomally active agents (Fosdyke 1975; Salmeron and Lipsky 1983; Acha-Orbea et al. 1983; Thiele and Lipsky 1985a, b; Lipsky 1986).
The potential for CQ to inhibit NK activity in RA patients that received this drug was investigated by Barbieri et al. (1985) as well as by Ausiello et al. (1986). They found that both spontaneous- and interferon-induced cytotoxicity were reduced by treatment with CQ (500 mg/day for the first 4 weeks, then 250 mg/day for the following 7 months) compared with patients who had not received this drug or healthy control subjects matches for age and sex.
The focus on mechanisms of action of CQ on monocyte activities initially involved the lysosomotropic effects in response to exposure of human cells to antigens (e.g. soluble antigen streptolysin O; polyclonal stimulant Staphylococcus areus protein A) in which CQ like ammonium chloride prevented antigen presentation (Scala and Oppenheim 1983). Cell membrane allo-antigen presentation was unaffected by these agents. It was inferred from these studies that the reversible inhibitors, like CQ, of phagosome–lysosome functions, inhibit intracellular processing of the stimulants, during which interleukin-1 (IL-1) has co-stimulatory effects.
Polyclonal B cell activation in mouse spleen cells has been shown to be inhibited by CQ with an EC50 of 0.1 µM, as well as gold complexes and prostaglandin E1 (PGE1) (Ohsugi and Gershwin 1984).
The involvement of cytokines in the PHA-induced lymphocyte proliferation as targets of action of immunosuppressive agents and NSAIDs was shown by Gordon and Lewis (1984) in which they found that amongst these agents, CQ and mepacrine were potent inhibitors of mononuclear cell factor (MCP), which in turn stimulates the release of IL-2 and PGE2 production.
Mitogenic responses to concanavalin A (ConA) of spleen cells from normal rats were found by Pasternak and co-workers to be enhanced by CQ 10–1.0 µM (Pasternak et al. 1985). In contrast, the blastogenesis of cells from arthritic rats was suppressed by CQ as well as tilorone, levamisole and gold sodium thiomalate enhanced blastogenesis in these cells (Pasternak et al. 1985). The authors suggested that on the basis of these results it may be possible to classify anti-rheumatic agents as stimulators or suppressors of immune functions. Certainly, the well-known immunostimulant actions of levamisole could be explained by these results, whereas CQ is clearly immunosuppressive.
IL-2 production by human lymphocytes has been found to be suppressed by CQ and other anti-malarials at concentrations which are about twice as high as those that are required for the suppression of lymphocyte proliferation (Bygbjerg et al. 1987). Addition of IL-2 partially reversed this suppressive effect suggesting that intracellular processing events may be targeted by these drugs. Similar conclusions can be drawn from the observations about the actions of CQ in the mixed lymphocyte reactions involving collaborations between dentritic cells and monocytes in which it was found by Räsänen et al. (1989) that CQ affected the processing of Bacillus Calmette Guerim (BCG).
Pokeweed-mitogen (PWM) induced immunoglobulin (Ig) production in normal human peripheral blood mononuclear cells (PBMC) was inhibited by 0.25–6.25 μM CQ (van Loenen et al. (1990). Thorens and Vassalli (1986) showed that CQ 100 μM, like NH4Cl, blocked the terminal glycosylation of Ig involving addition of sialic acid in the distal Golgi apparatus. T cell proliferation of human mononuclear cells induced by anti-CD3 was found to be inhibited by CQ in a concentration-dependent manner (Vayuvegula et al. 1990). This effect was shown to be due to inhibition by CQ of DNA synthesis and resulted in inhibition of CD25 expression but not that of HLA-DR expression on monocytes. Antigen presentation of human foetal cartilage proteoglycan (PrGn) by synoviocytes and spleen cells has been found to be inhibited by CQ (Brennan et al. (1995) indicating that this drug may prevent the immunological reactions in joints caused by degraded cartilage components.
HLA antigens are selectively eluted by CQ from human platelets without affecting plasma membrane integrity (Kao 1988). Using scanning electron microscopic (SEM) techniques, the binding and uptake of Ig-coated gold particles to specific receptors on macrophages and subsequent endocytosis and transfer to lysosomes have been found to be selectively affected by CQ 50uM, with the latter intracellular processes being inhibited in a time-dependent manner (Hedin and Thyberg 1985).
Cytokine production and actions
In adjuvant arthritic rats, oral administration of CQ 20–35 mg/kg/day on days 3–17 post-adjuvant reduced non-injected paw swelling, like that of the DMARDs, gold sodium thiomalate, auranofin and d-penicillamine, but caused a marked loss in body weight (Connolly et al. (1988). As noted earlier, it has been found that CQ did not reduce ankle swelling in adjuvant arthritic rats and this has not been accompanied by reduction in radiologically observed joint damage (Rainsford 1992). Splenic cell stimulation in arthritic rats was slightly reduced by CQ 30 mg/kg/day but was more markedly inhibited by other DMARDs (Connolly et al. 1988). In these studies, plasma C-reactive protein (CRP) and iron levels were unaffected by CQ (20.35 mg/kg/day) but were partly restored to normal levels by GST and high doses of auranofin, but not by d-penicillamine (Connolly et al. 1988). Studies from the same group (Stecher et al. 1987) showed that plasma fibronectin levels were reduced by HCQ and some other DMARDs in parallel with paw swelling in arthritic rats, but this was not observed with NSAIDs. The spleen cell production of lymphocyte-activating factor (LAF), a measure of bioactive IL-1, was unaffected by CQ although it was reduced in those arthritic rats given gold complexes (Connolly et al. 1988). Clearly, these drug effects separate the cellular-immunologic actions of different DMARDs although their effects may depend on the intensity of the disease in different rat strains.
Although the latter studies in arthritic rats showed that CQ had no effect in vivo on IL-1 production, studies in normal human PBMC’s with HCQ showed that 100–1000 μM was found to inhibit LPS-stimulated IL-1 in concentration-related manner (Sperber et al. 1993). Likewise, HCQ causes a concentration-related reduction in both ELISA-assayed and bioassay of IL-6 in the concentration range of 1.0–1000 μM ((Stecher et al. 1987). In contrast to these results, HCQ did not alter the synthesis of mRNA for IL-6 or IL-1α suggesting that there was a post-translational block on the synthesis of these cytokines by HCQ (Stecher et al. 1987). Production of TNF-α from human macrophages stimulated with lipopolysaccharide has also been found to be inhibited in a concentration-related manner by CQ (0.1–100 μg/mL) (Pico et al. 1991).
Studies by Jang and co-workers suggest that CQ 50 or 100 µM affects the production of mRNA for these cytokines (Jang et al. 2006). The production of TNFα, IL-2, IL-4 or INFα in monocytes or T cells was unaffected by low concentrations of HCQ. Higher concentrations (25–100 µM) of CQ have been found to reduce TNFα in human PBMC and monocytes as well as in LPS-stimulated U937 and THP-1 mononuclear cell lines (Jang et al. 2006). At the highest concentration, 100 µM CQ reduced the production of mRNA for TNFα in these cells without blocking production of the TNFα precursor (Pico et al. 1991).
Concentration-dependent inhibition of TNFα, IL-6 and IFN-α has been shown by CQ in mitogen-stimulated peripheral blood mononuclear cells (Karres et al. 1998) and by HCQ in endotoxin-stimulated whole blood (Zhang et al. 2007).
Zhou et al. (2015) have found that CQ 15 μM inhibited the expression of heat-inactivated Staphylococcus aureus (75 μg/mL)-induced IL-6, TNFα and CCL2 in cultured RAW 264.7 macrophages. However, there were contrasting effects on the levels of mRNA for these pro-inflammatory cytokines. The mRNA for IL-6 was decreased; mRNA for CCL2 was increased, while the mRNA for TNFα was unaffected. It is possible that the differential effects of CQ could be related to a single concentration levels of the drug and Staphylococcus aureus being employed. Thus, higher or lower concentrations of these may have resulted in different effects. These authors also showed that the intracellular levels of the signalling pathways involved in regulating the transcription and post-transcriptional pathways controlling the above-mentioned cytokines, i.e. mitogen-activated protein kinases (MAPK), nuclear factor κB (NFκB) and p70S6K (an indicator of mTORC1 activity) were reduced in a time-dependent manner over 0.5 to 24 h. Other components of intracellular transduction pathways, janus kinases (JK), p-Erk1/2 and p38 were reduced but at shorter time intervals of 9 to 60 min. This suggests that there are multiple sites of effects of CQ in controlling pro-inflammatory cytokine expression. It would be useful to establish wider ranges of the effects of CQ and Staphylococcus aureus to demonstrate full concentration-dependent effects of the drug in macrophages.
HCQ orally administered at doses of 2.5 mg/kg/day for 24 to 36 weeks has been found to reduce proteinuria in a time-dependent manner after 26–28 weeks dosing in NZB/W mice, a model for lupus (Chafin et al. 2013). This co-incided with reduced plasma levels of TNFα, IL-6, IL-10, anti-dsDNA IgG2a, the latter being a biochemical parameter for lupus disease. Similar results were obtained in the same strain of mice given prednisolone 1.0 mg/kg/day over the same time period. Both drugs reduced the expression of a micro-RNA, miR-155, in mesangial and DC cells as well as urine from lupus mice that were dosed for 24, 32 and 36 weeks of age. Other micro-RNAs that regulate inflammatory reactions were also affected over the same time periods by these drugs. The results suggest that HCQ, like that of prednisolone, may exert epigenetic control of cytokine gene expression as part of the anti-inflammatory actions of HCQ in lupus disease.
Of particular interest in relation to the skin reactions that occur in SLE are the observations of Wozniacka et al. (2008) in which mRNA levels for IL-1β, IL-6 and TNFα were measured in UV-radiated biopsied skin sites of 14 patients with SLE before and after monotherapy with CQ phosphate 125 mg b.i.d. for 3 months. CQ did not affect the messenger expression for these cytokines in non-irradiated sites but the UV treatment which causes an increase in expression was reduced by CQ by about 1/3–1/2. Abnormal production of IL-1 and diminished T cell responsiveness especially to IL-2 are features of SLE (Miller 1995). Thus, inhibition by CQ of IL-1 production and subsequent IL-6 may have particular therapeutic significance in patients with SLE.
T cell responses
T cell responses to MHC antigens that underlie graft versus host (GVH) disease may be affected by HCQ although inhibition of GVH has been found to only be variably inhibited in patients who had bone marrow transplantation (Ben-Zvi et al. 2012).
Using a T cell clone (CD4+/CD8− phenotype) from an RA patient, Landewe and co-workers (Landewe et al. 1995) found that CQ 2–50 µM inhibited T cell proliferation and IL-2 production induced by an immobilised monoclonal antibody to αCD3 in an identical concentration-related manner with the EC50 being 7 or 11 µM, respectively. Comparisons with cyclosporin-A (CsA) showed that this drug was more potent and had an EC50 for inhibiting proliferation which was 70 µM and 11 nM for IL-2 production. These authors showed that the inhibition by CQ of IL-2 production was due to the reduction in MkNA. CQ 6–24 µM was also found to reduce that responsiveness of the synovial T cell clones to IL-2. There may be differences in responsiveness of RA synovial cells involving cytokines compared with that in T cells derived from normal PBMCs. These studies with RA T cell clones may give better definition of pharmacological actions of anti-malarials because of the relative homogeneity of the cell population.
In an investigation of T cell antigen receptor (TCR) signalling events that might be affected by HCQ, Goldman and co-workers showed that proximal TCR events including protein tyrosine phosphorylation, phospholipase-Cα1 phosphorylation total production of inositol phosphates, as well as anti-TCR-induced ras-signalling in Jurkat T cells treated with anti-CD3, were all unaffected by HCQ 1–100 µM (Goldman et al. 2000). However, antigen receptor intracellular calcium mobilisation was inhibited in Jurkat T cells and Ramos B cells by 50 or 100uM HCQ, and in normal human PBMC T cells by 25-100 µM HCQ (Goldman et al. 2000).
Another target for anti-malarial drugs is the process of the T cell programmed cell death, or apoptosis. This might be linked to the observations by Neill et al. (1973) of chromosomal aberrations induced by CQ in PBMC of rheumatic patients since Lai et al. (2001) have shown that HCQ 3.75 or 7.5 µM (in what is considered therapeutic concentrations) induces cell death in IL-2-stimulated and resting normal human PBMC and Jurkat T cells or other T cell lines in a time-dependent fashion by mechanisms involving DNA damage through caspase-3 as well as caspase-8 independent, by a Z-Asp-Glu-Val-Asp-fluoromethyl ketone-sensitive signalling pathway. There is no involvement of Fas in mediating the apoptosis induced by HCQ or other anti-rheumatic drugs. These studies were performed in normal human PBMC (and cell lines) but the situation is probably different in rheumatic patients, especially those with SLE in which apoptosis is increased as part of the disease in which autoreactive T cell subsets can kill monocytes (Kaplan et al. 2002). Apoptotic ligands mediate autologous monocyte cell death induced by lupus T cells and this cytotoxicity is due to increased expression of receptors on activated T cells (Kaplan et al. 2002). However, the expression of apoptotic ligands (TRAIL, TWEAK and FasL) has been found by Kaplan et al. (2002) to be unaffected by 0.1–100 µM of CQ, hydrocortisone, 6-methylpurine, indomethacin or combinations thereof. These results highlight the complexity of comparisons between T cells of normal and rheumatic (SLE) patients.
Several studies have shown that antigen-presenting cell (APC) activity is affected by anti-malarials (Ben-Zvi et al. 2012). Among these, Yi et al. (1996) showed that 25 µM CQ abrogated APC activity in monocytes by PBMC from patients with monoclonal gammaglobulinopathies stimulated with IgGF(ab1)2 fragments or a purified protein derivative.
Another mode of action of CQ involves effects on chemokine expression. Hugosson et al. (2002) found that CQ 10 or 30 µM reduced antigen- and mitogen-induced proliferation of PBMC, and that 10 µM CQ enhanced the number of IL-10 producing cells exposed to these stimuli. CQ had no effect on the number of TNF-α producing cells in PBMC exposed to these stimuli. CQ 10 µM increased the expression of the surface adhesion or reactive molecules, ICAM-1 (CD54), CD80 (137-1), CD86 (B7-2) and CD14 (Hugosson et al. 2002). The enhanced expression of the anti-inflammatory cytokine, IL-10, by CQ may affect the balance of Th1/Tc1 and Th2/Tc2 cytokine responses. The authors of this study observed that the increased expression of ICAM-1 was surprising in the context of immunosuppression. They suggested that the possibility that the upregulated molecules may be altered or non-functional, but their increased expression indicates that the APCs are prepared for effective antigen presentation. Alternatively, CQ might down-regulate other molecules or increase inhibitory molecules so as to modulate the actions of ICAM-1 or other surface molecules.
A key element to the innate immune functions that have been found to be regulated by HCQ is the Toll-like receptor protein, whose production is higher in synovial tissues from patients with RA compared with that from those with OA (Bretano et al. 2005; Kyburz et al. 2006). HCQ and CQ reduce the expression of TLR-3 in synovial fibroblasts and this is suggested as another means of immunological regulation by these drugs (Bretano et al. 2005; Kyburz et al. 2006; Lafyatis et al. 2006). Production of interferon-γ in NK cells that is regulated by Toll receptors in cells stimulated with IL-12 has been found to be inhibited by CQ (Girart et al. (2007). Other studies support the roles of the Toll-like receptors TLR7/9 as potential targets for CQ and HCQ in SLE and RA (Sun et al. 2007).
Actions on neutrophils (PMNs)
Ward in 1966 showed that CQ, like that of glucocorticoids, inhibited the chemotaxis of rabbit polymorphonuclear neutrophil leucocytes (PMNs) in response to a chemotactic factor in rabbit serum; the EC50 for this being 8.4 µM (Ward 1966). Phagocytosis of zymosan particles was reduced but at a higher effective concentration of 0.1 mM than required for chemotaxis, and yet the drug has no effect on complement activation. Using the reversed passive Arthus reaction in guinea pigs as a model for chemotaxis in vivo, CQ 20 mg i.m. or the same dose 30 min before and followed by 30 mg i.m. reduced the PMN counts at skin sites, vasculitis and gross oedema and erythema.
Ferrante and co-workers found that only high concentrations of 50 μM CQ had any effects on chemotaxis induced by fMLP of human PMNs, while other anti-malarials (e.g. mefloquine) were more potent inhibitors of this reaction (Farrante et al. 1986). Activity of the hexose-monophosphate shunt was only slightly inhibited by CQ, but was more markedly inhibited by other anti-malarials. RNA and protein synthesis were unaffected by these treatments.
The production of superoxide anion (O ·−2 ) by human PMNs exposed to fMLP was shown by Hurst and co-workers to be inhibited equally by 100μM HCQ or CQ, but not by the lower concentrations of 10 or 1.0 μM (Hurst et al. 1987). The production of O ·−2 induced by fluoride was also reduced in a time-dependent manner by 100 μM CQ. The release of diacyl-glycerol following stimulation by fMLP was also moderately reduced by 100 μM CQ. The same group showed that the uptake of CQ and HCQ into PMNs (and other leucocytes) was concentration and time related, but did not affect cell viability (French et al. 1987). The concentration of HCQ in PMNs of RA patients who had taken 400 mg of the drug daily for at least 3 months was 0.2 ± 0.2 (SD) nmol/106 cells while cellular levels in mononuclear cells were much higher, being 0.6 ± 0.4 (SD) nmol/106 cells. The authors noted that much higher concentrations of CQ and HCQ are required when added in vitro to achieve equivalent therapeutic concentrations to those achieved in patients.
Using opsonised zymosan as the stimulant of O ·−2 production by human PMNs, Miyachi and co-workers showed that CQ and quinacrine both suppressed O ·−2 production at the lowest concentration of 2.5 nM while inhibition increased progressively with increase in drug concentration up to 2.5 μM of both drugs (Miyachi et al. 1986). The production of O ·−2 by the xanthine–xanthine oxidase enzyme system was unaffected by CQ up to 2.5 μM and was slightly reduced by the highest concentration of 2.5 μM quinacrine. The generation of the hydroxyl radical (OH·) by zymosan-stimulated PMNs was also reduced in a concentration-related fashion paralleling that of O ·−2 production. However, OH· production by the xanthine/xanthine oxidase enzyme system was reduced by >250 nM of both drugs.
