Abstract
Healthcare utilization studies show how well documented disparities between migrants and non-migrants. Reducing such disparities is a major goal in European countries. However, healthcare utilization among Italian immigrants is under-studied. The objective of this study is to explore differences in healthcare use between immigrant and native Italians. Cross-sectional study using the latest available (2004/2005) Italian Health Conditions Survey. We estimated separate hurdle binomial negative regression models for GP, specialist, and telephone consultations and a logit model for emergency room (ER) use. We used logistic regression and zero-truncated negative binomial regression to model the zero (contact decision) and count processes (frequency decisions) respectively. Adjusting for risk factors, immigrants are significantly less likely to use healthcare services with 2.4 and 2.7 % lower utilization probability for specialist and telephone consultations, respectively. First- and second-generation immigrants’ probability for specialist and telephone contact is significantly lower than natives’. Immigrants, ceteris paribus, have a much higher probability of using ERs than natives (0.7 %). First-generation immigrants show a higher probability of visiting ERs (1 %). GP visits show no significant difference. In conclusion Italian immigrants are much less likely to use specialist healthcare and medical telephone consultations than natives but more likely to use ERs. Hence, we report an over-use of ERs and under-utilization of preventive care among immigrants. We recommend improved health policies for immigrants: promotion of better information dissemination among them, simplification of organizational procedures, better communications between providers and immigrants, and an increased supply of health services for the most disadvantaged populations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Immigration to Italy is a relatively recent phenomenon that started in the 1970s and took off during the 1990s. This process has been fueled by the collapse of the Soviet Union, the expansion of the European Union, and political instability in Northern Africa. Immigrants come to Italy as asylum seekers, legal immigrants, refugees, and irregular arrivals. The number of residence permits rose by five-fold, from 436,000 in 1990 (less than 1 % of the total population) to over 2.2 million in 2003, 4 % of population (Del Boca and Venturini 2003). During the recent economic and financial crisis, immigration flows to Italy have decreased slightly, while illegal immigration has increased (Ambrosseti 2009). Despite efforts to register legal immigrants, only 68 % of them have signed up with the National Health Service, according to the Ministry of the Interior’s first report on the activity of the territorial boards on immigration (Ministero dell Interno 2007).
It is well established that migration and health have a very complex relationship. The health status of immigrants is influenced by all aspects of the migration journey, including the country of origin, the transit process, the destination country, and even return journeys back to the country of origin. The increasing heterogeneity of health care use as a result of both the immigration process and the changing face of the immigration population represents a challenge to health care professionals as well as to the national health care system. The changes that have created at least part of the challenge include new migration patterns and the emergence and re-emergence of various infectious diseases. Together with advances in technology, these factors have affected the assessment, development, and implementation of the policies that have an impact on both the form and delivery of health care services (Key Message section, par. 1, 2010). Spurred on by recommendations from the International Organization for Migration (IOM) about the need for monitoring of migration health policies and the concomitant need for a swift overhaul of immigrant healthcare policies, Italy, like the rest of the EU member states, has made a concerted political commitment to meet these challenges and to promote better access to health services for the affected population (see, for instance, ECDC 2009).Footnote 1
The Italian National Health Care System (henceforth, SSN),Footnote 2 mainly funded through taxes, provides comprehensive insurance and uniform health care for the entire population regardless of ability to pay and citizenship. The SSN is also a highly decentralized system that relies on the 20 administrative regions of Italy to supply public health services. It is estimated that approximately 70 % of health expenditures are publicly funded through general taxation; the remainder are financed through out-of-pocket payments (France et al. 2005). Regular immigrants are granted equal treatment and have the same rights and duties as other Italian citizens provided that they are registered with the SSN (Legislative Decree 286/1998). Irregular immigrants may access services at special SSN centers if they are identified and certified as a Temporarily Present Foreigner, or Straniero Temporaneamente Presente (STP), and this applies to all immigrants no matter what their country of origin. Before receiving an STP, irregular immigrants must fill out an official form of declaration of insufficient economic resources called Dichiarazione di Indigenza. However, even when entitlements are clearly specified by the law, access to health care may be prevented by immigrants’ lack of knowledge of the national laws, for instance, the need for a medical card for foreigners to gain access to a general practitioner. Finally, asylum seekers in Italy—as elsewhere in Europe—are entitled to receive basic treatment for acute diseases free of charge. Nevertheless, the lack of knowledge and information about national regulations can act as an important obstacle to a person’s benefitting from health care in a host country. Other factors that may limit immigrants’ access to health care (hence the differential use of health care services) include poorer economic and social conditions experienced by immigrants. For instance, it is well documented that immigrants experience worse labor market conditions (Borjas 2000).
Differences in the use of health services between immigrants and natives may also be based on people’s individual characteristics and physical conditions/and or psychological conditions. Immigrants might be more vulnerable to a number of health problems, present disease profiles that differ from those of the general population and might also have different perceptions of illness and health (Jensen et al. 2010). One of the main arguments for the disparity is related to differences in initial health, which would thus affect needs, as well as health care-seeking behavior. There might be a positive selection effect (Jasso et al. 2004). Since immigration has both monetary (moving and transportation expenses) and non-monetary (emotional) costs, the healthier, more educated are more likely to change their residence.Footnote 3 From this point of view, it would be reasonable to expect lower utilization rates for health care services from immigrants. In particular, this effect has been noted in several studies (e.g., Crimmins et al. 2007; Burón et al. 2008). However, there might be a decline of this healthy-immigrant effect over a longer length of residence. Thus, the final outcome is an increased use of health services due to both the relative worsening of the immigrants’ healthFootnote 4 and improved knowledge of how to access health services over time (e.g., Stronks et al. 2001; Hjern et al. 2001). According to Fernandes and Miguel (2009), Italy has experienced a decrease in the health standards of migrants over the last decade. In particular, they pointed out that “the ‘healthy interval’ between arrival in Italy and the first request for medical help has decreased from 10–12 months in 1993–1994 to 3–4 months in the last few years”.
In addition, language difficulties when making appointments with primary care physicians by phone may result in the use of emergency services as a substitute (Flores et al. 1998; Kristiansen et al. 2007). Language difficulties can also lead to a misunderstanding of the information related to preventive care; to treatment; and, more broadly, to access to the health care system (Chaouchi et al. 2006). Immigrants may also use emergency services as a substitute for other health services because of a lack of knowledge about the health care system and the fact that hospital facilities are easier to access (Norredam et al. 2004).
