Abstract
To provide financial protection against catastrophic illness, the Korean government expanded the National Health Insurance (NHI) benefit coverage for cancer patients in 2005. This paper examined whether the policy improved the income-related equality in health care utilization. This study analyzed the extent to which the policy improved income-related equality in outpatient visits, inpatient days, and inpatient and outpatient care expenditure based on triple difference estimator. Using nationwide claims data of the NHI from 2002 to 2004 and from 2006 to 2010, we compared cancer patients as a treatment group with liver disease as a control group and low-income group with the highest-income group. The results showed that the extension of NHI benefits coverage led to an increase in the utilization of outpatient services across all income groups, but with a greater increase for the low-income groups, among cancer patients. Moreover, the policy led to a less decrease in the utilization of inpatient services for the low-income group while it decreased across all income groups. Our finding suggests that the extension of NHI benefits coverage improved the income-related equality in health care utilization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Out-of-pocket (OOP) payments for health care in Korea are high compared to other Organisation for Economic Co-operation and Development (OECD) countries although it has National Health Insurance (NHI) covering the entire population. For example, public spending accounted for 58.2 % of the total health care expenditure in Korea while the OECD average was 72.2 % in 2010 (OECD 2012). The public share in total health expenditure in Korea is only slightly higher than that in the United States of America and Mexico among OECD countries. High OOP payments have caused concerns about the heavy burden of medical expenses and the financial barrier to health care access in Korea (Ruger and Kim 2007). If the majority of health expenditure is from OOP payment, health care utilization may be skewed toward the better-off (O’Donnell et al. 2008a, b; Veugelers and Yip 2003).
Heavy reliance on OOP payments, despite NHI system in Korea, results from limited benefit coverage of the NHI scheme. The Korean government established the health insurance system as a part of economic development and for the legitimization of the former military regime (Song 2003). As the government wanted to minimize the risk of fiscal deficits caused by the insurance system, NHI started with stringent benefit packages by providing coverage for a limited number of services with high copayments (Kwon 2007). Individuals were liable for the full cost of services that were not covered by NHI, and households faced higher financial risk when they had a catastrophic illness. Policies to expand NHI benefit coverage were implemented intensively by the then progressive government around the year 2005. For example, the NHI system reduced cost sharing from 20–50 to 10 % for catastrophic illnesses such as cancer and cardio-cerebrovascular diseases, and the benefit package was expanded to advanced treatment and expensive drugs for cancer patients in 2005.
Previous studies demonstrated that the reform led to overall improvement in access to care and service utilization (Bae 2010; Lee 2009). However, there are few studies which investigate whether the policy had an effect on the equality in health care utilization. It is important to monitor the impact of the policy on health care utilization among people with low socio-economic status, because benefits from the policy may be unevenly distributed across socio-economic status (Liu et al. 2002; Mackenbach et al. 2004). There is one study which examined the impact of the benefit coverage expansion for cancer patients on healthcare equality (Kim et al. 2008), but it was carried out immediately following the introduction of the policy and only presented the extent of the equality in healthcare utilization before and after the introduction of the policy without comparing the individuals who were impacted by the policy with those who were not.
This study aims to examine the impact of the policy to expand benefit coverage for cancer patients in 2005, which was one of the main policies implemented in order to improve financial protection. We evaluated the impact of the policy on income-related equality in health care utilization. In this study, the definition of equality in health care utilization was based on horizontal equality, “an equal treatment for equal need” (Lu et al. 2007). We assumed that all cancer patients had the same need. Thus, if policy increases utilization for the lowest income quintile more than for the highest income quintile, it is regarded as an improvement of equality, even if the high-income group still utilizes medical care more than the low-income group does even after the introduction of the policy. We estimated the effect of the policy with the difference-in-difference (DID) method comparing cancer patients as a treatment group with liver-disease patients as a control group using NHI claims data from 2002 to 2010. We also used triple difference (TD) estimation to evaluate the extent to which the policy had an effect on health care utilization across different income groups, comparing cancer patients with liver-disease patients and the low-income group with the high-income group.