Similar drug effects on chemiluminescence were observed by >25 nM of both drugs in a linear concentration-related manner. These authors (Miyachi et al. 1986) noted that the effects of these anti-malarials could be linked to their inhibitory effects on phospholipase A2 (Rainsford 1988). Undoubtedly, the antioxidant effects of HCQ and CQ have considerable therapeutic significance, especially since they are apparent at concentrations that are well within the therapeutic range.
In addition to confirming the effects of HCQ and CQ on the opsonised zymosan—and fluoride stimulation O ·−2 pathway, Hurst and co-workers (Hurst et al. 1987) observed that these drugs blocked production by phorbol myristate acetate (PMA) and aside from the Mo-1-zymosan receptor (whose expression was only slightly reduced at high concentrations of these drugs) the other receptors, FMC4 and FMC13 (which are activated by the other 2 stimulants) did not appear to exhibit altered expression (French et al. 1987). The authors concluded that HCQ and CQ show multiplicity of actions on O ·−2 production via non-lysosomal pathways.
Additionally, several authors have established that CQ or HCQ inhibit the production of the superoxide anion (O ·−2 ) from human polymorphs (Hurst et al. 1988; Minta and Williams 1986; Neal et al. 1987) by immune complexes and other stimuli accompanied by reduction in chemiluminescence (Muller-Peddinghaus and Wurl 1987), a surrogate measure of oxyradical production.
Arachidonic acid and phosphoinositide metabolism and actions on prostaglandins
It is well established that CQ like other anti-malarials inhibits lysosomal phospholipases A1 and C (Matsuzawa and Hostettler 1980; Kubo and Hostettler 1980). In the case of the effects on phospholipase C, there are notable effects on lysosomal storage of phosphoinosites in various organs and tissues, including that in brain (Pappu and Hauser 1981; Hostetler and Richman 1982; Gräbner and Meerbach 1983). These effects of CQ may be relevant to the potential of this drug and HCQ to result in improvement of symptoms in the skin and central nervous system of patients with SLE.
CQ but not mepacrine or some other 4- and 8-aminoquinolines inhibits the transmethylation of phosphatidyl ethanolamine to phosphatidyl choline (lecithin) (Hurst et al. 1988). However, this effect was notably not evident with HCQ (Edmead et al. 1996).
In contrast to the inhibitory effects of CQ and mepacrine on PLA2 activity in various tissue systems noted above, studies with PLA2 from neutrophil sonicates incubated with 14C-labelled phospholipids of Escherichia coli showed that high concentrations of CQ and mepacrine increased their hydrolysis (Authi and Traynor 1982). Using a PLA2 preparation from peritoneal fluid, a biphasic inhibitory effect on 14C-phospholipid production was noted by Authi and Traynor (1982) with a progressive decline in activity by CQ, mepacrine and primaquine in the concentration range of 0.1–1.0 mM followed by either decline (with CQ) or in the case of mepacrine, an increase in activity at higher concentrations. In reality, the relevant concentrations for effects are probably in the sub-millimolar range, except where there may be high concentrations of these drugs in organs such as the gastrointestinal tract or in lysosomes/autophagosomes.
CQ has also been reported to affect the lysosomal acidic form of sphingomyelinase (Wiegmann et al. 1994), with evidence that CQ inhibits this enzyme during T cell receptor arrangements. CQ also affects downstream regulation of the generation of the transcription factors, NFκB and to a lesser extent AP-1; both these signalling reactions being important in the epigenetic control of the production of inflammatory mediators and regulation of T cells (Edmead et al. 1996).
In addition to the possibility that CQ may reduce the production of prostaglandins and leukotrienes, via inhibition of phospholipase A2 (Rainsford 1988); studies using rat mesenteric vascular bed preparations showed that CQ, quinine and some analogues could antagonize the actions of several prostaglandins, with the most prominent being PGE2 (Manku and Horrobin 1976). The inhibitory effects of CQ on the pressor responses to adrenaline in the presence of PGE2 could be demonstrated at concentrations as low as 9.5 μM (Manku and Horrobin 1976).
It is apparent from these studies that CQ may affect several pathways involved in phospholipids and arachidonic acid metabolism. It is possible that there are differences between CQ and HCQ (e.g. in phospholipid methylation) (Hurst et al. 1988), but these and other observations require further investigation to establish if there are differences between these two drugs on the arachidonate/phosphoinositide pathways as well as on signalling via NFκB and AP-1.
Cartilage metabolism and degradation
Whitehouse and Cowley 1966 showed that CQ inhibits the protease-induced release of peptides by cartilage slices. Lysosomal stabilisation by CQ and other anti-malarials could conceivably be a major site of action of these drugs in controlling degradation of connective tissues in arthritic conditions (Whitehouse and Cowley 1966). Several studies have shown that CQ inhibits degradation of proteoglycans in vitro and has direct effects on elastase and other enzymes released from macrophages (Whitehouse and Boström 1965; Cowey and Whitehouse 1966; Fulkerson et al. 1979; Famaey and Fontaine 1980; Ackerman et al. 1981; Tauber et al. 1985; Bartholomew and Lowther 1987; Adeyemi et al. 1990; Kamal and Bassiouni 1992; Schug and Kalbhen 1995; Lullmann-Rauch et al. 1996). The central role of the destruction of cartilage (and bone) by pro-inflammatory cytokines (IL-1, TNFα) in arthritic conditions has been well recognised for several decades (Etherington et al. 1981; Cox and Duff 1996).
Investigations of the effects of CQ, HCQ and structural variants of these drugs showed that both CQ and HCQ were potent inhibitors of catabolin (a mix of IL-1, TNF-α and IL-6 from porcine leucocytes (Saklatvala et al. 1984; Saklatvala and Sarsfield 1988), or purified porcine or human recombinant IL-1α-induced cartilage proteoglycan degradation (Rainsford 1985, 1986, 1987; Fig. 9). The EC50 for effects of these drugs on porcine IL-1α was 50–60 µM while that on human recombinant IL-1α was 10–20 µM (Rainsford 1986). These differences could reflect the porcine IL-1α being glycosylated whereas the human recombinant form is a pure peptide without being glycosylated as isolated from transfected bacteria. Investigations with different structural analogues of CQ revealed the importance of the tertiary alky or hydroxyl amino-side chain-substituent for the actions of CQ since the amino- or N-pyrrolidone derivatives were inactive. More lypophilic anti-malarials such as mefloquine were more potent inhibitors of IL-1-induced cartilage destruction (Rainsford 1986). Other studies have also shown that CQ inhibits cartilage PrGn resorption induced by human recombinant IL-1 (Arner et al. 1987; Neidel and Zeidler 1993). CQ has also been shown to inhibit collagen breakdown in cartilage from OA patients (Trnavská and Trnavský 1967).
In studies investigating the uptake of tritium-labelled CQ into the bovine nasal cartilage in organ culture in the presence and absence of IL-1 or catabolin (Saklatvala et al. 1984; Saklatvala and Sarsfield 1988) that cartilage could accumulate as much as 6 times the radioactivity when incubated without IL-1 or catabolin but in the presence of these cytokines, there was a time-dependent decline in accumulation of radiolabelled CQ (Fig. 9). Autoradiographic studies with tritium-labelled HCQ have shown that this drug accumulates in the cartilage and surrounding articular tissues of mice in vivo (Cecchi and Porzio 1964), thus showing the effects of accumulating anti-malarial drugs may occur in vivo.
The accumulation of CQ in cartilage could be due to the affinity of this basic water-soluble drug to acidic proteoglycans in the presence of the aqueous milieu that surrounds proteoglycan molecules. This could effectively protect proteoglycans from destructive attack by enzymes. When the proteoglycans have been partially degraded as a result of induction of tissue-destructive enzymes by IL-1 and TNF-α, then the structures of proteoglycans could be more “exposed” to proteolytic attack and so with fewer acidic groups so that the basic drug cannot bind too much to these macromolecules.
Sheppeard and co-workers claimed that CQ (40 μg/mL) inhibited the release and activity of catabolin from cultured pig synovium (Sheppeard et al. 1982). However, others have found that the release of this cartilage degrading activity (or catabolin) from porcine synovial tissue in organ culture was either unaffected or slightly increased by CQ (Rainsford 1987). The differences in these effects are probably due to assay methodologies as well as high concentrations of the drug in the former study (Sheppeard et al. 1982). Also buffering of the media and serum components could have influenced the activity: aspects which have been found subsequently to be important (Rainsford 1987).
Based on these studies showing protection of cartilage by CQ, it has been proposed (Rainsford 1990) that CQ could reduce cartilage destruction in arthritic diseases (especially in osteoarthritis) as a consequence of its ability to accumulate in the aqueous environment of acidic proteoglycans in the cartilage and actions on the inflammatory cells and synovial production of cytokines and enzymes. The potential clinical implications of these and other observations are considered in the next section (“Osteoarthritis”).
The central role of nitric oxide (NO) in mediating cartilage matrix degradation, along with cytokines, joint destructive enzymes and reactive oxygen species has led to much interest in the control of NO being part of the means of controlling joint destruction (Krane et al. 1986; Pettipher et al. 1986; Vuolteenaho et al. 2003; Yasuda 2006; Järvinen et al. 2008), in particular as the actions of NO appear to be mediated via TNFα eliciting cytotoxicity (Estrada et al. 1992) and the generalised increase in NO in activated chondrocytes. Vuolteenaho et al. (2005) showed evidence for NO as a potent inflammatory mediator a particularly interesting target for drug actions in arthritic disease. Using immortalised H4 chondrocytes, they observed that HCQ, like that of the DMARDs, sodium aurothiomalate, methotrexate and leflunomide, inhibited the IL-1β-induced NO synthase and NO production; d-penicillamine and sulphasalazine had no effect (Vuolteenaho et al. 2005). The site of action of these 4 inhibitory DMARDs was suggested to be the IL-1β-induced induction of the NFκB transcription factor. These authors also found that HCQ and sodium aurothiomale reduced IL-1β-induced NO production in primary chondrocyte cultures and OA cartilage. They suggested that HCQ might be of possible therapeutic benefit in controlling joint destruction in OA, thus supporting the same suggestion (Pettipher et al. 1986) which was based on the effects of CQ on IL-1-induced cartilage proteoglycan destruction.
Aside from the effects of anti-malarials on cytokine-mediated cartilage destruction, earlier studies showed that these drugs inhibit cartilage metabolism (Whitehouse and Boström 1962, 1965; Boström et al. 1963; Whitehouse 1967), especially that involved in the biosynthesis of proteoglycans (PrGns) or the mucopolysaccharide components of PrGns (Whitehouse and Boström 1962, 1965; Boström et al. 1963). Interest in this mode of action of anti-rheumatic agents at that time centred on the view that by inhibiting metabolism, these drugs would control the proliferation of connective tissues around joints (pannus) and so prevent the immobility of joints. More recent views suggest that the inhibition of cartilage PrGns may underlie the joint space narrowing and cartilage destruction seen in arthritic patients who have taken some, but not all, NSAIDs (e.g. indomethacin) (Rainsford et al. 1992). While CQ and HCQ at millimolar concentrations have been found to inhibit the biosynthesis of PrGns in vitro (Whitehouse and Boström 1962, 1965; Boström et al. 1963), this has not been observed in rats in vivo (Boström et al. 1964). Thus, the situation about the actions of these drugs on cartilage PrGns is unclear.
An attempt to identify key marker genes termed molecular signatures in chondrocytes that are involved in expression of catabolic mediators (inflammatory mediators, cytokines, chemokines and matrix destructive enzymes) and anabolic mediators (matrix synthesis, proliferation and differentiation) was undertaken by Andreas et al. (2009). Of 110 RA-related genes identified in human chondrocyte cultures (derived from knees of post-mortem subjects), the expression of those genes controlling key enzymes was markedly reduced by non-cytotoxic concentrations of azathioprine, sodium aurothiomalate and methotrexate but less so by CQ, while the NSAIDs, diclofenac and piroxicam affected genes expressing inflammation (NFκB) and chemokines/cytokines. The corticosteroids, methyl-prednisolone and prednisolone were particularly effective in suppressing those genes controlling inflammatory mediators (NFκB, cytokines, chemokines) of the immune responses matrix degeneration, but they also suppressed genes controlling matrix remodelling as well as cell proliferation and differentiation. Hierarchical cluster analysis and principal components analysis showed that corticosteroids were most potent, while CQ and diclofenac had minor effects on disease genes in contrast to DMARDs which reduced the RA-associated signature. To some extent, these results from an elaborate genomic expression study confirm what is known about molecular actions of the range of drugs that were studied. Criticisms of this study include the fact that only the genes controlling the immuno-inflammatory and regenerative activities but not the protein expression, were studied. Also, the studies were performed in chondrocytes derived from 6 post-mortem donors supposedly normal and grown in alginate cultures; the donors had no apparent joint diseases. It could be argued that “real world” studies should be performed in intact cartilage from patients with RA or OA.
Studies in arthritic patients
Rheumatoid arthritis
In view of the wide range of cellular and molecular actions of CQ, to a lesser extent HCQ, which have been identified as potentially important in controlling synovial inflammation, cartilage and bone destruction it is instructive to examine how these pharmacological effects translate into controlling joint destruction in animal models of arthritic diseases as well as in patients with RA.
Studies in adjuvant arthritic rats have, as noted previously, not produced evidence of protective effects of CQ or HCQ in controlling systemic manifestations or joint destruction. Silva et al. (2005) noted that combinations of CQ with methotrexate are effective in controlling blood levels of acid phosphatase and alanine aminotransferases which the authors considered as reflecting inflammatory reactions. Combination therapy with HCQ and methotrexate has proven popular in recent years and there is evidence that the joint manifestations of RA disease are more effectively controlled by both drugs compared with that of these drugs alone (O’Dell 1999; Biasi et al. 2000; O’Dell et al. 2001; Goekoop et al. 2001; Carmichael et al. 2002; Mottonen et al. 2002; Verstappen et al. 2003; Korpela et al. 2004; Katchamart et al. 2009; van Vollenhoven et al. 2009).
An earlier histological investigation by Julkunen and co-workers in 28 RA patients showed that CQ taken for ≤6 months resulted in fewer changes in articular cartilage, reduced pannus formation and more vigorous bone regeneration (Julkunen et al. 1976). These authors concluded that CQ appears to have a prophylactic effect on joints in RA.
A double-blind radiological investigation by van der Heijde and co-workers in 60 RA patients (who had not previously been exposed to DMARDs) was performed in which patients were randomised to receive HCQ or sulphasalazine for 48 weeks (van der Heijde et al. 1989). There were fewer joint erosions in the sulphasalazine compared with the HCQ group at 24 and 48 weeks of treatment. It is difficult to establish what relative changes took place in the drug-treated groups compared with those at baseline. A review of 8 randomised controlled clinical trials involving treatments with HCQ and CQ undertaken by Sanders (2000) concluded that these treatments had little, if any, effects on the radiologically observed progression of bone erosion and joint destruction in RA whereas gold complexes, methotrexate and azathioprine showed some improvement. There may be dose- and time-related effects of HCQ or CQ that were not considered in the outcomes from these trials, but the results suggest these anti-malarials have less favourable outcomes on joint destruction in RA.
A further radiological study by Eklund and co-workers involved comparison of joint changes at 24 months with plasma IL-1β and CRP levels in RA patients that received HCQ, sulphasalazine and methotrexate alone or in combination (Eklund et al. 2007). By 6 months of treatment, there were no changes in the levels of IL-1β or CRP. The IL-1β levels correlated with radiologic indices of joint damage at the start but not after 24 months of treatment with the DMARDs. It is difficult to draw conclusions about the effectiveness of these drug treatments with radiological evidence of improvement in joint damage, since it is possible that the drug had effects on one of these parameters that was not revealed in the correlation analysis.
Of importance in relation to effects of combinations of DMARDs, HCQ appears to minimise the acute hepatic effects due to MTX (Carmichael et al. 2003) which may prolong the benefits of this important DMARD. HCQ also appears to be beneficial in reducing MTX nodulosis (Combe et al. 1993), a complication of MTX therapy that makes it difficult for some patients to continue methotrexate therapy.
Overall, these studies on the pharmacological actions of HCQ and CQ do not appear to have a parallel in the therapy of RA, especially in joint damage. It is possible that the trial designs and means of assessing joint damage may represent substantial limitations. The use of MRI and more extensive screening of biomarkers of joint injury, cytokines and acute phase reactants may be approached in the future.
Systemic lupus erythematosus
A long-term study reviewed by Petri 1996 and later in 2005 involved SLE patients in the Baltimore Lupus Cohort I, a study which involved the monitoring plasma levels of lipids, glucose and thrombotic activities of patients that took HCQ (Petri 1996, Petri 2005). These observations have particular significance for the health of a group of patients that are at risk of cardiovascular disease, diabetes mellitus and liver function tests; elevated liver enzymes being a consequence of therapies such as methotrexate (Petri 1996). There is increasing evidence that HCQ may have multiple beneficial effects in SLE, in particular reducing the risk of cardiovascular events (Tang et al. 2012). Among the molecular actions of anti-malarials that may be beneficial in prevention of atherosclerosis, CQ may affect lipid metabolism by inhibition of cholesterol synthesis (via effects on 2,3-oxidosqualene-lansterol cyclase), blockade of lysosomal metabolism of cholesterol, stimulation of LDL receptor activity, increased HMG-CoA reductase and reducing precursors for biliary steroids, and through these actions have lipid-lowering actions in treatment of hyperlipidaemia associated with SLE. A patient cohort of 3027 SLE patients that received HCQ or prednisone (a risk factor for hyperlipidaemia) showed that HCQ lowered serum cholesterol by 8.9 % (Petri 1996). There are several mechanisms by which CQ might control glucose levels and metabolism as well as insulin turnover in diabetes mellitus (Petri 1996, 2005; Petri et al. 2012). Among these, HCQ exerts an insulin-sparing effect in diabetic rats (Emami et al. 1999a) and reduces the receptor-mediated degradation of insulin, leading to enhanced activity of insulin (Knutson et al. 1985; Emami et al. 1999b). In streptozotocin-induced diabetic rats, renal clearance of HCQ and its enantiomers was reduced compared with controls (Emami et al. 1999b). Likewise, in adjuvant arthritic rats the renal clearance of HCQ and its enantiomers is reduced. The increased plasma concentrations of HCQ enantiomers were related to the relative anti-inflammatory activity of the drug (Emami et al. 1998). CQ also reduced the flux of glucose through the hexose-monophosphate shunt and gluconeogenesis (Kelman et al. 1981; Jarzyna et al. 2001). There is also evidence for modest improvement in glucose tolerance in patients with SLE (Gerstein et al. 2002; Petri et al. 2012). These studies suggest that HCQ and CQ have potential benefits in insulin-dependent diabetic patients.
