Abstract
Allanblackia gabonensis (Guttiferae) is a plant used in the African traditional medicine as remedies against pain, rheumatism, inflammations. In the present work, the analgesic effect of aqueous extract has been evaluated using acetic acid, formalin, hot-plate test, tail immersion and paw-pressure test. The anti-inflammatory effect of this extract was also investigated on carrageenan, histamine or serotonin induced by paw oedema. Aqueous extract of stem bark of A. gabonensis administrated p.o. showed significant activity against paw oedema induced by carrageenan, with a maximum percentage of inhibition reaching the 74.01% at the preventive test at a dose of 200 mg/kg. A. gabonensis exhibited a significant reduction of paw oedema induced by both histamine and serotonin with a maximal inhibition of 56.94% (200 mg/kg) and 40.83% (100 mg/kg), respectively. It showed significant protective effects against chemical stimuli (acetic acid and formalin) in the mouse. Administered orally at the doses of 100–400 mg/kg, exhibited protective effect of at least 69.78% on the pain induced by acetic acid and also reduced first (67.18% at 200 mg/kg) and second (83.87% at 400 mg/kg) phase of pain-induced par formalin. It also produced a significant increase of the threshold of sensitivity to pressure and hot plate-induced pain in the rats. These results suggest a peripheral and central analgesic activities as well as an anti-inflammatory effect of the stem bark of A. gabonensis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory diseases are currently treated with steroidal and non-steroidal anti-inflammatory drugs (NSAIDS). These drugs are also used to relieve pain which is a major symptom that accompanies several illnesses. NSAIDS exert their effects by inhibiting the metabolism of arachidonic acid by both cyclooxygenase and lipoxygenase enzyme pathways (Insel 1996). But the chronic use of NSAIDS are often associated with the several adverse effects, the most common being gastrointestinal bleeding (Fung and Kirschenbaun 1999) such as, gastro intestinal ulcerations. This explains the fact that new compounds are still needed to fight against those diseases mentioned above.
Inflammation and pain remain inadequately managed everywhere, despite the large number of anti-inflammatory and analgesic drugs, sometimes used in association, most people in developing countries have poor access to modern health care. Therefore, pharmacological validation of medicinal plants or ethnomedical treatment methods could greatly benefit populations with poor economic resources. In Cameroon, the floral biodiversity has enabled the development of such an alternative low-cost therapies from which plants are selected as remedies, and/or as ingredients to prepare herbal medicines to manage various human ailments. Allanblackia gabonensis (Guttiferae) is a medicinal plant found in tropical Africa (Bamps 1970). Crude extract of stem bark of this plant is used locally to enhance sexual energy. The stem bark and seeds of A. gabonensis are also used for analgesic effect to relieve pain and the decoction is used to treat rheumatism.
Phytochemical investigation has demonstrated that Allanblackia genus contains compounds which belong to the phytosterols, xanthones, biflavonoids and alkaloids classes (Azebaze et al. 2004, 2006). The phytochemical study of the stem bark of A. gabonensis has resulted in the isolation and characterization of xanthone derivatives, named allanxanthone D, allanxanthone A, 1,5-dihydroxyxanthone, 1,7-dihydroxyxanthone and 1,3,6,7-tetrahydroxy-2-(3-methylbut-2-enyl)xanthone, forbexanthone, 6-deoxyisojacareubin, one polyisoprenylated benzophenone, guttiferone F, one flavanol, epicatechin, two phytosterols, β-sitosterol and campesterol (Azebaze et al. 2008).
Moreover methanolic and aqueous extract of stem bark of A. gabonensis were found to be non-toxic or less toxic when oral acute and subacute toxicities were performed (results not published).
In continuation of our pharmacological studies on bioactive constituents of Cameroonian plants (Dongmo et al. 2003, 2004, 2005), we have found that the stem bark extract of A. gabonensis which is the form of extract used by traditional healer is easy to prepare by native population.
The aim of the present study was to evaluate the analgesic and antiinflammatory effects of A. gabonensis stem bark aqueous extract on experimentally induced pain and inflammation.