Our findings showed that after benefit coverage was expanded, low-income cancer patients experienced a larger increase or smaller reduction in service utilization. In other words, government policy had a positive impact on equity in health care utilization, favoring low-income patients.
The paper is organized as follows. The next section describes our empirical strategy and data. The result section gives the findings of our analysis. We conclude the paper with a discussion of the implications of our findings, limitations of our study, and suggested areas for future research.
Methods
Data
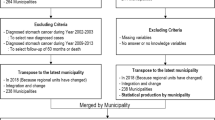
We used data from 2002 to 2004 (i.e. pre-policy) and from 2006 to 2010 (i.e. post-policy), taken from the Korean NHI database, which includes electronic insurance claims data for all citizens. The database contains descriptions of services that are provided in all medical institutions and reimbursed by the NHI. It also contains patients’ demographic information, including age, gender, and health insurance contribution, and indicators of health care utilization such as type of services, diagnostic codes (ICD-10), the number of consultation, and medical expenses.
For the treatment group, we collected patient records with the diagnostic code of cancer identified by the corresponding ICD-10 codes C00–C97 (malignant neoplasm); for the control group, we collected patient records with the diagnostic code of liver disease identified by the corresponding ICD-10 codes, K70–K77. Patients whose claims records showed at least a single hospitalization or more than two outpatient visits with the same disease code were included, and patients who were treated for both diseases in the same year were excluded. We also only included patients aged 20–64 because the level of cost-sharing for other age groups changed during the study period and elderly people have different severity of disease and different treatment patterns from younger people.
Variables
We analyzed health care utilization using inpatient days and outpatient visits, annual health care expenditure of inpatient and outpatient care, and expenditure per visit and day as measures of intensity of treatment. Health care expenditure are total expenses for medical consultations and hospitalization, comprising co-paid OOP expenses and reimbursement paid by the NHI. Health expenditure was adjusted by the annual increase in health care fees scheduled with 2010 as the base year.
The variables used in the analysis were those available from the database (Table 1). We adopted income as a main measure of socio-economic status. The income variable was constructed based on the NHI contribution data, which was determined using income, property and so on. We defined income quintiles, ranking all NHI subscribers into quintile in order of the NHI contribution. That is, we used quintile from the entire population. Other variables affecting health care utilization, such as gender, age, disability and death, were included. We analyzed inpatient days and outpatient visit days using negative binomial distribution and all types of expenditure using log-transformation.
Methods
We estimated the impact of the expanded benefit coverage on income-related equality in health service utilization, using DID methodology which has been widely applied in policy evaluation (Chen et al. 2007; Liao et al. 2012; Liu et al. 2002; Mott et al. 2010; Polsky et al. 2009). DID models estimate the effect of policies by comparing pre and post differences in the outcome of treatment groups (composed of people affected by the policy) with that in the outcome of control groups (composed of people not affected by the policy). We defined the control group as liver-disease patients that were not entitled to the extension of benefit coverage though it was a serious illness. On the other hand, cancer patients who were entitled to the policy were regarded as the treatment group.
In the first place, we assessed the effect of the policy on health care utilization of cancer patients by comparing them with liver-disease patients. If \(y_{ijt}\) is the outcome of interest for individual i in group j (such as a treatment group or a control group) by time t (such as a year), the corresponding DID specification reads as the following regression framework where \(y_{ ijt}\) indicates the variable on health service utilization:
As the distribution of variables such as expenditure are skewed substantially to the right, we performed a natural log transformation to cost information (O’Donnell et al. 2008a, b). We applied the negative binomial regression model to the analysis of outpatient visits and inpatient days in order to deal explicitly with the characteristics of our count outcome (J.S. Long 1997).
Dummy variable ‘\(cancer_{j}\)’ equals one if an individual \(i\) is a cancer patient and zero otherwise; ‘\(post policy_{t}\)’ is a dummy variable equal to one for observations from 2006–2010 (i.e. after the introduction of the policy) and zero otherwise; \(x_{ijt}\) are exogenous variables including age, gender, disability, and survival status; \(e_{ijt}\) is an error term.