Several lines of investigation have indicated that HCQ may have anti-thrombotic activity (Petri et al. 2012) partly as a result of its actions on arachidonic acid metabolism and inhibition of platelet activation and adhesion to the sub-endothelium (Gallus, 1979; Achuthan et al. 2015). CQ does not inhibit cyclo-oxygenase-1 (COX-1) whereas HCQ is a modest inhibitor of this enzyme in whole blood (Ben-Chetrit et al. 2005), and this is probably a factor in its effects on platelet aggregation. A study by Achuthan et al. (2015) in human volunteers showed that prior treatment for 7 or 14 days with HCQ resulted in a 11 % reduction in arachidonic acid-induced platelet aggregation, but not when adenosine disphosphate or collagen was used as agonists, thus confirming the site of action of HCQ on COX-1. However, of particular interest are the observations by these authors that a combination of HCQ and an anti-platelet dose of aspirin had markedly increased inhibitory effects on platelet aggregation but this did not relate to decrease in serum levels of 11-dehydroxy-thromboxane B2 (the stable metabolite of thromboxane A2) compared with that from aspirin or HCQ. The authors suggested that perhaps HCQ has a site of action downstream from the COX-1 site affected by aspirin. HCQ alone or in combination with aspirin can result in a significant decrease in fibrinogen and erythrocyte sedimentation rate, highlighting the disease-modifying effects of HCQ.
Amongst the most significant actions of HCQ is the ability of this drug to reduce the pronounced thrombogenic properties of anti-phospholipid antibodies (Edwards et al. 1997; Rand et al. 2008). Studies in the Baltimore Lupus Cohort SLE patients suggested that HCQ might have protective effects against future thrombotic events (Petri 1996, 2005; Petri et al. 2012).
Derksen and de Groot (2010) have questioned the current recommendations for the long-term management of aPL syndrome which include high dose, and sometimes life-long anticoagulation, stating that many of the studies had not been prospective or well controlled and many had not distinguished between venous or arterial thromboses. This has resulted in a call for “evidence based treatment of thrombotic aPL syndrome” and a trend toward a more conservative approach using HCQ and/or low dose ASA in these patients such as employed by Hereng et al. (2008).
The “Euro-Lupus cohort” is a long-term project in 1000 patients addressing the epidemiology of SLE which has revealed that the 5 and 10 years survival has improved substantially since the 1950s but the causes of death still remain: active disease 26 %, infection 25 %, thrombosis 25 % and malignancy 6 % (Cervera et al. 2009). Even though HCQ use was initially limited to the more benign manifestations of arthritis and dermatitis in patients with SLE, recent publications have suggested that the use of HCQ improves morbidity and mortality for patients with SLE and this has resulted in increased use of this drug in these patients (Ruiz-Irastorza et al. 2010). Other reports have shown that HCQ may have a protective effect on renal damage in patients with lupus nephritis, which is also known to be an important factor influencing mortality in these patients (Sisó et al. 2008; Pons-Estel et al. 2009) as are thrombovascular events for which there is increasing evidence that they can be prevented by anti-malarials (Jung et al. 2010; Ruiz-Irastorza et al. 2010; Katz and Russell, 2011).
Neonatal lupus syndrome
Antibodies to Ro extractable nuclear antigen are primarily found in patients with SLE and SS. Two percent of mothers with Ro antibodies may produce a child with primary congenital complete heart block, an irreversible feature of the neonatal lupus syndrome. (Brucato et al. 2001). This syndrome is considered to be a manifestation of the transplacental passage of the Ro antibody and many of these infants require permanent pacemakers. Once established, the complete heart block is not reversible, so the emphasis has been on prophylaxis with closed monitoring in an attempt to prevent lesser degrees of heart block from progressing. Recent reports, however, have suggested that HCQ may be able to prevent the cardiac damage that results in the scarring of the foetal conducting system (Izmirly et al. 2010). Izmirly et al. (2010)studied 50 children with cardiac disease and 151 control children born to lupus mothers with Ro/La antibodies and determined that 14 % of the children with cardiac disease had been exposed to HCQ compared to 37 % of the controls. Multivariable analysis led these authors to conclude that the OR for developing cardiac disease associated with HCQ use was 0.46 (Izmirly et al. 2010).
Sjögren’s syndrome
Sjögren’s syndrome is a chronic systemic autoimmune disease with a predilection for the exocrine glands—an autoimmune exocrinopathy. Recent concepts have considered it to be “SLE of the exocrine glands” and as such patients with this disease are finally being treated more aggressively. Fox published data in 1996 from a retrospective open-label study that showed HCQ were able to improve local (painful eyes and painful mouth) and systemic manifestations (arthralgias and myalgias) as well as laboratory markers (lowering of the ESR and improvement in quantitative IgG levels) in patients with primary Sjögren’s Syndrome (pSS) (Fox 1996).
Recently, there have been refinements in the outcome measures of pSS with the development of disease-specific questionnaires, clinical definitions of pSS such as the American–European Consensus Group (AECG) Criteria (Vitali et al. 2002), and international projects such as that developed, e.g. under the sponsorship of the European League Against Rheumatism (EULAR) in which indices of disease activity have been devised (Seror et al. 2014) and validated (Seror et al. 2015). The issue of clinical definitions of pSS has been debated (Vitali et al. 2103) and attempts at obtaining consensus statements have been published (Seror et al. 2015). The need for more precise definitions that addressed disease-specific measures arose to meet the challenge of obtaining primary endpoints, the development of new biologic agents to treat pSS and notably to demonstrate the efficacy of HCQ (Seror et al. 2014). In their review of outcome measure of pSS, Seror et al. (2014) pointed out that although HCQ is the most frequently used treatment based on observational studies (e.g. see Fox 1996), that in one double-blind cross-over study which extended for 2 years, HCQ had no significant clinical effects but only showed improvement in biological values (Kruize et al. 1993). The need for clear definitions and criteria for efficacy became recognised. As a result of a EULAR initiative indices for symptomatic efficacy (the EULAR Sjögren’s Syndrome Patient Reported Index, or ESSPRI) and disease activity (the EULAR Sjögren’s Syndrome Disease Activity Index, or ESSDAI) were developed to obtain evidence for efficacy (Seror et al. 2014, 2015).
Recently, the results of a randomised placebo-controlled multicentre study was performed in 15 centres in France during the period of April 2008 and May 2011 known as the JOQUER Trial (Gottenberg et al. 2014). This study compared the effects of daily HCQ 400 mg/d with placebo assigned in a 1:1 ratio from 0 to 24 weeks with an ‘open-label’ extension to 48 weeks initially in 120 randomised patients with pSS defined by the AECG criteria, with data being analysed on the basis of intention-to-treat. The primary end-point was evaluated at week 24 and was the proportion of patients with a >30 % reduction in 2 of 3 of the following symptoms, i.e. dryness, fatigue and pain scores. Secondary end-points were the ESSPRI and ESSDAI indices, as well some biologic and symptomatic scores of outcomes.
The primary outcome measure showed, in essence, that there were no significant differences in the responses to HCQ compared with placebo. The proportion of patients meeting the primary end-point was 17.9 % in the HCQ group and 17.2 % in the placebo group. There were no significant changes in the individual values for dryness, pain or fatigue. Similarly, there were no significant changes in the values of ESSPRI and ESSDAI. There was, however, a significant change in the erythrocyte sedimentation rate (ESR) between the two groups at week 24 but not in any other biological or indeed clinical parameters. Only 2 serious adverse events occurred in the HCQ group and 3 in the placebo group in the first 24 weeks of the study, with 3 in the HCQ group and 4 in the placebo group in the last 24 weeks. This suggests that overall toxicity was not a major issue with HCQ treatment and was of low grade.
At the outset, this negative efficacy outcome from such a large-scale trial performed using the most advanced clinical and biological measures raised serious questions about the use and efficacy of HCQ in pSS. This is at least a superficial view until the conditions of the trail are closely examined. The most obvious treatment issue was that patients were allowed concomitant treatment with a ‘stable dose’ of NSAIDs, oral corticosteroids, pilocarpine, tear substitutes and topical cyclosporine was allowed. There was no record provided in the published study of the intake or use of these medications. Thus, there are important implications from the allowance of these medications, namely that (a) the patients were obviously having medications that would be expected to have profound effects on the symptoms and probably disease outcomes in the study; and (b) the study is NOT a comparison of HCQ with placebo in otherwise naive pSS patients BUT an investigation of the additive effects of HCQ in addition to normal symptomatic treatment with drugs that are used during therapy of pSS. Indeed the extent of disease in the patients seemed to be limited. Thus, the major conclusion that can be drawn from this study is that HCQ does not have additional efficacy above that of normal treatment with NSAIDs, corticosteroids and other agents used to control the symptoms of pSS, but it does not enable a conclusion to be drawn about the efficacy of HCQ in pSS per se.
A second and indeed significant study involving HCQ has also been reported recently by Migkos et al. (2014) which indicates that this drug has considerable long-term benefits in controlling the lipid profile and atherogenic index in patients with pSS. The authors of this study undertook a retrospective observational investigation of 71 out of 806 pSS patients who met inclusion criteria of which 103 had received HCQ who had arthralgias and symptoms of dry eyes and dry mouth (sicca symptoms) on a long-term basis for at least 5 years. The subjects had not taken lipid-lowering agents and did not have diabetes mellitus. The selected patients had undergone lipid profile analysis on a regular basis and total cholesterol (TC) high-density lipoprotein (HDL), low density lipoprotein (LDL) total triglycerides (TG) and atherogenic index (TC/HDL) were determined. The 71 patients were all women and had received HCQ (dose unspecified) for 7.2 years as well as concomitant therapy with DMARDs or steroids (doses unspecified). Progressive decrease in values for TC, LDL with increased HDL and the atherogenic index were decreased in a time-dependent manner over 6, 12, 36 and 60 month periods.
Although this was a retrospective study, it was performed in a ‘real world’ situation and showed that there were pronounced lipid lowering and HDL improvements in patients with pSS. These studies further confirm that HCQ has long-term effects in attenuating the risk of dyslipidaemia in non-diabetic patients with pSS. Thus, patients with pSS with dyslipidaemia may benefit from HCQ therapy (Migkos et al. 2014).
In other conditions that accompany SS, the rampant tooth decay that occurs as a consequence of the xerostomia is very difficult to manage but several recent studies have now shown that oral glandular secretions and sicca complaints can be improved with HCQ (Dawson et al. 2005; Descloux et al. 2009; Cankaya et al. 2010).
Osteoarthritis
There are a small number of published studies on the use of hydroxychloroquine or chloroquine in osteoarthritis. We searched the literature (MEDLINE and PubMed) for “osteoarthritis” and “hydroxychloroquine” or “chloroquine,” and limited our analysis to prospective or retrospective studies. This method returned 10 studies, published between 1977 and 2014. Of these, 7 were prospective studies and 3 were retrospective reviews. Additionally, our search produced a study protocol for an RCT that is currently underway (Detert et al. 2014).
Tejeswar Rao (1977) published the first study using an anti-malarial to treat osteoarthritis. It is unique as the only study which has used chloroquine instead of hydroxychloroquine, and which used intra-articular rather than oral administration of the drug. 15 patients with knee osteoarthritis were randomly selected from an orthopaedic clinic and given biweekly injections of chloroquine phosphate for a total of six doses. Patients were evaluated after the conclusion of treatment, based on pain, mobility, and presence of joint swelling. According to these criteria, 9 patients achieved satisfactory results, with an additional 4 showing mild improvement and only 2 out of 15 demonstrating no improvement. This study had a number of key limitations, most importantly the small sample size and lack of placebo control. Furthermore, the improvement was based on general clinical assessment and thus there is no objective measure by which to compare outcomes of other studies. Finally, the OA patient population was poorly defined, with no information provided on the presence of OA in other joints, classification as primary or secondary OA, and previous failed treatments. Despite these limitations, this study provided some early suggestion that anti-malarials merited further investigation in the treatment of OA.
Robertson et al. (1993) performed a retrospective review of 7 patients who were treated with hydroxychloroquine (HCQ) after failing to respond adequately to NSAIDs alone. All patients had osteoarthritis of the hands, involving the DIPs, PIPs, MCPs, and/or first CMC. Three patients had central erosions of the DIPs. Of note, 4 patients also had disease involving the wrist, and 2 had disease involving the knee. All patients were rheumatoid factor-negative, and two had a weakly positive ANA. Patients were treated with 200–400 mg HCQ per day (according to body weight). Within 6 months of initiating treatment, all 7 patients reported subjective improvement in OA symptoms, and the 4 who had synovitis when therapy was initiated experienced resolution.
Bryant et al. (1995) published a similar review of 8 patients with erosive OA who did not respond to therapy with NSAIDs alone. The selected patients had inflammatory arthritis of the PIPs and DIPs; however, unlike Robertson et al., these authors excluded patients with any other joint involvement. All patients had erosions of the IP joints. Notably, 3 patients were ANA positive (one strongly positive) and 2 were positive for RF. In the remaining 3 patients, ANA and/or RF testing was not performed. Treatment was 200 mg HCQ/day, and improvement was assessed based on duration of morning stiffness, clinical assessment of synovitis, and patient global assessment. 6 out of 8 patients showed improvement with HCQ, and in those who improved, the effect was evident within 7 months. Both these studies showed promising results in using HCQ to treat erosive osteoarthritis in patients who did not respond to NSAIDs, but they were limited by their retrospective design and small sample sizes.
Punzi et al. (1996) undertook the first prospective trial on HCQ in erosive osteoarthritis, selecting 15 patients who had failed to respond to conventional treatment with analgesics and NSAIDs. The selected patients had inflammatory arthritis of the small joints of the hands in addition to bone erosions. 7 patients were randomised to receive HCQ (dose not reported), and 8 were randomised to receive analgesics and NSAID. Patients were evaluated according to Ritchie index (scale of joint tenderness), ESR, and sIL-2R (soluble receptor of interleukin-2, an indicator of lymphocytic activity) at baseline, 6 months, and 12 months after treatment. The authors chose to treat with HCQ and to assess sIL-2R as an outcome after their unpublished observation that levels of s-IL2R were significantly higher in a subset of patients with erosive OA compared to those with nodal OA and compared to controls. The HCQ group had statistically significant improvements in joint tenderness at 6 and 12 months, and in ESR and sIL-2R at 12 months. The control group had improvements in these parameters that were not statistically significant.
McKendry et al. (2001) performed a randomised, double-blind, placebo controlled study to assess whether either hydroxychloroquine or acetaminophen (ACM, paracetamol) was superior to placebo in treating nodal osteoarthritis of the hands. 88 patients were randomised to one of HCQ 400 mg/day (n = 29), ACM 3.9 gm/day (n = 29), or placebo (n = 30). Assessment at baseline and 24 weeks after initiating therapy was based on the number of tender joints (assessed all IP joints and first CMC joint), Doyle index, pain Visual Analogue Scale, and duration of morning stiffness. While the HCQ group improved in all parameters, none of these improvements were statistically significant when compared to placebo. Although the sample size of this study surpassed those published earlier, we have minimal information on the patient baseline characteristics, particularly with respect to previous failed treatments and the presence of any bone erosions on radiography. Another major limitation of this study was the number of patients who discontinued treatment early (38/88). In the HCQ group, 13 patients failed to complete 24 weeks of therapy, 5 due to lack of effect, 5 due to adverse effects (details unavailable), and 3 were lost to follow-up.
Sibtain et al. (2007) undertook a retrospective review of 8 patients with osteoarthritis, all of whom were negative for rheumatoid factor. 6 patients had inflammatory OA; the remaining 2 had erosive OA. Patients received doses of 200–400 mg HCQ/day, with a mean follow-up of 2 years. 5 of the patients reported clinical improvement, and three discontinued the drug (2 due to adverse effects and 1 due to lack of effect). These results suggested a possible role for HCQ in the treatment of inflammatory/erosive OA, but these findings are limited by the retrospective nature of the study and small sample size, as well as minimal information on previous responsiveness to therapy in this subset of patients (i.e. does not delineate whether these patients had OA which was NSAID-resistant).
Bonfante et al. (2008) performed a randomised controlled trial involving 29 patients with knee osteoarthritis (Kellgren and Lawrence grades II and III), assigned to receive either hydroxychloroquine 400 mg/day (n = 16) or placebo (n = 13). Patients were assessed at baseline and at 4 months according to the WOMAC index, pain Visual Analogue Scale, and Lequèsne scale. While the HCQ group improved in all domains, their improvement was not superior to that of the placebo group. A major limitation of this study was the relatively small sample size and the short duration of follow-up.
Saviola et al. (2012) conducted a randomised pilot study of 38 patients with active erosive osteoarthritis of the hands. Patients were either assigned to clodronate (a bisphosphonate, n = 24), or HCQ 400 mg/day for first month, 200 mg/day for 11 subsequent months (n = 14). Patients were assessed based on number of swollen joints, number of painful joints, pain VAS, hand disability index (Dreiser’s questionnaire), strength (dynamometer), duration of morning stiffness, and patient and physician global assessment. Patients in the HCQ group did not have statistically significant improvement in any parameters, and as a result follow-up was shortened (initially planned for 24 months rather than 12) and enrolment was stopped (as a result the HCQ group was smaller than the clodronate group). Only 8/14 patients in the HCQ group completed 12 months of treatment, with 4 withdrawing due to inefficacy and 2 withdrawing due to a cutaneous rash. This study, unlike previous ones, did not support a role for HCQ in the treatment of erosive osteoarthritis, though these results were limited by the high rate of dropout and discontinued enrolment. Interestingly, the authors of this study noted that 5/14 patients in the HCQ group were rheumatoid factor-positive, and these 5 patients were among the 8 who were able to complete 12 months of treatment. Notably, in Brennan et al. (1995), 2 patients were RF positive, and these were among the 6 patients in whom HCQ was effective. Thus, the authors suggested that there might be two subsets of patients with erosive osteoarthritis; distinguished by their rheumatoid factor serology, and that those patients who are rheumatoid factor-positive may have more benefit with hydroxychloroquine. Interestingly, however, in the study by Robertson et al. (1993), all 7 patients were RF-negative and experienced benefit from HCQ. Ultimately, further prospective randomised studies that define the RF serology of enroled patients are needed to better answer this question.
