Abstract
Macrophage-related inflammatory response is one of the main biological factors resulting in failure of anterior cruciate ligament (ACL) reconstruction, although the specific pathomechanism remains to be clarified. Our aim was to investigate the association between graft loosening and macrophage-related inflammation in cases of loosening of reconstructed ACL autografts. Tissue samples were obtained from 21 patients who underwent a second-look arthroscopy within the first year after arthroscopic ACL reconstruction using single-bundle hamstring tendon autografts. Possible biological factors of graft loosening were analyzed using polymerase chain reaction, Western blot, and hematoxylin/eosin and immunohistochemical staining of graft tissue samples obtained during the second-look arthroscopy. Graft loosening was closely related to increased gene and protein expression of inflammatory cytokines (TNF-α, IL-6, and IL-8) and activation of the inflammation-related toll-like receptor (TLR) signaling (TLR2 and TLR4). The molecular expression of TGF-β and type I and III collagen was also inhibited to varying degrees, with decreased vascularization of the graft due to an inhibition of VEGF. iNOS, a marker of M1 macrophage activation, was highly expressed in cases of graft loosening, with no effect of M2 macrophages identified. The activation of M1 macrophages and aseptic inflammation signaling is an important biological factor of graft loosening after ACL reconstruction, affecting ligamentization and the health of grafts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Rupture of the anterior cruciate ligament (ACL) is one of the most common sport-related orthopedic injuries. Arthroscopic ACL reconstruction (ACLR) is recognized as the treatment of choice, with good-to-excellent outcomes achieved in 75 to 90% of cases. However, the failure rate of ACL reconstruction remains at approximately 9.6% for autograft repairs and 25.0% for allograft repairs [1,2,3]. ACLR failure usually occurs in young and middle-aged adults, typically 18 to 35 years of age, and requires revision surgery to restore knee function and improve patients’ quality of life.
A recent multicenter ACL revision study (MARS) identified traumatic reinjury (32%), technical errors (24%), and a combination of trauma and errors (37%) as the main causes of ACLR failure. The MARS study further identified biological factors as having a probable causative role in ACLR failure in 7% of cases [4]. However, our understanding of the role of biological factors in the mechanism of ACLR failures mainly due to graft loosening is limited. Healing of the ACL graft involves both intra-tunnel and intra-articular graft remodeling, commonly referred to as ‘tendon-bone healing’ and ‘ligamentization’, respectively [5,6,7,8].
Biological factors, and macrophage activity more specifically, can negatively affect tendon-bone healing, resulting in graft loosening and ACLR failure [9]. Moreover, the accumulation of macrophages following tendon-to-bone repair might contribute to the formation of a scar-tissue interface and, therefore, be an important component of biological factors that influence the process of tendon-bone healing [9]. In response to cues in the microenvironment of the ACLR, classically activated macrophages (M1) and alternatively activated macrophages (M2) are phenotypically polarized to perform proinflammatory and immunoregulatory functions, respectively [10, 11]. M1 macrophages promote the Th1 response, as well as microbicidal and tumoricidal activity, while M2 macrophages promote the Th2 response during the phase of tissue remodeling [12,13,14]. This differential proinflammatory and immunoregulatory function of M1 and M2 has been confirmed in tumors and in cases of inflammation and fibrosis [11].
With regard to ACLR grafts, animal studies have provided evidence that accumulation of M1 macrophages might give rise to poor tendon-bone healing. Moreover, Killian et al. identified that mechanical stimulation of the reconstructed ligament influences macrophage accumulation on the graft and is therefore likely to play an important role in tendon-bone healing [15]. However, the interaction between macrophage accumulation and poor tendon-bone healing in graft loosening has not been investigated in detail, including molecular signaling underlying this biological mechanism of ACLR graft healing. Therefore, based on detection results of tissue specimens and follow-up data of our patients undergoing arthroscopic ACLR, the aim of our study was to investigate the association between graft loosening of post-ACLR and macrophage-related inflammation.