Lastly, cultural factors and traumatic experiences in the host country may limit health care use by immigrants (see, for instance, Bach et al. 2004). The empirical literature is not unanimous about the pattern of use of health care services by immigrants and the native population. Some authors report that immigrants tend to have more visits to physicians (Stronks et al. 2001; García-Gomez 2007; Solé-Auró et al. 2009; Hernández Quevedo and Jiménez Rubio 2009; Nauenberg et al. 2011), while others do not find any significant effect (Muñoz de Bustillo and Antón 2010). Nevertheless, there is a consensus that immigrants tend to use more emergency room (henceforth, ER) services than the native-born population for several European countries (Hjern et al. 2001; Cots et al. 2007; Burón et al. 2008; Rue et al. 2008; Muñoz de Bustillo and Antón 2010).
There is a great deal of the literature tackling this issue for countries such as the U.S. (Tarraf et al. 2012), the Netherlands (Uiters et al. 2006), England (Bach et al. 2004), Ireland (Nolan 2011), Spain (Burón et al. 2008; Rue et al. 2008; Hernández Quevedo and Jiménez Rubio 2009; Muñoz de Bustillo and Antón 2010; Calderón-Larrañaga et al. 2011), and Portugal (Dias et al. 2008; Barros and Pereira 2010). Nevertheless, for the Italian case, few studies have explored the existence of inequalities in health and inequity in access to health care services for the Italian population (Costa et al. 2000; Cacciani et al. 2006; Tognetti Bordogna 2008; Baglio et al. 2010; Masseria and Giannoni 2010; Petrelli et al. 2010). Furthermore, we are not aware of any empirical study investigating this issue at the national level (see, Norredam et al. 2009 for an excellent review on this topic). Most papers focus on socio-economic inequity among Italian regions in healthcare access and utilization (Costa et al. 2000; Petrelli et al. 2010 among others). Therefore, in order to facilitate a better understanding of immigrant health, we examine differences in health care utilization between the immigrants and the native-born population in Italy. This study can help elucidate both the inequality in the use of services by these two different populations in general as well as the horizontal inequity that exists between the consumption of equally available services by individual members of each group who have equivalent needs.
Our paper also distinguishes between the foreign born immigrants (first generation) and Second generation of immigrants. There are several reasons to analyze separately both groups of immigrants. Firstly, differences in health care use might be due to the assimilation or acculturation process (Rumbaut 2004). Several empirical studies have confirmed this hypothesis which proposes that the adoption of the host country’s cultural patterns might lead to a convergence in health status between native population and second generation immigrants (for instance, Kao 2009; Steinhausen et al. 2009; Rumbaut 2004; Leclere et al. 1994). There might be also differences in language skills between the two different generations of immigrants. The Second generation might have fewer difficulties in speaking Italian compared to the first generation. In addition, the Second generation might be more influenced by the Italian culture, and thus by the cultural perceptions of health and health seeking behavior in the country. It is therefore interesting to investigate a potential difference in behavior between first and second generation immigrants in our empirical framework to get an indication of differences in health care use.
We explore differences in utilization of health services between the immigrant and the native-born populations by using recently released, nationally representative data from the 2005 Italian Health Conditions Survey (ISTAT-Condizioni di salute e Ricorso ai Servizi Sanitari), carried out by the Italian National Statistical Office (ISTAT). This survey includes a sufficient number of observations of immigrants thus overcoming limitations of past studies that have used small samples or had a lack of national representativeness. Lastly, the question of whether health systems will be financially sustainable is frequently raised in health policy debate. In Italy, immigration is not a big issue, both because of its size, as it accounts for about 3 % of resources, and its gravity, as most of immigrants are young and have modest needs (see Agenzia Nazionale per i Servizi Sanitari Regionali 2008). The fact that immigrants overuse ERs may contribute to crowding. The shift to primary care settings has much more of an implication from an equity point of view, since the cost savings from this shift do not imply a substantial cost reduction except, perhaps, for some regions in the North which have a larger immigrant population.
The paper is organized as follows: second section describes the data and the model used in the empirical analysis, third section presents the main results, fourth section discusses the main findings and final section offers conclusions.
Data and model specification
Sample
In this study we used data from the latest available wave (2004/2005) of the Italian Health Conditions carried out by the ISTAT (2005). This survey is conducted every five years on a nationally representative sample of 50,474 households for a total of 128,040 individuals including 3,509 foreigners resident in Italy. Given the age restriction of the sample of foreign-born individuals (aged 0–64), the total cross-sectional sample size of people aged below 65 reduced to 102,857 individuals. The survey provides information on citizenship at birth and birthplace and on a wide range of both demographic and socio-economic characteristics of individuals and households as well as on perceived health status, lifestyle, living and working conditions, and health care utilization. Despite the lack of a longitudinal dimension in the survey, one of the advantages of this dataset relates to its level of detail, since it contains information for different types of healthcare use variables. For example, it provides information not only on visits to GPs and specialists but also on ER visits and telephone consultations which occurred in the latest four weeks immediately prior to the interview.
Variables
As dependent variables we used four different typologies of access to health care: GP visits, specialist medical visits, phone consultations, and ER care. The reference period was the last four weeks immediately prior to the interview. The number of visits was self-reported.
The main independent variable of interest is immigrant status defined according to both the place of birth and the citizenship criteria. In this way we identified four categories: (1) the native reference group consisting of Italian citizens born in Italy, (2) first-generation immigrants defined as individuals born outside of Italy who did not have Italian citizenship, (3) second-generation immigrants identified as individuals born in Italy who did not hold Italian citizenship, and (4) naturalized Italians who were individuals born outside of Italy who have Italian citizenship. Moreover, since the ISTAT dataset contains information on the country of birth for first-generation immigrants, we disaggregated this category according to the birthplace into Albanian, Moroccan, Romanian, born in EU 25, born in the extra-EU 25, other Africans, and Americans to explore different health care utilization patters among these groups.Footnote 5 Following the health care utilization framework proposed by Andersen and Newman (1973), the analysis is adjusted for: (1) variables on predisposing factors to health care use (i.e., socio-demographic characteristics), (2) variables on enabling factors for health care use (i.e., family resources), (3) variables on need, (4) variables on health behavior, and (5) variables on health services system. These variables are described briefly and discussed below.
