Abstract
This paper examines the relationship between country health spending and selected health outcomes (infant mortality and child mortality), using data from 133 low and middle-income countries for the years 1995, 2000, 2005, and 2006. Health spending has a significant effect on reducing infant and under-5 child mortality with an elasticity of 0.13 to 0.33 for infant mortality and 0.15 to 0.38 for under-5 child mortality in models estimated using fixed effects methods (depending on models employed). Government health spending also has a significant effect on reducing infant and child mortality and the size of the coefficient depends on the level of good governance achieved by the country, indicating that good governance increases the effectiveness of health spending. This paper contributes to the new evidence pointing to the importance of investing in health care services and the importance of governance in improving health outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developing countries are faced with conflicting evidence on what matters for improving their populations’ health. A large body of empirical studies suggest that investing in health care sectors matters very little for improving population health outcomes when country’s income is controlled for. This indicates that a country’s level of development in general and economic development in particular is what matters for population health (Kim and Moody 1992; McGuire et al. 1993; Musgrove 1996; Filmer and Pritchett 1997; Filmer et al. 1998). However, a limited number of studies find evidence for an effect of country’s health spending on population health outcomes (Anand and Ravallion 1993; Bidani and Ravallion 1997; Bokhari et al. 2007). These studies—with the exception of the study by Bokhari et al.—have been critiqued for having small samples of fewer than 40 countries and in many cases a single year of data. Therefore, even though most studies evaluating individual mother and child health (MCH) program interventions find evidence of their effectiveness, earlier research often found little evidence linking aggregate country level health spending to health outcomes after controlling for country’s income. In order to reconcile these findings, some authors suggested that this contradiction might be a result of countries not spending their health money on the “right” health interventions. While, it is true that there is potential for improving the effectiveness of aggregate country level health spending by improving its allocative efficiency, increasing country level investment in health care sectors at the aggregate level could also matter. This paper re-examines the relationship between health spending and health outcomes using a large panel dataset for 133 developing countries.
The availability of clearer evidence on this issue is particularly important now, as the millennium development goals (MDGs) have created momentum for change that should be guided by evidence. The MDGs are eight international development goals that are based on the United Nations Millennium Declaration, which was adopted by 189 member states at the Millennium Summit in September 2000. The declaration includes commitments to poverty eradication, development, and protecting the environment. Each MDG has a set of targets with indicators to assess progress towards goal achievement.
This paper contributes to the research evidence guiding low and middle countries as they work towards achieving the MDGs and it is specifically relevant to goal 4 (target 4 A), which states that the under-five mortality rate should be reduced by two thirds, between 1990 and 2015.
Recent evidence shows that considerable progress has been made in reducing childhood mortality. The under-five child mortality rate has declined continuously from the MDG baseline in 1990 (Lozano et al. 2011). However, there are large variations across countries and geographical regions. The decline in child mortality has been slower in Sub-Saharan Africa contributing to an increase in this region’s percentage share of under-five deaths from 33 % in 1990 to 49 % in 2011 (Lozano et al. 2011).
Lozano et al. (2011) found that even though there is acceleration in the decline of the child mortality rate in many developing countries, “only nine of 137 developing countries were likely to achieve both the MDG 4 target by 2015”. It is very unlikely that the MDG goal 4 (target 4 A) can be met by 2015 without concerted effort to accelerate the decline in morality (Lozano et al. 2011). Therefore timely research evidence examining the factors contributing to the decline of under-five childhood mortality could provide important input to assist countries in further accelerating the decline.
The purpose of this paper is to examine the relationship between a country’s health spending and selected health outcomes (infant mortality and child mortality). We choose infant mortality and child (under 5 years) mortality because they are the widest and best-measured indicators of health status. In addition, they are factors that are associated with the wellbeing of a population in general. Unhealthy infants and children grow up to become sickly adults, which creates a vicious cycle of low productivity, weak economic progress, and in turn worse population health status. In addition, lower infant and child mortality rates are the major contributing factors to increased life expectancy in developing countries. Using infant and child mortality as the health outcomes of interest in this study also allows us to compare our results with previous research examining the relationship between health spending and health outcomes at the national level.
Research evidence indicates that factors other than health spending affect health outcomes. Most previous studies show that income has a strong impact on health. Income influences health through improved nutrition, housing, and access to water and sanitation—to name but a few channels. Income has a strong influence on health in general and infant and child mortality in particular (Pritchett and Summers 1996; Filmer et al. 1998; Filmer and Pritchett 1999; Rutstein 2000; Shi 2000). Therefore, we include income as a necessary control variable. In addition to income, female education has been identified as an important factor in improving heath outcomes for children (Subbarao and Raney 1995; Filmer and Pritchett 1999). Therefore we also control for female education. The fertility rate is known to be strongly associated with infant and child mortality rates as indicated by previous studies (Zakir and Wunnava 1999) and hence we include total fertility rate as a control variable. We also include female labour force participation and percentage of the population living in urban areas as controls (Zakir and Wunnava 1999).