MATERIALS AND METHODS
Human Model and Inclusion Criteria
Our study was approved by Sun Yat-sen Memorial Hospital’s Ethics Committee. The study group of interest consisted of patients who underwent a primary ACLR at our hospital using a single-bundle hamstring tendon autograft and requiring a second-look arthroscopy, again at our hospital, for possible graft loosening, within the first year after ACLR. Patients who underwent these procedures between 2012 and 2015 were screened on the following inclusion criteria: (1) isolated arthroscopic ACLR and normal contralateral knee; (2) no repeated injury between the primary ACLR and second-look arthroscopy; and (3) patients’ consent to second-look arthroscopy to remove the U-shaped staples used to fix the graft at the tibial site. Exclusion criteria were additional ligamentous injuries, articular cartilage damage, intercondylar notch impingement, and articular infection. Both the primary ACLR and second-look arthroscopy were performed by one experienced surgeon (W. L.) for all patients included in the analysis, with the same technique and materials used in all cases. The morphology and tension of the graft were confirmed to be normal under arthroscopy for all ACLR cases, with confirmation of negative anterior drawer, pivot shift, and Lachman tests, with respect to the uninvolved contralateral knee, after ACLR. All patients underwent a standardized rehabilitation protocol post-ACLR.
After a 1-year follow-up, patients with a poor tendon-bone healing status were identified based on the ACL failure criteria described by Noyes and Barber-Westin [16]: a complete graft tear, associated with >6 mm of anterior displacement of the tibia compared to healthy the knee, measured using the Kneelax 3 (Monitored Rehab Systems, Haarlem, Netherlands) [17]; a positive pivot shift test of grade + 2 or +3, compared to the healthy knee, with or without knee pain or inflammation; and a subjective sensation of instability or functional limitation in activities of daily life and/or sports, assessed by the Lysholm score [18, 19]. These patients formed our graft loosening group for analysis. Patients with no symptoms or signs of graft loosening and no radiographic evidence of fracture and graft rupture formed our normal graft group (control group) in our analysis. The healing status of all grafts with regard to graft tension, synovial coverage, and bundle condition was ultimately confirmed during the second-look arthroscopy of the 21 patients who required a second-look arthroscopy within the first year post-ACLR. Among these 21 patients, 11 met the failure criteria (graft loosening group) and 10 patients formed the control group for analysis. Relevant demographic data for two groups are summarized in Table 1.
Tissue Collection and Preparation
Approximately 200 mg of graft tissues was collected from the surface of the reconstructed ACL during the second-look arthroscopy using a rongeur. Tissue samples were obtained at the opening of the femoral tunnel, close to the intercondylar fossa. A portion of the tissue sample was rapidly stored in liquid nitrogen or at −80 °C for molecular analysis, with the remaining tissue specimens fixed in 4% paraformaldehyde for histological and immunohistochemical staining.
Hematoxylin/Eosin Staining and Immunohistochemical Staining
Tissue samples fixed in 4% paraformaldehyde were embedded in paraffin and sliced in section of 5 μm thickness using a microtome. A portion of these sections were stained in HE solution, with the other portion incubated with primary antibodies against collagen I, collagen III, toll-like receptor 2 (TLR2), TLR4, IL-8, IL-6, TNF-α, TGF-β1, VEGFA, CD68, CD206, iNOS (Abcam, Cambridge, UK) and then incubated with biotinylated secondary antibody (Bioss, Beijing, China) for immunohistochemistry. All sections were evaluated under light microscopy combined with a CCD camera (Chongqing Optec Instrument Co., Chongqing, China). The immunohistochemical scoring was performed as described previously [20].
Real-Time Polymerase Chain Reaction
Using the tissue samples stored in liquid nitrogen, the total RNA was extracted using a Trizol reagent kit (Life Technologies, USA) and subjected to cDNA synthesis using a TaKaRa PrimeScript™ RT reagent Kit (TaKaRa, Otsu, Japan). Real-time PCR with TaKaRa SYBR® Premix Ex Taq™ II kit (TaKaRa, Otsu, Japan) was performed in a total volume of 20 μL containing 1 μL cDNA, 10 μL SYBR premix EX Taq™ (2×), 0.5 μL forward primer (10 μM), 0.5 μL reverse primer (10 μM), and 8 μL RNAase-free H2O. Gene quantification was analyzed in triplicate using the Bio-Rad CFX96 Real-Time PCR System. The gene primer sequences used for quantitative real-time PCR are summarized in Table 2, with GAPDH used as the reference gene. All analyses were performed according to the manufacturer’s instructions.