Predisposing factors
First, we included gender, age, marital status, number of children in the household, and education as socio-demographic variables. Gender was identified with a dummy variable taking the value 1, if the respondent was female. We categorized age measured in years into seven groups, i.e., 0–9 (the reference category), 10–19, 20–29, 30–39, 40–49, 50–59, and 60–64. We also included a dummy variable taking value 1 if the respondent was married and 0 otherwise (i.e., never married, widowed, separated, or divorced). To take into account the presence of children in the household, we included a categorical variable with the following categories: no children (reference category), two or three children and more than three children. We also adjusted the analysis for educational level, classified into seven categories and grouped into three: no and primary education, lower secondary education, upper secondary education and higher education (the reference category).
We used the available information about employment status to compare the effect of being unemployed, i.e., a housewife, a student, retired, and other (including individuals who were unable to work, in the military, or civil servants) on healthcare utilization with respect to the reference category of employed.
Enabling factors
The dataset does not provide information on income, but it does offer information (self-evaluations) on a four-point scale of family wealth: very high, high, low, very low. Using this information, we built a dummy variable to allow for the effect of self-assessed household wealth on healthcare utilization, taking the value of 1 if wealth was low or very low and zero otherwise (reference category). Given the lack of information on family income in the survey, we used wealth as a proxy of income, but we advise that this coefficient should be treated with caution, since a subjective evaluation of economic circumstances and endogeneity problems may lead to biased estimates.Footnote 6
Need factors
We used three indicators of health status: self-assessed health status (henceforth, SAH), chronic diseases, and disability conditions. SAH is measured by the standard question, “How is your health in general?” with five standard answers: very good, good, fair, bad, very bad which we have grouped into three categories of health status: bad, fair, and good health (reference category). Regarding individual health, we have information on the following chronic conditions: asthma, allergy, diabetes, cataracts, hypertension, stroke, angina, heart disease, bronchitis, arthritis, osteoporosis, mental disorders, cancer, gastric or duodenal ulcer, and others. These chronic conditions were reported by the individuals but diagnosed by a physician,Footnote 7 something which would ensure that we referred to objective health conditions. We generated a dummy variable taking the value of 1 if an individual suffered from at least one chronic disease and zero otherwise (the reference category). Finally, we used information on disability conditions classified into five categories: whether the individual reported suffering from sensory difficulties, disability, difficulties in moving, difficulty in functioning, or being bedridden and coded as a dummy variable taking the value of 1 if an individual suffered from at least one type of disability and zero otherwise (the reference category).
Health behavior
Three types of variables were selected to take into account how health behavior affected healthcare utilization: being a smoker; engaging in strong- moderate- or light physical activity at least once per week; and checking weight at least once per week.
Health services system
Finally, dummies on geographical areas (reference category: South)Footnote 8 and city size (reference category: very small cities) were included in all specifications to control for unobserved environmental characteristics as well as geographic and supply factors that influence health care use across areas of residence.
Empirical analysis
The dependent variables used in the empirical analysis are non-negative counts of health care utilization. It is well known that the OLS method is not appropriate when data are non-negative integers, since it can predict negative values of the dependent variable (Cameron and Trivedi 1998). As an alternative approach to classical linear regression models, count data models have become increasingly popular in many fields of empirical economics. Applications include, for example, studies in transportation, health economics, and industrial organization among others. In this section we compare and discuss alternative count data models aiming at identifying the more appropriate estimator to use in the empirical analysis.
The point of departure in the econometrics of count data is the Poisson regression model, where the number of occurrences of an event has a Poisson distribution. This model explicitly assumes the independence of observations and the equality of the conditional mean and conditional variance. These assumptions are widely recognized as very strong and in many cases (as in our data) may be violated. In fact, from a simple inspection of Table 2, it emerges that the sample mean for each dependent variable is lower than the sample variance. This feature is known as overdispersion in count data models which could be generated from unobservable individual heterogeneity and/or a large proportion of zeros and a skewed distribution of positive outcomes for health care utilization data. Therefore, since in our data there is clear evidence of overdispersion, using the classical Poisson model may lead to biased estimates.
In order to deal with overdispersion, the negative binomial regression model (henceforth NBRM) is often proposed. The NBRM is a generalization of the Poisson model that partly accounts for unobserved individual heterogeneity by including a dispersion parameter in the conditional mean of the Poisson model as an error term. However, if overdispersion is generated from a large number of zeros in the data, the negative binomial regression model will produce biased estimates. This problem is likely to be present in our dataset, since most individuals had not used any health care services in the last four weeks prior the interview. Therefore, the high proportion of zero values motivates the use of zero-inflated models, which are proposed in the literature as a solution to this type of problem. Zero-inflated models explicitly account for excess zeros relative to the Poisson model and also allow for the variance to differ from the mean. Like the hurdle model, they supplement a count density with a binary process for which the observed outcome is always zero if the binary process takes on a value of zero, while it is positive if the binary process takes on a value of 1. This model is known as a Zero-Inflated Negative Binomial model (henceforth ZINB). As in the case of the hurdle model, the observed zero for the dependent variable may be a constant or may be parameterized through a binomial model like the logit or probit while all positive counts for the dependent variable may be generated from the NB process. However, in contrast to zero-inflated models, hurdle models can be interpreted as two-part models. The first part is typically a binary response model, and the second part is usually a truncated-at-zero count model (Cameron and Trivedi 1998).
In our context the two different processes correspond to a situation where the patient initiates the first contact and the decisions of the physicians determine subsequent visits, that is, the intensity of the treatment. Here, our purpose was to compare standard Poisson model with zero-inflated and hurdle models. Hence, in the next section we use several criteria to compare and select the most appropriate model to use in the empirical analysis. Lastly, it is worthwhile pointing out that the use of cross-sectional data does not represent a serious shortcoming in our analysis, as the use of fixed effects, which allows us to control for unobserved heterogeneity, would prevent us to estimate the effect of time invariant variables such as immigrant status on health care use.