In comparison with earlier cross country studies, the main contributions of this study lie in the following: (1) using a panel data structure that allows us to control for country and time unobservable effects, in contrast to the cross-sectional single year datasets which were used in most previous studies (2) using a considerably larger sample size of 133 countries compared to smaller sample sizes of many previous studies (For example, 22 countries (Anand and Ravallion 1993); 35 countries (Bidani and Ravallion 1997); 50 countries (Gupta et al. 2002)) (3) the use of National Health Accounts (NHA) data on total health spending including government and private health spending; (4) examining the effect of governance and how it influences the impact of health spending; and (5) employing robust econometric methods to answer questions about the relationship between health spending and health outcomes.
Previous research
The question “does spending on health care services matter in achieving better heath outcomes?” has received much attention in the literature. This question has been asked in both developed and developing country contexts. It has been analyzed at the aggregate country level using cross-country datasets (Pritchett and Summers 1996; Filmer et al. 1998; Filmer and Pritchett 1999; Rutstein 2000; Shi 2000), at the regional level within one country (Dreze and Murthi 1999), and at the household level using DHS and fertility surveys (Hughes and Dunleavy 2000). Finally, this issue has been analyzed using a wide range of measures to capture health outcomes ranging from maternal and child mortality to cancer deaths.
However, the empirical evidence on this topic is mixed. Some early evidence generated using developed country level data showed that spending on health care services was not associated with noticeable improvements in health outcomes leading to the notion that health care services play more of a “caring” rather than “curing” role in developed countries. “Countries that spend more may well buy more caring, but little additional curing” (Newhouse 1977, p. 122)
Anderson and Poullier (1999) found that while from 1990 to 1997 US health spending per capita increased 4.3 % per year, compared with the OECD median of 3.8 %, the US was generally in the bottom half according to available measures and its relative place has been declining since 1960 (Anderson and Poullier 1999; Andreson and Hussey 2001). Fisher et al. (2003) using US Medicare data found that patients’ health status was similar across five regions with different spending levels, but those who lived in high-spending regions utilized more health care services. They also found “no evidence of lower death rates, better functional status, or consistently better satisfaction with care for patients in the high-spending regions” (Fisher et al. 2003).
On the other hand, there are studies showing a positive effect for health spending on health outcomes in developed countries. The study by Cremieux et al. (1999) using province level data showed that health care spending does matter. Cremieux et al. (1999) examined the relationship between health care spending and health outcomes using province level Canadian data and found evidence that lower health care spending was associated with a statistically significant increase in infant mortality and a decrease in life expectancy in Canada controlling for economic, socio-demographic, nutritional and lifestyle factors, time trends and province level factors. More specifically they found that a 10 % reduction in health care spending was associated with infant mortality rates higher by 0.5 % among males and 0.4 % among females and life expectancies lower by 6 months for men and 3 months for women (Cremieux et al. 1999). Martin et al. (2008) used programme budgeting data from 295 English Primary Care Trusts to examine the link between health spending and health outcomes (cancer and circulatory diseases). The study estimated a health expenditure equation and a health outcomes equation using instrumental variables. The authors found a negative effect of health spending on cancer and circulatory disease deaths (Martin et al. 2008).
Empirical literature on the link between health spending and health outcomes using datasets that include developing countries’ data is also inconclusive. However, the general view in the literature based on the majority of previous studies indicates that health spending either plays a minor or insignificant role in improving health outcomes. Musgrove (1996) found no evidence that public spending on health has any impact on child mortality, which was strongly associated with income per capita instead. Zakir and Wunnava (1999), using a cross-sectional dataset of 117 countries (developing and some developed countries) for 1 year (1993), also found that government spending on health played a minor role in determining infant mortality rates.
However there are studies that present different conclusions. Anand and Ravallion (1993) attributed “two-thirds of the elasticity of life expectancy with respect to average income to the positive effect of income on public health spending.” Using a dataset for 22 countries for 1 year. Bidani and Ravallion (1997) used a random coefficients model regressing aggregate life expectancy and infant/perinatal mortality rates across 35 countries against data on the distribution of consumption per person and allowing for differential impacts of public health spending and primary schooling. They found that public health spending matters and concluded that it matters most for poor people living in these countries (Bidani and Ravallion 1997). Both studies have been critiqued because their results are sensitive to the small sample sizes used.
Bokhari et al. (2007) treated the variables government health expenditures and income as endogenous and therefore used instrumental variables (generalized method of moments—GMM-H2SL) to estimate the relationship between government health expenditures and health outcomes. They found that the elasticity of under-five mortality with respect to government expenditures was about 0.33 for developing countries and therefore the authors emphasized that even though economic growth is important for achieving better health outcomes, government spending on health is “just as important” (Bokhari et al. 2007). These studies are considered an exception to the widely held view that country level aggregate health spending matters very little after controlling for country’s income.