Western Blotting Analysis
For protein expression analysis, tissue samples were ground and lysed using a RIPA buffer. An equal amount of protein from tissue extracts were separated on SDS-polyacrylamide gels and transferred onto PVDF membranes (Millipore, MA, USA). The membranes were incubated with blocking solution (5% BSA) for 60 min at room temperature. Samples were then incubated overnight at 4 °C with primary antibodies (Abcam, Cambridge, UK) for collagen I, collagen III, TLR2, TLR4, IL-8, IL-6, TNF-α, TGF-β1, VEGFA, and GAPDH, with subsequent incubation with secondary antibody (goat anti-rabbit IgG (H&L)-HRP; Southern Biotech, Birmingham, AL) applied for 90 min at room temperature. The protein bands of interest were visualized by enhanced chemiluminescence, with the intensity of each band analyzed using the Quantity One software (Bio-Rad Laboratories, Hercules, CA).
Statistical Analysis
The data from each group are presented as the mean ± standard deviation (SD). Between-group differences in inflammation- and tendon-related gene and protein expression were analyzed using Student’s t test. Spearman test was used to evaluate correlations between biological expression and knee function score. Data analysis was performed with SPSS 13.0 software (SPSS Inc., Chicago, USA). A value of P < 0.05 indicated statistical significance between groups.
RESULTS
Gross Appearance of Reconstructed ACL Grafts Under Second-Look Arthroscopy
On visual inspection, the grafts from the control group showed good survival, with the surface of the graft covered by a peripheral vessel-rich synovial sheath, with an appropriate anatomical position and good continuity and vascularization (Fig. 1a, b). However, in the graft loosening group, the graft appeared pale and coarse, with absence of vascularization and poor continuity (Fig. 1c, d). Importantly, between-group differences in graft laxity were further confirmed by the anterior drawer test performed under arthroscopy, with the detected laxity being consistent with physical examination and knee function scores.
Histological Observation of Reconstructed ACL Grafts Under Light Microscope
At low magnification (100×), alignment of collagen fibers and few inflammatory cells were shown in graft tissues from the control group. However, in the graft loosening group, significant infiltration of macrophages was identified in collagen-lacking graft tissue (Fig. 2). The disorganized tissue structure and macrophage infiltration in patients who had experienced loosening of the graft (graft loosening group) were evident on high magnification (200×).
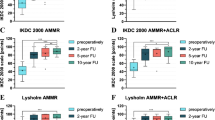
Between-Group Differences in Target Protein Expression in Tendon Tissue Samples
In order to further clarify the potential influence and relationship of inflammatory reaction on graft tissue samples obtained from patients in graft loosening group and on their clinical outcomes, immunohistochemistry analysis was performed. Results indicated an increased expression of TNF-α, IL-6, IL-8, TLR2, and TLR4, as well as a substantive infiltration of macrophages, identified using CD68 labeling (Fig. 3). In contrast, a decreased expression of TGF-β, VEGFA, collagen I, and collagen III, to varying extent, was identified in these tissues (Fig. 3). Importantly, the expression of iNOS, one of the key indicators of activated M1 macrophages, was significantly increased in tendon tissue samples obtained from graft loosening group compared to sampled obtained from the control group. However, the expression of CD206, one of the key markers of M2 macrophage activation, was comparable between the two groups (Fig. 3). Further, quantitative results of the above-mentioned immunohistochemical staining demonstrated that the differences of between-groups were all significant statistically (Fig. 4, P < 0.01). Collectively, these results confirmed the activation of inflammatory cells in tendon tissue samples obtained from failed ACLR cases. Moreover, our analysis further identified a probable role of M1 cells in the pathological inflammatory process resulting in ACLR failure.