Model selection
In this section, we use the likelihood ratio (LR) test, and akaike, and Bayes information criteria (AIC and BIC) to test the assumptions imposed by the different estimation approaches. Examples of the use of these criteria to assess the appropriateness of different health care use models can be found among others in Gerdtham and Trivedi (2001) and Cotter (2008). In the next section, we show only the results of the models that best fit the data. Detailed results from the other econometric models and specifications are available upon request.
Most of these models are non-nested, so LR tests are not possible. The LR test can be used to test the NB against the Poisson model. Therefore, as a first step, in Table 5 (column 1) we compared these two models. The LR test statistics supported the view that the NB model is preferable to the Poisson model.
As a next step, we tested if overdispersion was also due to excess zeros. For this purpose, we used the non-nested LR test of Vuong (1989) to discriminate between the ZINB and the NB models (column 2 of Table 5). The test statistic has a normal distribution, with large positive values favoring the ZINB model and large negative values favoring the NB model. In our case the Voung test of ZINB against the NB model clearly favored the zero-inflated specification. This shows evidence of a split between users and non-users of medical visits. The estimated alpha is highly significant, which shows evidence against the nested ZIP.Footnote 9
As a further step, the ZINB and the ZIP models were compared using an LR test (column 3 of Table 5). The LR test provides evidence for preferring the ZINB over the ZIP model. As a final step, we examined the fit of all models presented before and also of the hurdle negative binomial (HNB) model—which has been adopted, among others, by Pohlmeier and Ulrich (1995)—using AIC and BIC for each model with observed counts (Table 6). The AIC and BIC criteria favor the HNB model over all other considered models as regards GP and Specialist visits; however, there is little difference in the ZINB- and HNB-computed AIC values for telephone consultations (97962.3 and 97987.7, respectively).Footnote 10 Therefore, in light of these specification tests, the HNB was our chosen model. We used logistic regression and zero truncated negative binomial regression to model the zero (contact decision) and count processes (frequency decisions), respectively. We estimated separate HNB regression models for GPs and specialist visits, telephone consultations and a logit model for ER use. We adjusted the analysis by controlling for potential confounding factors that were likely to affect healthcare utilization, including demographic and socio-economic factors, self-reported health status, living and working conditions, and health behavior risk factors. Geographical macro dummies were also used to control for unobserved environmental and geographical factors that influenced health care use across areas. However, even if we included in the analysis a wide range of control variables, potential bias may still arise if unobservable factors are correlated with the decision of immigrants to utilize healthcare services. For instance, if immigrant individuals were different from native people in some unobservable characteristics, such as being unhealthier than native people, then the estimated effects can partly capture these unmeasured differences in healthcare utilization.
Results
Descriptive statistics
Table 1 reports the distribution of the weighted sampled population by place of birth and by citizenship. Around 94.5 % of the sample consisted of natives; 2.13 % were naturalized citizens; 2.89 % were first-generation immigrants, while second-generation immigrants represented only 0.45 % of the sample.
Weighted summary statistics for the main variables used in the empirical analysis are reported in Table 2 (whole sample) and in Tables 3 and 4 for the two main subgroups of individuals: immigrant and native-born. Immigrants are 5,628 (Table 3) and those of the first generation were mostly born in Asia (11.3 %), followed by those from Non-EU Countries (9.2 %), other Africans (8 %), Albania (7.7 %), Morocco (7.5 %), Romania (7 %), America (6.9 %), and EU 25 (4.4 %). The sample was gender balanced. About 47 % were married. All in all, the immigrants were generally younger and less educated and had lower levels of self-assessed wealth than Italian natives. A comparison of some salient health outcomes between the immigrant and the native populations—self-reported health status and chronic diseases—indicates that immigrants appeared to be in slightly better health than the native-born. Immigrants also reported a lower prevalence of chronic conditions than the native-born.
The mean of the GP medical visits is equal to 0.18 (with a range from 0 to 20) for the Italian sample compared to 0.14 (with a range from 0 to 25) for the immigrants. Similarly, the propensity to visit a specialist was larger among natives (mean: 0.28 with a range from 0 to 24) than immigrants (mean: 0.19 with a range from 0 to 14). Natives had higher number of telephone consultations (mean: 0.22 with a range from 0 to 30) compared to immigrants (mean: 0.13 with a range from 0 to 10). In contrast, a higher use of ER services was found among immigrants (5.4 %) compared to native Italians (4.2 %) (Tables 3–6).
Regression results for econometric models of health care use
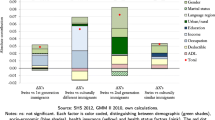
In this section, we evaluate differences in health care use between immigrants and natives controlling for a wide range of demographic and socio-economic characteristics, living and working conditions, several measures of health need, health behavior, and geographical dummy variables. Table 7 contains the results of the HNB model for visits to a GP, Table 8 the results for visits to a specialist and Table 9 the results for consultation practices provided by phone. The first stage equation represents the contact decision, while the second stage equation models the frequency decision. In order to make interpretations much easier, we computed the marginal effects evaluated at covariate means for both the logit and ZTNB models For each model we report three specifications: in the first one we compare immigrants with natives (columns 1 and 2 of each table); in the second one we disaggregate the immigrant status into naturalized, first- and second-generation immigrants (columns 3 and 4); in the third one, we disaggregate further immigrants of first generation according to the country of origin (columns 5 and 6).
First stage: probability of health care utilization
From the results it emerges that, ceteris paribus, being an immigrant had a negative influence on the probability of a doctor contact compared to being native. Though the influence is not found to be significant, this result is in line with previous research. Nevertheless, the estimated coefficient for the immigrant variable is negative and statistically significant for specialist visits (\(-\)2.4 %) and telephone consultations (\(-\)2.7 %). This shows that being an immigrant lowered the probability of a specialist visit and telephone contact significantly. Explanations for that finding can be twofold: On the one hand, it could reflect cultural barriers to access to health care; on the other hand, it could reflect different utilization behavior. First- and second-generation immigrants had a lower probability of contacting a specialist or having a telephone consultation than those who were native born. Naturalized citizens had a lower probability of having a telephone consultation (\(-\)1.3 %) compared to natives. A look at the country of birth makes it evident that only Moroccans had a higher probability of a GP visit (5.3 %) than natives, while Asians had roughly 4.4 % fewer consultations with a GP than natives. All the remaining first-generation immigrants did not show significant differences in the probability of contacting a GP. Albanian, Romanian, non-European, and Asian individuals had a lower probability of contacting a specialist or having a telephone consultation than natives.
