Abstract
The purpose of this study was to investigate the inhibition neuroinflammation mechanisms of hyperbaric oxygen therapy (HBOT). Primary astrocytes were incubated with lipopolysaccharide (LPS) after which they underwent HBOT and separate administration of inflammatory cytokine inhibitors. The respective expression of inflammatory factors was then detected. Results showed that LPS significantly induced increases in the expression levels of chemokine (C-X-C motif) ligand 1 (CXCL1), chemokine C-C motif ligand 2 (CCL2), phospho-nuclear factor-kappa B (p-NF-κB), phospho-c-Jun N-terminal kinase (p-JNK), phospho-extracellular signal-regulated kinase (p-ERK), and phospho-p38 (p-p38) in cultured astrocytes and peaked at 3 h. HBOT downregulated the expression of some inflammation mediators including CXCL1 and CCL2. Furthermore, HBOT inhibited the expression of some up-stream regulators of inflammation mediators including p-NF-κB, p-JNK, p-p38 (at 3 and 6 h), and p-ERK (3 h). Inhibitors of NF-κB, ERK, and JNK (BAY117082, PD98059, and SP600125) significantly suppressed the expression of CXCL1 and CCL2 that were induced by LPS for 3 h. However, the p38 inhibitor, SB203580, had no obvious effect on expression levels of CXCL1 and CCL2. In conclusion, we found that HBOT inhibits neuroinflammation via regulation of the LPS-induced NF-κB/mitogen-activated protein kinases (MAPKs, JNK, and ERK) -CCL2/CXCL1 signaling pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
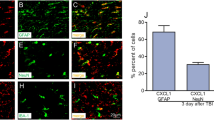
Neuroinflammation is prominent in the short- and long-term responses of neuronal injuries that occur after traumatic brain injury (TBI). Neuroinflammation involves the activation of astrocytes and microglia followed by the active release of inflammatory mediators such as chemokines and cytokines by activated astrocytes [1, 2]. The chemokine C-C motif ligand 2 (CCL2, also known as monocyte chemoattractant protein-1 (MCP-1) and chemokine (C-X-C motif) ligand 1 (CXCL1) are key mediators of inflammation following TBI [3,4,5]. Consistent with the above, our previous study showed that astrocytes of injured brains activated significantly in TBI rats [6]. We also found that CCL2 protein was mainly co-localized with the astroglial marker glial fibrillary acidic protein (GFAP) and that the expression of CCL2 was significantly increased in the injured cortex of TBI rats [7].
Hyperbaric oxygen therapy (HBOT) is widely used in TBI and has a neuroprotective effect by inhibiting the inflammatory response to TBI. Current reports have demonstrated that the neuroprotective effect of HBOT is partly realized by inhibiting or alleviating the inflammatory response with changes in expression levels of inflammatory factors such as interleukin (IL)-6, IL-1, IL-10, IL-1β, IL-18, CXCL1, CCL2, and tumor necrosis factor-α (TNF-α) in TBI animal studies [8,9,10,11,12]. Our preliminary studies demonstrated that the number of astrocytes in the ipsilateral hippocampal region and cortex in TBI rats was significantly reduced after 2 weeks of HBOT [6].
Based on above studies, HBOT reduced the activation of astrocytes and inhibited inflammation responses, but the mechanisms have not been fully clarified. In this study, the main aim was to investigate the effects of HBOT on lipopolysaccharide (LPS)-activated inflammatory mediator production (CXCL1, CCL2) in primary astrocytes from cerebral cortices of neonatal rats. In addition, we also studied whether HBOT has any effect on mitogen-activated protein kinases (MAPKs) and nuclear factor-kappa B (NF-κB), as well as explore possible mechanisms of inhibition of inflammation by HBOT.