Between-Group Differences in Inflammation- and Tendon-Related Gene Expression
The relative increase in inflammation-related gene expression, including TNF-α, IL-6, and IL-8, in tissue samples from the graft loosening group, compared to the control group, is shown in Fig. 5a (P < 0.01). Gene expression for TLR2 and TLR4 was also increased in the graft loosening group compared to the control group (P < 0.01; Fig. 5a). As expected, this increase in inflammation-related gene expression was associated with inhibition in the expression of VEGF and tendon-related genes in the graft loosening group, compared to the control group (P < 0.01; Fig. 5b). Moreover, Kneelax function scores had a significant negative correlation with the gene expression of inflammatory cytokines and TLRs and a significant positive correlation with tendon-related and VEGF gene expression (P < 0.05; Table 3).
Between-group differences in mRNA expression levels normalized against the normal graft group as 1.0. a The between-group fold-difference in gene expression levels of inflammatory cytokines (TNF-α, IL-6, and IL-8) and related signaling receptors (TLR-2 and TLR-4). b The between-group fold-difference in gene expression levels of collagen I, collagen III, VEGF, and TGF-β1. **P < 0.01 between groups.
Between-Group Differences in Inflammation- and Tendon-Related Protein Expression
Overexpression of inflammatory proteins was also identified by Western blotting, including TNF-α, IL-6, IL-8, TLR2, and TLR4 proteins. This overexpression was associated with an inhibition in the expression of VEGF and tendon-related proteins (Fig. 6a). Gray intensity analysis of protein bands confirmed the significance of these between-group differences in protein expression (P < 0.01; Fig. 6b, c). Likewise, a negative significant correlation between knee function scores and the gene expression of inflammatory cytokines and TLRs was identified, with scores being positively correlated to tendon-related and VEGF gene expression (P < 0.05; Table 4).
DISCUSSION
ACLR, using tendon autografts or allografts, is the most effective treatment for ACL rupture. However, loosening of the graft caused by poor tendon-bone healing is a significant concern, resulting in ACLR failure and the need for revision surgery. Several studies have purported biological factors to play an important role in ACLR failure, with evidence of a significant association between increased inflammation and an increased aggregation of macrophages on the graft, based on second-look arthroscopy and tendon tissue biopsy analysis. However, remarkably, surgical technique and biomechanical environment equally play pivotal roles in ACLR failure. The altered biomechanical environment, such as graft-tunnel micromotion, stress deprivation etc., can also affect the biologic events in the grafts [21, 22]. Although these abiotic factors are hard to avoid with ACLR, individual differences of the biomechanical environment and surgical technique were controlled to the greatest extent possible in our study, with all repairs performed using the same surgical procedure by a single experienced doctor.
To date, a universally applied gold standard for the diagnosis of ACLR failure has not been provided. Barrett et al. defined ACLR failure as an absence of an end-point on the Lachman test, combined with a positive pivot shift and a >5-mm side-to-side difference in anterior tibial translation measured using a KT-1000 arthrometer [23]. Kamath et al. further included subjective sensation of recurrent knee instability in their definition of ACLR failure [24]. In our study, we defined ACLR failure based on the criteria of Noyes and Barber-Westin [16], which combines both objective and subjective measures. Specifically, we subclassified our patients for analysis based on presence of anterior translation of the tibia, measured using pivot shift test, Kneelax and Lysholm score, self-reported sensation of knee joint laxity and knee-related limitations in activities and participation. This combination of objective and subjective measures provided us with relatively specific and comprehensive criteria of ACLR failure.
Poor graft healing has been considered as a principal cause of non-traumatic ACLR failure. Graft healing is a slow biological process that includes both graft remodeling, with intra-tunnel tendon-bone incorporation, and intra-articular graft ligamentization. The effects of biological factors, especially inflammation, on tendon-bone healing have been at the forefront of research on ACLR failure in recent years, with possible benefits of controlling inflammation, through transformed growth factor-beta (TGF-β), mesenchymal stem cells, osteogenic factors, and other modalities reducing local inflammation, having been proposed to promote graft healing post-ACLR [25].