Materials and methods
Plant material
The stem bark of A. gabonensis were collected in June 2007 from Kola Mountain at Nkolbisson, Yaoundé, Center Province, Cameroon and identified by authorized botanist at the National Herbarium where a voucher specimen No. 23255/SRF/Cam is deposited for future reference.
Preparation of extract
The air dried stem bark was powdered (1,000 g) and extracted by decoction in distilled water for 15 min and kept cool for 1 h. After filtration, the filtrate was concentrated in oven at 55°C giving brown residue yielding 83 g (8.3%).
HPLC analysis
High-Performance Liquid Chromatography (HPLC) test was performed to determine the type of compounds present in the extract.
Samples of aqueous extract of A. gabonensis were analysed without any treatment. 5 mg dried extract is dissolved in 1 ml water, filtered over Millipore filtration unit, type 0.45 μm and injected into the HPLC apparatus.
HPLC analysis was carried out using Knauer HPLC equipment containing Jasco multiwavelength detector MD-910, two pumps type Jasco Intelligent Prep. Pump PU-987 with mixing chamber, injection valve (type Rheodyne). The column used was an Eurochrom 4.6 × 125 mm without pre-column, the stationary phase was nucleosil NP 100-C18 with particle size 5 μm. The injection volume was 20 μl, mobile phase consisted of water (pH = 2.5) acidified with phosphoric acid and (solvent A), acetonotrile (solvent B). The linear gradient profile was 0–15 min, 10–30% B, 15–30 min, 45–75% B. The data were acquired using a photodiode array detector in the range 190–370 nm. Data acquisition were performed using HPLC software V2.22.
Animals
Wistar rats (120–150 g) and Swiss albino mice (20–25 g) of both sexes were used for this study. Animals were bred in the animal house of the Faculty of Science, University of Yaounde I. They were fed with standard food and water ad libitum. The animals were fasted (with free access to water) overnight before treatment. The ‘principle of laboratory animal care’ was followed in this study (Covino et al. 1980). Prior authorization for the use of laboratory animals in this study was obtained from the Cameroon National Ethical Committee (Reg. N° FWAIRD 0001954).
Pharmacological activities
Anti-inflammatory activity
Carrageenan-induced paw oedema
Carrageenan-induced paw inflammation was produced according to the method described by Winter et al. (1962). One hour after (preventive effect) or before (curative effect) oral administration of the aqueous extract of A. gabonensis (100, 200 and 400 mg/kg), reference drug (indomethacin, 10 mg/kg) or vehicle (distilled water), an injection of 0.1 mL of carrageenan (1% carrageenan suspended in 0.9% NaCl) was made into the right hind limb of each rat under the sub-plantar aponeurosis.
Measurement of paw size was done by means of volume displacement technique using plethysmometer (Ugo Basile no. 7140) immediately before carrageenan injection and 1/2, 1, 2, 3, 4, 5 and 6 h (preventive test) and 4, 4.5, 5, 6 and 24 h (curative test) after carrageenan injection.
Percentages of inhibition were obtained using the following ratio:
Vt is the average volume for each group after treatment and Vo is the average volume for each group before any treatment (Lanhers et al. 1991).
Histamine and serotonin induced paw oedema
The anti-inflammatory activity of the aqueous extract of A. gabonensis was tested with two phlogistic agents (histamine, serotonin). The paw oedema was induced in the rats by sub-plantar injection of freshly prepared histamine (0.1 mL of a 10−3g/mL), and serotonin (0.1 mL of a 10−3 g/mL) solutions, respectively (Singh et al. 1996). The paw volume was recorded at 0 and 1 h after histamine injection (Parma and Ghosh 1978) or 0 and 30 min after serotonin injection (Ghosh and Singh 1974). The drugs (aqueous extract of A. gabonensis, references products and vehicle) were administered orally 1 h before eliciting paw oedema.