The evidence to date is mixed and the results are inconsistent, so there is a need to gain more clarity about the effectiveness of investing in health care. The overwhelming majority of the cross-country studies (especially studies of developing countries) use cross-sectional datasets to explore this question of effectiveness of health spending. However, our understanding of this issue would benefit greatly from using a panel dataset and adequately controlling for country specific effects, which has rarely been done in the literature due to the unavailability of panel data. In addition, this paper examines the interaction effects of health spending and government effectiveness.
Study methods and data
Data
Our database consists of 133 low-income, lower-middle income, and upper-middle income countries. The years covered are 1995, 2000, 2005 and 2006. The choice of this time period is due to the availability of data. Data were obtained from several sources. Health spending and gross domestic product data were obtained from National Health Accounts (NHA) provided by the World Health Organization (WHO); the dataset was constructed from individual country data available from WHO at http://www.who.int/nha/country/en/index.html. Primary data sources for NHA and estimation methods are not discussed here as they are discussed in detail elsewhere (WHO 2008). The quality of the information varies considerably among countries. However, the WHO NHA estimates provide the only data on total, public and private health spending for countries other than OECD members.
Data on infant and child mortality are obtained from United Nations Children’s Fund (UNICEF) at http://www.unicef.org/sowc09/index.php and http://www.childinfo.org. Data on the following control variables: access to improved water and sanitation, physicians per 100,000 people, gender parity in secondary school education and literacy rates were obtained from World Resources Institute at http://earthtrends.wri.org/searchable_db/index.php?theme=4. Data on labour force participation and percentage of population living in urban areas, total fertility rate, and secondary school female enrolment rate were obtained from the World Databank. http://databank.worldbank.org/ddp/home.do. The governance indices are taken from the World Bank at http://www.worldbank.org/wbi/governance/govdata/index.html.
Finally, the countries included in this analysis are the ones that are classified as low income, low-middle income and upper-middle income according to the World Bank Country classification system. The World Bank’s main criterion for classifying economies is gross national income (GNI) per capita.
Methods
Our empirical strategy is as follows: we specify and estimate multivariate regressions that use country level health outcomes (infant mortality and child mortality) as the dependent variables. We use health spending (total and public) and GDP per capita as the main explanatory variables of interest. The inclusion of GDP per capita is a necessary control for the widely acknowledged impact of income on health, which works through a variety of indirect channels (e.g., better education, better nutrition, better housing, better sanitation) and therefore GDP per capita is used in all the models we estimate. We use real GDP per capita at 2000 constant prices in international dollars in the estimation. We use the log of the share of spending on health in GDP to avoid the multicollinearity and bias that could result from including health spending directly in the same model with GDP per capita. Including the log of the share of health spending in GDP gives numerically the same estimate for the health-spending coefficient as using the log of health spending because the log of a ratio equals the difference of logs.
The analysis is divided into two sections:
Section one examines the relationship between total health spending and health outcomes. We employ a fixed effects model, which controls for time-invariant country-specific unobservable determinants of health outcomes. This model allows us to examine the effect of increased health spending and income on health outcomes over the time period 1995–2006 without being concerned about the bias coming from these countries having intrinsic differences that predisposes them to have higher or lower mortality. The fixed effects model is also referred to as a “within” regression, which means that it is estimating the change in health outcomes associated with changes in health spending and income in each country and then using this country level information to arrive at the overall association. We estimate one-way and two-way fixed effects models. We present the models without year dummies (one-way fixed effects) because most previous studies with which we can compare our findings use a single year of data, and hence they examined the effect of levels of health spending and income rather than change/growth of health spending on health outcomes.
However, not including year dummies could be problematic because there are time trends and year specific shocks such as war, epidemics, drought which might be interfering with this relationship. Therefore, we also present two-way fixed effects models with year dummies.
Section two examines the relationship between government health spending and health outcomes. The models in this section include private health spending as a control variable. NHA data availability allowed us to include the variable on private health spending, which was not possible in any of the previous studies, and constituted an omission because of the importance of private health spending.
We also include a “government effectiveness” variable that is developed and measured by the World Bank, which “looks at the ability of the government to implement socially sound policies, i.e. the level and quality of public service provision and the smooth functioning of the bureaucracy.” (Kaufmann and Kraay 2006). Government effectiveness is one of six dimensions of the Worldwide Governance Indicators (WGI) developed by the World Bank. The latest update of the WGI is based on 35 data sources from 33 organizations around the world. The reason for including this variable is to investigate if good governance improves the effectiveness of government health spending. We estimate this model using four waves/years of data.
Results
Descriptive results
Figure 1 below presents a first look at the data where we can observe that there is clearly a negative association between income and infant mortality. However, it also shows that countries at the same level of economic development seem to have considerably different health outcomes, which implies that there are factors other than income that could be driving this variation.
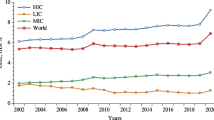
Table 1 presents descriptive statistics on the main variables used in the econometric models. The mean of total health spending in our sample of 133 countries over the time period 1995–2006 is 233 international constant 2,000 dollars. Government health spending has a mean of $148. The Infant mortality rate is 20 deaths per 1,000 live births at the lowest 25th percentile and as high as 76 at the 75th percentile, with an average infant mortality rate of 51 per 1,000 live births. The descriptive statistics show wide variations in infant and child mortality among countries included in the study.