Once macrophages recruited from circulating blood monocytes are activated, they release pro-inflammatory cytokines, such as TNF-α and IL-1, 6, and 8, which initiates an inflammatory response that disrupts formation of a normal tendon-bone structure. Moreover, the accumulation of these cytokines around a graft has been associated with dysfunction of collagen formation, as well as denaturation and poor revascularization of grafts. In our study, we used four indices of ligament remodeling, maturation, and formation after ACLR, namely COL3A1, COL1A1 VEGF, and TGF-β1, to explore the role of biological responses on tendon-tissue mRNA and protein expression in situ. As we had expected a priori, we identified a significant decrease in the expression of collagen I and III in tendon tissue samples obtained from ACLR failure cases, with an associated increase in mRNA and protein expression of TNF-α and ILs. In addition, the TLR 2 and 4 signaling pathways, which are related to the activation of macrophages and facilitation of inflammatory events, were invoked. Thus, our findings provide evidence of an association between poor graft health and an enhanced inflammatory and macrophage response. For these reasons, the expression level of VEGF, a reliable biomarker of tissue healing, was inhibited, a finding which was consistent with Yoshikawa et al. report [26]. The decrease in VEGF expression could impair revascularization of the graft, reducing oxygen supply to cells, limiting the production of growth factors, and inhibiting cell proliferation which, ultimately, would disrupt ligamentization and tissue viability of the graft. Moreover, evidence of a benefit of exogenously applied TGF-β to enhance tissue healing, extracellular matrix synthesis, and remodeling of grafts has previously been reported [27,28,29]. Likewise, the expression of TGF-β was significantly downregulated among patients who experienced a loosening of their ACL graft loosening. Remarkably, the statistical correlation between all above-mentioned biological factors and knee function scores was significant. Therefore, we initially speculated that graft loosening resulted from poor graft viability related to the inflammatory microenvironment around the graft, involving cytokines and macrophages.
As we have known, macrophages are indispensable cells in the process of inflammation and immune defense. In fact, according to their specific roles, polarized macrophages are broadly divided into two main types, classically activated M1 macrophages, and alternatively activated M2 macrophages. It is universally accepted that polarization of M1 macrophages is related to tissue destruction and inflammation, while M2 macrophages are active in angiogenesis, anti-inflammation, and wound repair [30, 31]. Moreover, inflammatory stimuli, such as LPS and IFN γ, can activate M1 macrophages, while M2 polarized macrophages have opposite functions, such as clearing inflammation and reducing secretion of proinflammatory cytokines [32, 33]. Thus, activation of macrophages can lead either to tissue degeneration and destruction, or to tissue regeneration and wound healing. In this study, a significant correlation between macrophages and aseptic inflammation of grafts in patients has been confirmed. More importantly, regarding the role of macrophages in patients who experienced a loosening of the graft after ACLR surgery, we identified a probable role of M1 but not M2 macrophages in the pathological process leading to graft loosening by using immunohistochemical staining with antibodies of macrophage-specific CD68, M2 macrophage-specific CD206, and M1 macrophage-specific iNOS. However, considering the limitations of our small study group and the bias of single center studies, future studies are needed to confirm our results. Moreover, in fact, there is no way to know whether the histologic changes described in this study are cause or effect, because it is also possible that macrophage accumulation occurs subsequent to the failure of the graft, as a result of certain factors such as the altered mechanical environment due to recurrent knee instability. Thus, our further research is required to identify possible biological or mechanical factors related to the surgery and to patients, which could trigger the activation of M1 macrophages in graft tissues, as well as to clearly define the inflammation-related signaling pathways. Ultimately, our aim is to identify effective prevention strategies to prevent loosening of the graft after ACLR.
CONCLUSIONS
Combining histological and molecular analyses, we identified a clear correlation between inflammation, M1 macrophage infiltration, and poor graft tissue viability. TLR-2/4 expressed on the surface of macrophages might regulate the local microenvironment that results in poor tendon-bone healing. These findings could help us to better understand biological factors of graft loosening and provide a reference for potential targets of prevention and treatment.