Analgesic activities
Acetic acid-induced pain
The method used in this test has been described by Koster et al. (1959). The total number of writhings following intraperitoneal administration of acetic acid solution (1%, 10 mL/kg) was recorded over a period of 30 min, starting 5 min after acetic acid injection. The mice were treated with the aqueous extract of A. gabonensis (100, 200 and 400 mg/kg) or water (vehicle) or standard drug (Aspirin, 200 mg/kg), 30 min before administration of acetic acid. The number of writhings and stretching was recorded and permitted to express the percentage of protection using the following ratio: (control mean-treated mean) × 100/control mean (Dongmo et al. 2005).
Formalin-induced pain
The animals were injected with formalin (1.4%, 20 μL) into the sub plantar area of the left hind paw of the mice. Extract (100, 200 and 400 mg/kg), aspirin 200 mg/kg, tramadol (20 mg/kg) or distilled water were administered p.o. 30 min before the injection of formalin. These mice were individually placed in a transparent plexiglas cage and observed. The duration of paw licking was recorded at the early phase (1–5 min) and late phase (15–30 min) after formalin injection.
Hot plate-induced pain
The heated surface of a hot plate analgesia meter (Ugo Basil, Italy; Socrel DS-37) was maintained at 55 ± 0.2°C. Each animal was placed into a glass cylinder (diameter 20 cm) on the heated surface of the plate. Licking of paws and jumping evaluated as the parameters of the thermal reactions were registered (Lanhers et al. 1991). In order to minimize damage to the animal paw, the cut-off time for latency of response was taken as 20 s (Shalheen et al. 2000). The mouse was treated with aqueous extract (100 or 200 mg/kg), tramadol (20 mg/kg) or vehicle (distilled water) 30 min before being placed on the hot plate. The time for licking and jumping of any mice was taken before administration of different products and then taken at 0, 0.5, 1, 2, 3, 4, 5, 6 h after this administration. The following formula was used to calculate the percentage of inhibition (Asongalem et al. 2004).
-
Tb: Average time after treatment
-
Tb: Average time before treatment
Tail-immersion test
The procedure described by Aydin et al. (1999) was used to conduct this test. 3 cm of the tail was introduced in hot water at a temperature of 55 ± 0.5°C. Within a few minutes, the rat reacted by withdrawing the tail. The reaction time was recorded with a stopwatch, in this test each animal served as its own control and two readings were obtained for the control at 0 and 10 min interval. The average of the two values was the initial reaction time. The animals were treated by the extract (100, 200 mg/kg), tramadol (20 mg/kg), or vehicle 30 min before the immersion of the tail. The time reaction is taken at 0, 0.5, 1, 2, 3, 4, and 6 h after administration of different products.
Paw pressure test
The paw pressure test has been previously described by Randall and Selitto (1957). The test was carried out on rats using Ugo basile analgesy meter (7200). In these experiments, a force was applied to the left hind paw of the experimental animals using the Ugo Basile analgesy-meter. This instrument generates a linearly increasing mechanical force or pressure by a dome-shaped on the dorsal surface on the rat’s hind paw. The rat was suspended vertically while its left hind paw was placed between the plinth and the finger. As the applied pressure increases, it gets to a point where the animal struggles to free its paw. This is the level at which the animal feels pain (Dongmo et al. 2003). The pressure causing pain before treatment, 30 min and 2 h after treatment of the animals with the aqueous extract (100, 200 and 400 mg/kg) and the reference drug (tramadol, 20 mg/kg) was determined.
Statistical analysis
The results were presented in tables as mean ± SEM and the comparisons within the experimental groups made using one way analysis of variance (ANOVA) followed by Dunnett’s test. P value less than 0.05 was considered as indicative of significance.
Results
HPLC analysis
A correct assignment to the various compounds was not possible. From UV spectra and retention times of the main peaks, some compound classes contained in the extract have been determined. High-Performance Liquid Chromatography (HPLC) revealed the presence of phytosterols, xanthone (derivatives), epicatechin and polyphenol (derivatives) (Fig. 1).
Anti-inflammatory activity
Effects of the aqueous extract on carrageenan-induced oedema
In the carrageenan-induced oedema test, the paw volumes and percentages of inhibition by the aqueous extract of A. gabonensis and standard drugs are shown in Table 2.