Table 2 shows correlations between some key variables of the study. As expected, GDP per capita, health spending per capita, female education are negatively correlated with infant and child mortality. Fertility on the other hand is positively correlated with the health outcomes. Therefore, we also control for female education. There are two variables in our dataset that capture this factor: female literacy rate and secondary school female enrolment rate. We use the latter in the fixed effects models because the data are more complete. We also include total fertility rate, percentage of population living in urban areas and female labour force participation rate as controls. We do not include health spending directly in the model because it is highly correlated with income and therefore we use health-spending percentage of GDP instead, as in other studies (Filmer and Pritchett 1999).
Multivariate analysis results
Section 1: total health spending and health outcomes
This section examines the effect of increasing total health spending on health outcomes during the 4 years studied, controlling for countries’ per capita income and for country-specific unobservable time-invariant factors using one-way and two-way fixed effects models.
We performed the Hausman test to determine whether a random or fixed effects model is more appropriate. The Hausman’s test results for fixed versus random effects) for the main models in the first section of the analysis are \( {\chi }^{2} (9) = 36.12\) with \(p<0.0000\) and \({\chi }^{2}(9) = 33.32\) with \(p\) value of 0.0001. The results indicate that the fixed effects model is the appropriate model to use in this case. We estimate these models using four waves/years of data (1995, 2000, 2005, and 2006) for the full sample of 133 countries.
Table 3 reports the results of the log–log regressions with infant and under-five child mortality rates as dependent variables. Total health spending is statistically significant and negative in all the models indicating that controlling for income, health spending in developing countries is associated with reductions in infant and child mortality. When dummy variables for years are added, total health spending remains significant but the size of the coefficients of GDP per capita and total health spending are smaller.
Specifications 1 and 4 in Table 3 show that the direction and magnitude of the coefficient estimates are consistent with results reported in previous studies, which employ a single year of data. We estimate elasticities of infant and child mortality with respect to income of \(-0.58\) and \(-0.64\) respectively which means that 1 % increase in GDP per capita is associated with a 0.58 % reduction in infant mortality and a 0.64 % reduction in under five child mortality. According to specifications 3 and 6 in Table 3, the elasticities of infant and child mortality with respect to income—controlling for relevant variables and including year fixed effects—are \(-0.23\) and \(-0.27.\) The reduction in the size of the coefficient as a result of including control variables and year fixed effects is in line with our expectations that previous studies might have overestimated the effect of income, as a result of using cross-sectional datasets.
The key variable of interest—total health spending relative to GDP—is statistically significant in all the models. Our results suggest that elasticities of infant and child mortality with respect to total health spending as a share of GDP are \(-0.32\) and \(-0.37.\)
Specifications 3 and 6 in Table 3 repeat the analyses this time including year dummies and a set of control variables. The coefficients on health spending are statistically significant and negative indicating that increasing health spending reduces infant and child mortality over and above the reduction resulting from increased income. The total health spending elasticities according to the model, which includes year fixed effects are \(-0.13\) and \(-0.15\) for infant and child mortality respectively.
We also conduct the analyses by country-income group to examine the effect of health spending on health outcomes in countries at different levels of the income distribution. The coefficients on health spending are statistically significant and negative for all country-income groups. Using Model 1 with country fixed effects, we found that total health spending elasticity of infant mortality is \(-0.27,\) \(-0.36,\) \(-0.34,\) for low income, lower-middle income, and upper-middle income countries respectively and the total health spending elasticity of under-five child morality is \(-0.31,\) \(-0.48,\) \(-0.38.\) Our results indicate that health spending matters for countries at different levels of development.
Section 2: government health spending and health outcomes
This section examines the effect of increases in government health spending on health outcomes during the 4 years studied, controlling for per capita income, other covariates, and countryspecific unobservable time-invariant factors.
We employ a fixed effects model as in the previous section. For the two models in this analysis, the Hausman’s test results for fixed versus random effects are \({\chi }^{2} =\,52.15\) with \(p\) value of 0.0000 and \({\chi }^{2} =\,41.71\) with \(p<0.0000.\) The test results indicate that the fixed effects model is the appropriate model to use in both cases.
According to specifications 1 and 3 in Table 4, elasticity with respect to per capita income is \(-0.64\) for infant mortality and \(-0.71\) for child mortality and both statistically significant.