Jokar et al. (2013) performed a double-blind, randomised placebo-controlled trial of HCQ in 44 patients with knee osteoarthritis (Kellgren and Lawrence grades II and III). Patients were assigned to 400 mg/day HCQ or placebo, and assessed according to the WOMAC index at baseline and every 4 weeks for a total of 24 weeks. Compared to controls, patients in the HCQ group had statistically significant improvements in total WOMAC score and in the three sub-categories of pain, stiffness, and functional limitation. Further, the HCQ group used significantly less analgesics and NSAIDs than the control group. The benefit of the HCQ group was maximal by 8 weeks, and continued throughout the 24 weeks of follow-up.
Another recent randomised controlled trial by Abou-Raya et al. (2014) recruited 166 patients with primary knee OA (moderate-severe by Kellgren-Lawrence grading) and persistent pain despite maximum doses of analgesics/NSAIDs and assigned them to either HCQ 400 mg/day or placebo for 36 weeks. The HCQ group had a number of statistically significant outcomes: decreased pain by Visual Analogue Scale, improvement in WOMAC physical function scores, and less conventional pain medication use. The HCQ group also had a “clinically relevant reduction in synovitis,” though it is not clear how synovitis was graded.
Ultimately, despite the relatively limited number of studies performed on HCQ in OA, and the poor design of some of these studies, there is evidence to support further investigation of this treatment modality. There is evidence through multiple retrospective reviews (Robertson et al. 1993; Brennan et al. 1995; Sibtain et al. 2007) that HCQ has a role for treating patients with erosive OA. One study (Saviola et al. 2012) showed that clodronate was superior to HCQ in treating erosive OA, but this study was limited by discontinued enrolment and high degree of dropout. It was worth noting that in this study, all RF-positive OA patients were able to complete HCQ treatment. This leads to the question of whether RF-positive erosive OA patients represent a subpopulation in which HCQ would be of greater benefit. The only study done to date which specifically assessed HCQ in nodal OA found that it was not superior to acetaminophen or placebo (McKendry et al. 2001). Two recent RCTs (Jokar et al. 2013; Abou-Raya et al. 2014) (with a combined enrolment of 210) demonstrated benefit with HCQ vs. placebo in the treatment of knee OA, in contrast to an earlier study (Bonfante et al. 2008) (total n = 29) that showed improvement not greater than that with placebo.
Future studies of HCQ in OA should endeavour to enrol larger numbers of patients, clearly define groups of patients with erosive vs. nonerosive OA, and among those patients with erosive OA, clearly define groups of patients who are RF-positive vs. RF-negative. This will hopefully better delineate whether there is a subgroup of patients with OA in whom HCQ could be an effective therapy.
One study protocol for an upcoming investigation has been published (Kingsbury et al. 2013); this study aims to look at the role of HCQ in reducing pain and synovitis in patients with hand OA. The study will take 252 patients with symptomatic hand OA who either have inadequate response or toxicity with conventional analgesics. Patients will be randomised to either placebo or 200–400 mg HCQ daily. RF and anti-CCP serology will be obtained at baseline. The primary outcome will be an averaged hand pain severity score, assessed at 0, 3, 6, and 12 months. Secondary outcomes include ultrasound assessment of synovitis, and findings from bilateral hand X-ray. The results of this study should better delineate whether HCQ is an effective treatment for the pain and synovitis associated with OA and, interestingly, whether HCQ offers any long-term structural benefit in patients with OA. Another prospective study (OA-TREAT) is proposed by an investigator-led German-based group in a randomised (in a ratio of 1:1) double-blind investigation in a total of 510 patients comprising a relatively subset or erosive hand OA; these patients will receive either 400 or 200 mg HCQ or placebo (Detert et al. 2014).
Complications of rheumatic diseases
Since RA and other rheumatic patients are at risk of developing cardiovascular disease as a result of their disease: as well as from intake of COX-2 inhibitory NSAIDs (McGettigan and Henry 2006; Padol and Hunt 2010); as well as from complications from diabetes mellitus (Neil et al. 2008; Wolfe and Michaud 2008): there would seem to be a good case for investigation of the long-term benefits of HCQ in preventing thrombotic events and complications from diabetes mellitus in patients with RA as well as other rheumatic diseases (Cansu and Korkmaz 2008). A more recent study of glycaemic control in women with RA or SLE demonstrated that patients treated with HCQ had lower fasting glucose levels than those not receiving HCQ (Hage et al. 2014), leading to the conclusion that HCQ may be beneficial in reducing the risk of cardiovascular disease which is known to be a significant factor contributing to premature mortality in these patients (Penn et al. 2010).
Uses in other rheumatic disease states
With the enormous spectrum of mechanisms of action that can reduce inflammation, it is not suprising that these agents are also used in many other rheumatic diseases including dermatomyositis (Woo et al. 1984; Stringer et al. 2010), inflammatory osteoarthritis (Bryant et al. 1995) and seronegative arthritis (Gladman et al. 1992).
Drug toxicity
The 4-amino anti-malarials remain one of the safest classes of antirheumatic drugs. HCQ is better tolerated than chloroquine, but nausea, vomiting, diarrhoea and abdominal bloating with cramping are among the most common reasons for discontinuing these drugs. The adverse effects that have been observed in patients with rheumatic conditions are summarised in Table 6. Other rarer side effects include myopathy, cardiomyopathy, psychosis, deafness, nervousness, rashes, an increase in skin pigment, bleaching of hair and alopecia (Meller et al. 2008; Ben-Zvi et al. 2012). Rare conditions such as toxic epidermal necrolysis do not appear to have been reported very often but complications such as concomitant use of other high risk medications (NSAIDs, anti-convulsants and sulphonamides) need to be considered (Cameron et al. 2014).
There are various eye pathologies that can occur as a complication of these drugs including corneal deposits, which are more common with CQ, and cause patients to see halos around lights, but it is the rare retinopathy, which gives the greatest cause for concern (Hobbs et al. 1959; Shearer and Dubois 1967; Das et al. 2007; Hanna et al. 2008; Tehrani et al. 2008; Ruiz-Irastorza et al. 2010; Jover et al. 2012; Geamănu-Pancă et al. 2014). This is because the retinopathy leads to vision loss, and frequently is irreversible even after discontinuing the drug and in some cases can even progress, long after the medication has been discontinued (Wei et al. 2001). Previous studies have shown that the retinal toxicity is directly related to the total dose of drug exposure and the current recommendations are to keep the daily dose of HCQ to 6 mg/kilogram body weight and chloroquine to 4 mg/kilogram body weight, or less, if at all possible [Marmor et al. 2002) and the total drug dosage to less than 200 g (Grierson 1997). Patients are recommended to get eye examinations, with visual fields’ examination every 6 months (Marmor et al. 2002; Easterbrook 2002). Some recent reports in the ophthalmological literature, however, suggest that annual or even biennial examinations are adequate, but the persistence of the tissue deposition of these drugs is so long that patients will continue to be exposed to the toxic effects of these drugs for months or even years after the drugs are discontinued, so it is vital to stop these drugs as soon as any retinal changes are observed. Rarer ocular conditions such as the occurrence of conjunctival rheumatoid nodule (Kheirkhah et al. 2012) mean that there must be careful and thorough examination of the eye in patients with RA that are being treated with anti-malarials.
In recent years, there have been instrumental procedures devised to improve the detection of early stages of retinopathy. These include full-field and multifocal electro-retinography (Tzekov 2005; Nebbioso et al. 2011) and microperimetry (Martínez-Costa et al. 2013). The latter technique has been found to lead to sensitive detection of retinal changes in the elderly who seem to be more prone to retinopathy (Martínez-Costa et al. 2013).
One of the complicating factors is the gradual appearance of renal insufficiency, particularly in the patient with SLE as it is known that discontinuing CQ or HCQ in lupus patients can exacerbate the disease, and this can lead to additional renal disease. Reducing the dosage and the frequency of administration of the drug with careful frequent monitoring for eye toxicity can be tried in an attempt to allow the patient to stay on the anti-malarial drug.
Conclusions
The 4-aminoquinolone drugs are some of many drugs used for years to treat malaria. Fortuitously, CQ and HCQ were discovered to be useful in the treatment of rheumatic diseases, particularly RA and SLE. These drugs are now being used to treat other rheumatic diseases including Sjögren’s Syndrome, phospholipid antibody (aPL) syndrome, dermatomyositis and inflammatory osteoarthritis. They are some of the better tolerated and less toxic anti-rheumatic drugs. The irreversible retinopathy leading to vision loss is of major concern but HCQ is associated with lower risk of retinopathy as compared to CQ, and the incidence of retinopathy has declined with better understanding of the dosage factors that contribute to this toxicity and regular ophthalmological evaluations. Our understanding of the many mechanisms of action of this class of drug has improved considerably in the last few decades and with it therapeutic horizons have expanded. These versatile drugs are extremely useful for managing a variety of rheumatic disease and a better understanding of the properties of this class of drugs may lead to the development of new agents or continue the expansion of clinical indications for the old ones.
References
Abdel-Hamid H, Oddis CV, Lacomis D (2008) Severe hydroxychloroquine myopathy. Muscle Nerve 38:1206–1210
Abou-Raya S et al. (2014) Efficacy of hydroxychloroquine in the treatment of symptomatic knee osteoarthritis in older adults: a randomized placebo-controlled trial. Ann Rheum Dis 73:756–757
Acha-Orbea H, Groscurth P, Lang R, Stitz J, Hengartner H (1983) Characterization of cloned cytotoxic lymphocytes with NK-like activity. J Immunol 130:2952–2959
Achuthan S, Ahluwalia J, Shafig N, Pareek A, Chandurkar N, Malhotra S (2015) Hydroxychloroquine’s efficacy as an antiplatelet agent study in healthy volunteers: a proof of concept study. J Cardiovasc Pharmacol Ther 20:174–180
Ackerman NR, Jubb S, Marlowe SL (1981) Effects of various anti-inflammatory and anti-rheumatic agents on the synthesis, secretion and activity of a cartilage proteoglycan-degrading enzyme and other macrophage enzymes. Biochem Pharmacol 30:2147–2155
Adams EM, Yocum DE, Bell CL (1983) Hydroxychloroquine in the treatment of rheumatoid arthritis. Am J Med 75:321–326
Adedoyin A, Frye RF, Mauro K, Branch RA (1998) Chloroquine modulation of specific metabolizing enzymes activities: investigation with selective five drug cocktail. Br J Clin Pharmacol 46:215–219
Aderounmu AF, Fleckstein L (1983) Pharmacokinetics of chloroquine diphosphate in the dog. J Pharmacol Exp Ther 1983(223):633–639
Adeyemi EO, Chadwick VS, Hodgson HJ (1990) The effect of some anti-inflammatory agents on elastase release from neutrophils in vitro. J Pharm Pharmacol 42:487–490
Adjepon-Yamoah KK, Woolhouse NM, Prescott LF (1986) The effect of chloroquine on paracetamol disposition and kinetics. Br J Clin Pharmacol 21:322–324
Akintonwa A, Gbajumo SA, Mabadeje AF (1988) Placental and milk transfer of chloroquine in humans. Ther Drug Monit 10:147–149
Ali HM (1985) Reduced ampicillin bioavailability following oral coadministration with chloroquine. J Antimicrob Chemother 15:781–784
Alisky JM, Chertkova EL, Iczkowski KA (2006) Drug interactions and pharmacogenetic reactions are the basis for chloroquine and mefloquine-induced psychosis. Med Hypotheses 67:1090–1094
Andreas K, Haupl T, Lubke C, Ringe J, Morawietz L, Wachtel A, Sittinger M, Kaps C (2009) Antirheumatic drug response signatures in human chondrocytes: potential molecular targets to stimulate cartilage regeneration. Arthritis Res Ther 11:R15
Antoine JC, Goud B, Jouanne C, Maurice M, Feldmann G (1985) Ammonium chloride, methylamine and chloroquine reversibly inhibit antibody secretion by plasma cells. Cell Biol 55:41–54
Arner EC, Darnell LR, Pratta MA, Newton RC, Ackerman NR, Galbraith W (1987) Effect of antiinflammatory drugs on human interleukin-1-induced cartilage degradation. Agents Actions 21:334–336
Ashraf T, Jiang W, Hogue MT, Henderson J, Wu C, Bendayan R (2014) Role of anti-inflammatory compounds in human immunodeficiency virus-1 glycoprotein120-mediated brain inflammation. J Neuroinflamm 11:11. doi:10.1186/1742-2094-11
Ausiello CM, Barbieri P, Spagnoli GC, Ciompi ML, Casciani CU (1986) In vivo effects of chloroquine treatment on spontaneous and interferon-induced natural killer activities in rheumatoid arthritis patients. Clin Exp Rheumatol 4:255–259
Authi KS, Traynor JR (1982) Stimulation of polymorphonuclear leucocyte phospholipase A2 activity by chloroquine and mepacrine. J Pharm Pharmacol 34:736–738
Avina-Zubieta JA, Galindo-Rodriguez G, Newman S, Suarez-Almazor ME, Russell AS (1998) Long-term effectiveness of antimalarial drugs in rheumatic diseases. Ann Rheum Dis 57:582–587
Bannwarth B, Pehourcq F, Schaeverbeke T, Dehais J (1996) Clinical pharmacokinetics of low-dose pulse methotrexate in rheumatoid arthritis. Clin Pharmacokinet 30:194–210
Barbieri P, Ausiello C, Spagnoli GC, Qintieri F, Ciompi ML (1985) Chloroquine treatment induces decrease of spontaneous and interferon enhanced NK activity in rheumatoid arthritis. Int J Immunother 1:211–214
Bartholomew JS, Lowther DA (1987) Receptor-mediated binding of leukocyte elastase by chondrocytes. Arthritis Rheum 30:431–438
Baum J (1983) Treatment of juvenile arthritis. Am Fam Physician 27:133–139
Bellamy N, Brooks PM (1986) Current practice in antimalarial drug prescribing in rheumatoid arthritis. J Rheumatol 13:551–555
Ben-Chetrit E, Fischel R, Hinz B, Levy M (2005) The effects of cochicine and hydroxychloroquine on the cyclo-oxygenases COX-1 and COX-1. Rheumatol Int 25:332–335
Ben-Zvi I, Kivity S, Langevitz P, Shoenfeld Y (2012) Hydroxychloroquine: from malaria to autoimmunity. Clin Rev Allergy Immunol 42:145–153
Bergqvist Y, Hed C, Funding L, Suther A (1985) Determination of chloroquine and its metabolites in urine: a field method based on ion-pair extraction. Bull WHO 63:893–898
Biasi D, Caramaschi P, Carletto A, Pacor ML, Bambara LM (2000) Combination therapy with hydroxychloroquine, gold sodium thiomalate and methotrexate in early rheumatoid arthritis. An open 3-year study. Clin Rheumatol 19:505–507
Blackham A, Radziwonik H, Shaw IH (1975) The Arthus reaction in guinea-pig knee joints. A test for anti-inflammatory drugs. Agents Actions 5:519–527
Boelaert JR, Piette J, Sperber K (2001a) The potential place of chloroquine in the treatment of HIV-1-infected patients. J Clin Virol 20:137–140
Boelaert JR, Yaro S, Augustijns P, Meda N, Schneider YJ, Schols D, Mols R, De Laere EA, Van de Perre P (2001b) Chloroquine accumulates in breast-milk cells: potential impact in the prophylaxis of postnatal mother-to-child transmission of HIV-1. AIDS 15:2205–2207
Bonfante H et al. (2008) Assessment of the use of hydroxychloroquine on knees’ osteoarthritis treatment. Rev Bras Rheumatol 48:208–212
Borden MB, Parke AL (2001) Antimalarial drugs in systemic lupus erythematosus: use in pregnancy. Drug Saf 24:1055–1063
Boström H, Moretti A, Whitehouse M (1963) Studies of the biochemistry of heart valves. On the biosynthesis of mucopolysaccharides in bovine heart valves. Biochem Biophys Acta 74:213–221