Injection of carrageenan was done 1 h after oral administration of the extract (100, 200, and 400 mg/kg), indomethacin (reference drug) and water. Measurement of paw size was taken before carrageenan injection and then 0, 0.5, 1, 2, 3, 4, 5 and 6 h after carrageenan injection. The aqueous extract of A. gabonensis at the preventive test showed a significative inhibition of paw oedema starting from the first hour up to the sixth hour. A maximal volume of oedema (0.12 ml) with inhibition percentage of about 74.01% at a dose of 200 mg/kg was obtained 6 h following carrageenan injection (Table 1). In the curative test, the extract reduced paw oedema at a maximum percentage of 42.76% was obtained 24 h after treatment with extract at a dose of 200 mg/kg (Table 2). The reference drug, indomethacin (10 mg/kg) used in this experiment showed a maximum inhibition of paw oedema of about 64.44% (6 h) in the preventive test and 23.02% in the curative test.
Effects of the aqueous extract on paw oedema induced by serotonin and histamine
Table 3 shows the effect of the aqueous extract of A. gabonensis on paw oedema induced by histamine and serotonin. The plant extract exhibited a significant reduction of paw oedema induced by both histamine and serotonin with a maximal inhibition of 56.94% (200 mg/kg) and 40.83% (100 mg/kg), respectively. Promethazine and prednisone used as reference drugs decreased paw oedema inflammation volume induced by serotonin and histamine for 38.91 and 44.44%, respectively.
Analgesic activity
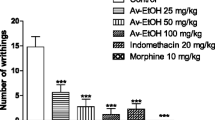
Writhing test
The aqueous extract of A. gabonensis (100, 200 and 400 mg/kg) significantly and dose dependently reduced the number of abdominal constriction induced in mice by a solution of acetic acid 1%. This dose-dependent protective effect reached a maximum inhibition of 84.38% at the dose of 400 mg/kg. Acetylsalicylic acid exerted a significant protective effect, inducing a protection of 51.84% at a dose of 100 mg/kg (Table 4).
Formalin test
The extract of A. gabonensis at any dose used (100, 200, 400 mg/kg) had significant effects on both first (0–5 min) and second phases (15–30 min) of formalin test as shown in Table 5. The maximum percentage of inhibition was 67.18% (200 mg/kg) at the first phase and 83.87% (400 mg/kg) at second phase. The positive control drugs, aspirin (100 mg/Kg) and tramadol (20 mg/kg), significantly attenuated the pain responses on the two phases. In the presence of naloxone, the plant extract produced 77.58% of inhibition during the late phase.
Hot-plate test
The results of hot-plate test are reported in Table 6. The administration of A. gabonensis (100, 200, 400 mg/kg) and tramadol (20 mg/kg, i.p.) significantly increased the reaction time to the nociceptive response in the hot plate when compared with control group.
Tail immersion
As presented in Table 7, A. gabonensis administrated at doses of 100–400 mg/kg caused a light increase in the tail-flick response latency time as compared to the control with a significant values 30 min (200 mg/kg), 1 h (400 mg/kg), 3 h (200 and 400 mg/kg) and 4 h (400 mg/kg) after the treatment. The maximum effect was observed after the treatment with tramadol with a percentage of inhibition reaching 87.33% (0.5 h).
Paw pressure test
Table 8 shows that A. gabonensis at a dose of 100 mg/kg significantly increased the paw pressure-induced force at which pain was felt from 67.5 g in the controls to 118 g, 0.5 h after administration of the extract. At a dose of 400 mg/kg, the extract exerts maximum and significant protective effect, inducing a protection of 80.85% (from 87 g to 127.5 g) 3 h after administration of the extract. Tramadol (20 mg/kg) was equally effective as the extract of A. gabonensis reducing sensitivity to pain at the dose tested.
Discussion
The present study assessed the pharmacological effects of the stem back of A. gabonensis for its anti-inflammatory and analgesic activities, using chemical (acetic acid and formalin) and mechanical stimuli.