MATERIALS AND METHODS
Primary Astrocytes Cultures
Primary astrocyte cultures were prepared from cerebral cortices of neonatal rats [13, 14]. Neonatal rats were provided by the Experimental Animal Center of Nantong University, China (Nantong, China). Bilateral cerebral cortices were isolated and transferred to ice-cold D-Hank’s buffer and the meninges were carefully removed. The tissues were then dissociated and filtered through nylon mesh with a pore size of 100 μm and collected by centrifugation at ~ 3000×g for 5 min. The cell pellets were dispersed with a pipette and resuspended in a medium containing 10% fetal bovine serum (FBS) in low glucose Dulbecco’s Modified Eagle’s Medium (Gibco, Grand Island, NY, USA). After trituration, the cells were filtered through a 10-μm screen and then seeded into 6-well plates at a density of 2.5 × 105 cells/cm2 and cultured for approximately 10 days. The medium was replaced every 3 days with 10% FBS. Dibutyryl cAMP (d-cAMP, 0.15 mM, Sigma, CA, USA) was added to induce morphological and functional differentiation when the cells were grown to 90% confluence.
The cells were used 3 days later. Opti-MEM (Gibco, Grand Island, NY, USA) was replaced and then the cells were incubated with lipopolysaccharide (LPS, 1 μg/mL, Santa Cruz, CA, USA) for different time periods from 1 to 12 h depending on the following experiments.
HBOT Intervention
When the astrocytes were ready, they were randomly divided into 4 groups: (1) control group; (2) control + HBO group; (3) LPS group; and (4) LPS + HBO group. The cells of the control + HBO group and LPS + HBO group at 2 or 5 h were transferred individually to HBO chamber [15]. The oxygen pressure was first increased over 10 min to 2 atm absolute (ATA), held at 2 ATA for 60 min (O2 concentration above 98%), and then decreased over 10 min to atmospheric pressure for an 80-min HBO exposure. After the treatments, the cells were collected for ELISA or western blotting.
Drugs Administration
Inhibitors of NF-κB, ERK, JNK, and p38 were purchased from Calbiochem (Merck, Darmstadt, Germany). Before 30-min LPS induction, cells were pre-treated with specific inhibitors, including NF-κB inhibitor (BAY117082), JNK inhibitor (PD98059), ERK inhibitor (SP600125), and p38 inhibitor (SB203580) using two different doses: 20 and 50 μmol/L. Cultured cells were then collected for further experiments.
ELISA
Rat CCL2 ELISA kit was purchased from R&D systems (MN, USA). Rat CXCL1 ELISA kit was purchased from Lianke-Bio systems (Hangzhou, China). For in vitro experiments, cultured cells were collected after treatment or stimulation. Protein concentrations were determined by BCA Protein Assay (Pierce, Rockford, IL, USA). For each reaction in a 96-well plate, 100 μg of proteins or 100 μL of culture medium were used, and ELISA was performed according to manufacturer’s protocol. The standard curve was included in each experiment.
Western Blotting
Protein samples were prepared in the same way as for ELISA analysis, and 30 μg of proteins were loaded for each lane and separated on SDS-PAGE gel (10%, Beyotime, Shanghai, China). After the transfer, the blots were incubated overnight at 4 °C with polyclonal antibody against p-NF-κB (anti-rabbit, 1:1000, Cell signaling, Boston, USA), p-JNK (1:500, anti-rabbit, Cell signaling, Boston, USA), p-ERK (rabbit, 1:1000, Cell signaling, Boston, USA), and p-p38 (anti-rabbit, 1:1000, Cell signaling, Boston, USA). For loading control, the blots were probed with GAPDH antibody (1:10000, anti-mouse, Millipore, Billerica, MA, USA). These blots were further incubated with IRDye® 800CW (1:10000, Goat anti-Rabbit IgG, LICOR, Lincoln, NE, USA; 1:10000, Goat anti-Mouse IgG, LICOR, Lincoln, NE, USA) for 2 h. Blots were exposed with CLx Infrared Imaging System (LICOR, Lincoln, NE, USA). The intensity of the selected bands was analyzed using Image J software (NIH, Bethesda, MD, USA).