In equation (1), the parameter \(\beta _{1}\) measures the change in health service utilization during the period of pre- and post-2005 in the control group. The coefficient on ‘\(cancer',\beta _{2}\), captures any differences in health service utilization between the control group and the treatment groups within the pre-policy period. The coefficient of interest \(\beta _{3}\) for the interaction term (\(cancer \times post policy\)) measures the change in health service utilization associated with the introduction of the policy for cancer patients. In this equation, we will reject the null hypothesis of no positive effects of the policy on health care utilization if the coefficient on the interaction term of ‘cancer’ and ‘post policy’ is significantly positive.
Next, we estimated the extent to which the policy improves income-related equality in health service utilization, using a TD estimator to compare cancer patients with liver-disease patients and the lowest-income group with the highest-income group. The corresponding TD specification reads as follows where the interaction term of ‘cancer’, ‘post policy’ and ‘income’ is added to equation (1) to estimate the effects of the policy on health care utilization across different income groups:
The coefficient \(\beta _{7}\) of the interaction term (\(income \times post policy\times cancer\)), measures the change in health service utilization across different income groups associated with the introduction of the policy for cancer patients. Thus, we will reject the null hypothesis of no positive effects of the policy on equality in health care utilization if the coefficient on the interaction term of ‘cancer’, ‘post policy’ and ‘income’ is significantly higher in lower-income quintiles.
Meanwhile, we estimated standard errors considering serial correlation. Bertrand et al. (2004) found that serial correlation had an especially large effect on standard errors in DID models using long-term data because the binary treatment variable changed only once and was highly correlated through time. That is, it can lead to a severe bias in conventional standard error estimates. Thus, we estimated cluster-robust standard errors, creating 20 clusters using income quintiles by treatment group by gender. Data analysis was performed with SAS 9.2 software.
Results
Table 2 provides the descriptive statistics for the variables associated with inpatient care utilization before and after the introduction of the policy. The total numbers of patients were 438,391 before the policy and 770,747 after the policy change. The distribution of each variable is different before and after the introduction of the policy. For example, the proportion of cancer patients increased after the policy was introduced. The proportions of male patients and older patients were greater than their counterparts before the policy was implemented, and the proportion of female patients and older patients increased compared to their counterparts after the policy was introduced. The distribution of patients according to income level showed that the proportion of high-income patients was greater than low-income patients and increased slightly more than that of low-income patients after the policy. Particularly, the proportion of high-income patients increased more in cancer patients than in liver disease patients after the policy
Table 3 shows the descriptive statistics for the variables associated with outpatient care utilization before and after the policy change. The total numbers of patients in the two disease groups were 3,503,512 before the policy and 5,364,821 after the policy. After the introduction of the policy, the proportion of cancer patients increased compared to that of liver disease patients. Furthermore, the number of high-income patients increased more than low-income patients after the implementation of the policy, and the number of high-income patients increased more in the cancer group than in the liver disease group after the policy change.
The effect on inpatient care utilization across income groups
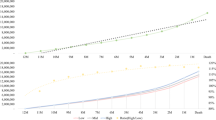
Table 4 presents the results of DID and TD analyses comparing inpatient care utilization of cancer patients with that of liver disease patients. In the DID model, the effect of the policy is captured by the coefficients of the interaction term ‘post cancer’. In model 1, the coefficient on the interaction term is negative and significant, \(-\)0.047, which means that the policy led to a reduction in annual inpatient days of cancer patients, compared to liver disease patients. In model 5, the coefficient of the interaction term is positive and significant, 0.101, which means that inpatient expenditure per day increased for cancer patients after the implementation of the policy, compared to liver disease patients.
We can identify the effect of the policy across different income groups based on the TD model, which compares the lowe-income group with the high-income group and cancer patients with liver disease patients. In model 4 and 6, several coefficients of the interaction term ‘post cancer income i’ are positive and partially significant, which means that annual inpatient expenditure and daily expenditure of low-income cancer patients increased more than those of the highest-income patients after the introduction of the policy, compared with liver disease patients. In model 2, the coefficient of the triple interaction term is positive but rarely significant, which implies that the effect of the policy is not significantly different across different income groups. Thus, the policy has positive impacts on inpatient expenditure and daily expenditure of cancer patients, favoring low-income patients.