Government health spending, the key variable of interest in Sect. 2 models, is interacted with the government effectiveness variable, in order to examine potential synergies between good governance and government health spending. We find that indeed the coefficient on the interaction term is significant in all models, implying that government effectiveness does enhance the impact of health spending, leading to further reductions in infant and child mortality. Since government health spending and government effectiveness are interacted, we can no longer interpret their main-effect coefficients directly because the full effect of each variable depends on the value of the other variable. Our findings indicate that government effectiveness is a moderator for government health spending. Government effectiveness influences health outcomes through the government health spending channel, as well as directly. At the mean value of government effectiveness, the elasticity estimates with respect to government health spending are (\(-.065\) to \(-0.109\)) and (\(-.071\) to \(-0.120\)) for infant and child mortality respectively depending on the model estimated.
Table 5 indicates that government effectiveness enhances the effect of government health spending. The elasticity of infant mortality with respect to government health spending is \(-0.06\) for the countries in the lowest quartile of performance in terms of government effectiveness compared with \(-0.16\) at the 75th percentile. The same is true for child mortality; the elasticity of child mortality with respect to government health spending ranges from \(-0.06\) in poor performing countries to \(-0.18\) in countries performing better on the government effectiveness indicator according to Model 3. Therefore, the return on public investment in health care is clearly much higher in countries that perform better in terms of government effectiveness. On the other hand, the joint significance test indicated that improvements in overall government effectiveness that are not associated with increases in health spending do not lead to reductions in infant and child mortality. Government effectiveness only influences health outcomes through its interaction with government health spending. We also tested if government effectiveness has a similar interactive effect with private health spending and we found the interaction term to be insignificant.
Discussion
Our results indicate that income indeed matters, but that health spending is also an important determinant of health outcomes. Our estimates of elasticities of infant and child mortality with respect to income of \(-0.58\) and \(-0.64\) respectively (according to the fixed effects models, which do not include year dummies) compare to elasticities ranging from \(-0.40\) to \(-0.76\) measured from the cross-country single year cross-sectional data in the literature. Kakwani (1993) estimated elasticities between \(-0.5\) and \(-0.6.\) Jamison et al. (1996) used cross section and time series data and estimated an income elasticity of child mortality of \(-0.40\) in 1996. In models including year dummies, the income elasticities are close to \(-0.23,\) which compares to \(-0.2\) to \(-0.4\) in models estimated by Pritchett and Summers (1996).
Our results suggest that elasticities of infant mortality with respect to total health spending as a share of GDP are between \(-0.13\) and \(-0.32\). Elasticities of Child mortality with respect to total health spending as a share of GDP are between \(-0.15\) and \(-0.37\). This means that doubling the share of health spending of GDP is associated with significant reduction of infant mortality by between 13 % and 32 % and reduction of child mortality by between 15 % and 37 % . Given that most low-income countries are spending less than 5 % of GDP on health, there is a great potential for improving health outcomes through increasing investments in health. Therefore, even though the sizes of the coefficients on health spending are not large in all models, the coefficients are always negative and significant which means that spending on health does matter. for reducing infant and child mortality.
Government health spending also has a significant effect on reducing infant and child mortality and the return on public investment in health care depends on the level of government effectiveness achieved by the country. The results indicate that the elasticities of infant mortality with respect to government health spending are much higher in countries performing better in terms of government effectiveness. The elasticity estimates of infant mortality are 0.06 for countries in the lowest governance performance quartile compared to 0.16 in countries in the highest. The same is true for child mortality; the elasticity of child mortality with respect to government health spending is 0.07 for countries in the lowest performing quartile and 0.18 for countries in the best performing quartile. This represents more than doubling the effect of government health spending.The only other study that we could find that is examining the effect of government effectiveness on health capital is a study by Lazarova and Mosca (2008), in which they find evidence for a threshold effect, below which government effectiveness is not significant as a determinant of health outcomes. For countries above the income threshold, government effectiveness is significant in increasing life expectancy (Lazarova and Mosca 2008). We, on the other hand found that government effectiveness acts as a moderator for government health spending and therefore improvements in government effectiveness enhance the effect of government health spending. Lazarova and Mosca’s models did not include a health-spending variable or an interaction term since they were asking a different research question from the one we are posing in this paper (Lazarova and Mosca 2008).
The coefficients on private health spending are significant in all the fixed effects models, implying that increases in private health spending at the country level are also associated with reductions in infant and child mortality. The size and significance of private health spending coefficients are always lower than those for government health spending. This finding means that spending more on health matters whether the spending is public or private. However, public spending is more effective in improving health outcomes than private health spending. The results do not take into account informal payments for health care, which are not captured in the data and could potentially alter the results.
The finding that the returns on public investment in health care are higher than private investment in terms of achieving lower infant and child mortality are understandable; government health services tend to focus more on preventive care and they are also more likely to target poorer income groups who otherwise would be denied care. However, the coefficient on government health spending is almost the same as on private health spending in countries performing poorly in terms of government effectiveness.
Conclusions
The widely- held notion that health care contributes to “caring” rather than “curing” and that economic growth and better living conditions are what matters for creating improvements in health has not been adequately challenged for developing countries. The policy implications of holding such a view is that it makes little sense for policy makers in developing countries to prioritize investing in health care services since it is not viewed as effective in producing better heath outcomes. Social sector policy in developing countries is constantly challenged, and priorities have an insufficient empirical basis. The scarcity of resources and the competing demands on public sector budgets make it very important that investment allocation across the different social sectors be based on evidence.