With regard to the control variables, we also found that females had a higher probability of contacting a specialist or GP and having a telephone consultation compared to males. As one would expect, an older age class came with a higher probability of contacting a GP. This has been expected, as age reflects physical circumstances and morbidity is associated with an increase in age. An older age class reduced the probability of contacting a specialist and having a telephone consultation, while it increased the probability of contact with a GP. Note that our reference category is constituted by children aged 0–9 years. Married individuals showed a higher probability of a doctor contact in comparison with single, widowed, never married, or divorced individuals. The presence of one or two-children in the household decreased the probability of a GP contact. However, being in a household with three or more children had significant influence on the probability of contacting specialists or having a telephone consultation. The results show a negative association of education level on the probability of contacting a specialist and having a telephone consultation and a positive association between the middle-level education and GP visits. Being unemployed, a housewife or a student had only a negative significant influence on the probability of a specialist contact with respect to the employed reference category. Being a student was associated with a higher probability of having a telephone consultation and a lower probability of contacting a GP. As one would expect, individuals reporting Bad, Very bad, and fair health status were associated with a higher probability of a doctor contact compared to those claiming that their health was Good or Excellent. People with high, low and very low wealth level had a higher probability of a doctor contact. People with low wealth had a lower probability for a specialist contact. Having a chronic disease increased the probability of a GP contact, a specialist contact, and having a telephone consultation with respect to the reference category (i.e., individuals with no chronic conditions or disability). Except for GP contact, the same applied to those with or at least one disability. Being a smoker reduced the probability of a GP or specialist visit or having a telephone consultation in comparison with being non-smoker. We also observed that modest physical activity had a positive influence on the contact decision for a specialist visit and negative for a telephone consultation.
Living in medium and small cities had a negative influence on the decision to contact a GP. The urbanity variable had no influence on the probability of contacting a specialist. Individuals from small, medium, and large cities had a higher probability of having a telephone consultation compared to those who lived in very small cities.
Second stage: frequency of health care utilization
In comparison to the contact decision, the sample size of the frequency decision (ZTNB) is reduced. Regarding the intensity of visits, immigrants were not significantly different from native-born Italians. There is weak evidence that first- and second-generation immigrants consulted specialists less often than natives (4.1 and 5.1 %, respectively). Women make more visits to a specialist and have more telephone consultations than men. Age did not influence the expected number of doctor visits. Age lowered the frequency of telephone consultations. A middle educational level led to a rise in the expected number of GP visits. Being unemployed or a housewife was associated with higher expected number of GP visits. The expected number of GP, specialists visits and telephone consultations increased with Bad and Very bad health status. The existence of a chronic disease or disability increased the expected number of all physician visits and telephone consultations. Living in a large city lowered the expected number of doctor visits. This variable had no influence on the frequency of specialist visits or telephone consultations.
Emergency visits
We performed a logit regression model (for the usual three specifications—as shown in Tables 7–9), aiming at evaluating potential differences between immigrants and the natives in the probability of use of ER services. The marginal effects and their standard errors adjusted for clustering within households are displayed in Table 10. Column 1 indicates that being an immigrant led, ceteris paribus, to a much higher probability of using emergency services than being a native (0.7 %). Similarly, first-generation immigrants visited ERs with a higher probability than natives (1 %). Immigrants from Morocco showed a greater probability of using emergency care than natives (2.8 %) followed by other Africans (1.7 %) and Albanians (1.5 %). Regarding the control variables, being female highly decreased the probability of visiting an ER in comparison to being male. Older age classes seem to be significantly and negatively correlated with the probability of using emergency services. Education level was not significant, while, with respect to the employed baseline category, being a housewife, a student, or retired strongly reduced the probability of recourse to an ER. Individuals reporting Fair and Bad or Very bad health status are associated with a higher probability of using an ER compared to those claiming that their health is Good or Excellent. Individuals living in the North, Center or in the Islands had a much higher probability of using ER services compared to those living in the South. In detail, residing in the North-East, in the North-West, in the Center, and in the Islands led respectively to a 2.8, 2.1, and 2.4 % increase in the probability of ER usage.
Discussion
The primary aim of this research has been to investigate the association between immigration status and healthcare utilization in Italy. We have also been interested in investigating the importance of other predisposing factors as well as enabling, behavioral, and health system factors affecting healthcare utilization using all information on individual and health system-related characteristics. Our analysis finds that immigrants tend to use specialist services and have telephone consultations less frequently than natives, whereas they use ER services more often than natives. These results are also in line with other international studies (Sanz and Torres 2000; Sarma and Simpson 2006; Muñoz de Bustillo and Antón 2010). As noted earlier, there might be several explanations for why immigrants avail themselves of more or fewer health care services than natives. The perceived benefits and the costs in terms of efforts required to access various types of health care might vary between immigrants and natives and therefore might result in different choices in terms of whether to demand health services and which services to demand.
The over-utilization of urgent care services by immigrants compared with natives may have different explanations. Emergency services are easier to access for immigrants and provide an immediate solution to their health care needs by reducing language, cultural, and bureaucratic barriers that immigrants may face when trying to access ordinary health care services (primary and specialist medical services, consultations provided by phone). These results also constitute evidence of the immigrants’ tendency to substitute excessive use of ER services for both specialty and preventive medicine (leading to a an increase in the consumption of more costly medical services). Moreover, immigrants may also tend to overuse urgent care services because they are usually employed in high-risk jobs and thus are more exposed to the risk of accidents at work. The higher usage of emergency care services by the immigrant community compared to the native population is in line with previous findings (Sanz and Torres 2000; Cots et al. 2007; Muñoz de Bustillo and Antón 2010).
In regards to the other control variable, gender is associated with GP and specialist visits, telephone consultations, and ER utilization. Females tend to use fewer emergency services and more GP and specialist visits and have more telephone consultations than males. Women might also make more specialist visits because of motherhood and childbirth. This is consistent with other international studies (Cameron et al. 1998; Dunlop et al. 2000; Burón et al. 2008; Dias et al. 2008) and the Italian pattern observed in another study (Masseria and Giannoni 2010). The use of GP services increases with age groups. The effect of age is the reverse with negative associations with specialist visits, telephone consultations, and ER visits (see Asada and Kephart 2007). Wealth does influence GP and ER utilization. The use of health care services increases with increasing family wealth. This finding is in line with previous studies claiming that people with higher incomes visit the general practitioner more than people with lower incomes (Van Doorslaer et al. 2006; Allin et al. 2009). Another significant result is that marital status is determinative of all visits. The presence of children is also relevant when explaining the intensity of the use of health care services.