Boström H, Bernsten K, Whitehouse MW (1964) Biochemical properties of anti-inflammatory drugs-II. Some effects on sulphate-35S metabolism in vivo. Biochem Pharmacol 13:413–420
Brandriss MW, Schlesinger JJ (1984) Antibody-mediated infection of P388D1 cells with 17D yellow fever virus: effects of chloroquine and cytochalasin B. J Gen Virol 65:791–794
Brennan FR, Negroiu G, Buzás EI, Fülöp C, Holló K, Mikecz K, Glant TT (1995) Presentation of cartilage proteoglycan to a T cell hybridoma derived from a mouse with proteoglycan-induced arthritis. Clin Exp Immunol 100:104–110
Bretano F, Schorr O, Gay RE, Gay S, Kyburz D (2005) RNA released from necrotic synovial fluid in RA—evidence of an inhibitory effect on toll-like receptor signalling. Arthritis Rheum 52:2656–2665
British National Formulary 57 (2009) BMJ Group and RPS Publishing, London, p 566
Brocks DR, Mehvar R (2003) Stereoselectivity in the pharmacodynamics and pharmacokinetics of the chiral antimalarial drugs. Clin Pharmacokinet 42:1359–1382
Brocks DR, Pasutto FM, Jamali F (1992) Analytical and semi-preparative high-performance liquid chromatographic separation and assay of hydroxychloroquine enantiomers. J Chromatogr 581:83–92
Brown ND, Poon BT, Chulay JD (1985) Chloroquine metabolism in man: urinary excretion of 7-chloro-4-hydroxy-quinoline and 7-chloro-4-aminoquinoline metabolites. J Chromatogr 345:209–214
Brucato A, Frassi M, Franceschini F, Cimaz R, Faden D, Pisoni MP, Muscarà M, Vignati G, Stramba-Badiale M, Catelli L, Lojacono A, Cavazzana I, Ghirardello A, Vescovi F, Gambari PF, Doria A, Meroni PL, Tincani A (2001) Risk of congenital complete heart block in newborns of mothers with anti-Ro/SSA antibodies detected by counter-immunoelectrophoresis: a prospective study of 100 women. Arthritis Rheum 44:1832–1835
Bryant LR et al. (1995) Hydroxychloroquine in the treatment of erosive osteoarthritis. J Rheumatol 22:1527–1531
Bygbjerg IC, Theander TG, Andersen BJ, Flachs H, Jepsen S, Larsen PB (1986) In vitro effect of chloroquine, mefloquine and quinine on human lymphocyte proliferative responses to malaria antigens and other antigens/mitogens. Trop Med Parasit 37:245–247
Bygbjerg IC, Svenson M, Theander TG, Bendtzen K (1987) Effect of antimalarial drugs on stimulation and interleukin 2 production of human lymphocytes. Int J Immunopharmacol 9:513–519
Cameron MC, Word AP, Dominguez A (2014) Hydroxychloroquine-induced fatal toxic epidermal necrolysis complicated by angioinvasive rhizopus. Dermatol Online J 20 (pii: 13030/qt1q90q0h5)
Canadian Rheumatology Association (2000) Canadian Consensus Conference on hydroxychloroquine. J Rheumatol 27:2919–2921
Cankaya H, Alpöz E, Karabulut G, Güneri P, Boyacioglu H, Kabasakal Y (2010) Effects of hydroxychloroquine on salivary flow rates and oral complaints of Sjögren patients: a prospective sample study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110:62–67
Cansu DU, Korkmaz C (2008) Hypoglycaemia induced by hydroxychloroquine in a non-diabetic patient treated for RA. Rheumatology (Oxford) 47:378–379
Carmichael SJ, Beal J, Day RO, Tett SE (2002) Combination therapy with methotrexate and hydroxychloroquine for rheumatoid arthritis increases exposure to methotrexate. J Rheumatol 29:2077–2083
Carmichael SJ, Charles B, Tett SE (2003) Population pharmacokinetics of hydroxychloroquine in patients with rheumatoid arthritis. Ther Drug Monit 25:671–681
Carmichael SJ, Day RO, Tett SE (2013) A cross-ectional survey of hydroxychloroquine concentrations and effects in people with systemic lupus erythematosus. Intern Med J 43:547–553
Cecchi E, Porzio F (1964) Affinité de l-hydroxychloroquine pour les tissues articulaires. Rhumatologie 16:399–400
Cervera R, Khamashta MA, Hughes GR (2009) The Euro-lupus project: epidemiology of systemic lupus erythematosus in Europe. Lupus 18:869–874
Chafin CB, Regna NL, Hammanod SE, Reilly CM (2013) Cellular and urinary microRNA alterations in NZB/W mice with hydroxychloroquine and prednisone treatment. Int Immunopharmacol 17:894–906
Chiang G, Sassaroli M, Louie M, Chen H, Stecher VJ, Sperber K (1996) Inhibition of HIV-1 replication by hydroxychloroquine: mechanism of action and comparison with zidovudine. Clin Ther 18:1080–1092
Choi HK, Seeger JD, Kuntz KM (2000) A cost-effectiveness analysis of treatment options for patients with methotrexate-resistant rheumatoid arthritis. Arthritis Rheum 43:2316–2327
Churchill FC, Mount DL, Schwartz IK (1983) Determination of chloroquine and its major metabolite in blood using perfluoroacylation followed by fused-silica capillary gas chromatography with nitrogen-sensitive detection. J Chromatogr 274:111–120
Clarke AK (1998) Antimalarial drugs in the treatment of rheumatological diseases. Br J Rheumatol 37:580
Clarke AK, Vernon-Roberts B, Currey HLF (1975) Assessment of anti-inflammatory drugs in the rat using subcutaneous implants of polyurethane foam impregnated with dead tubercule bacilli. Ann Rheum Dis 34:326–331
Clegg DO, Dietz F, Duffy J, Willkens RF, Hurd E, Germain BF, Wall B, Wallace DJ, Bell CL, Sleckman J (1997) Safety and efficacy of hydroxychloroquine as maintenance therapy for rheumatoid arthritis after combination therapy with methotrexate and hydroxychloroquine. J Rheumatol 24:1896–1902
Colombo C, Butler M, Hickman L, Selwyn M, Chart J, Steinetz B (1983) A new model of osteoarthritis in rabbits. II. Evaluation of anti-osteoarthritic effects of selected antirheumatic drugs administered systemically. Arthritis Rheum 26:1132–1139
Combe B, Guttierrez M, Anaya JM, Sany J (1993) Possible efficacy of hydroxychloroquine on accelerated nodulosis during methotrexate therapy for rheumatoid arthritis. J Rheumatol 20:755–756
Conaghan PG, Lehmann T, Brooks P (1997) Disease-modifying antirheumatic drugs. Curr Opin Rheumatol 9:183–190
Connolly KM, Stecher VJ, Danis E, Pruden DJ, LaBrie T (1988) Alteration of interleukin-1 activity and the acute phase response in adjuvant arthritic rats treated with disease modifying antirheumatic drugs. Agents Actions 25:94–105
Cook JA, Randinitis EJ, Bramson CR, Wesche DL (2006) Lack of a pharmacokinetic interaction between azithromycin and chloroquine. Am J Trop Med Hyg 74:407–412
Costedoat-Chalumeau N, Amoura Z, Aymard G, Le TH, Wechsler B, Vauthier D, Dermer ME, Darbois Y, Piette JC (2002) Evidence of transplacental passage of hydroxychloroquine in humans. Arthritis Rheum 46:1123–1124
Costedoat-Chalumeau N, Amoura Z, Duhaut P, Huong DL, Sebbough D, Wechsler B, Vauthier D, Denjoy I, Lupoglazoff JM, Piette JC (2003) Safety of hydroxychloroquine in pregnant patients with connective tissue diseases: a study of one hundred thirty-three cases compared with a control group. Arthritis Rheum 48:3207–3211
Cowey FK, Whitehouse MW (1966) Biochemical properties of anti-inflammatory drugs. VII. Inhibition of proteolytic enzymes in connective tissue by chloroquine (resorchin) and related antimalarial antirheumatic drugs. Biochem Pharmacol 15:1071–1084
Cox A, Duff GW (1996) Cytokines as genetic modifying factors in immune and inflammatory diseases. J Pediatric Endocrinol Metab 9:129–132
Craig JC, Bhargava HN, Everhart ET, LaBelle B, Ohnsorge U, Webster RV (1988) Absolute configuration of the enantiomers of 7-chloro-4-[[4-diethylamino)-1-methylbutyl]amino]quinoline (chloroquine). J Org Chem 53:1167–1170
Crossley MJ, Spowage M, Hunneyball IM (1987) Studies on the effects of pharmacological agents on antigen-induced arthritis in BALB/c mice. Drugs Exp Clin Res 13:273–277
Csuka M, Carrera GF, McCarty DJ (1986) Treatment of intractable rheumatoid arthritis with combined cyclophosphamide, azathioprine, and hydroxychloroquine. A follow-up study. JAMA 255:2315–2319
Cutler DJ (1993) Possible mechanisms of action of antimalarials in rheumatic disease. Agents Actions Suppl 44:139–143
Cutler DJ, MacIntyre AC, Tett SE (1988) Pharmacokinetics and cellular uptake of 4-aminoquinoline antimalarials. Agents Actions Suppl 24:142–157
Das SK, Pareek A, Mathur DS, Wanchu A, Srivastava R, Agarwal GG, Chauhan RS (2002) Efficacy and safety of hydroxychloroquine sulphate in rheumatoid arthritis: a randomized, double-blind, placebo controlled clinical trial—an Indian experience. Curr Med Res Opin 23:2227–2234
Das SK, Pareek A, Mathur DS, Wanchu A, Srivastava R, Agarwal GG, Chauhan RS (2007) Efficacy and safety of hydroxychloroquine sulphate in rheumatoid arthritis: a randomized, double-blind, placebo controlled clinical trial–an Indian experience. Curr Med Res Opin 23:2227–2234
Davila L, Ranganathan P (2011) Pharmacogenetics: implications for therapy in rheumatic diseases. Nat Rev Rheumatol 7:537–550
Davis MJ, Woolf AD (1996) Role of antimalarials in rheumatoid arthritis–the British experience. Lupus 5(Suppl 1):S37–S40
Dawson LJ, Caulfield VL, Stanbury JB, Field AE, Christmas SE, Smith PM (2005) Hydroxychloroquine therapy in patients with primary Sjögren’s syndrome may improve salivary gland hypofunction by inhibition of glandular cholinesterase. Rheumatology 44:449–455
Detert J, Klaus P, Listing J, Höhne-Zimmer V, Braun T, Wassenberg S, Rau R, Buttgereit F, Burmester GR (2014) Hydroxychloroquine in patients with inflammatory and erosive osteoarthritis of the hands (OA TREAT): study protocol for a randomized controlled trial. Trials 15:412. doi:10.1186/1745-6215-15-412
De Duve C (1965) The separation and characterization of subcellular particles. Harvey Lect 59:49–87
de Oliveira AR, Cardoso CD, Bonato PS (2007) Stereoselective determination of hydroxychloroquine and its metabolites in human urine by liquid-phase microextraction and CE. Electrophoresis 28:1081–1091
Derksen RH, de Groot PG (2010) Towards evidence-based treatment of thrombotic antiphospholipid syndrome. Lupus 19:470–474
Descloux E, Durieu I, Cochat P, Vital-Durand D, Ninet J, Fabien N, Cimaz R (2009) Influence of age at disease onset in the outcome of paediatric systemic lupus erythematosus. Rheumatology 48:779–784
Dixon JS, Pickup ME, Bird HA, Lee MR (1981) Biochemical indices of response to hydroxychloroquine and sodium aurothiomalate in rheumatoid arthritis. Ann Rheum Dis 40:480–488
Dubois EL (1967) Management and prognosis of systemic lupus erythematosus. Bull Rheum Dis 18:477–482
Dubois EL (1978) Antimalarials in the management of discoid and systemic lupus erythematosus. Semin Arthritis Rheum 8:33–51
Ducharme J, Farinotti R (1996) Clinical pharmacokinetics and metabolism of chloroquine. Focus on recent advancements. Clin Pharmacokinet 31:257–274
Ducharme J, Fieger H, Ducharme MP, Khalil SK, Wainer IW (1995) Enantioselective disposition of hydroxychloroquine after a single oral dose of the racemate to healthy subjects. Br J Clin Pharmacol 40:127–133
Duve De, Wattiaux R, Wibo M (1962) Effects of fat-soluble compounds on lysosomes in vitro. Biochem Pharmacol 9:97–116
Easterbrook M (1990) Is corneal disposition of anti-malarials any indication of retinal toxicity? Can J Opthal 25:249–251
Easterbrook M (2002) Screening for antimalarial toxicity: current concepts. Can J Ophthalmol. 37:325–358 (331–334)
Edmead CE, Patel YI, Wilson A, Boulougouris G, Hall ND, Ward SG, Sansom DM (1996) Induction of activator protein (AP)-1 and nuclear factor-κB by CD28 stimulation involves both phosphoinositol-3-kinase and acidic sphingomyelinase signals. J Immunol 157:3290–3297
Edstein MD, Veenendaal JR, Newman K, Hyslop R (1986) Excretion of chloroquine, dapsone and pyrimethamine in human milk. Br J Clin Pharmacol 22:733–735
Edwards MH, Pierangeli S, Liu XW, Barker JH, Anderson G, Harris EN (1997) Hydroxychloroquine reverses thrombogenic properties of antiphospholipid antibodies in mice. Circulation 96:4380–4384
Eklund KK, Leirisalo-Repo M, Ranta P, Mäki T, Kautiainen H, Hannonen P, Korpela M, Hakala M, Järvinen P, Möttönen T (2007) Serum IL-1beta levels are associated with the presence of erosions in recent onset rheumatoid arthritis. Clin Exp Rheumatol 25:684–689
Emami J, Pasutto FM, Jamali F (1998) Effect of experimental diabetes mellitus and arthritis on the pharmacokinetics of hydroxychloroquine enantiomers in rats. Pharm Res 15:897–903
Emami J, Gerstein HC, Pasutto FM, Jamali F (1999a) Insulin-sparing effect of hydroxychloroquine in diabetic rats is concentration dependent. Can J Physiol Pharmacol 77:118–123
Emami J, Pasutto FM, Mercer JR, Jamali F (1999b) Inhibition of insulin metabolism by hydroxychloroquine and its enantiomers in cytosolic fraction of liver homogenates from healthy and diabetic rats. Life Sci 64:325–335
Estrada C, Gómez C, Martin C, Moncada S, González C (1992) Nitric oxide mediates tumor necrosis factor-α cytotoxicity in endothelial cells. Biochem Biophys Res Commun 186:475–482
Etherington DJ, Pugh D, Silver IA (1981) Collagen degradation in an experimental inflammatory lesion: studies on the role of the macrophage. Acta Biol Med Ger 40:1625–1636
Ette EI, Brorm-Awala EA, Essien EE (1987a) Effect of ranitidine on chloroquine disposition. Drug Intell Clin Pharm 21:732–734
Ette EI, Essien EE, Ogonor JI, Brown-Awala EA (1987b) Chloroquine in human milk. J Clin Pharmacol 27:499–502
Ette EI, Brown-Awala EA, Essien EE (1987c) Chloroquine elimination in humans: effect of low-dose cimetidine. J Clin Pharmacol 27:813–816
Evans D, Williamson WRN (1987) Chemistry of clinically active anti-inflammatory compounds. In: Williamson WRN (ed) Anti-inflammatory compounds. Marcel Dekker, New York, pp 193–302
Famaey JP, Fontaine J (1980) Prevention by chloroquine of hexosamine cartilage depletion by E-prostaglandins. Arthritis Rheum 23:780–781
Farrante A, Rowan-Kelly B, Seow WK, Thong YH (1986) Depression of human polymorphonuclear leucocyte function by anti-malarial drugs. Immunology 58:125–130
Finbloom DS, Silver K, Newsome DA, Gunkel R (1985) Comparison of hydroxychloroquine and chloroquine use and the development of retinal toxicity. J Rheumatol 12:692–694
Fosdyke DR (1975) Evidence for a relationship between chloroquine and complement from studies with lymphocyte mitogens: possible implications for the mechanism of chloroquine in disease. Can J Microbiol 21:1581–1586
Fox RI (1993) Mechanism of action of hydroxychloroquine as an antirheumatic drug. Semin Arthritis Rheum 23:82–91
Fox R (1996) Anti-malarial drugs: possible mechanisms of action in autoimmune disease and prospects for drug development. Lupus 5(Suppl 1):S4–S10
Fox RI, Dixon R, Guarrasi V, Krubel S (1996) Treatment of primary Sjogren’s syndrome with hydroxychloroquine: a retrospective, open-label study. Lupus 5(Suppl 1):S31–S36
French JK, Hurst NP, O’Donnell ML, Betts WH (1987) Uptake of chloroquine and hydroxychloroquine by human blood leucocytes in vitro: relation to cellular concentrations during antirheumatic therapy. Ann Rheum Dis 46:42–45
Fryauff DJ, Richards AL, Baird JK, Richie TL, Mouzin E, Tjitra E, Sutamihardja MA, Ratiwayanto S, Hadiputranto H, Larasati RP, Pudjoprawoto N, Subianto B, Hoffman SL (1996) Lymphocyte proliferative response and subset profiles during extended periods of chloroquine or primaquine prophylaxis. Antimicrob Agents Chemother 40:2737–2742
Fu S, Björkman A, Wåhlin B, Ofori-Adjei D, Ericsson O, Sjöqvist F (1986) In vitro activity of chloroquine, the two enantiomers of chloroquine, desethylchloroquine and pyronaridine against Plasmodium falciparum. Br J Clin Pharmacol 22:93–96
Fulkerson JP, Ladenbauer-Bellis IM, Chrisman OD (1979) In vitro hexosamine depletion of intact articular cartilage by E-prostaglandins: prevention by chloroquine. Arthritis Rheum 22:1117–1121
Furst DE (1993) Optimizing combination chemotherapy for rheumatoid arthritis. Ann N Y Acad Sci 696:285–291
Furst DE (1996) Pharmacokinetics of hydroxychloroquine and chloroquine during treatment of rheumatic diseases. Lupus 5(Suppl 1):S11–S15
Furst DE, Lindsley H, Baethge B, Botstein GR, Caldwell J, Dietz F, Ettlinger R, Golden HE, McLaughlin GE, Moreland LW, Roberts WN, Rooney TW, Rothschild B, Sack M, Sebba AI, Weisman M, Welch KE, Yocum D (1999) Dose-loading with hydroxychloroquine improves the rate of response in early, active rheumatoid arthritis: a randomized, double-blind six-week trial with eighteen-week extension. Arthritis Rheum 42:357–365