Change history
15 August 2017
An erratum to this article has been published.
References
George, M.S., W.R. Dunn, and K.P. Spindler. 2006. Current concepts review: Revision anterior cruciate ligament reconstruction. The American Journal of Sports Medicine 34: 2026–2037.
Yamamoto, Y., W.H. Hsu, S.L. Woo, A.H. Van Scyoc, Y. Takakura, and R.E. Debski. 2004. Knee stability and graft function after anterior cruciate ligament reconstruction: A comparison of a lateral and an anatomical femoral tunnel placement. The American Journal of Sports Medicine 32: 1825–1832.
Wasserstein, D., U. Sheth, A. Cabrera, and K.P. Spindler. 2015. A systematic review of failed anterior cruciate ligament reconstruction with autograft compared with allograft in young patients. Sports Health 7: 207–216.
Group M, R.W. Wright, L.J. Huston, K.P. Spindler, W.R. Dunn, A.K. Haas, et al. 2010. Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. The American Journal of Sports Medicine 38: 1979–1986.
Claes, S., P. Verdonk, R. Forsyth, and J. Bellemans. 2011. The “Ligamentization” process in anterior cruciate ligament reconstruction what happens to the Human graft? A systematic review of the literature. The American Journal of Sports Medicine 39: 2476–2483.
Janssen, R.P., and S.U. Scheffler. 2014. Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 22: 2102–2108.
Pauzenberger, L., S. Syre, and M. Schurz. 2013. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: A systematic review of the literature and a glimpse into the future. Arthroscopy 29: 1712–1721.
Scheffler, S.U., F.N. Unterhauser, and A. Weiler. 2008. Graft remodeling and ligamentization after cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 16: 834–842.
Hays, P.L., S. Kawamura, X.H. Deng, E. Dagher, K. Mithoefer, L. Ying, et al. 2008. The role of macrophages in early healing of a tendon graft in a bone tunnel. The Journal of Bone and Joint Surgery. American 90: 565–579.
Martinez, F.O., A. Sica, A. Mantovani, and M. Locati. 2008. Macrophage activation and polarization. Frontiers in Bioscience 13: 453–461.
Sica, A., and A. Mantovani. 2012. Macrophage plasticity and polarization: In vivo veritas. The Journal of Clinical Investigation 122: 787–795.
Biswas, S.K., and A. Mantovani. 2010. Macrophage plasticity and interaction with lymphocyte subsets: Cancer as a paradigm. Nature Immunology 11: 889–896.
Gordon, S., and F.O. Martinez. 2010. Alternative activation of macrophages: Mechanism and functions. Immunity 32: 593–604.
Sica, A., and V. Bronte. 2007. Altered macrophage differentiation and immune dysfunction in tumor development. The Journal of Clinical Investigation 117: 1155–1166.
Killian, M.L., L. Cavinatto, L.M. Galatz, and S. Thomopoulos. 2012. The role of mechanobiology in tendon healing. Journal of Shoulder and Elbow Surgery 21: 228–237.
Noyes, F.R., and S.D. Barber-Westin. 2001. Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. The Journal of Bone and Joint Surgery. American 83: 1131–1143.
Paine, R., and W. Lowe. 2012. Comparison of Kneelax and KT-1000 knee ligament arthrometers. The Journal of Knee Surgery 25: 151–154.
Briggs, K.K., J. Lysholm, Y. Tegner, W.G. Rodkey, M.S. Kocher, and J.R. Steadman. 2009. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. The American Journal of Sports Medicine 37: 890–897.
Lysholm, J., and J. Gillquist. 1982. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. The American Journal of Sports Medicine 10: 150–154.
Zhu, H., X. Zhou, S. Redfield, J. Lewin, and L. Miele. 2013. Elevated jagged-1 and notch-1 expression in high grade and metastatic prostate cancers. American Journal of Translational Research 5: 368–378.