Individuals with higher levels of education visit GPs less often but visit more specialists and have more telephone medical consultations than those with lower levels of education. The decrease in the number of GP visits is consistent with the idea that individuals with higher education are more efficient at managing their health and, therefore, we would expect to see them consume fewer health care services (Grossman 1972, 1982; Wagstaff 1996; Hernández Quevedo and Jiménez Rubio 2009).Footnote 11 Other studies find that visit counts increase with education (see for instance, Santos Silva and Windmeijer 2001; Deb and Trivedi 2002). Consistent with this position, we find that individuals with poor health make more GP and specialist visits, use the ER more frequently, and have more telephone consultations. This finding also supports previous empirical literature for Italy (Fabbri and Monfardini 2003; Masseria and Giannoni 2010).
Behavioral risk factors, for example smoking behavior, has been found to influence negatively the utilization of GP services and positively the use of ER services. This result is in line with other international studies (for example, Sarma and Simpson 2006 for Canada). People who engage in physical exercise visit their GPs and specialists more often and use ER services more frequently.
Results of this paper are subject to some caveats. The health outcome variables might suffer from endogeneity bias. For instance, the use of preventive health care services can reduce the possibility of developing certain chronic conditions. Moreover, potential bias may still arise if unobservable factors are correlated with the decisions of immigrants to utilize healthcare services. For instance, if immigrant individuals are different from native people in some unobservable characteristics, such as being unhealthier than native people, then the estimated effects can partly capture these unmeasured differences in healthcare utilization. Finally, our study does not account for immigrants’ number of years of residence in Italy. This variable has been identified in other studies as an important predictor of health care service utilization, as it might be a proxy variable for the knowledge of the health system (e.g., Dias et al. 2008; Nolan 2011). Future research should consider the inclusion of these factors.
Conclusion
This study provides empirical evidence of the effect of immigration status on healthcare utilization in Italy by using individual records from the Italian Health Conditions Survey (ISTAT 2005). Inverse associations are observed between immigration status and specialist visits and between immigration status and medical telephone consultations. A positive association is observed for ER services, and no evidence is found for either increased or decreased frequency of GP visits. What clearly emerges from our study is an over-utilization of emergency services associated with an under-utilization of preventive care services among the immigrant population. It is worthwhile to notice that the Italian national health system has universal coverage, and resident immigrants are regularly granted the same access to and use of health care services as the native population. Illegal immigrants, in contrast, are only provided coverage for emergency care and for preventive care and treatment related to communicable disease and pregnancy and childbirth (see art.35, Legislative Decree 286/98). Since legal immigrants have the same rights as Italian citizens, a number of factors may explain the over-use of ERs by immigrant individuals in comparison to the natives. First, emergency services respond more easily to immigrants’ health care needs by offering an immediate solution to a given health problem. Second, language difficulties, which can complicate making appointments with primary care physicians by phone, may result in using emergency services as a substitute. Language difficulties can also lead to a misunderstanding of the information related to preventive care, to treatment, and more broadly to access to the health care system. Third, immigrants may use emergency services as a substitute for regular health services because of a lack of knowledge about the health care system and the easier access they have to hospital facilities. Finally, since immigrants are usually employed in high-risk jobs and thus are more exposed to the risk of accidents at work, a higher incidence of accidents among them may also explain the excessive use of emergency services.
The immigrants’ excessive use of emergency services at the expense of specialty and preventive medicine creates some doubt about not only the equity in access to the healthcare system but also its efficiency, the latter being threatened by an increase in the consumption of more costly medical services. (being emergency care free of charge at the point of delivery).
The results of the study suggest the societal value of implementing adequate national policies directed towards promoting better knowledge about the health care system and about the rights and duties of those who use it as well as the usefulness of simplifying bureaucratic procedures. Italy should prioritize (as do the U.K. and Spain) the reduction of disparities in health care utilization between immigrants by improving both the availability of information and communication between providers and immigrants by making translation services available both in person and by telephone, and increasing the service supply (i.e., dedicated community-based healthcare structures or consulting services) especially in the most disadvantaged areas. These policies may contribute to reducing the need for costly emergency care and more generally to improving the health of the immigrant population. The Italian Ministry of Health, while confirming universality of health care and equity as basic principles of the Italian SSN, needs to highlight some major objectives for its future development including the adoption of a specific health policy for immigrant individuals through appropriate health promotion campaigns or service delivery schemes in order to ensure an equitable access to the Italian SSN among the immigrant population.
Notes
For instance, the EU paid attention to disparities in the delivery of health care to immigrants by assisting the research program named Assisting Migrants and Communities: Analysis of Social Determinants of Health and Health Inequalities in 2007.
Servizio Sanitario Nazionale.
In some countries (for instance, Canada) immigrants are screened for good health before entering the country. This might also result in lower health care use.
This healthy effect could disappear as a result of the stress of adapting and of reallocation.
In the formal literature, some empirical studies documented the existence of disparities in health care use according to country of origin (for instance, Glaesmer et al. 2011). All these countries of origin might be characterized by different religious practices. They are also culturally speaking far from each other (other Western European countries and Morocco, Albania, and Romania) as well as in some cases geographically distant.
The same can be applied to our measures of self-reported indicators included in the empirical analysis that might be measured with error (for instance, see Benitez-Silva et al. 2004).
In the survey, individuals are asked whether or not the disease is diagnosed by a physician.
North-West includes the following regions: Piedmont, Valle d’Aosta, Lombardy, Liguria; North-East includes Veneto, Trentino Alto Adige, Friuli Venezia Giulia, Emilia Romagna; Center includes Tuscany, Lazio, Marche, Umbria; South includes Abruzzi, Campania, Apulia, Molise, Basilicata, Calabria; Islands includes Sicily and Sardinia.
Results are available upon request to authors.
To check the robustness of our results we have also estimated a Zero-Inflated Negative Binomial model for telephone consultations, the results concerning our variable of interests remain nearly unchanged.