Gallus AS (1979) Antiplatelet drugs: clinical pharmacology and therapeutic use. Drugs 18:439–477
Geamănu-Pancă A, Popa-Cheracheanu A, Marinescu B, Geamănu CD, Voinea LM (2014) Retinal toxicity associated with chronic exposure to hydroxychloroquine and its ocular screening. Review. J Med Life 7:322–326
Gendrel D, Verdier F, Richard-Lenoble D, Nardou M (1990) Interaction of cholestyramine and chloroquine. Arch Fr Pediatr 47:387–388
Gerstein HC, Thorpe KE, Taylor DW, Haynes RB (2002) The effectiveness of hydroxychloroquine in patients with type 2 diabetes mellitus who are refractory to sulfonylureas—a randomized trial. Diabetes Res Clin Pract 55:209–219
Gil JP, Gil Berglund E (2007) CYP2C8 and antimalarial drug efficacy. Pharmacogenomics 8:187–198
Ginsburg H, Geary TG (1987) Current concepts and new ideas on the mechanism of action of quinoline-containing antimalarials. Biochem Pharmacol 36:1567–1576
Girart MV, Fuertes MB, Domaica CI, Rossi LE, Zwirner NW (2007) Engagement of TLR3, TLR7, and NKG2D regulate IFN-gamma secretion but not NKG2D-mediated cytotoxicity by human NK cells stimulated with suboptimal doses of IL-12. J Immunol 179:3472–3479
Gladman DD, Blake R, Brubacher B, Farewell VT (1992) Chloroquine therapy in psoriatic arthritis. J Rheumatol 19:1724–1726
Glaumann H, Ahlberg J, Berkenstam A (1985) Rapid isolation of rat liver secondary lysosomes—autophagic vacuoles—following chloroquine administration. Exp Cell Res 163:151–158
Goekoop YP, Allaart CF, Breedveld FC, Dijkmans BA (2001) Combination therapy in rheumatoid arthritis. Curr Opin Rheumatol 13:177–183
Goldman FD, Gilman AL, Hollenback C, Kato RM, Premack BA, Rawlings DJ (2000) Hydroxychloroquine inhibits calcium signals in T cells: a new mechanism to explain its immunomodulatory properties. Blood 95:3460–3466
Gordon D, Lewis GP (1984) Effects of piroxicam on mononuclear cells. Comparison with other antiarthritic drugs. Inflammation 8(Suppl):S87–S102
Gottenberg JE, Ravaud P, Puéchal X, Le Guern V, Sibilia J, Goeb V, Larroche C, Dubost JJ, Rist S, Saraux A, Devauchelle-Pensec V, Morel J, Hayem G, Hatron P, Perdriger A, Sene D, Zarnitsky C, Batouche D, Furlan V, Benessiano J, Perrodeau E, Seror R, Mariette X (2014) Effects of hydroxychloroquine on symptomatic improvement in primary Sjögren syndrome: the JOQUER randomized clinical trial. JAMA 312:249–258
Gräbner R, Meerbach W (1983) Imipramine and chloroquine induce alterations in phospholipid content of rat lung. Exp Path 24:253–259
Grierson DJ (1997) Hydroxychloroquine and visual screening in a rheumatology outpatient clinic. Ann Rheum Dis 56:188–190
Gupta JD, Gruca M, Ablett W (1979) Effect of other drugs and chemicals on the degradation of aspirin in vitro: possible extrapolation to in vivo metabolism of aspirin. Eur J Drug Metab Pharmacokinet 4:103–108
Haberkorn A, Kraft HP, Blaschke G (1979) Antimalarial activity of the optical isomers of chloroquine diphosphate. Tropenmed Parasitol 30:308–312
Hage MP, Al-Badri MR, Azar ST (2014) A favourable effect of hydroxychloroquine on glucose and lipid metabolism beyond its anti-inflammatory role. Ther Adv Endocronol Metab 5:77–85
Hanna B, Holdeman NR, Tang RA, Schiffman JS (2008) Retinal toxicity secondary to Plaquenil therapy. Optometry 79:90–94
Hedin U, Thyberg J (1985) Receptor-mediated endocytosis of immunoglobulin-coated colloidal gold particles in cultured mouse peritoneal macrophages. Chloroquine and monensin inhibit transfer of the ligand from endocytic vesicles to lysosomes. Eur J Cell Biology 39:130–135
Hereng T, Lambert M, Hachulla E, Samor M, Dubucquoi S, Caron C, Launay D, Morell-Dubois S, Queyrel V, Hatron PY (2008) Influence of aspirin on the clinical outcomes of 103 anti-phospholipid antibodies-positive patients. Lupus 17:11–15
Hobbs HE, Sorsby A, Freeman A (1959) Retinopathy following chloroquine therapy. Lancet 2:478–480
Homewood CA, Warhurst DC, Peters W, Baggaly VC (1972) Lysosomes, pH and the anti-malarial action of chloroquine. Nature 235:50–52
Hostetler KY, Richman DD (1982) Studies on the mechanism of phospholipid storage induced by amantadine and chloroquine in Madin Darby canine kidney cells. Biochem Pharmacol 31:3795–3799
Hugosson E, Bjökman A, Troye-Blomberg M (2002) Chloroquine enhances the number of IL-10 producing cells and the expression of B7-2 and ICAM in in vitro-cultured PBMC. Scan J Immunol 55:399–402
Hunneyball IM, Crossley MJ, Spowage M (1986) Pharmacological studies of antigen-induced arthritis in BALB/c mice. II. The effects of second-line antirheumatic drugs and cytotoxic agents on the histopathological changes. Agents Actions 18:394–400
Hurst NP, French JK, Gorjatsschko L, Betts WH (1987) Studies on the mechanism of inhibition of chemotactic tripeptide stimulated human neutrophil polymorphonuclear leucocyte superoxide production by chloroquine and hydroxychloroquine. Ann Rheum Dis 46:750–756
Hurst NP, French JK, Gorjatschko L, Betts WH (1988) Chloroquine and hydroxychloroquine inhibit multiple sites in metabolic pathways leading to neutrophil superoxide release. J Rheumatol 15:23–27
Hurvitz D, Hurschhorn K (1965) Suppression of in vitro lymphocyte responses by chloroquine. New Engl J Med 273:23–26
Ignarro LJ (1971) Dissimilar effects of anti-inflammatory drugs on stability of lysosomes from peritoneal and circulating leukocytes and liver. Biochem Pharmacol 20:2861–2870
Ignarro LJ (1974) Release of neutral protease and beta-glucuronidase from human neutrophils in the presence of cartilage treated with various immunologic reactants. J Immunol 113:298–308
Ignarro LJ, Colombo C (1972) Enzyme release from guinea-pig polymorphonuclear leucocyte lysosomes inhibited in vitro by anti-inflammatory drugs. Nat New Biol 239:155–157
Ilo EC, Orisakwe OE, Ilondu NA, Okwoli N, Brown SA, Elo-Ilo J, Agbasi PU (2006) Effect of chloroquine on the bioavailability of ciprofloxacin in man. J Control Release 116:e109–e110
Ilo CE, Ezejiofor NA, Agbakoba N, Brown SA, Maduagwuna CA, Agbasi PU, Orisakwe OE (2008) Effect of chloroquine on the urinary excretion of ciprofloxacin. Am J Ther 15:419–422
Iredale J, Fieger H, Wainer IW (1993) Determination of the stereoisomers of hydroxychloroquine and its major metabolites in plasma and urine following a single oral administration of racemic hydroxychloroquine. Semin Arthritis Rheum 23:74–81
Izmirly PM, Kim MY, Llanos C, Le PU, Guerra MM, Askanase AD, Salmon JE, Buyon JP (2010) Evaluation of the risk of anti-SSA/Ro-SSB/La antibody-associated cardiac manifestations of neonatal lupus in fetuses of mothers with systemic lupus erythematosus exposed to hydroxychloroquine. Ann Rheum Dis 69:1827–1830
Jang C-H, Choi J-H, Byun M-S, Jue D-M (2006) Chloroquine inhibits production of TNF-α, IL-1β and IL-6 from lipopolysaccharide-stimulated human monocytes/macrophages by different modes. Rheumatology 45:703–710
Järvinen K, Vuolteenaho K, Nieminen R, Moilanen T, Knowles RG, Moilanen E (2008) Selective iNOS inhibitor 1400 W enhances anti-catabolic IL-10 and reduces destructive MMP-10 in OA cartilage. Survey of the effects of 1400 W on inflammatory mediators produced by OA cartilage as etected by protein antibody array. Clin Exp Rheumatol 26:275–282
Jarzyna R, Kiersztan A, Lisowa O, Bryła J (2001) The inhibition of gluconeogenesis by chloroquine contributes to its hypoglycaemic action. Eur J Pharmacol 428:381–388
Jokar M et al. (2013) The effect of hydroxychloroquine on symptoms of knee osteoarthritis: a double-blind randomized controlled clinical trial. Iran J Med Sci 38(3):221–226
Jones CJP, Jayson MIV (1984) Chloroquine: its effect on leucocyte auto- and heterophagocytosis. Ann Rheum Dis 43:205–212
Jones CJP, Salisbury RS, Jayson MIV (1984) The presence of abnormal lysosomes in lymphocytes and neutrophils during chloroquine therapy: a quantitative ultrastructural study. Ann Rheum Dis 43:710–715
Jover JA, Leon L, Pato E, Loza E, Rosales Z, Matias MA, Mendez-Fernandez R, Díaz-Valle D, Benitez-Del-Castillo JM, Abasolo L (2012) Long-term use of antimalarial drugs in rheumatic diseases. Clin Exp Rheumatol 30:380–387
Julkunen H, Rokkanen P, Laine H (1976) Chloroquine treatment and bone changes in rheumatoid arthritis. Scand J Rheumatol 5:36–38
Jung H, Bobba R, Su J, Shariati-Sarabi Z, Gladman DD, Urowitz M, Lou W, Fortin PR (2010) The protective effect of antimalarial drugs on thrombovascular events in systemic lupus erythematosus. Arthritis Rheum 62:863–868
Kalmanson GM, Guze LB (1963) Effects of hydroxyl-chloroquine on immune mechanisms. Clin Res 11:106
Kamal M, Bassiouni M (1992) Chloroquine inhibits elastase enzyme activity in vitro. Clin Exp Rheumatol 10:99–104
Kamal MA, Jusko WJ (2004) Interactions of prednisolone and other immunosuppressants used in dual treatment of systemic lupus erythematosus in lymphocyte proliferation assays. J Clin Pharmacol 44:1034–1045
Kao KJ (1988) Selective elution of HLA antigens and β2-microglobulin from human platelets by chloroquine diphosphate. Transfusion 28:14–17
Kaplan MJ, Lewis EE, Shelden EA, Somers E, Pavlic R, McCune WJ, Richardson BC (2002) The apoptotic ligands, TRAIL, TWEAK, and Fas ligand mediate monocyte death induced by autologous lupus T cells. J Immunol 169:6020–6029
Karres I, Kremer JP, Dietl I, Steckholzer U, Jochum M, Ertel W (1998) Chloroquine inhibits roinflammatory cytokine release into human whole blood. Am J Physiol 274:R1058–R1064
Katchamart W, Trudeau J, Phumethum V, Bombardier C (2009) Efficacy and toxicity of methotrexate (MTX) monotherapy versus MTX combination therapy with non-biological disease-modifying antirheumatic drugs in rheumatoid arthritis: a systematic review and meta-analysis. Ann Rheum Dis 68:1105–1112
Katz SJ, Russell AS (2011) Re-evaluation of antimalarials in treating rheumatic diseases: re-appreciation and insights into new mechanisms of action. Curr Opin Rheumatol 23:278–281
Kelman SM, Sullivan SG, Stern A (1981) Chloroquine- and primaquiine-induced alterations of glucose metabolism in the uninfected red cell. Biochem Pharmacol 30:81–87
Kheirkhah A, Amoli FA, Azari AA, Molaei S, Roozbahani M (2012) Conjunctival nodule in rheumatoid arthritis. Int Ophthalmol 32:81–83
Khraishi MM, Singh G (1996) The role of anti-malarials in rheumatoid arthritis—the American experience. Lupus 5(Suppl 1):S41–S44
Kingsbury SR et al. (2013) Hydroxychloroquine effectiveness in reducing symptoms of hand osteoarthritis (HERO): study protocol for a randomized controlled trial. Trials 14:64
Kim KA, Park JY, Lee JS, Lim S (2003) Cytochrome P450 2C8 and CYP3A4/5 are involved in chloroquine metabolism in human liver microsomes. Arch Pharm Res 26:631–637
Klinefelter HF, Achurra A (1973) Effect of gold salts and antimalarials on the rheumatoid factor in rheumatoid arthritis. Scand J Rheumatol 2:177–182
Knutson VP, Ronnett GV, Lane MD (1985) The effects of cycloheximide and chloroquine on insulin receptor metabolism. J Biol Chem 260:14180–14188
Köppel C, Tenczer J, Ibe K (1987) Urinary metabolism of chloroquine. Arzneim Forsch 37:208–211
Korpela M, Laasonen L, Hannonen P, Kautiainen H, Leirisalo-Repo M, Hakala M, Paimela L, Blafield H, Puolakka K, Mottonen T, FIN-RACo Trial Group (2004) Retardation of joint damage in patients with early rheumatoid arthritis by initial aggressive treatment with disease-modifying antirheumatic drugs: five-year experience from the FIN-RACo study. Arthritis Rheum 50:2072–2081
Krane SM, Amento EP, Goldring SR (1986) Cellular interactions in tissue breakdown in rheumatoid arthritis. Adv Inflamm Res 11:1–12
Kruize AA, Hene RJ, Kallenberg CG, van Bijsterveld OP, van der Heide A, Kater L, Bijlsma JW (1993) Hydroxychloroquine treatment for primary Sjögren’s syndrome: a two year double blind crossover trial. Ann Rheum Dis 52:360–364
Kubo M, Hostettler KY (1980) Mechanism of cationic amphiphilic drug inhibition of purified lysosomal phospholipase A1. Biochemistry 24:6515–6520
Kull FC Jr, Besterman JM (1990) Drug-induced alterations of tumour necrosis factor-mediated cytotoxicity: discrimination of early versus late stage action. J Cell Biochem 42:1–12
Kyburz D, Bretano F, Gay S (2006) Mode of action of hydroxychloroquine in RA—evidence of an inhibitory effect on toll-like signalling. Nature Clin Pract Rheumatol 2:458–459
Laaksonen AL, Koskiahde V, Juva K (1974) Dosage of antimalarial drugs for children with juvenile rheumatoid arthritis and systemic lupus erythematosus. A clinical study with determination of serum concentrations of chloroquine and hydroxychloroquine. Scand J Rheumatol 3:103–108
Lafyatis R, York M, Marshak-Rothstein A (2006) Antimalarial agents: closing the gate on toll-like receptors. Arthritis Rheum 54:3068–3070
Lai J-H, Ho L-J, Lu K-C, Chang D-M, Shaio M-F, Han S-H (2001) Western and Chinese antirheumatic drug-induced T cell apoptotic DNA damage uses different caspases cascades and is independent of Fas/Fas ligand interaction. J Immunol 166:6914–6924
Landewe RBM, Miltenburg AMM, Verdonk MJA, Verweij CL, Breedveld FC, Daha MR, Dijkmans BAC (1995) Chloroquine inhibits T cell proliferation by interfering with IL-2 production and responsiveness. Clin Exp Immunol 102:144–151
Leoni A (1955) Gli effetti della chlorochina sulla riposte eritematosa al fenolo nei portatori di eritematode cronico. Minerva Derm 30:410–411
Li XQ, Björkman A, Andersson TB, Gustafsson LL, Masimirembwa CM (2003) Identification of human cytochrome P(450)s that metabolise anti-parasitic drugs and predictions of in vivo drug hepatic clearance from in vitro data. Eur J Clin Pharmacol 59:429–442
Lim HS, Im JS, Cho JY, Bae KS, Klein TA, Yeom JS, Kim TS, Choi JS, Jang IJ, Park JW (2009) Pharmacokinetics of hydroxychloroquine and its clinical implications in chemoprophylaxis against malaria caused by Plasmodium vivax. Antimicrob Agents Chemother 53:1468–1475
Lipsky PE (1986) Natural killer cell function in rheumatoid arthritis. Clin Exp Rheumatol 4:303–305
Littler TR (1990) Anti-rheumatic drugs. In: Orme M (ed) Anti-rheumatic drugs. Pergamon Press, New York, pp 189–216
Lomater G, Gattinara M, Gerloni V, Zeni S, Fantini F (1994) Combination therapy of juvenile rheumatoid arthritis with hydroxychloroquine-gold-methotrexate: a pilot study. Acta Univ Carol Med (Praha) 40:109–112
Lowe JS, Turner EH (1973) The effect of adjuvant arthritis and drugs on the ability of rat plasma to inhibit the triton X-100 induced lysis of rabbit polymorphonuclear leucocyte granules. Biochem Pharmacol 22:2069–2078
Lullmann-Rauch R, Pods R, von Witzendorff B (1996) The antimalarials quinacrine and chloroquine induce weak lysosomal storage of sulphated glycosaminoglycans in cell culture and in vivo. Toxicology 110:27–37
MacIntyre AC, Cutler DJ (1986) In vitro binding of chloroquine to rat muscle preparations. J Pharm Sci 75:1068–1070
MacIntyre AC, Cutler DJ (1988) Role of lysosomes in hepatic accumulation of chloroquine. J Pharm Sci 77:196–199
Mackenzie AH (1970) An appraisal of chloroquine. Arthritis Rheum 13:280–291
Mackenzie AH (1983a) Antimalarial drugs for rheumatoid arthritis. Am J Med 75:48–58
Mackenzie AH (1983b) Pharmacologic actions of 4-aminoquinoline compounds. Am J Med 75(1A):5–10
Mackenzie AH (1983c) Dose refinements in long-term therapy of rheumatoid arthritis with antimalarials. Am J Med 75(1A):40–45
Maksymowych W, Russell AS (1987) Antimalarials in rheumatology: efficacy and safety. Semin Arthritis Rheum 16:206–221
Malbica JO, Hart LG (1971) Effect of adenosine triphosphate and some anti-inflammatory agents on a purified lysosomal fraction having high acid phosphatase and labile β-glucuronidase activity. Biochem Pharmacol 20:2017–2026
Manku MS, Horrobin DF (1976) Chloroquine, quinacrine, procaine, quinidine and clomipramine are prostanglandin agonsist and antagonists. Prostaglandins 12:789–801
Marmor MF (2004) Hydroxychloroquine at the recommended dose (<or = 6.5 mg/kg/day) is safe for the retina in patients with rheumatoid arthritis and systemic lupus erythematosus. Clin Exp Rheumatol 22:143–144
Marmor MF, Carr RE, Easterbrook M, Farjo AA, Mieler WF, American Academy of Ophthalmology (2002) Recommendations on screening for chloroquine and hydroxychloroquine retinopathy: a report by the American Academy of Ophthalmology. Ophthalmology 109:1377–1382