The effect on outpatient care utilization across income groups
Table 5 demonstrates the results of the DID and TD analyses comparing outpatient care utilization of cancer patients with that of liver disease patients. In model 1, 3 and 5, the coefficients of the interaction term ‘post cancer’ are positive and significant, 0.241, 0.392 and 0.090, respectively, which means that the implementation of the policy led to the increased frequency of outpatient visits, annual expenditure and daily expenditure of cancer patients, compared to those of liver disease patients.
The effect of the policy on outpatient care utilization across different income groups is identified using the TD model. In model 2, 4 and 6, the coefficients of the interaction term ‘post cancer income i’ are positive and partially significant, which means that the number of consultations, annual expenditure and daily expenditure increased more among low-income cancer patients than the highest-income ones, compared with liver-disease patients. In other words, the expanded benefit coverage has contributed to improving income-related equality in outpatient care utilization of cancer patients, with a greater increase in utilization for the low-income people.
Discussion and conclusion
Though many policies are likely to have an impact on health inequalities, there has been a paucity of studies evaluating the impact of government policy on inequalities and exploring the mechanisms of inequalities in Korea (Khang and Lee 2012). This analysis attempts to address the equality issue by assessing the relative changes in health care utilization across different income groups after the NHI benefit coverage was expanded to cancer patients in Korea.
By exploiting the DID approach on a nationwide claims data set, our results show that health service utilization for outpatient and inpatient care increased more in the low-income group than in the high-income group after the expansion of NHI benefit coverage for cancer patients. More specifically, we found that cancer patients utilized more services in outpatient care, not in inpatient care, after the implication of the policy. After benefit coverage was expanded, low-income cancer patients were likely to experience a larger increase or smaller reduction in service utilization in terms of number of outpatient visits, annual expenditure of inpatient and outpatient care, and expenditure per day. In other words, policy had a positive impact on equality in health care utilization, favoring low-income patients.
One study that examined the impact of expanded benefit coverage on health care equality presented concentration index of health care utilization before and after the policy change. The study suggested that the policy reduced inequality, particularly in inpatient care utilization by cancer patients (Kim et al. 2008). However, they did not find any significant improvement in income-related equality in outpatient care, unlike our finding. It may be because they evaluated the effect of the policy immediately following its introduction. Individuals with low socio-economic status are likely to acquire information about new policy after a substantial amount of time has lapsed (Lorant et al. 2002; Tudor Hart 1971). Particularly, the information gap may be more pronounced in outpatient care as there is more discretion of patients and more variation in utilization (Korda et al. 2009), whereas providers’ influence is more important in inpatient care. Hence, it may take some time for the policy to influence low-income patients in the utilization of outpatient care.
Our findings that equality in health care utilization was improved are consistent with some studies that estimated the effect of extension of health insurance coverage in other countries (Card et al. 2008; Chen et al. 2007; Enterline et al. 1973; Grootendorst 1997; Liu et al. 2002; Long 2008). Chen and colleagues documented the impact of Taiwan’s NHI, established in 1995, on improving elderly access to care and the extent to which NHI reduces gaps in access to care across different income groups. They found that Taiwan’s NHI has significantly increased the utilization of both outpatient and inpatient care, and such effects were more salient for people in low-income groups (Chen et al. 2007). In China, the pilot experiment of urban health insurance reform led to a significant increase in outpatient care utilization in low socioeconomic groups, making a contribution to achieving horizontal equality in access to basic care (Liu et al. 2002). In United States of America, the onset of Medicare eligibility at age 65 led to an improvement in equality in routine doctor visits (Card et al. 2008).
The improvement in equality might be because low-income individuals are particularly sensitive to cost-sharing. One study which evaluates the effect of increased copayments of prescription drugs presented that people in low-income areas had been impacted differently from those in high-income areas. They suggested that low-income patients would be more sensitive to copayment changes than high-income patients (Chernew et al. 2008). That is, low-income individuals had to pay a larger proportion of their income than high-income individuals, even if they paid the same cost, and therefore copayments were a greater deterrent for the poor than the rich in the utilization of health care (Davis and Reynolds 1975).