Quantification and Statistical Analysis
All data were expressed as mean ± SEM. For the quantification of Western blot, the density of specific bands for p-NF-κB, p-JNK, p-ERK, p-p38, and GAPDH were measured with imaging J software. The differences between groups were tested for statistical significance using one-way analysis of variance (ANOVA), followed by Tukey’s post hoc multiple comparison tests. Differences between two groups were compared using Student’s t test. The criterion for statistical significance was P < 0.05.
RESULTS
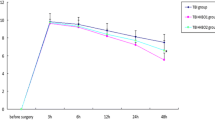
LPS Induces Increase of CXCL1 and CCL2 Expression in Cultured Astrocytes
The change in levels of expression of CXCL1 and CCL2 in primary astrocytes by LPS induction were detected by ELISA at 1, 3, 6, and 12 h. As shown in Fig. 1, the expression levels of CXCL1 and CCL2 in primary astrocytes were higher at 1 h compared to the control group. The peak expression levels for both transcripts were reached at 3 and 6 h of coculture with LPS and gradually decreased thereafter.
LPS Induces Upregulation of p-NF-κB, p-JNK, p-ERK, and p-p38 Expression in Cultured Astrocytes
LPS-induced NF-κB, JNK, ERK, and p38 activation in primary astrocytes was detected by western blotting at 1, 3, and 6 h. As shown in Fig. 2, the expression levels of p-NF-κB, p-JNK, p-ERK, and p-p38 in primary astrocytes were higher at 1 h compared with the control group. The peak expression levels of p-NF-κB, p-JNK, p-ERK, and p-p38 were all reached at 3 h of coculture with LPS and gradually decreased thereafter.
HBOT Suppresses LPS-Induced Expressions of CXCL1 and CCL2
To investigate the anti-inflammatory effects of HBOT on neuroinflammation, in LPS-induced primary astrocytes, ELISA was used to explore the changes of CXCL1 and CCL2 expression. As shown in Fig. 3a, b, the results showed that the exposure of primary astrocytes to LPS increased the production of CXCL1 and CCL2. Compared with the LPS group, CXCL1 and CCL2 expression in the HBO + LPS group was significantly reduced with HBO therapy 1 h after LPS stimulation at 3 and 6 h. These results demonstrate HBOT can downregulate the expression of CXCL1 and CCL2.
a HBOT inhibits CXCL1 expression in activated astrocytes. The values presented are the means ± SEM of four independent experiments. *P < 0.05, ***P < 0.001 vs. LPS group. b. HBOT inhibits CCL2 expression activated astrocytes. The values presented are the means ± SEM of four independent experiments. *P < 0.05, ***P < 0.001 vs. LPS group.
HBOT Reduces LPS-Induced Activation of p-NF-κB, p-JNK, p-ERK, and p-p38
To investigate the anti-inflammatory mechanism of HBOT, LPS-induced NF-κB, JNK, ERK, and p38 activation was detected in this study. As shown in Fig. 4a, a significant increase in expression of p-NF-κB, p-JNK, p-ERK, and p-p38 resulted from LPS stimulation for 3 h in primary astrocytes was suppressed by HBO therapy for 1 h. As shown in Fig. 4b, HBO therapy on primary astrocytes for 1 h after coculture for 5 h with LPS resulted in a significant reduction in expression of p-NF-κB, p-JNK, and p-p38, although HBOT had no significant effect on p-ERK expression. From the above results, we concluded that HBOT may inhibit the expression of some up-stream regulators of mediators of inflammation. This needs to be examined more carefully.
a HBOT inhibits p-NF-κB, p-JNK, p-ERK, and p-p38 expressions after astrocyte activation by LPS-induced 3 h. The values presented are the means ± SEM of four independent experiments. *P < 0.05, ***P < 0.001 vs. LPS group. ###P < 0.001 vs. control group. b HBOT inhibits p-NF-κB, p-JNK, and p-p38 expressions after astrocyte activation by LPS-induced 6 h. The values presented are the means ± SEM of four independent experiments. *P < 0.05, **P < 0.01 vs. LPS group. ##P < 0.01, ###P < 0.001 vs. control group.