In addition, progress towards the MDGs has been slow and uneven across countries. Bokhari et al. (2007) noted that for child mortality “the developing world managed only a 2.5 % average annual reduction in the 1990s, well short of the target of 4.2 % required to reduce the indicator by two-thirds between 1990 and 2015”.
Under-five deaths have declined reaching 7.2 million in 2011 from a baseline of 11.9 million in 1990 (Lozano et al. 2011). However, evidence to date on the progress made towards achieving goal 4 suggests that most countries will not be able to achieve this goal by 2015 in spite of the fact that the rate of decline in childhood mortality has increased in 106 countries since 2000 (Lozano et al. 2011). Therefore, even though progress was made towards reaching this goal, more effort is needed to accelerate the rate of decline in childhood mortality.
Our findings indicate that spending on health significantly reduces infant and child mortality in all the models we specified. We also found synergistic effects of government health spending and government effectiveness. Our results indicate that improvements in government effectiveness enhance the effect of government health spending. Government effectiveness played a moderator role, influencing how effective government health spending was in lowering infant and under-five child mortality. Thus, increasing government expenditures is likely to lead to better improvements of health outcomes if it is accompanied by the right policies and institutions.
This paper finds clear evidence for significant beneficial effects of macro level health spending on health outcomes. However, it does not examine the composition of health spending. It is very likely that the choices countries make with their health funding matter very much for improving health outcomes. Whether countries choose to place more emphasis on investing in primary health care or hospital services will matter in terms of outcomes. For example, we know that “many hospital services at the intensive margin are irrelevant to improving the health outcomes of the majority of the population at risk in the poorest countries because they are too costly to be provided to any but a small minority of the population” (Bokhari et al. 2007). Therefore, there is always potential for improving the allocative efficiency of health spending and in turn increasing the effectiveness of health spending beyond the levels estimated in this paper. Examining the composition of health spending will be a very relevant topic for future research as better data about the composition of health spending becomes available.
References
Anand, S., & Ravallion, M. (1993). Human development in poor countries: On the role of private incomes and public Services. Journal of Economic Perspectives, 7(1), 133–150.
Anderson, G. F., & Poullier, J. (1999). Health spending, access, and outcomes: Trends in industrialized countries. Health Affairs, 18(3), 178–192.
Andreson, G., & Hussey, P. S. (2001). Comparing health system performance in OECD countries: Cross-national comparisons can determine whether additional health care spending results in better outcomes. Health Affairs, 20(3), 219.
Balfour, B. L. (1996). Inequality in income and mortality in the United States: Analysis of mortality and potential pathways, 312(7037), 999–1003.
Barros, P. P. (1998). The black box of health care expenditure growth determinants. Health Economics, 7, 533–544.
Bauer, P. (1972). Dissent on development. Cambridge: Harvard University Press.
Becker, G. S. (1964). Human capital. New York: Columbia University Press (for the National Bureau of Economic Research).
Becker, G. S. (1993). Human capital: A theoretical and empirical analysis with special reference to education. Chicago: National Bureau of Economic Research: The University of Chicago Press.
Beynon, J. (1991). “Assessing Aid” and the Collier/Dollar poverty efficient aid allocations: A critique. London: DFIDDFID.
Bhattacharya, B., Singh, K. K., & Singh, U. (1995). Proximate determinants of fertility in Eastern Uttar Pradesh. Human Biology, 67, 867–86.
Bidani, B., & Ravallion, M. (1997). Decomposing social indicators using distributional data. Journal of Econometrics, 77, 125–139.
Blomqvist, A. G., & Carter, R. A. L. (1997). Is health care really a luxury good? Journal of Health Economics, 16, 207–229.
Bokhari, F. A. S., Gai, Y., & Gottret, P. (2007). Government health expenditures and health outcomes. Health Economics, 16, 257–273.
Boone, P. (1996). Politics and the effectiveness of foreign aid. European Economic Review, 40(2), 289–239.
Burnside, C., & Dollar, D. (1998). Aid, the incentive regime and poverty reduction. Policy Research Working Paper No. 1937. Cambridge: World Bank.
Cochrane, A. L., St. Leger, A. S., & Moore, F. (1978). Health service ‘input’ and mortality ‘output’ in develop countries. Journal of Epidemiology and Community Health, 32, 200–205.
Controversies in Health Care Financing. (2007). Perspectives and debate: Special session at the 6th congress of IIHEA. Copenhagen: Danish Ministry of Foreign Affairs Ministry of Foreign Affairs.
Cremieux, P. Y., Ouellette, P., & Pilon, C. (1999). Health care spending as determinants of health outcomes. Health Economics, 8(7), 627–639.
Deaton, A., & Paxson, C. (1999). Mortality, education, income, and inequality among American cohorts. Working Paper No. 7140. Cambridge, MA: National Bureau of Economic Research.