Martínez-Costa L, Victoria Ibañez M, Murcia-Bello C, Epifanio I, Verdejo-Gimeno C, Beltrán-Catalán E, Marco-Ventura P (2013) Use of microperimetry to evaluate hydroxychloroquine and chloroquine retinal toxicity. Can J Ophthalmol 48:400–405
Mary CF, Legros J (1987) Experimental study of ocular effects of hydroxychloroquine in the rat: influence of oxidiser status. Br J Clin Pract 41(Suppl 52):46–49
Matsuzawa Y, Hostettler KY (1980) Inhibition of lysosomal phospholipase A and phospholipase C by chloroiquine and 4,4′-bis(diethylaminoethoxy)α, β-diethyldiphenylethane. J Biol Chem 255:5190–5194
McCarty DJ, Carrera GF (1982) Intractable rheumatoid arthritis. Treatment with combined cyclophosphamide, azathioprine, and hydroxychloroquine. J Am Med Assn 248:1718–1723
McChesney EW (1983) Animal toxicity and pharmacokinetics of hydroxychloroquine sulphate. Am J Med 75(6A):11–18
McChesney EW, Fitch CD (1984) 4-Aminoquinolines. In: Peters W, Richards WHG (eds) Antimalarial drugs II. Springer, Berlin, pp 3–60
McChesney EW, Banks WF Jr, Sullivan DJ (1965) Metabolism of chloroquine and hydroxychloroquine in albino and pigmented rats. Toxicol Appl Pharmacol 7:627–636
McChesney EW, Conway WD, Banks WF Jr, Rogers JE, Shekosky JM (1966) Studies on the metabolism of some compounds of the 4-amino-7-chloroquinoline series. J Pharmacol Exp Ther 151:482–493
McChesney EW, Banks WF Jr, Fabian RJ (1967a) Tissue distribution of chloroquine, hydroxychloroquine, and desethylchloroquine. Toxicol Appl Pharmacol 10:501–513
McChesney EW, Fasco MJ, Banks WF (1967b) The metabolism of chloroquine in man after repeated oral dosage. J Pharmacol Exp Ther 158:323–331
McElnay JC, Sidahmed AM, D’Arcy PF, McQuade RD (1985) Chloroquine-digoxin interaction. Int J Pharm 1985:267–274
McGettigan P, Henry D (2006) Cardiovascular risk and inhibition of cyclooxygenase: asystematic review of the observational studies of selective and nonselective inhibitors of cyclooxygenase 2. J Am Med Assn 296:1633–1644
McKendry RJR et al. (2001) Hydroxychloroquine (HCQ) versus acetaminophen (ACM) versus placebo (PL) in the treatment of nodal osteoarthritis (NOA) of the hands. J Rheumatol 28:1421–1421
McLachlan AJ, Tett SE, Cutler DJ, Day RO (1993) Disposition of the enantiomers of hydroxychloroquine in patients with rheumatoid arthritis following multiple doses of the racemate. Br J Clin Pharmacol 36:78–81
McLachlan AJ, Tett SE, Cutler DJ, Day RO (1994) Disposition and absorption of hydroxychloroquine enantiomers following a single dose of the racemate. Chirality 6:360–364
Meller S, Gerber PA, Homey B (2008) Clinical image: blonde by prescription. Arthritis Rheum 58:2286
Midha KK, McKay G, Rawson MJ, Hubbard JW (1998) The impact of stereoisomerism in bioequivalence studies. J Pharm Sci 87:797–802
Migkos MP, Markatseli TE, Iliou C, Voulgari PV, Drosos AA (2014) Effect of hydroxychloroquine on the lipid profile of patients with Sjögren syndrome. J Rheumatol 41:902–908
Miller LC (1995) Cytokines in rheumatic diseases. Biotherapy 8:99–111
Minta JO, Williams MD (1986) Interactions of antirheumatic drugs with the superoxide generation system of activated human polymorphonuclear leukocytes. J Rheumatol 13:498–504
Miyachi Y, Yoshioka A, Imamura S, Niwa Y (1986) Antioxidant action of antimalarials. Ann Rheum Dis 45:244–248
Mottonen T, Hannonen P, Korpela M, Nissila M, Kautiainen H, Ilonen J, Laasonen L, Kaipiainen-Seppanen O, Franzen P, Helve T, Koski J, Gripenberg-Gahmberg M, Myllykangas-Luosujarvi R, Leirisalo-Repo M, the FIN-RACo Trial Group (2002) FINnish Rheumatoid Arthritis Combination therapy. Delay to institution of therapy and induction of remission using single-drug or combination-disease-modifying antirheumatic drug therapy in early rheumatoid arthritis. Arthritis Rheum 46:894–898
Muller-Peddinghaus R, Wurl M (1987) The amplified chemiluminescence test to characterize antirheumatic drugs as oxygen radical scavengers. Biochem Pharmacol 36:1125–1132
Mullié C, Jonet A, Desgrouas C, Taudon N, Sonnet P (2012) Differences in anti-malarial activity of 4-aminoalcohol quinoline enantiomers and investigation of the presumed underlying mechanism of action. Malar J 11:65
Munster T, Gibbs JP, Shen D, Baethge BA, Botstein GR, Caldwell J, Dietz F, Ettlinger R, Golden HE, Lindsley H, McLaughlin GE, Moreland LW, Roberts WN, Rooney TW, Rothschild B, Sack M, Sebba AI, Weisman M, Welch KE, Yocum D, Furst DE (2002) Hydroxychloroquine concentration-response relationships in patients with rheumatoid arthritis. Arthritis Rheum 46:1460–1469
Namazi MR (2009) The potential negative impact of proton pump inhibitors on the immunopharmacologic effects of chloroquine and hydroxychloroquine. Lupus 18:104–105
Nation RL, Hackett LP, Dusci LJ, Ilett KF (1984) Excretion of hydroxychloroquine in human milk. Br J Clin Pharmacol 17:368–369
Nayak V, Esdaile JM (1996) The efficacy of antimalarials in systemic lupus erythematosus. Lupus 5(Suppl 1):S23–S27
Neal TM, Vissers MC, Winterbourn CC (1987) Inhibition by nonsteroidal anti-inflammatory drugs of superoxide production and granule enzyme release by polymorphonuclear leukocytes stimulated with immune complexes or formyl-methionyl-leucyl-phenylalanine. Biochem Pharmacol 36:2511–2517
Nebbioso M, Livani ML, Steigerwalt RD, Panetta V, Rispoli E (2011) Retina in rheumatic diseases: standard full field and multifocal electroretinography in hydroxychloroquine retinal dysfunction. Clin Exp Optom 94:276–283
Neidel J, Zeidler U (1993) Independent effects of interleukin 1 on proteoglycan synthesis and proteoglycan breakdown of bovine articular cartilage in vitro. Agents Actions 39:82–90
Neil HA, Perera R, Armitage JM, Farmer AJ, Mant D, Durrington PN (2008) Estimated 10-year cardiovascular risk in a British population: results of a national screening project. Int J Clin Pract 62:1322–1331
Neill WA, Panayi GS, Duthie JJR (1973) Action of chloroquine phosphate in rheumatoid arthritis. 2. Chromosome damaging effect. Ann Rheum Dis 32:547–550
Newbold BB (1963) Chemotherapy of arthritis induced in rats by mycobacterial adjuvant. Br J Pharmacol Chemother 21:127–136
Northover BJ (1977) Effect of indomethacin and related drugs on the calcium ion-dependent secretion of lysosomal and other enzymes by neutrophil polymorphonuclear leucocytes in vitro. Br J Pharmacol 59:253–259
Novikoff AB, Beafay H, De Duve C (1956) Electron microscopy of lysosome rich fractions from rat liver. J Biophys Biochem Cytol 25(4 Suppl):179–184
Obua C, Ntale M, Lundblad MS, Mahindi M, Gustafsson LL, Ogwal-Okeng JW, Anokbonggo WW, Hellgren U (2006) Pharmacokinetic interactions between chloroquine, sulfadoxine and pyrimethamine and their bioequivalence in a generic fixed-dose combination in healthy volunteers in Uganda. Afr Health Sci 6:86–92
O’Dell JR (1998) Triple therapy with methotrexate, sulfasalazine, and hydroxychloroquine in patients with rheumatoid arthritis. Rheum Dis Clin North Am 24:465–477
O’Dell JR (1999) Combination DMARD therapy with hydroxychloroquine, sulfasalazine, and methotrexate. Clin Exp Rheumatol 17:S53–S58
O’Dell JR, Blakely KW, Mallek JA, Eckhoff PJ, Leff RD, Wees SJ, Sems KM, Fernandez AM, Palmer WR, Klassen LW, Paulsen GA, Haire CE, Moore GF (2001) Treatment of early seropositive rheumatoid arthritis: a two-year, double-blind comparison of minocycline and hydroxychloroquine. Arthritis Rheum 44:2235–2241
O’Dell JR, Petersen K, Leff R, Palmer W, Schned E, Blakely K, Haire C, Fernandez A (2006) Etanercept in combination with sulfasalazine, hydroxychloroquine, or gold in the treatment of rheumatoid arthritis. J Rheumatol 33:213–218
Oforah E, Anyogo S (2000) The contributions of various chloroquine salts to the biliary and urinary execretion of hepatic paracetamol conjugation metabolites in the rat. Drug Metabol Drug Interact 16:129–141
Ogunbona FA, Onyeji CO, Bolaji OO, Torimiro SE (1987) Excretion of chloroquine and desethylchloroquine in human milk. Br J Clin Pharmacol 23:473–476
Ohsugi Y, Gershwin ME (1984) Inhibition by various antiarthritic agents of murine splenic B cell colony formation. Immunopharmacology 7:1–7
Onyeji CO, Toriola TA, Ogunbona FA (1993) Lack of pharmacokinetic interaction between chloroquine and imipramine. Ther Drug Monit 15:43–46
Østensen M, Brown ND, Chiang PK, Aarbakke J (1985) Hydroxychloroquine in human breast milk. Eur J Clin Pharmacol 28:357
Padol IT, Hunt RH (2010) Association of myocardial infarctions with COX-2 inhibition may be related to immunomodulation towards a Th1 response resulting in atheromatous plaque instability: an evidence-based interpretation. Rheumatology 49:837–843
Page F (1951) Treatment of lupus erythematosus with mepacrine. Lancet 2:755–758
Panayi GS, Neill WA, Duthie JJR, McCormick JN (1973) Action of chloroquine phosphate in rheumatoid arthritis. 1. Immunosuppressive effect. Ann Rheum Dis 32:316
Pappu A, Hauser G (1981) Changes in brain phosphoinositide metabolism induced by cationic amphiphilic drugs in vitro. Biochem Pharmacol 30:3234–3246
Parke AL (1993) Antimalarial drugs, pregnancy and lactation. Lupus 2(Suppl 1):S21–S23
Pasternak RD, Marks RL, Hubbs SJ, DiPasquale G (1985) Effects of antirheumatic agents on the mitogen response of arthritic rat spleen cells. Rec Commun Chem Path Pharmacol 48:353–367
Paulus HE (1988) Antimalarial agents compared with or in combination with other disease-modifying antirheumatic drugs. Am J Med 85:45–52
Pavelka K Jr, Pavelka Sen K, Peliskova Z, Vacha J, Trnavsky K (1989) Hydroxychloroquine sulphate in the treatment of rheumatoid arthritis: a double blind comparison of two dose regimens. Ann Rheum Dis 48:542–546
Payne JP (1894) A lecture on lupus erythematosus. Clin J IV:223
Penn SK, Kao AH, Schott LL, Elliott JR, Toledo FG, Kuller L, Manzi S, Wasko MC (2010) Hydroxychloroquine and glycemia in women with rheumatoid arthritis and systemic lupus erythematosus. J Rheumatol 37:1136–1142
Perrin DD (1965) Dissociation constants of organic bases in aqueous solutions. Butterworths, London
Petri M (1996) Hydroxychloroquine use in the Baltimore Lupus Cohort; effects on lipids, glucose and thrombosis. Lupus 5(Suppl 1):S16–S22
Petri M (2005) Lupus in Baltimore: evidence-based ‘clinical pearls’ from the Hopkins Lupus Cohort. Lupus 14:970–973
Petri M, Purvey S, Fang H, Magder LS (2012) Predictors of organ damage in systemic lupus erythematosus: the Hopkins Lupus Cohort. Arthritis Rheum 64:4021–4028
Pettipher ER, Higgs GA, Henderson B (1986) Interleukin 1 induces leukocyte infiltration and cartilage proteoglycan degradation in the synovial joint. Proc Natl Acad Sci USA 1986(83):8749–8753
Pico S, Peyron F, Vuillez J-P, Polack B, Ambroise-Thomas P (1991) Chloroquine inhibits tumour necrosis factor production by human macrophages in vitro. J Infect Dis 164:830
Pons-Estel GJ, Alarcón GS, McGwin G Jr, Danila MI, Zhang J, Bastian HM, Reveille JD, Vilá LM, Lumina Study Group (2009) Protective effect of hydroxychloroquine on renal damage in patients with lupus nephritis: LXV, data from a multiethnic US cohort. Arthritis Rheum 61:830–839
Projean D, Baune B, Farinotti R, Flinois JP, Beaune P, Taburet AM, Ducharme J (2003) In vitro metabolism of chloroquine: identification of CYP2C8, CYP3A4, and CYP2D6 as the main isoforms catalyzing N-desethylchloroquine formation. Drug Metab Dispos 31:748–754
Punzi L et al. (1996) Soluble interleukin 2 receptors and treatment with hydroxychloroquine in erosive osteoarthritis. J Rheumatol 23:1477–1478
Pussard E, Verdier, Blayo M-C (1986) Simultaneous determination of chloroquine, amadiaquine and their metabolites in human plasma, red blood cells, and whole blood and urine by column liquid chromatography. J Chromatogr 374:111–118
Raghoebar M, Peeters PA, van den Berg W, van Ginneken CA (1986) Mechanisms of cell association of chloroquine to leucocytes. J Pharmacol Exp Ther 238:302–306
Raina RK, Bano G, Amla V, Kapoor V, Gupta KL (1993) The effect of aspirin, paracetamol and analgin on pharmacokinetics of chloroquine. Indian J Physiol Pharmacol 37:229–231
Rainsford KD (1985) Effects of anti-inflammatory drugs on catabolin-induced cartilage destruction in vitro. Int J Tissue React 7:123–126
Rainsford KD (1986) Effects of antimalarial drugs on interleukin 1-induced cartilage proteoglycan degradation in-vitro. J Pharm Pharmacol 38:829–833
Rainsford KD (1987) Effects of anti-inflammatory drugs on the release from synovial tissues of cartilage-resorbing (catabolin-like) activity in vitro: role of assay conditions and drug effects on eicosanoid metabolism. In: The control of tissue damage. The Strangeways Research Laboratory 75th Annual Symposium. Arthritis and Rheumatism Council for Research, p 130
Rainsford KD (1988) Inhibitors of prostaglandin and leukotriene production. In: Curtis-Prior PB (ed) Prostaglandins: biology and chemistry of prostaglandins and related eicosanoids. Churchill-Livingstone, London, pp 52–68
Rainsford KD (1990) Analgesics vs. nonsteroidal anti-inflammatory drugs (NSAIDs): differences among NSAIDs. In: Brandt KD (ed) Cartilage changes in osteoarthritis. Indiana University School of Medicine, pp 129–136
Rainsford KD (1992). Effects of antimalarial drugs oin the progression of adjuvant induced arthritis in rats. Unpublished studies
Rainsford KD, Rashad SY, Revell PA, Low FM, Hemingway AP, Walker FS, Johnson D, Stetsko P, Ying C, Smith F (1992) Effects of NSAIDs on cartilage proteoglycan and synovial prostaglandin metabolism in relation to progression of joint deterioration in osteoarthritis. In: Bálint G, Gömör B, Hadinka L (eds) Rheumatology, state of the art. Elsevier, Amsterdam, pp 177–183
Rand JH, Wu X-X, Quinn AS, Chen PP, Hathcock JJ, Taatjes DJ (2008) Hydroxychloroquine directly reduces the binding of anti-phospholipid antibody-β2-glycoprotein I complexes to phospholipid bilayers. Blood 112:1687–1695
Räsänen L, Lehto M, Hyöty H, Leinikki P (1989) Collaboration between human blood dentritic cells and monocytes in antigen presentation. APMIS 97:981–986
Riches DWH, Stanworth DR (1982) Weak-base induced lysosomal secretion by macrophages: an alternative trigger mechanism that is independent of complement activation. Adv Exp Biol 155:313–323
Riches DWH, Morris CJ, Stanworth DR (1981) Induction of selective acid hydrolase release from mouse macrophages during exposure to chloroquine and quinine. Biochem Pharmacol 30:629–634
Robertson CR et al. (1993) Treatment of erosive osteoarthritis with hydroxychloroquine. Arthritis Rheum 36:S167
Ruiz-Irastorza G, Khamashta MA (2008) Hydroxychloroquine: the cornerstone of lupus therapy. Lupus 17:271–273
Ruiz-Irastorza G, Ramos-Casals M, Brito-Zeron P, Khamashta MA (2010) Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus. Ann Rheum Dis 69:20–28
RxFiles Detailing Program (2008) Drug comparison charts, 7th edn. In: Jensen B, Regier LD (Eds). Saskatoon City Hospital, Saskatoon, p 62
Rynes RI (1988) Toxicity of antimalarial drugs in rheumatoid arthritis. Agents Actions Suppl 44:151–157
Rynes RI (1992) Antimalarials. In: Dixon JS, Furst DE (eds) Second-line agents in the treatment of rheumatic diseases. Marcel Dekker, New York, pp 245–266
Rynes RI (1997) Antimalarial drugs in the treatment of rheumatological diseases. Br J Rheumatol 36:799–805
Saklatvala J, Sarsfield SJ (1988) How do interleukin-1 and tumour necrosis factor induce degradation of proteoglycan in cartilage? In: Glauert A (ed) The control of tissue damage. Elsevier, Amsterdam, pp 97–108
Saklatvala J, Pilsworth LMC, Sarsfield SJ, Gavrilovic J, Health JK (1984) Pig catabolin is a form of interleukin 1. Cartilage and bone resorb, fibroblasts make prostaglandins and collagen, and thymocyte proliferation is augmented in response to one protein. Biochem J 224:461–466
Salaffi F, Carotti M, Cervini C (1996) Combination therapy of cyclosporine A with methotrexate or hydroxychloroquine in refractory rheumatoid arthritis. Scand J Rheumatol 25:16–23
Salmeron G, Lipsky PE (1983) Immunosuppressive potential of antimalarials. Am Med J 75(1A):19–24
Salton DJ (1987) Chloroquine and the eye. Br J Clin Pract 41(Suppl 52):50–55
Sammaritano LR, Bermas BL (2014) Rheumatoid arthritis medications and lactation. Curr Opin Rheumatol 26:354–360
Sams WM (1967) Chloroquine: mechanism of action. Mayo Clin Proc 42:300–309