Inhibitors NF-κB, JNK, and ERK Decrease CXCL1 and CCL2 Expressions
Based on the above results, we speculated that HBOT suppressed expression of CXCL1 and CCL2 by inhibiting the production of up-stream regulators of CXCL1 and CCL2. To verify this, we explored the changes in levels of expression of CXCL1 and CCL2 after pre-treated with inhibitors of NF-κB, ERK, JNK, or p38 at different doses (20 and 50 μM). As shown in Fig. 5a, b, inhibitors of NF-κB, ERK, and JNK (BAY117082, PD98059, and SP600125) significantly suppressed expression of CXCL1 and CCL2, which had been induced by LPS for 3 h. However, p38 inhibitor SB203580 (20 and 50 μM) had no obvious effect on expression of CXCL1 and CCL2. From the above results, we concluded that HBOT suppressed expression of CXCL1 and CCL2, by inhibiting the production of some up-stream regulators of CXCL1 and CCL2, including NF-κB, ERK, and JNK.
a Inhibitors p-NF-κB (BAY117082, 20 and 50 μM), p-JNK (PD98059, 50 μM), and p-ERK (SP600125, 20 and 50 μM) reduce CXCL1 expression in activated astrocytes. *P < 0.05, **P < 0.01, ***P < 0.001 vs. LPS group. ###P < 0.001 vs. control group. b Inhibitors of p-NF-κB (BAY117082, 20 and 50 μM), p-JNK (PD98059, 20 and 50 μM), and p-ERK (SP600125, 20 and 50 μM) reduce CCL2 expression in activated astrocytes. **P < 0.01, ***P < 0.001 vs. LPS group. ###P < 0.001 vs. control group.
DISCUSSION
Astrocyte secreted chemokines CCL2 and CXCL1 are important mediators of inflammation that recruit inflammatory cells to sites of tissue injury in the central nervous system [7, 16,17,18,19]. CXCL1 secreted by astrocytes, and endothelial CXCR2 play essential roles in cerebral endothelial activation and subsequent leukocyte recruitment during neuroinflammation after intracerebroventricular injection of LPS [19]. LPS molecules are essential outer membrane components of most Gram-negative bacteria, which is composed of lipid, O-antigen, and the core oligosaccharide [20]. Astrocytes play a key role in the maintenance of neuronal functions in the central nervous system by producing various cytokines and chemokines. LPS-induced astrocytes release inflammatory molecules such as TNF-α, IL-10, CCL2 (MCP-1), NF-κB, ERK, JNK, and p38 in animal experiments [21,22,23]. In cultured human astrocytes, some expressed chemokines include CXCL1 and CCL2. The NF-kB signaling pathway differentially regulates gene expression of chemokines that play both neuroprotective, and neurotoxic roles in neuroinflammation in human astrocytes under physiological and inflammatory conditions [24].
In this study, LPS induced significant upregulation of CXCL1, CCL2, p-NF-κB, p-JNK, p-ERK, and p-p38 expression in cultured primary astrocytes. Inhibitors of NF-κB, ERK, and JNK significantly suppressed expression of CXCL1 and CCL2 that was induced by 3-h LPS treatment. However, p38 inhibitor had no obvious effect on expressions of CXCL1 and CCL2. The results confirmed the role of NF-κB, ERK, and JNK signaling pathways by using specific inhibitors, which mediated suppression of LPS-induced CXCL1 and CCL2 production.