Carrageenan-induced rat paw is a suitable experimental animal model to evaluate the anti-oedematous effect of natural products and is believed to be biphasic; the first phase (1 h) involves the release of serotonin and histamine and second phase (over 1 h) is mediated by prostaglandins, cyclooxygenase products, and the continuity between the two phases is provided by kinins (Periaayagam et al. 2006). Aqueous extract of A. gabonensis significantly reduced oedema in all the three phases in preventive treatment as well as in curative treatment. This anti-inflammatory response was also significant in rats pretreated with indomethacin, a known non specific cyclooxygenase inhibitor.
To ascertain the effect of the aqueous extract of A. gabonensis, different inflammatory mediator agents were used as oedemogens. It was observed that the aqueous extract of A. gabonensis was able to inhibit oedema induced by histamine and also that provoked by serotonin. Both histamine and serotonin are characterised by the increase of vascular permeability. Our results have also demonstrated that promethazine and prednisone, used as standard drug exhibited significant activity against histamine- and serotonin-induced oedema, respectively. These results suggest a possible interaction of our extract with the liberation and/or action of endogenous histamine and serotonin.
Since the inflammation process is also characterised by the production of leukotrienes from lipoxygenase degradation and prostaglandins from cylooxygenase (Zhang and Cuzzucrea 2000; Jain et al. 2001) in the late phase of oedema induces by carrageenan, the reduction of the oedema in this phase by the extract indicates that A. gabonensis may act through the pathway of arachidonate metabolism.
The antinociceptive activity of the aqueous extract of A. gabonensis was evaluated using acetic acid-induced writhing, formalin test, hot-plate test, tail immersion and paw pressure test. The aqueous extract of A. gabonensis significantly inhibited the acetic acid-induced writhings in mice, which are related to the increase in the peritoneal fluids levels of PGE2 and PGF2 (Deraedt et al. 1980). Locale peritoneal receptors are postulated to be partly involved in abdominal writhing response (Bentley et al. 1999; Spereni et al. 2005). Moreover, intraperitoneal injection of acetic acid produced pains through activation of chemosensitive nociceptors (Stai et al. 1995) or irritation of the visceral surface, which lead to the liberation of histamine, bradykinin, prostaglandins and serotonin (Schowb and Dubost 1984; Garcia et al. 2004). Thus, antinociceptive activity of opioid agonist, opioid partial agonist and non-steroidal anti-inflammatory agents can be determined by writhing test. Since A. gabonensis extracts were active in this type of pain, they may belong to at least one of these classes of analgesics. In order to assess the mechanism of action of these extracts their effects were tested on the pain induced by formalin.
In order to assess the mechanism of action of these extracts their effects were tested on the pain induced by formalin. It is well-known that formalin test involves two phases: neurogenic with release of substance P and inflammatory with release of serotonin, histamine, bradykinin and prostaglandins (Murray et al. 1988; Tjolsen et al. 1992; Gaertner et al. 1999, Sayyah et al. 2004). According to Stai et al. (1995), the peripheral analgesics as aspirin preferentially inhibit the second phase whereas the narcotic analgesics inhibit the two phases. The fact that the extracts of A. gabonenis significantly inhibited the two phases of the pain induced by formalin suggests that they may act as narcotic analgesics. It has also been reported that methylene chloride fraction of A. monticola on nociceptive response in the late phase of formalin test suggesting that the anti-nociceptive might be due to its peripheral (or anti-inflammatory) action (Nguemfo et al. 2007). The significant and potential inhibition effect of the aqueous extract of A. gabonensis on both first and second phases of formalin test suggest that it possesses both central and peripheral action. To corroborate that the extract had central analgesic actions, hot-plate and tail-immersion tests (Knoll 1967) were conducted. Significant results noted for aqueous extract in immersion test and hot-plate test (a test suitable for identifying centrally and not peripherally acting analgesics) were due to central acting activities of the extract. This means that the opioid-like receptors are involved.
The peripheral activities of the extracts were also tested on the pain induced by pressure, which is a model for the study of non-inflammatory pain. In this model, pain seems to be due to sensitisation of sensory nerves and the involvement of endogenous substances such as prostaglandins may be minimized. The significant activity of the extracts on this model of pain suggests that they may protect nociceptors. It can then be concluded that extracts from A. gabonensis act as peripheral and narcotic analgesics.