Deaton, A. (2001). Relative deprivation, inequality, and mortality. Working Paper No, 8099. Cambridge, MA: National Bureau of Economic Research.
Deaton, A. (1999). Inequalities in income and inequalities in health. Working Paper 7141. Cambridge, MA: National Bureau of Economic Research.
Dreze, J., & Murthi, M. (1999). Fertility education and development: Further evidence from India. Population and Development Review, 27(1), 33–63.
Ettner, S. L. (1996). New evidence on the relationship between income and health. Journal of Health Economics, 15, 67–85.
Filmer, D., & Pritchett, L. (1999). The impact of public spending on health: Does money matter? Social Science and Medicine, 49, 1309–1323.
Filmer, D., Hammer, J., & Pritchett, L. (1998). Health policy in poor countries: Weak links in the chain. Policy Research Working Paper No. (1874). Washington, DC: World Bank.
Filmer, D., & Pritchett, L. (1997). Child mortality and public spending on health: How much does money matter? Policy Research Working Paper No. (1864). Washington, DC: World Bank.
Fisher, E. S., Wennberg, D. E., Stukel, T. A., Gottlieb, D. J., Lucas, F. L., & Pinder, E. L. (2003). The implications of regional variations in medicare spending part 2: Health outcomes and satisfaction with care. Annals of Internal Medicine, 13, 288–298.
Foster, M., & Leavy, J. (2001). The choice of financial aid instruments. ODI Working Paper No. 158, October 2001. London: Overseas Development Institute.
Freeman, D. G. (2003). Is health care a necessity or a luxury? Pooled estimates of income elasticity from US state-level data. Applied Economics, 35, 495–502.
Gangadharan, L., & Valenzuela, M. R. (2001). Interrelationships between income, health and the environment: Extending the environmental Kuznets curve hypothesis. Ecological Economics, 36(3), 365–547.
Grossman, M. (1972). Concept of health capital and demand for health. Journal of Political Economy, 80(2), 223–255.
Gupta, S., Verhoeven, M., & Tiongson, E. R. (2002). The effectiveness of government spending on education and health care in developing and transition economies. European Journal of Political Economy, 18(2002), 717–737.
High-Level Forum on the Health MDGs. (2005). Fiscal space and sustainability from the perspective of the health sector. Paris: High-Level Forum on the Health MDGs.
Hirschman, A. O. (1967). Development projects observed. Washington, DC: Brookings Institution.
Hughes, G., & Dunleavy, M. (2000). Why do babies and young children die in India? Income, and maternal mental and physical health: Cross sectional national survey. India in the new millennium. Bulletin of the World Health Organization, 78(1), 216–218.
Jalan, J., & Ravallion, M. (2003). Does piped water reduce diarrhea for children in rural India? Journal of Econometrics, 112, 153–173.
Jamison, D. T., Wang, J., Hill, K., & Londono, J. L. (1996). Income, mortality and fertility control in Latin America: Country-level performance 1960–90. Mimeo, Washington, DC: LAC Technical Department, The World Bank.
Kakwani, N. (1993). Performance in living standards: An international assessment. Journal of Development Economics, 41, 307–336.
Kaufmann, D., Kraay, A. (2006). Governance indicators: Where are we, where should we be going? World Bank Policy Research Working Paper WPS4730. Washington, DC: World Bank.
Kim, K., & Moody, P. M. (1992). More resources better health? A cross-national perspective. Social Sciences and Medicine, 34, 837–842.
Lazarova, E. A., & Mosca, I. (2008). Does governance matter for aggregate health capital? Applied Economic Letters, 15, 199–202.
Lichtenbery, F. R. (2005). The impact of new drug launches on longevity: Evidence from longitudinal, disease-level data from 52 Countries, 1982–2001. International Journal of Health Care Finance and Economics, 5, 47–73.
Lozano, R., Wang, H., Foreman, K. J., Rajaratnam, J. K., Naghavi, M., Marcus, J. R., et al. (2011). Progress towards millennium development goals 4 and 5 on maternal and child mortality: An updated systematic analysis. Lancet, 378, 1139–65.
Martin, S., Rice, N., & Smith, P. (2008). Does health care spending improve health outcomes? Evidence from English programme budgeting data. Journal of Health Economics, 27, 826–842.
Masud, N., & Yontcheva, B. (2005). Does foreign aid reduce poverty? Empirical evidence from nongovernmental and bilateral aid. IMF Working Paper 05/100. Washington, DC: International Monetary Fund.
Maxwell, R. (1981). Health and wealth: An international study of health care spending. MA: Lexington Books.
McGuire, A., Parkin, D., Hughes, D., & Gerard, K. (1993). Econometric analyses of national health expenditures: Can positive economics help answer normative questions? Health Economics, 2, 113–126.
Mishra, P., & Newhouse, D. (2009). Does health aid matter? Journal of Health Economics, 28, 855–872.
Musgrove, P. (1996). Public and private roles in health: Theory and finance patterns. Discussion Paper No. 339. Washington, DC: World Bank.