TBI secondary injury involves a cascade of molecular mechanisms that are activated over hours to days and include the critical mechanism of neuroinflammation [25, 26]. TBI significantly up-regulated MAPKs (ERK, JNK, and p38) and NF-κB signaling, in injured brain regions of a rodent model of TBI, which also involved a proinflammatory response [27,28,29]. HBOT is defined as the inhalation of pure oxygen in a hyperbaric chamber that is pressurized higher than 1 absolute atmosphere and proposed widely as an effective treatment for TBI. HBOT reduces proinflammatory factor generation and promotes anti-inflammatory factor production, thereby reducing inflammatory responses in brain tissue and assisting in reducing TBI secondary injury [8, 30, 31]. Our study demonstrated HBOT alleviated the expression of proinflammatory mediators CXCL1 and CCL2, in LPS induced in primary astrocytes. HBOT has recognized therapeutic effect through inhibition of the Toll-like receptor 4 (TLR4)/NF-kB and vascular endothelial growth factor (VEGF)/ERK signaling pathways after TBI in rats [10, 32]. We furthermore found that HBOT downregulated the expressions of up-stream regulators of inflammatory mediators including p-NF-κB, p-JNK, p-p38, and p-ERK. Taken together, these results suggested that HBOT inhibited LPS-induced CXCL1 and CCL2 by inhibiting NF-κB, JNK, and ERK signaling pathways in cultured primary rat astrocytes.
In conclusion, our results showed that HBOT inhibited neuroinflammation via inhibiting the LPS-induced NF-κB/MAPKs (JNK and ERK)-CCL2/CXCL1 signaling pathways. This provides the theoretical basis for clinical treatment with HBOT.
References
Chiu, C.C., Y.E. Liao, L.Y. Yang, J.Y. Wang, D. Tweedie, H.K. Karnati, N.H. Greig, and J.Y. Wang. 2016. Neuroinflammation in animal models of traumatic brain injury. Journal of Neuroscience Methods 272: 38–49.
Gyoneva, S., and R.M. Ransohoff. 2015. Inflammatory reaction after traumatic brain injury: Therapeutic potential of targeting cell-cell communication by chemokines. Trends in Pharmacological Sciences 36 (7): 471–480.
Yang, T., Y.W. Liu, L. Zhao, H. Wang, N. Yang, S.S. Dai, and F. He. 2017. Metabotropic glutamate receptor 5 deficiency inhibits neutrophil infiltration after traumatic brain injury in mice. Scientific Reports 7 (1): 9998.
Dalgard, C.L., J.T. Cole, W.S. Kean, J.J. Lucky, G. Sukumar, D.C. McMullen, H.B. Pollard, and W.D. Watson. 2012. The cytokine temporal profile in rat cortex after controlled cortical impact. Frontiers in Molecular Neuroscience 5: 6.
Foerstner P, Rehman R, Anastasiadou S, Haffner-Luntzer M, Sinske D, Ignatius A, Roselli F, Knoell B. Neuroinflammation after traumatic brain injury (TBI) is enhanced in activating transcription factor 3 (ATF3) mutant mice. Journal of Neurotrauma 2018.
Liu, S., G.Y. Shen, S.K. Deng, X.B. Wang, Q.F. Wu, and A.S. Guo. 2013. Hyperbaric oxygen therapy improves cognitive functioning after brain injury. Neural Regeneration Research 8 (35): 3334–3343.
Liu, S., L. Zhang, Q. Wu, Q. Wu, and T. Wang. 2013. Chemokine CCL2 induces apoptosis in cortex following traumatic brain injury. Journal of Molecular Neuroscience 51 (3): 1021–1029.
Chen, X., X.S. Duan, L.J. Xu, J.J. Zhao, Z.F. She, W.W. Chen, Z.J. Zheng, and G.D. Jiang. 2014. Interleukin-10 mediates the neuroprotection of hyperbaric oxygen therapy against traumatic brain injury in mice. Neuroscience 266: 235–243.