At the same time, high-income individuals are more likely to purchase supplementary private insurance and thus face a lower net price (Kassab et al. 1996; Korda et al. 2009; Link et al. 1982). Because of this, low income patients may have more unmet health-care needs than high-income patients. Therefore, benefit coverage expansion of public health insurance can reduce the effect of private insurance and improve equality in health care utilization. In conclusion, we expect that the policy of extending benefit coverage in public insurance or the policy to reduce OOP payments can decrease the impact of individual income as an enabling factor and result in a larger increase in health care utilization among low-income individuals as compared to those more financially better off.
Our study has some limitations and the caveats need to be taken into account regarding the interpretation of these findings. First, we collected data of cancer patients on the basis of the diagnostic code of claims data. The data of patients having at least one inpatient stay or more than two outpatient visits were included and analyzed based on annual per capita health care utilization. As a result, marginal cases with shorter stays are more likely to appear in the data after the policy of reducing OOP payments is introduced, which could make it appear as if the policy does not increase the length of inpatient stay. That is, the bias can attenuate the coefficient of interest in the DID regression. Indeed, our findings showed that the length of stay and inpatient expenses decreased after the introduction of the policy. Second, DID estimators require a parallel trend assumption, which means that the treatment group and the control group would have experienced the same trend over time. In other words, any unobserved factor that affected health care utilization over time should have an equivalent proportional effect on cancer patients, a treatment group, and patients with liver disease, a control group. Furthermore, when we use the TD estimator, any unobserved factor that affected health care utilization over time should have an equivalent proportional effect on the gap of utilization across different income quintiles in cancer patients and that in patients with liver disease. Although we estimated the effect of the policy under those assumptions, a violation of the parallel trend assumption might have led to biased coefficients. Third, the indicators for health care utilization did not include services that were not covered by NHI because data was not available. Some studies reported that equality might be worsened in utilizing certain services with low coverage or uninsured services (Card et al. 2008; Liu et al. 2002; Wagstaff et al. 2009), but we did not evaluate the effect of the policy on uncovered services. Second, we did not adjust to all potential risk factors such as the stages of cancer, which might have an effect on health care utilization. Though we expect that survival/death and disability variables controlled partially for health status of cancer patients, a failure to control all potential risk factors could bias the study results. Especially, the days and expenditure of visits and admissions are higher in the low-income group than in the high-income group, which might be a result from the worse health of the poor. Fifth, we estimated the effect of the policy on income-related equality in health care utilization, not access. We found that the number of high-income patients increased more in cancer patients than in liver disease patients after the policy change, which means that disparity in access might have been worsened though we could not estimate the effect.
Despite these limitations, we expect our paper to make the following contributions. First, unlike most studies, which have examined the impact of expanded benefit coverage on health care utilization, this study evaluates its impact on equity in utilization. Socioeconomic status is an important factor to affect appropriate access to care. Considering that a major goal of universal coverage is to guarantee access to needed services, we need to investigate whether the effect of the policy differs across socioeconomic status. Yet, many studies have not examined the effect of expanded benefit coverage on improving inequity in health care.
Second, we expect our study to provide valuable policy implications for countries that have considered health care reform for improving financial protection. Recently, developing countries as well as United Sates of America and China have attempted to implement health care financing reform for universal coverage. Whereas most European countries have long-standing social health protection mechanisms, Korea is among the countries which have taken steps incrementally toward universal health coverage. It started to expand benefit packages and reduce OOP payment recently, after achieving universal population coverage with stringent benefic coverage and high copayment in 1989. Considering many countries have been struggling to achieve universal coverage under the condition of limited resources, the way that Korea chose may provide policy lessons for them.
Finally, we employed a study design and methodology, such as DID, which allows us to identify the causal effect of the policy, as well as data over 10 years to identify the long-term effect of the policy. We also estimated cluster-robust standard errors to avoid a severe bias to conventional standard error estimates in longer series data. We expect that our findings will provide robust results, compared to previous studies.