Although a person with formal education and in better health could tend to use more GP services for preventive care reasons. See, for instance, Birch et al. (1993).
References
Agenzia Nazionale per i Servizi Sanitari Regionali. (2008). Elementi di analisi e osservazione del sistema salute. Anno VII, Numero 21, Roma, Italy.
Allin, S., Masseria, C., & Mossialos, E. (2009). Measuring socioeconomic differences in use of health care services by wealth versus by income. American Journal of Public Health, 99, 1849–1855.
Ambrosseti, E. (2009). The impact of economic crisis on migration flows between Italy and North Africa. CARIM Analytic and Synthetic Notes 2009/36. Robert Schuman Centre for Advanced Studies. European University Institute.
Andersen, R., & Newman, J. (1973). Societal and individual determinants of medical care utilization in the United States. Milbank Quarterly, 51, 95–124.
Asada, Y., & Kephart, G. (2007). Equity in health services use and intensity of use in Canada. BMC Health Services Research, 7, 41.
Bach, P. B., Pham, H. H., Schrag, D., Tate, R. C., & Hargraves, J. L. (2004). Primary physicians who treat blacks and whites. New England Journal of Medicine, 5(6), 575–584.
Baglio, G., Saunders, C., Spinelli, A., & Osborn, J. (2010). Utilisation of hospital services in Italy: A comparative analysis of immigrant and Italian citizens. Journal of Immigrant and Minority Health, 12(4), 598–609.
Barros, P. P., & Pereira, I. M. (2010). Health care and health outcomes of immigrants: Evidence from Portugal. CEFAGE-UAE Working Papers 2010/04, Evora, Portugal.
Benitez-Silva, H., Buchinsky, M., Chan, H. M., Cheidvasser, S., & Rust, J. (2004). How large is the bias in self-reported disabilty? Journal of Applied Econometrics, 19, 649–670.
Birch, S., Eyles, J., & Newbold, K. B. (1993). Equitable access to health care: Methodological extensions to the analysis of physician utilization in Canada. Health Economics, 2(2), 87–101.
Borjas, G. J. (2000). The economic progress of immigrants. In J. B. George (Ed.), Issues in the economics of immigration (pp. 15–49). Chicago: University of Chicago Press.
Burón, A., Cots, F., García, O., Vall, O., & Castells, X. (2008). Hospital emergency department utilization rates among the immigrant population in Barcelona, Spain. BMC Health Services Research, 8, 51–60.
Cacciani, L., Baglio, G., Rossi, L., Materia, E., Marceca, M., Geraci, S., et al. (2006). Hospitalisation among immigrants in Italy. Emerging Themes in Epidemiology, 3, 4.
Calderón-Larrañaga, A., Gimeno-Feliu, L. A., Macipe-Costa, R., Poblador-Plou, B., Bordonaba-Bosque, D., & Prados-Torres, A. (2011). Primary care utilisation patterns among an urban immigrant population in the Spanish National Health System. BMC Public Health, 11, 432.
Cameron, A. C., & Trivedi, P. K. (1998). Regression analysis of count data. New York: Cambridge University Press.
Cameron, A. C., Trivedi, P. K., Milne, F., & Piggot, J. (1998). A microeconometric model of the demand for health care and health insurance in Australia. Review of Economic Studies, 55, 85–106.
Chaouchi, S., Casu, C., & Caussidier, J. (2006). L’état de santé et accès aux soins des migrants en France. Montpellier: ORS.
Costa, G., Spadea, T., Faggiano, F., & Cardano, M. (2000). Diseguaglianze nella salute: determinanti e politiche in Italia negli anni ‘90. Report.
Cots, F., Castells, X., García, O., Riu, M., Felipe, A., & Vall, O. (2007). Impact of immigration on the cost of emergency visits in Barcelona. BMC Health Services Research, 7, 9.
Cotter, J. (2008). The determinants of health care use utilization in Portugal: An approach with count data models. Swiss Journal of Economics and Statistics, 144, 437–458.
Crimmins, E. M., Kim, J. K., Alley, D. E., Karlamangla, A., & Seeman, T. (2007). Hispanic paradox in biological risk profiles. American Journal of Public Health, 97, 1305–1310.
Deb, P., & Trivedi, P. K. (2002). The structure of demand for health care: Latent class versus two-partmodels. Journal of Health Economics, 41, 601–625.
Del Boca, D., & Venturini, A. (2003). Italian migration. IZA Discussion Paper No. 938.
Dias, S. F., Severo, M., & Barros, H. (2008). Determinants of health care utilization by immigrants in Portugal. BMC Health Services Research, 8, 207.
Dunlop, S., Coyte, P. C., & McIsaac, W. (2000). Socio-economic status and the utilisation of physicians’ services: Results from the Canadian National Population Health Survey. Social Science and Medicine, 51(1), 123–133.
ECDC. (2009). Migrant health: Background note to the ECDC Report on migration and infectious diseases in the EU. ECDC Technical report.
Fabbri, D., & Monfardini, C. (2003). Public vs. private health care services demand in Italy. Giornale degli Economisti e Annali di Economia, 62, 93–123.
Fernandes, A., & Miguel, J. P. (2009). Health and migration in the European Union: Better health for all in an inclusive society. Lisboa: Instituto Nacional de Saúde Doutor Ricardo Jorge.
Flores, G., Abreu, M., Olivar, M. A., & Kastner, B. (1998). Access barriers to health care for Latino children. Archives of Pediatrics and Adolescent Medicine, 152, 1119–1125.
France, G., Taroni, F., & Donatini, A. (2005). The Italian health care system. Health Economics, 14, S187–S202.
García-Gomez, P. (2007). Salud y utilización de recursos sanitarios: Un análisis de las diferencias y similitudes entre población inmigrante y autóctona. Presupuesto y Gasto Público, 49, 67–85.
Gerdtham, U. G., & Trivedi, P. K. (2001). Equity in Swedish health care reconsidered: New results based on the finite mixture model. Health Economics, 10, 565–572.
Glaesmer, H., Wittig, U., Braehler, E., Martin, A., Mewes, R., & Rief, W. (2011). Health care utilization among first and second generation immigrants and native born Germans: A population based study. International Journal of Public Health, 56, 541–548.