Zhang, Y., Y. Yang, H. Tang, W. Sun, X. Xiong, D. Smerin, and J. Liu. 2014. Hyperbaric oxygen therapy ameliorates local brain metabolism, brain edema and inflammatory response in a blast-induced traumatic brain injury model in rabbits. Neurochemical Research 39 (5): 950–960.
Meng, X.E., Y. Zhang, N. Li, D.F. Fan, C. Yang, H. Li, D.Z. Guo, and S.Y. Pan. 2016. Hyperbaric oxygen alleviates secondary brain injury after trauma through inhibition of TLR4/NF-κB signaling pathway. Medical Science Monitor 22: 284–288.
Wee, H.Y., S.W. Lim, C.C. Chio, K.C. Niu, C.C. Wang, and J.R. Kuo. 2015. Hyperbaric oxygen effects on neuronal apoptosis associations in a traumatic brain injury rat model. The Journal of Surgical Research 197 (2): 382–389.
Geng, F., Y. Ma, T. Xing, X. Zhuang, J. Zhu, and L. Yao. 2016. Effects of hyperbaric oxygen therapy on inflammasome signaling after traumatic brain injury. Neuroimmunomodulation 23 (2): 122–129.
Lu, Y., B.C. Jiang, D.L. Cao, Z.J. Zhang, X. Zhang, R.R. Ji, and Y.J. Gao. 2014. TRAF6 upregulation in spinal astrocytes maintains neuropathic pain by integrating TNF-α and IL-1β signaling. Pain 155 (12): 2618–2629.
Gao, Y.J., L. Zhang, O.A. Samad, M.R. Suter, K. Yasuhiko, Z.Z. Xu, J.Y. Park, A.L. Lind, Q. Ma, and R.R. Ji. 2009. JNK-induced MCP-1 production in spinal cord astrocytes contributes to central sensitization and neuropathic pain. The Journal of Neuroscience 29 (13): 4096–4108.
Hui, J., Z.J. Zhang, X. Zhang, Y. Shen, and Y.J. Gao. 2013. Repetitive hyperbaric oxygen treatment attenuates complete Freund’s adjuvant-induced pain and reduces glia-mediated neuroinflammation in the spinal cord. The Journal of Pain 14 (7): 747–758.
Berman, J.W., M.P. Guida, J. Warren, J. Amat, and C.F. Brosnan. 1996. Localization of monocyte chemoattractant peptide-1 expression in the central nervous system in experimental autoimmune encephalomyelitis and trauma in the rat. Journal of Immunology 156 (8): 3017–3023.
Merkel, S.F., A.M. Andrews, E.M. Lutton, R. Razmpour, L.A. Cannella, and S.H. Ramirez. 2017. Dexamethasone attenuates the enhanced rewarding effects of cocaine following experimental traumatic brain injury. Cell Transplantation 26 (7): 1178–1192.
Pineau, I., L. Sun, D. Bastien, and S. Lacroix. 2010. Astrocytes initiate inflammation in the injured mouse spinal cord by promoting the entry of neutrophils and inflammatory monocytes in an IL-1 receptor/MyD88-dependent fashion. Brain, Behavior, and Immunity 24 (4): 540–553.
Wu, F., Y. Zhao, T. Jiao, D. Shi, X. Zhu, M. Zhang, M. Shi, and H. Zhou. 2015. CXCR2 is essential for cerebral endothelial activation and leukocyte recruitment during neuroinflammation. Journal of Neuroinflammation 12: 98.
Vargas-Caraveo, A., A. Sayd, S.R. Maus, J.R. Caso, J.L.M. Madrigal, B. García-Bueno, and J.C. Leza. 2017. Lipopolysaccharide enters the rat brain by a lipoprotein-mediated transport mechanism in physiological conditions. Scientific Reports 7 (1): 13113.