Lui, P., P. Zhang, K. Chan, and L. Qin. 2010. Biology and augmentation of tendon-bone insertion repair. Journal of Orthopaedic Surgery and Research 5: 59.
Lavagnino, M., and S.P. Arnoczky. 2005. In vitro alterations in cytoskeletal tensional homeostasis control gene expression in tendon cells. Journal of Orthopaedic Research 23: 1211–1218.
Barrett, A.M., J.A. Craft, W.H. Replogle, J.M. Hydrick, and G.R. Barrett. 2011. Anterior cruciate ligament graft failure: A comparison of graft type based on age and Tegner activity level. The American Journal of Sports Medicine 39: 2194–2198.
Kamath, G.V., J.C. Redfern, P.E. Greis, and R.T. Burks. 2011. Revision anterior cruciate ligament reconstruction. The American Journal of Sports Medicine 39: 199–217.
Fu, S.C., Y.C. Cheuk, S.H. Yung, C.G. Rolf, and K.M. Chan. 2014. Systematic review of biological modulation of healing in anterior cruciate ligament reconstruction. Orthopaedic Journal of Sports Medicine 2: 2325967114526687.
Yoshikawa, T., H. Tohyama, H. Enomoto, H. Matsumoto, Y. Toyama, and K. Yasuda. 2006. Expression of vascular endothelial growth factor and angiogenesis in patellar tendon grafts in the early phase after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 14: 804–810.
Ignotz, R.A., and J. Massague. 1986. Transforming growth factor-beta stimulates the expression of fibronectin and collagen and their incorporation into the extracellular matrix. Journal of Biological Chemistry 261: 4337–4345.
Sumner, D.R., T.M. Turner, A.F. Purchio, W.R. Gombotz, R.M. Urban, and J.O. Galante. 1995. Enhancement of bone ingrowth by transforming growth factor-beta. The Journal of Bone and Joint Surgery. American 77: 1135–1147.
Yamazaki, S., K. Yasuda, F. Tomita, H. Tohyama, and A. Minami. 2005. The effect of transforming growth factor-beta1 on intraosseous healing of flexor tendon autograft replacement of anterior cruciate ligament in dogs. Arthroscopy 21: 1034–1041.
Magatti, M., E. Vertua, S. De Munari, M. Caro, M. Caruso, A. Silini, et al. 2016. Human amnion favours tissue repair by inducing the M1-to-M2 switch and enhancing M2 macrophage features. Journal of Tissue Engineering and Regenerative Medicine. doi:10.1002/term.2193.
Mosser, D.M., and J.P. Edwards. 2008. Exploring the full spectrum of macrophage activation. Nature Reviews. Immunology 8: 958–969.
Lawrence, T., and G. Natoli. 2011. Transcriptional regulation of macrophage polarization: Enabling diversity with identity. Nature Reviews. Immunology 11: 750–761.
Murray, P.J., and T.A. Wynn. 2011. Protective and pathogenic functions of macrophage subsets. Nature Reviews. Immunology 11: 723–737.
Acknowledgements
The study was financially supported by Higher Education Foundation of Sun Yat-sen University (81000-31911101) and Public Research and Capacity Building Special Fund Project of Guangdong Province (2014A020212431, 2014A020212722, 2016A020215065).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
All procedures performed in this study involving human tissues were in compliance with the ethical standards of Sun Yat-sen Memorial Hospital's Ethics Committee, and with the 1964 Helsinki declaration and its later amendments.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Additional information
The original version of this article was revised: The first author’s name in the original version of this article was wrong; Bing Song should be changed to Bin Song. With this, the original version was corrected and the correct name is now presented above.
Bin Song and Chuan Jiang contributed equally to this work.
An erratum to this article is available at https://doi.org/10.1007/s10753-017-0651-0.
Rights and permissions
About this article
Cite this article
Song, B., Jiang, C., Luo, H. et al. Macrophage M1 Plays a Positive Role in Aseptic Inflammation-Related Graft Loosening After Anterior Cruciate Ligament Reconstruction Surgery. Inflammation 40, 1815–1824 (2017). https://doi.org/10.1007/s10753-017-0616-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-017-0616-3