In sum, this study presents that the policy of NHI benefit coverage extension leads to an increase in health care utilization for low-income patients and promotes an equitable distribution of utilization. Our findings suggest that a NHI system with comprehensive coverage is an effective way to reduce health care disparities and the policy to extend the NHI benefits is worth supporting to improve income-related equality in health care service utilization. Future research is recommended to investigate the effect of the policy on quality of care and health outcome.
References
Bae, J.-Y. (2010). Impacts of health insurance coverage expansion on health care utilization and health status. Korean Journal of Social Welfare Studies, 41(2), 35–65.
Bertrand, M., Duflo, E., & Mullainathan, S. (2004). How much should we trust differences-in-differences estimates? Quarterly Journal of Economics, 119(1), 249–275. doi:10.1162/003355304772839588.
Card, D., Dobkin, C., & Maestas, N. (2008). The impact of nearly universal insurance coverage on health care utilization: Evidence from medicare. The American Economic Review, 98(5), 2242–2258. doi:10.1257/aer.98.5.2242.
Chen, L., Yip, W., Chang, M. C., Lin, H. S., Lee, S. D., Chiu, Y. L., et al. (2007). The effects of Taiwan’s National Health Insurance on access and health status of the elderly. Health Economics, 16(3), 223–242. doi:10.1002/hec.1160.
Chernew, M., Gibson, T. B., Yu-Isenberg, K., Sokol, M. C., Rosen, A. B., & Fendrick, A. M. (2008). Effects of increased patient cost sharing on socioeconomic disparities in health care. The Journal of General Internal Medicine, 23(8), 1131–1136. doi:10.1007/s11606-008-0614-0.
Davis, K., & Reynolds, R. (1975). Medicare and the utilization of health care services by the elderly. The Journal of Human Resources, 10(3), 361–377. doi:10.2307/145196.
Enterline, P. E., Salter, V., McDonald, A. D., & McDonald, J. C. (1973). The distribution of medical services before and after free medical care: The Quebec experience. New England Journal of Medicine, 289(22), 1174–1178. doi:10.1056/NEJM197311292892206.
Grootendorst, P. V. (1997). Health care policy evaluation using longitudinal insurance claims data: an application of the panel Tobit estimator. Health Economics, 6(4), 365–382.
Kassab, C., Luloff, A. E., Kelsey, T. W., & Smith, S. M. (1996). The influence of insurance status and income on health care use among the nonmetropolitan elderly. Journal of Rural Health, 12(2), 89–99.
Khang, Y. H., & Lee, S. I. (2012). Health inequalities policy in Korea: Current status and future challenges. Journal of Korean Medical Science, 27(Suppl), S33–40. doi:10.3346/jkms.2012.27.S.S33.
Kim, S., Ko, Y., Oh, J., & Kwon, S. (2008). The effect of expanding health insurance benefits for cancer patients on the equity in health care utilization. Korean Journal of Health Policy and Administration, 18(3), 90–109.
Korda, R. J., Clements, M. S., & Kelman, C. W. (2009). Universal health care no guarantee of equity: Comparison of socioeconomic inequalities in the receipt of coronary procedures in patients with acute myocardial infarction and angina. BMC Public Health, 9, 460. doi:10.1186/1471-2458-9-460.
Kwon, S. (2007). The fiscal crisis of National Health Insurance in the Republic of Korea: In search of a new paradigm. Social Policy and Administration, 41(2), 162–178. doi:10.1111/j.1467-9515.2007.00545.x.
Lee, Y.-J. (2009). A study on the influences of changes to the co-payment of cancer patients of their uses of medical services. The Journal of Korean Public Policy, 11(1), 3–25.
Liao, P.-A., Chang, H.-H., & Yang, F.-A. (2012). Does the universal health insurance program affect urban-rural differences in health service utilization among the elderly? Evidence from a longitudinal study in Taiwan. The Journal of Rural Health, 28(1), 84–91. doi:10.1111/j.1748-0361.2011.00363.x.
Link, C. R., Long, S. H., & Settle, R. F. (1982). Equity and the utilization of health care services by the Medicare elderly. The Journal of Human Resources, 17(2), 195–212.
Liu, G. G., Zhao, Z., Cai, R., & Yamada, T. (2002). Equity in health care access to: Assessing the urban health insurance reform in China. Social Science and Medicine, 55(10), 1779–1794.