The chemical analysis of the genus Allanblackia indicated the presence of a number of alkaloids, phytosterols, triperpenes and phenols. Some of these compounds have also been isolated on A. gabonensis (Azebaze et al. 2008). It has been reported that these classes of compounds possessed various important pharmacological activities including anti-inflammatory activity (Geetha and Varalakshmi 2001). According to these studies, the analgesic and anti-inflammatory activity of aqueous of A. gabonensis might be due to its content in xanthones and triterpenes.
In conclusion, our results shows that the aqueous extract of A. gabonensis possess a central, peripheral antinociceptive activity and anti-inflammatory activity. This finding support the use of A. gabonensis in traditional medicine for treatment of some painful and inflammation disorders and confirmed the presence of biologically active principles in the plant extract. Follow-up studies will concentrate on the study of the effects of A. gabonensis on prostaglandin synthesis, and lipoxygenase and cyclooxygenase activities to establish its possible mechanism of action.
References
Asongalem EA, Foyet HS, Ngogang J et al (2004) Analgesic and anti inflammatory activities of Erigeron floribundeus. J Ethnopharmacol 91:301–308
Aydin S, Demir T, Ozturk Y et al (1999) Analgesic activity of Nepeta italica L. Phytother Res 13:20–23
Azebaze AGB, Meyer M, Bodo B et al (2004) A new polyisoprenylated xanthones from the stem bark of Allanblackia monticola. Phytochemistry 65:2789–2795
Azebaze AGB, Meyer M, Valentin A et al (2006) Prenylated xanthone derivatives with activity from Allanblackia monticola Staner L.C. Chem Pharm Bull 54:111–113
Azebaze AGB, Ouahouo BMW, Vardamides JC, Valentin A, Kuete V, Acebey L, Beng VP, Nkengfack AE, Meyer M (2008) Antimicrobial and antileishmanial xanthones from the stem bark of Allanblackia gabonensis Chem Nat Comp 44:582–587
Bamps P (1970) Flore du Congo, Rwanda et Burundi, Spermaphytes Guttiferae 40
Bentley GA, Newtown SH, Starr J (1999) Analgesic activity of Nepeta italica L. Phytother Res 13:20–23
Covino BG, Dubner R, Gybels J et al (1980) IASP committee for research and ethical issues ethical standards for investigations of experimental pain in animals. Pain 9:141143
Deraedt R, Jougney S, Benzoni J et al (1980) Release of prostaglandins E and F in algogenic reaction and its inhibition. Eur J Pharmacol 61:17–24
Dongmo AB, Salah M, Kamanyi A et al (2003) Anti-inflammatory and analgesic properties of the stem bark extract of Mitragyna ciliata in rats. J Ethnopharmacol 84:17–21
Dongmo AB, Salah M, Kamanyi A et al (2004) Vasodilating properties of the stem bark extract of Mitragyna ciliata in rats and guinea pigs. Phytother Res 18:36–39
Dongmo AB, Ngueefack TB, Lacaille-Doubois MA (2005) Anti-nociceptive and anti-inflammatory activities of Acacia pennata Wild (Mimosaceae). J Ethnopharmacol 98:201–206
Fung HB, Kirschenbaun HL (1999) Selective cyclooxygenase-2 inhibitors for the treatment of arthritis. Clin Ther 221:1131–1157
Gaertner M, Muller L, Roos JF, Cani G, Santos ARS, Niero R, Calixto JB, Yunes RA, Delle Manache F, Cechinel-Filho V (1999) Analgesic triterpenes from Sebastiania schottiana roots. Phytomedicine 6:41–44
Garcia MD, Fernandez MA, Alvarez A, Saenz MT (2004) Antinociceptive and anti-inflammatory effect of the aqueous extract from leaves of Pimento racemosa var. ozua (Mimosaceae). J Ethnopharmacol 91:69–73
Geetha T, Varalakshmi P (2001) Anti-inflammatory activity of lupeol and linoleate in rats. J Ethnopharmacol 76:77–80