Sanders M (2000) A review of controlled clinical trials examining the effects of antimalarial compounds and gold compounds on radiographic progression in rheumatoid arthritis. J Rheumatol 27:523–529
Saviola G et al. (2012) Clondronate and hydroxychloroquine in erosive osteoarthritis: a 24-month open randomized pilot study. Mod Rheumatol 22(2):256–263
Scala G, Oppenheim JJ (1983) Antigen presentation by human monocytes: evidence for stimulant processing and requirement for interleuklin 1. J Immunol 131:1160–1166
Schug BS, Kalbhen DA (1995) Influence of chloroquine and other substances on the collagenolytic activity in human osteoarthritic cartilage in vitro. Arzneimittelforschung 45:285–289
Semrau K, Kuhn L, Kasonde P, Sinkala M, Kankasa C, Shutes E, Vwalika C, Ghosh M, Aldrovandi G, Thea DM (2006) Impact of chloroquine on viral load in breast milk. Trop Med Int Health 11:800–833
Seror R, Theander E, Bootsma H, Bowman SJ, Tzioufas A, Gottenberg JE, Ramos-Casals M, Dörner T, Ravaud P, Mariette X, Vitali C (2014) Outcome measures for primary Sjögren’s syndrome: a comprehensive review. J Autoimmun 51:51–56
Seror R, Theander E, Brun JG, Ramos-Casals M, Valim V, Dörner T, Bootsma H, Tzioufas A, Solans-Laqué R, Mandl T, Gottenberg JE, Hachulla E, Sivils KL, Ng WF, Fauchais AL, Bombardieri S, Valesini G, Bartoloni E, Saraux A, Tomsic M, Sumida T, Nishiyama S, Caporali R, Kruize AA, Vollenweider C, Ravaud P, Vitali C, Mariette X, Bowman SJ, Sjögren’s Task Force EULAR (2015) Validation of EULAR primary Sjögren’s syndrome disease activity (ESSDAI) and patient indexes (ESSPRI). Ann Rheum Dis 74:859–866
Shearer RV, Dubois EL (1967) Ocular changes induced by long-term hydroxychloroquine (plaquenil) therapy. Am J Ophthalmol 64:245–252
Sheppeard H, Pilsworth LM, Hazleman B, Dingle JT (1982) Effects of antirheumatoid drugs on the production and action of porcine catabolin. Ann Rheum Dis 41:463–468
Sibtain SK et al. (2007) Role of hydroxychloroquine in management of osteoarthritis. Rheumatology (Oxford) 46:i61–i61
Silva MA, Ishii-Iwamoto EL, Bracht A, Caparroz-Assef SM, Kimura E, Cuman RK, Bersani-Amado CA (2005) Efficiency of combined methotrexate/chloroquine therapy in adjuvant-induced arthritis. Fundam Clin Pharmacol 19:479–489
Sisó A, Ramos-Casals M, Bové A, Brito-Zerón P, Soria N, Muñoz S, Testi A, Plaza J, Sentís J, Coca A (2008) Previous antimalarial therapy in patients diagnosed with lupus nephritis: influence on outcomes and survival. Lupus 17:281–288
Skinner-Adams TS, Andrews KT, Melville L, McCarthy J, Gardiner DL (2007) Synergistic interactions of the antiretroviral protease inhibitors saquinavir and ritonavir with chloroquine and mefloquine against Plasmodium falciparum in vitro. Antimicrob Agents Chemother 51:759–762
Smith RJ (1977) Modulation of phagocytosis by and lysosomal enzyme secretion from guinea-pig neutrophils: effect of nonsteroid anti-inflammatory agents and prostaglandins. J Pharmacol Exp Ther 200:647–657
Sneader W (2005) Drug discovery. A history. John Wiley, Chichester
Somer M, Kallio J, Pesonen U, Pyykko K, Huupponen R, Scheinin M (2000) Influence of hydroxychloroquine on the bioavailability of oral metoprolol. Br J Clin Pharmacol 49:549–554
Spaldin V, Madden S, Pool WF, Woolf TF, Park BK (1994) The effect of enzyme inhibition on the metabolism and activation of tacrine by human liver microsomes. Br J Clin Pharmacol 38:15–22
Sperber K, Quraishi H, Kalb TH, Stecher V, Mayer L (1993) Selective regulation of cytokine secretion by hydroxychloroquine: inhibition of interleukin 1 alpha (IL-1α) and IL-6 in human monocytes and T cells. J Rheumatol 20:813–818
Stecher VJ, Connolly KM, Speicht PT (1987) Fibronectin and macrophages as parameters of disease-modifying antirheumatic activity. Br J Clin Practice 41(Suppl 52):64–71
Stepien KB, Wilczok T (1982) Studies on the mechanism of chloroquine binding to synthetic DOPA-melanin. Biochem Pharmacol 31:3359–3365
Stepien K, Porebska M, Wilczok T (1987) Interaction of chloroquine with melanosomes and model melanin complexes. Stud Biophys 122:165–174
Stringer E, Bohnsack J, Bowyer SL, Griffin TA, Huber AM, Lang B, Lindsley CB, Ota S, Pilkington C, Reed AM, Scuccimarri R, Feldman BM (2010) Treatment approaches to juvenile dermatomyositis (JDM) across North America: the Childhood Arthritis and Rheumatology Research Alliance (CARRA) JDM Treatment Survey. J Rheumatol 37:1953–1961
Sun S, Rao NL, Venable J, Thurmond R, Karlsson L (2007) TLR7/9 antagonists as therapeutics for immune-mediated inflammatory disorders. Inflamm Allergy Drug Targets 6:223–235
Suzuki Y, Ito I, Ito M, Yamagami I (1973) Changes of mucopolysaccharase, protease and collagenolytic activities in rats with adjuvant arthritis and the effects of various anti-inflammatory drugs. Nippon Yakurigaku Zasshi 69:947–968 (in Japanese)
Tagoe CN, Ofori-Adjei D (1995) Effects of chloroquine and its enantiomers on the development of rat embryos in vitro. Teratology 52:137–142
Tang C, Godfrey T, Stawell R, Nikpour M (2012) Hydroxychloroquine in lupus: emerging evidence supporting multiple beneficial effects. Intern Med J 42:968–978
Tauber R, Heinze K, Reutter W (1985) Effect of chloroquine on the degradation of l-fucose and the polypeptide moiety of plasma membrane glycoproteins. Eur J Cell Biology 39:380–385
Tehrani R, Ostrowski RA, Hariman R, Jay WM (2008) Ocular toxicity of hydroxychloroquine. Semin Ophthalmol 23:201–209
Teitz CC, Chrisman OD (1975) The effect of salicylate and chloroquine on prostaglandin-induced articular damage in the rabbit knee. Clin Orthop Relat Res 12:264–274
Tejeswar Rao P (1977) Intra-articular chloroquine in rheumatoid and osteo-arthritis of knee joint. J Indian Med Assoc 69(9):193–195
Tett SE (1993) Clinical pharmacokinetics of slow-acting antirheumatic drugs. Clin Pharmacokinet 25:392–407
Tett SE, Cutler DJ, Day RO, Brown KF (1989) Bioavailability of hydroxychloroquine tables in healthy volunteers. Br J Pharmacol 27:771–779
Tett S, Cutler D, Day R (1990) Antimalarials in rheumatic diseases. Bailliere’s Clin Rheumatol 4:467–489
Tett S, McLachlan A, Day R, Cutler D (1993) Insights from pharmacokinetic and pharmacodynamic studies of hydroxychloroquine. Agents Actions Suppl 44:145–190
Tett SE, McLachlan AJ, Cutler DJ, Day RO (1994) Pharmacokinetics and pharmacodynamics of hydroxychloroquine enantiomers in patients with rheumatoid arthritis receiving multiple doses of racemate. Chirality 6:355–359
Thiele DL, Lipsky PE (1985a) Modulation of human natural killer cell function by l-leucine methyl ester: monocyte-dependent depletion from human peripheral blood mononuclear cells. J Immunol 134:786–793
Thiele DL, Lipsky PE (1985b) Regulation of cellular function by products of lysosomal enzyme activity: elimination of human natural killer cells by a dipeptide methyl ester generated from l-leucine methyl ester by monocytes or poplymorphonuclear leukocytes. Proc Nat Acad Sci USA 82:2468–2472
Thompson GR, Bartholomew L (1964) The effect of chloroquine on antibody production. Univ Michigan Med Ctr J 30:227–230
Thorens B, Vassalli P (1986) Chloroquine and ammonium chloride prevent terminal glycosylation of immunoglobulins in plasma cells without affecting secretion. Nature 321:618–620
Titus EO (1989) Recent developments in the understanding of the phramacokinetics and mechanism of action of chloroquine. Ther Drug Monit 11:369–379
Trnavská Z, Trnavský K (1967) Influence of anti-rheumatic drugs on urinary excretion of hydroxyproline in lathyrism. Nature 214:384
Trnavsky K, Gatterova J, Linduskova M, Peliskova Z (1993) Combination therapy with hydroxychloroquine and methotrexate in rheumatoid arthritis. Z Rheumatol 52:292–296
Tzekov R (2005) Ocular toxicity due to chloroquine and hydroxychloroquine: electrophysiological and visual function correlates. Doc Ophthalmol 110:111–120
Van Cauwenberge H, Lecomte J, Lapiere C (1958a) Influence de la chloroquine sur l’oedeme a la ovalbumine ou au dextran, et sur la test d’ambrose et de eds chez le rat. C R Soc Biol 152:1405–1408
Van Cauwenberge H, Lecomte J, Lapiere C (1958b) Influence de la chloroquine sur le development du granulome a l’ouate et sur la poche granulomateuse. C R Soc Biol 152:1414–1417
van den Borne BE, Landewe RB, Goei The HS, Rietveld JH, Zwinderman AH, Bruyn GA, Breedveld FC, Dijkmans BA (1998) Combination therapy in recent onset rheumatoid arthritis: a randomized double blind trial of the addition of low dose cyclosporine to patients treated with low dose chloroquine. J Rheumatol 25:1493–1498
van der Heijde DM, van Riel PL, Nuver-Zwart IH, Gribnau FW, vad de Putte LB (1989) Effects of hydroxychloroquine and sulphasalazine on progression of joint damage in rheumatoid arthritis. Lancet 1:1036–1038
van Loenen HJ, Dijkmans BA, De Vries E (1990) Concentration dependency of cyclosporin and chloroquine as inhibitors of cell proliferation and immunoglobulin production upon mitogen stimulation of mononuclear cells. Clin Exp Rheumatol 1990(8):59–61
Van Roon EN, van den Bemt PMLA, Jansen TLThA, Houtman NM, van de Laar MAFJ, Brouwers JRBJ (2009) An evidence-based assessment of the clinical significance between disease-modifying antirheumatic drugs and non-antirheumatic drugs according to rheumatologists and pharmacists. Clin Ther 31:1737–1746
van Vollenhoven RF, Ernestam S, Geborek P, Petersson IF, Coster L, Waltbrand E, Zickert A, Theander J, Thorner A, Hellstrom H, Teleman A, Dackhammar C, Akre F, Forslind K, Ljung L, Oding R, Chatzidionysiou A, Wornert M, Bratt J (2009) Addition of infliximab compared with addition of sulfasalazine and hydroxychloroquine to methotrexate in patients with early rheumatoid arthritis (Swefot trial): 1-year results of a randomised trial. Lancet 374:459–466
Varga F (1968a) Tissue distribution of chloroquine in the rat. Acta Physiol Acad Sci Hung Tomus 34:319–325
Varga F (1968b) Intracellular localization of chloroquine in the liver and kidney of the rat. Acta Physiol Acad Sci Hung Tomus 34:327–332
Vayuvegula B, Ohira K, Gollapudi S, Gupta S (1990) Role of monocytes in anti-CD3—induced T-cell DNA synthesis: effect of chloroquine and monensin on anti-CD3—induced T-cell activation. J Clin Immunol 10:247–254
Verstappen SM, Jacobs JW, Bijlsma JW, Heurkens AH, van Booma-Frankfort C, Borg EJ, Hofman DM, van der Veen MJ, the Utrecht Arthritis Cohort Study Group (2003) Five-year follow-up of rheumatoid arthritis patients after early treatment with disease-modifying antirheumatic drugs versus treatment according to the pyramid approach in the first year. Arthritis Rheum 48:1797–1807
Vezmar M, Georges E (2000) Reversal of MRP-mediated doxorubicin resistance with quinoline-based drugs. Biochem Pharmacol 59:1245–1252
Viala A, Deturmeny E, Aubert C, Estadieu M, Durnad A, Cano JP, Delmont J (1983) Determination of chloroquine and monodesethylchloroquine in hair. J Forensic Sci 28:922–928
Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH, European Study Group on Classification Criteria for Sjögren’s Syndrome (2002) Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 61:554–558
Vitali C, Bootsma H, Bowman SJ, Dorner T, Gottenberg JE, Mariette X, Ramos-Casals M, Ravaud P, Seror R, Theander E, Tzioufas AG (2013) Classification criteria for Sjogren’s syndrome: we actually need to definitively resolve the long debate on the issue. Ann Rheum Dis 72:476–478
Volastro PS, Malawista SE, Chrisman OD (1973) Chloroquine: protective and destructive effects on injured rabbit cartilage in vivo. Clin Orthop Relat Res 14:243–248
Vuolteenaho K, Moilanen T, Hämäläinen M, Moilanen E (2003) Regulation of nitric oxide production in osteoarthritic and rheumatoid cartilage. Role of endogenous IL-1 inhibitors. Scand J Rheumatol 32:19–24
Vuolteenaho K, Kujala P, Moilanen T, Moilanen E (2005) Aurothiomalate and hydroxychloroquine inhibit nitric oxide production in chondrocytes and in human osteoarthritic cartilage. Scand J Rheumatol 34:475–479
Wallace DJ (1996) The history of antimalarials. Lupus 5(Suppl 1):S2–S3
Ward PA (1966) The chemosuppression of chemotaxis. J Exp Med 23:1038–1044
Wei LC, Chen SN, Ho CL, Kuo YH, Ho JD (2001) Progression of hydroxychloroquine retinopathy after discontinuation of therapy: case report. Chang Gung Med J 24:329–334
Weissmann G (1984) Labilization and stabilization of lysosomes. Federation Proc 23:1038–1044
White NJ (1985) Clinical pharmacokinetics of antimalarial drugs. Clin Pharmacokinet 10:187–215
Whitehead RW, Hager JP (1954) The anti-inflammatory and anti-hyaluronidase effect of chloroquine diphosphate. J Pharmacol Exp Ther 110:52–53
Whitehouse MW (1967) Evaluation of potential antirheumatic drugs in vitro using lymphocytes and epithelial cells. The selective action of indoxole, methyl glyoxal and chloroquine. J Pharm Pharmacol 19:590–595
Whitehouse MW, Boström H (1962) The effect of some anti-rheumatic drugs on the metabolism of connective tissues. Biochem Pharmacol 11:1175–1201
Whitehouse MW, Boström H (1965) Biochemical properties of anti-inflammatory drugs. VI. The effects of chloroquine (resochin), mepacrine (quinacrine) and some of their potential metabolites on cartilage metabolism and oxidative phosphorylation. Biochem Pharmacol 14:1173–1184
Whitehouse MW, Cowley FK (1966) Inhibition of connective tissue proteases by antimalarials. Biochem J 98:118–120
Wiegmann K, Schutze S, Machleidt T, Witte D, Kronke M (1994) Functional dichotomy of neutral and sphingomylinase in tumor necrosis factor signalling. Cell 78:1005
Wildfeuer A (1983) Action of antirheumatic drugs on the function of human leucocytes. Arzneimittelforschung 33:780–783
Williams WR, Davidson LAG (1983) Effects of therapeutic drugs on lymphocyte transformation. Br J Clin Pharmacol 15:83–90
Witiak DT, Grattan DA, Heaslip RJ, Rahwan RG (1981) Synthesis and preliminary pharmacological evaluation of asymmetric chloroquine analogues. J Med Chem 24:712–717
Wolfe F, Michaud K (2008) The risk of myocardial infarction and pharmacologic and nonpharmacologic myocardial infarction predictors in rheumatoid arthritis: a cohort and nested case-control analysis. Arthritis Rheum 58:2612–2621
Woo TY, Callen JP, Voorhees JJ, Bickers DR, Hanno R, Hawkins C (1984) Cutaneous lesions of dermatomyositis are improved by hydroxychloroquine. J Am Acad Dermatol 10:592–600
Wozniacka A, Lesiak A, Boncela J, Smolarczyk K, McCauliffe DP, Sysa-Jedrzejowska A (2008) The influence of antimalarial treatment in IL-1β, IL-6 and TNF-α mRNA expression on UVB-irradiated skin in systemic lupus erythematosus. Br J Dematol 159:1124–1130
Yanagishita M, Hascall VC (1984) Metabolism of proteoglycans in rat ovarian granulosa cell culture. Multiple intracellular degradative pathways and the effects of chloroquine. J Biol Chem 259:10270–10283
Yasuda T (2006) Cartilage destruction by matrix degradation products. Mod Rheumatol 16:197–205
Yi Q, Holm G, Lefvert AK (1996) Idiotype-induced T cell stimulation requires antigen presentation in association with HLA-DR molecules. Clin Exp Immunol 104:359–365
Zhang W, Doherty M, Leeb BF, Alekseeva L, Arden NK, Bijlsma JW, Dinçer F, Dziedzic K, Häuselmann HJ, Herrero-Beaumont G, Kaklamanis P, Lohmander S, Maheu E, Martín-Mola E, Pavelka K, Punzi L, Reiter S, Sautner J, Smolen J, Verbruggen G, Zimmermann-Górska I (2007) EULAR evidence based recommendations for the management of hand osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis 66:377–388
Zhou D, Liu Y, Xu LH, Ouyang DY, Pan H, Zhang XY, Zhao GX, He XH (2015) Chloroquine differentially modulates inflammatory cytokine expression in RAW 264.7 cells in response to inactivated Staphylococcus aureus. Inflammation 38:745–755
Conflict of interest
The authors declare no financial interest or support from commercial organizations marketing antimalarials in preparing this review. This was entirely author-initiated research for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rainsford, K.D., Parke, A.L., Clifford-Rashotte, M. et al. Therapy and pharmacological properties of hydroxychloroquine and chloroquine in treatment of systemic lupus erythematosus, rheumatoid arthritis and related diseases. Inflammopharmacol 23, 231–269 (2015). https://doi.org/10.1007/s10787-015-0239-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-015-0239-y