Long, J. S. (1997). Regression models for categorical and limited dependent variables. New York: SAGE Publications.
Long, S. K. (2008). On the road to universal coverage: impacts of reform in massachusetts at one year. Health Aff (Millwood), 27(4), w270–284. doi:10.1377/hlthaff.27.4.w270.
Lorant, V., Boland, B., Humblet, P., & Deliège, D. (2002). Equity in prevention and health care. Journal of Epidemiology and Community Health, 56(7), 510–516. doi:10.1136/jech.56.7.510.
Lu, J.-F. R., Leung, G. M., Kwon, S., Tin, K. Y. K., Van Doorslaer, E., & O’Donnell, O. (2007). Horizontal equity in health care utilization evidence from three high-income Asian economies. Social Science and Medicine, 64(1), 199–212. doi:10.1016/j.socscimed.2006.08.033.
Mackenbach, J. P., Veerman, J. L., Barendregt, J. J., & Kunst, A. E. (2004). Health inequalities and HIA. In J. S. Kemm & S. Palmer (Eds.), Health Impact Assessment. Oxford: Oxford University Press.
Mott, D. A., Thorpe, J. M., Thorpe, C. T., Kreling, D. H., & Gadkari, A. S. (2010). Effects of Medicare Part D on drug affordability and use: Are seniors with prior high out-of-pocket drug spending affected more? Research in Social and Administrative Pharmacy, 6(2), 90–99. doi:10.1016/j.sapharm.2010.02.004.
O’Donnell, O. A., Bank, W., & Wagstaff, A. (2008a). Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation: World Bank.
O’Donnell, O., van Doorslaer, E., Rannan-Eliya, R. P., Somanathan, A., Adhikari, S. R., Akkazieva, B., et al. (2008b). Who pays for health care in Asia? Journal of Health Economics, 27(2), 460–475. doi:10.1016/j.jhealeco.2007.08.005.
OECD (2012). OECD Health Data.
Polsky, D., Doshi, J. A., Escarce, J., Manning, W., Paddock, S. M., Cen, L., et al. (2009). The health effects of Medicare for the near-elderly uninsured. Health Services Research, 44(3), 926–945. doi:10.1111/j.1475-6773.2009.00964.x.
Ruger, J. P., & Kim, H.-J. (2007). Out-of-pocket healthcare spending by the poor and chronically ill in the Republic of Korea. American Journal of Public Health, 97(5), 804–811. doi:10.2105/ajph.2005.080184.
Song, H. K. (2003). The birth of a welfare state in Korea: The unfinished symphony of democratization and globalization. Journal of East Asian Studies, 3(3), 405–432. doi:10.5555/1598-2408-3.3.405.
Tudor Hart, J. (1971). The inverse care law. The Lancet, 297(7696), 405–412. doi:10.1016/S0140-6736(71)92410-X.
Veugelers, P. J., & Yip, A. M. (2003). Socioeconomic disparities in health care use: Does universal coverage reduce inequalities in health? Journal of Epidemiology and Community Health, 57(6), 424–428. doi:10.1136/jech.57.6.424.
Wagstaff, A., Lindelow, M., Jun, G., Ling, X., & Juncheng, Q. (2009). Extending health insurance to the rural population: An impact evaluation of China’s new cooperative medical scheme. Journal of Health Economics, 28(1), 1–19. doi:10.1016/j.jhealeco.2008.10.007.
Acknowledgments
This study was funded by the National Evidence-based Healthcare Collaborating Agency (NECA), Project No. NM2011-001, and approved by the Institutional Review Board of the same institute. We thank the NECA and also acknowledge support from the National Health Insurance Corporation that provided the data for our study. The anonymous reviewer and the editor of this journal provided insightful comments. We would like to thank Juhwan Oh, Hongsoo Kim and Youn Jung for their comments and supports.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S., Kwon, S. The effect of extension of benefit coverage for cancer patients on health care utilization across different income groups in South Korea. Int J Health Care Finance Econ 14, 161–177 (2014). https://doi.org/10.1007/s10754-014-9144-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-014-9144-y