Grossman, M. (1972). On the concept of health capital and the demand for health. Journal of Political Economy, 80(2), 223–255.
Grossman, M. (1982). The demand for health after a decade. Journal of Health Economics, 1(1), 1–3.
Hernández Quevedo, C., & Jiménez Rubio, D. (2009). A comparison of health status and health care utilization patterns between foreigners and the national population in Spain: New evidence from Spanish National Health Survey. Social Science and Medicine, 69, 370–378.
Hjern, A., Haglund, B., Persson, G., & Rosén, M. (2001). Is there equity in access to health services? European Journal of Public Health, 11, 147–152.
ISTAT (2005). Salute e ricorso ai servizi sanitari della popolazione straniera residente in Italia - Anno2005. Statistiche in breve - Sanità, ISTAT, Roma. Available from http://www3.istat.it/salastampa/comunicati/non_calendario/20081211_00/.
Jasso, G., Massey, S. D., Rosenzweig, M. R., & Smith, J. P. (2004). Immigrant health: Selectivity and acculturation. In N. B. Anderson (Ed.), Critical perspectives on racial and ethnic differences in health in late life. Washington, DC: National Academies Press.
Jensen, N. K., Nielsen, S. S., & Krasnik, A. (2010). Expert opinion on best practices in the delivery of health care services to immigrants in Denmark. Danish Medical Bulletin, 57(8), A4170.
Kao, D. T. (2009). Generational cohorts, age at arrival, and access to health services among Asian and Latino immigrant adults. Journal of Health Care Poor Underserved, 20, 395–414.
Kristiansen, M., Mygind, A., & Krasnik, A. (2007). Health effects of migration. Danish Medical Bulletin, 54, 46–47.
Leclere, F. B., Jensen, L., & Biddlecom, A. E. (1994). Health-care utilization, family context, and adaptation among immigrants to the United States. Journal Health and Social Behaviour, 35, 370–384.
Masseria, C., & Giannoni, M. (2010). Equity in access to health care in Italy: A disease-based approach. European Journal of Public Health, 20, 504–510.
Ministero dell Interno. (2007). Primo Rapporto sugli immigrati in Italia. Roma: Ministero dell” Interno.
Muñoz de Bustillo, R., & Antón, J. I. (2010). Health care utilization and immigration in Spain. European Journal of Health Economics, 11, 487–498.
Nauenberg, E., Laporte, A., & Shen, L. (2011). Social capital, community size and utilization of health services: A lagged analysis. Health Policy, 103(1), 38–46.
Nolan, A. (2011). The healthy immigrant effect: Initial evidence for Ireland. Health Economics Policy Law, 19, 1–20.
Norredam, M., Krasnik, A., Sorensen, T. M., Keiding, N., Michaelsen, J. J., & Nielsen, A. S. (2004). Emergency room utilization in Copenhagen: A comparison of immigrant groups and Danish born residents. Scandinavian Journal of Public Health, 32, 53–59.
Norredam, M., Nielsen, S. S., & Krasnik, A. (2009). Migrants’ utilization of somatic healthcare services in Europe—A systematic review. European Journal of Public Health, 20(5), 555–563.
Petrelli, A., Picariello, R., & Costa, G. (2010). Towards a needs based mechanism for capitation purpose in Italy: The role of socio-economic level in explaining differences in the use of health services. International Journal of Health Care and Finance, 10, 29–42.
Pohlmeier, W., & Ulrich, V. (1995). An econometric model of the two-part decision making process in the demand for health care. Journal of Human Resources, 30(2), 339–361.
Rue, M., Cabre, X., Soler Gonzalez, J., Bosch, A., Almirall, M., & Serna, M. C. (2008). Emergency hospital services utilization in Lleida (Spain). A cross sectional study of immigrant and Spanish born populations. BMC Health Services Research, 8, 81.
Rumbaut, R. G. (2004). Ages, life stages, and generational cohorts: Decomposing the immigrant first and second generations in the United States. International Migration Review, 38, 1160–1205.
Santos Silva, J. M. C., & Windmeijer, F. (2001). Two-part multiple spell models for health care demand. Journal of Econometrics, 104, 67–89.
Sanz, B., & Torres, A. M. (2000). Sociodemographic characteristics and use of health services by the immigrant population residing in a district of the community of Madrid. Atencion Primaria, 26, 314–318.
Sarma, S., & Simpson, W. (2006). A microeconometric analysis of Canadian healthcare utilization. Health Economics, 15(3), 219–239.
Solé-Auró, A., Guillén, M., & Crimmins, E. (2009). Health care utilization among immigrants and native born populations in 11 European countries. Results from the survey of Health, Ageing, and Retirement in Europe. Document de Treball XREAP 2009–2010.
Steinhausen, H. C., Bearth-Carrari, C., & Metzke, C. W. (2009). Psychosocial adaptation of adolescent migrants in a Swiss community survey. Social Psychiatry Epidemiology, 44, 308–316.
Stronks, K., Ravelli, A., & Reijneveld, S. (2001). Immigrants in the Netherlands: Equal access for equal needs? Journal of Epidemiology of Community Health, 55, 701–707.
Tarraf, W., Miranda, P. Y., & González, H. M. (2012). Medical expenditures among immigrant and nonimmigrant groups in the United States: Findings from the medical expenditures panel survey (2000–2008). Medical Care, 50(3), 233–242.
Tognetti Bordogna, M. (Ed.). (2008). Disuguaglianze di salute e immigrazione. Milano: Angeli F.
Uiters, E., Devillé, W. L., Foets, M., & Groenewegen, P. P. (2006). Use of health care services by ethnic minorities in The Netherlands: Do patterns differ? European Journal of Public Health, 16(4), 388–393.
Van Doorslaer, E., Masseria, C., & Koolman, X. (2006). Inequalities in access to medical care by income in developed countries. Canadian Medical Association Journal, 174, 177–183.
Vuong, Q. H. (1989). Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica, 57(2), 307–333.
Wagstaff, A. (1996). The demand for health: Some new empirical evidence. Journal of Health Economics, 5, 195–233.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Luca, G., Ponzo, M. & Andrés, A.R. Health care utilization by immigrants in Italy. Int J Health Care Finance Econ 13, 1–31 (2013). https://doi.org/10.1007/s10754-012-9119-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-012-9119-9