Musgrove, P., Zeramdini, R., & Carrin, G. (2002). Basic patterns in national health expenditure. Bulletin of the World Health Organization, 80(2), 134–142.
Newhouse, J. P. (1977). Medical care expenditure: A cross-national survey. Journal of Human Resources, 12, 115–125.
Noumba, I. (2004). Are wealthier nations healthier nations? A panel data approach to the determination of human development in Africa. African Development and Poverty Reduction: The Macro-Micro Linkage. Forum Paper 2004, South Africa.
Pritchett, L., & Summers, L. H. (1996). Wealthier is healthier. Journal of Human Resources, 31, 841–868.
Reinhardt, U. E., Hussey, P. S., & Anderson, G. F. (2002). Cross national comparisons of health care systems using OECD, 1999 data. Health affairs, 21, 169–182.
Rutstein, S. (2000). Factors associated with trends in infant and child mortality in developing countries during the 1990s. Bulletin of the World Health Organization.
Shi, A. (2000). How access to urban potable water and sewerage connections affect child mortality. Washington, DC: World Bank.
Subbarao, K. Y., & Raney, L. (1995). Social gains from female education: A cross-national study. Economic Development and Cultural Change, 44, 105–128.
Tresserras, R. J. C., Alvarez, J., Sentis, J., & Salleras, L. (1992). Infant mortality, per capita income, and adult illiteracy: An ecological approach. American Journal of Public Health, 82, 435–437.
Wagstaff, A., & Claeson, M. (2004). The millennium development goals for health: Rising to the challenges. Washington, DC: World Bank.
Wang, L. (2003). Health outcomes in low-income countries and policy implications: Empirical findings from demographic and health surveys. Health Policy, 65, 277–299.
WHO. (2008). Guide to producing national health accounts 2003. Retrieved 3 October, 2008 from http://www.who.int/nha/docs/English_PG.pdf.
World Development Report. (2004). Making services work for poor people: A copublication of the world bank and Oxford University Press, 2003. Washington, DC: The International Bank for Reconstruction and Development/The World Bank.
Zakir, H., & Wunnava, P. (1999). Factors affecting infant mortality rates: Evidence from cross-sectional data. Applied Economics Letters, 6, 271–273.
Author information
Authors and Affiliations
Corresponding author
Annex 1: List of countries used in the analysis
Annex 1: List of countries used in the analysis
List of countries used in the analysis |
|---|
133 Countries |
(Low-income, lower-middle income and upper-middle income countries) |
Afghanistan, Bangladesh, Benin, Burkina Faso, Burundi, Cambodia, Central African Rep, |
Chad, Comoros, Congo, Dem Rep, Cote d’Ivoire, Eritrea, Ethiopia, Gambia, Ghana, Guinea, |
Guinea-Bissau, Haiti, Kenya, Kyrgyzstan, Lao People’s Dem Rep, Madagascar, Malawi, Mali, |
Mauritania, Mozambique, Myanmar, Nepal, Niger, Nigeria, Pakistan, Papua New Guinea, |
Rwanda, Sao Tome & Principe, Senegal, Sierra Leone, Solomon Islands, Tajikistan, Tanzania, |
Togo, Uganda, Uzbekistan, Viet Nam, Yemen, Zambia, Albania, Algeria, Angola, Armenia, |
Azerbaijan, Bhutan, Bolivia, Bosnia and Herzegovina, Cameroon, Cape Verde, China, |
Colombia, Congo, Djibouti, Dominican Rep, Ecuador, Egypt, El Salvador, Georgia, |
Guatemala, Guyana, Honduras, India, Indonesia, Iran, Islamic Rep, Jordan, Kiribati, Lesotho, |
Macedonia-FYR, Maldives, Marshall Islands, Micronesia-Fed States, Moldova Rep, Mongolia, |
Morocco, Namibia, Nicaragua, Paraguay, Peru, Philippines, Samoa, Sri Lanka, Sudan, |
Swaziland, Syrian Arab Rep, Thailand, Timor-Leste, Tonga, Tunisia, Turkmenistan, Ukraine, |
Vanuatu, Argentina, Belarus, Belize, Botswana, Brazil, Bulgaria, Chile, Costa Rica, Croatia, |
Cuba, Dominica, Fiji, Gabon, Grenada, Jamaica, Kazakhstan, Latvia, Lebanon, Libyan Arab |
Jamahiriya, Lithuania, Malaysia, Mauritius, Mexico, Montenegro, Palau, Panama, Poland, |
Romania, Russian Federation, Serbia, Seychelles, South Africa, St. Lucia, |
St. Vincent & Grenadines, Suriname, Turkey, Uruguay, Venezuela |
Rights and permissions
About this article
Cite this article
Farag, M., Nandakumar, A.K., Wallack, S. et al. Health expenditures, health outcomes and the role of good governance. Int J Health Care Finance Econ 13, 33–52 (2013). https://doi.org/10.1007/s10754-012-9120-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-012-9120-3