Chistyakov, D.V., N.V. Azbukina, A.V. Lopachev, K.N. Kulichenkova, A.A. Astakhova, and M.G. Sergeeva. 2018. Rosiglitazone as a modulator of TLR4 and TLR3 signaling pathways in rat primary neurons and astrocytes. International Journal of Molecular Sciences 19 (1).
Moriyama, M., S. Fujitsuka, K. Kawabe, K. Takano, and Y. Nakamura. 2018. Zinc potentiates lipopolysaccharide-induced nitric oxide production in cultured primary rat astrocytes. Neurochemical Research 43 (2): 363–374.
Liu, H., J.R. Davis, Z.L. Wu, and A. Faez Abdelgawad. 2017. Dexmedetomidine attenuates lipopolysaccharide induced MCP-1 expression in primary astrocyte. BioMed Research International 6352159.
Choi, S.S., H.J. Lee, I. Lim, J. Satoh, and S.U. Kim. 2014. Human astrocytes: Secretome profiles of cytokines and chemokines. PLoS One 9 (4): e92325.
Ma, J., W. Xiao, J. Wang, J. Wu, J. Ren, J. Hou, J. Gu, K. Fan, and B. Yu. 2016. Propofol inhibits NLRP3 inflammasome and attenuates blast-induced traumatic brain injury in rats. Inflammation 39 (6): 2094–2103.
Hellewell, S., B.D. Semple, and M.C. Morganti-Kossmann. 2016. Therapies negating neuroinflammation after brain trauma. Brain Research 1640 (Pt A): 36–56.
Sun, W., J. Liu, Y. Huan, and C. Zhang. 2014. Intracranial injection of recombinant stromal-derived factor-1 alpha (SDF-1α) attenuates traumatic brain injury in rats. Inflammation Research 63 (4): 287–297.
Chu, W., M. Li, F. Li, R. Hu, Z. Chen, J. Lin, and H. Feng. 2013. Immediate splenectomy down-regulates the MAPK-NF-κB signaling pathway in rat brain after severe traumatic brain injury. Journal of Trauma and Acute Care Surgery 74 (6): 1446–1453.
Marshall, J., J. Szmydynger-Chodobska, M.S. Rioult-Pedotti, K. Lau, A.T. Chin, S.K.R. Kotla, R.K. Tiwari, K. Parang, S.W. Threlkeld, and A. Chodobski. 2017. TrkB-enhancer facilitates functional recovery after traumatic brain injury. Scientific Reports 7 (1): 10995.
Baratz-Goldstein, R., S. Toussia-Cohen, A. Elpaz, V. Rubovitch, and C.G. Pick. 2017. Immediate and delayed hyperbaric oxygen therapy as a neuroprotective treatment for traumatic brain injury in mice. Molecular and Cellular Neurosciences 83: 74–82.
Liu, S., Y. Liu, S.K. Deng, A.S. Guo, X.B. Wang, and G.Y. Shen. 2015. Beneficial effects of hyperbaric oxygen on edema in rat hippocampus following traumatic brain injury. Experimental Brain Research 233 (12): 3359–3365.
Yang, Y., H. Wei, X. Zhou, F. Zhang, and C. Wang. 2017. Hyperbaric oxygen promotes neural stem cell proliferation by activating vascular endothelial growth factor/extracellular signal-regulated kinase signaling after traumatic brain injury. Neuroreport 28 (18): 1232–1238.
Funding
This work was funded by the National Natural Science Foundation of China (NSFC 81702223) and the Science and Technology Planning Project of Nantong (MS22016044).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, S., Lu, C., Liu, Y. et al. Hyperbaric Oxygen Alleviates the Inflammatory Response Induced by LPS Through Inhibition of NF-κB/MAPKs-CCL2/CXCL1 Signaling Pathway in Cultured Astrocytes. Inflammation 41, 2003–2011 (2018). https://doi.org/10.1007/s10753-018-0843-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-018-0843-2