Ghosh MN, Singh H (1974) Inhibitory effect of a pyrrolizine alkaloid, crotalaburnine, on rat paw oedema and cotton pellet granuloma. Br J Pharmacol 51:503–508
Insel PA (1996) Analgesic, antipyretic and ant-inflammatory agents and drugs employed in the treatment of gout. In: Hardman JG, Limbord LE (eds) Mcgraw-Hill, New york. pp 617–657
Jain NK, Kulkami SK, Singh A (2001) Role of cysteinyl leukotrienes in nociceptive and inflammatory conditions in experimental animals. Eur J Pharmacol 415:85–94
Knoll J (1967) Screening and grouping of psychopharmacological agents. In: Siegler PE, Mover HJ (eds) Animal and clinical pharmacologic techniques in drug evaluation. Yearbook Med. Publishers. Inc, Chicago, pp 305–321
Koster R, Anderson M, De Beer J (1959) Acetic acid for analgesic screening. Fed Proceed 18:412–417
Lanhers MC, Fleurentin J, Dorfman P et al (1991) Analgesic, antipyretic and anti-inflammatory properties of Euphorbia hirta. Planta Med 57:225–231
Murray CW, Porreca F, Cowan A (1988) Methodological refinement in the mouse paw formalin test: an animal model of tonic pain. J Ethnopharmacol Methods 20:175–186
Nguemfo EA, Dimo T, Azebaze AGB et al (2007) Anti-inflammatory and antinociceptive activities of the stem bark extracts from Allanblackia monticola STANER L.C. (Guttiferae). J Ethnopharmacol 114:417–424
Parma NS, Ghosh MN (1978) Anti-inflammatory activity of gossypin a bioflavanoid isolated from Hibiscus vitifolius Linn. Ind J Pharmacol 10:277–293
Periaayagam JB, Sharma SA, Pillai KK (2006) Anti-inflammatory activity of Trichodesma indicun root extract in experimental animal. J Ethnopharmacol 104:410–414
Randall LO, Selitto JJ (1957) A method for measurement of analgesic activity on inflamed tissue. Arch Int Pharmacodyn 61:409–419
Sayyah M, Hadidi N, Kamalinejad M (2004) Analgesic and anti-inflammatory activity of Lactuca sativa seed extract in rats. J Ethnopharmacol 92:325–329
Schowb M, Dubost MC (1984) Entendre la douleur. Pharmapost, RC Montargis, p 99
Shalheen HM, Badreldin HA, Alquarawi AA et al (2000) Effect of Psidium guajava leaves on some aspects of the central nervous system in mice. Phytother Res 14:107–111
Singh G, Ramey DR, Shi H et al (1996) Gastrointestinal tract complications of non-steroidal anti-inflammatory drug treatment in rheumatoid arthritis. Arch Intern Med 156:1530–1537
Spereni E, Cervellati R, Innocenti G et al (2005) Anti-inflammatory, anti-nociceptive and antioxidant activities of Halanites aegyptica (L) Delile. J Ethnopharmacol 98:117–125
Stai HY, Chen YF, Wu TS (1995) Anti-inflammatory and analgesic activities of extract from roots of Angelica pubescens. Planta Med 61:1–8
Tjolsen A, Berge DG, Hunskaar S et al (1992) Popular medicine of the central plateau of Haiti-2. Ethnopharmacological inventory. J Ethnopharmacol 17:13–30
Winter CA, Risley EA, Nuss GW (1962) Carrageenan-induced oedema in hind paw of rat: an assay for anti-inflammatory drugs. Proc Soc Exp Biol Med 111:544–547
Zhang J, Cuzzucrea S (2000) GP16150, a poly adp-ribose polymerase inhibitor, exhibits an anti-inflammatory effect in at models of inflammatory. Auton Neurosci Basic Clin 85:141–147
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ymele, E.V., Dongmo, A.B. & Dimo, T. Analgesic and anti-inflammatory effect of aqueous extract of the stem bark of Allanblackia gabonensis (Guttiferae). Inflammopharmacol 21, 21–30 (2013). https://doi.org/10.1007/s10787-011-0096-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-011-0096-2