Abstract
Protease-activated receptors (PARs) are G protein-coupled receptors of which four members PAR1, PAR2, PAR3, and PAR4 have been identified, characterized by a typical mechanism of activation involving various related proteases. The amino-terminal sequence of PARs is cleaved by a broad array of proteases, leading to specific proteolytic cleavage which forms endogenous tethered ligands to induce agonist-biased PAR activation. The biological effect of PARs activated by coagulation proteases to regulate hemostasis and thrombosis plays an enormous role in the cardiovascular system, while PAR4 can also be activated by trypsin, cathepsin G, the activated factor X of the coagulation cascade, and trypsin IV. Irrespective of its role in thrombin-induced platelet aggregation, PAR4 activation is believed to be involved in inflammatory lesions, as show by investigations that have unmasked the effects of PAR4 on neutrophil recruitment, the regulation of edema, and plasma extravasation. This review summarizes the roles of PAR4 in coagulation and other extracellular protease pathways, which activate PAR4 to participate in normal regulation and disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The protease-activated receptors (PARs) belong to a developing family of four transmembrane G protein-coupled receptors (GCPR) activated by a unique mode, underlined by the proteolytic cleavage of their extracellular N-terminal domain. After the interaction with various proteases, this cleavage site releases a new N-terminal domain that acts as a tethered ligand to induce an intracellular signal by linking the receptor itself to its second extracellular loop [1–5]. Four members of the PARs family, PAR1, PAR3, and PAR4, have been cloned [3, 6, 7] as thrombin receptors, since they have been shown to be responsible for thrombin-induced platelet activation. PAR1, 3, and 4 were initially recognized as receptors for the coagulation protease and are involved in thrombin signaling, mainly as a heterodimer [8–11]. In addition, PAR1 activation is induced by other coagulation proteases [12, 13], matrix metalloproteinase 1 [14], and microbial proteases [15]. PAR2 is activated by a series of extracellular proteases including coagulation factors, trypsin, tryptase, tissue kallikreins, and transmembrane serine proteases at epithelial interfaces and in the cardiovascular and immune system. So far, four PARs have been perceived in multiple cells affiliated in the inflammatory reaction such as macrophages, neutrophils, and mast cells [16].
As the last identified member of the PARs family, PAR4 generates physiological functions in the presence of thrombin, trypsin, and cathepsin G [17]. Moreover, PAR4 activation has been discovered in a variety of cells including endothelial cells, neutrophils, and sensory neurons [18, 19], as well as in mouse knee joints [20]. As previously reported, except for platelet activation and relaxation of esophageal smooth muscle, PAR4 is functionally active in the human lung, pancreas, heart, thyroid, small intestine, uterus, prostate, testicles, lymph nodes, the nervous system, and so on [21–23]. Currently, a proinflammatory role for PAR4 was studied when researchers found that PAR4 agonists could cause leukocyte rolling and adherence, full granulocyte recruitment, and edema [19, 23–25]. For example, the selective PAR4 agonist AYPGKF-NH2 induces edema and enhanced blood flow, which result in leukocyte rolling and adhesion [19, 20, 24, 25], suggesting a proinflammatory character for this receptor [19, 24]. Russell et al. [26] proved that PAR4 is intricately connected to the B2 receptor regarding both its inflammatory and nociceptive roles. This review will focus on the role of PAR4 as a potent signaling mediator in inflammation.
PAR4-MEDIATED SIGNAL TRANSDUCTION
Platelet aggregation via PAR4-induced G protein signaling
G protein-coupled signaling is induced by the tethered ligand of PAR4 on the basis of effective collaboration with other factors, taking the effect of mediation of thrombin in platelets as an example. PAR4 is activated by higher concentrations of thrombin compared with PAR1 [27, 28], and PAR4 signaling has distinctive pathways for platelet activation [29–31]. Unlike PAR1 signaling, PAR4 does not need to be phosphorylated on key serine residues and internalizes slowly in comparison, resulting in prolonged degradation of the receptor [9, 32, 33]. Research in the field has indicated that PAR4, a receptor mediator with low affinity that is involved in thrombin signaling at high concentrations, has been shown to signal through at least two G protein signaling pathways (Gα12 and Gαq) [34]. Similar to thromboxane A2, PAR4 and PAR1 can cause the release of ADP, which could trigger Gi pathways through initiation of the P2Y12 receptor [1, 9, 35, 36]. However, Kim et al. [37, 38] affirmed that platelet aggregation-mediating PAR4 does not depend on Gi stimulation; indeed, the physiological function of the Gi pathway is accomplished by secondary release of ADP, which works for the Gi-coupled ADP receptor, P2Y12 [37–39]. It is noteworthy that the platelet aggregation mediated by PARs has remained from unclear mechanisms relating to Gq signaling alone or coactivation of an elusive G protein-coupled pathway apart from Gq signaling. As already reported, PAR4 is not a high-affinity thrombin receptor [27, 28, 40]. The function of PAR4 can only be initiated with the help of PAR1 in environments where thrombin is low. On the contrary, PAR4 is adequate for the mediation of platelet aggregation when the concentration of thrombin is high enough. As a matter of fact, two independent studies have shown that PAR4 signaling is connected with PAR3. The inositol phosphate (IP) accumulation in response to thrombin was increased by about 1.7-fold in COS7 cells which expressed mouse PAR4 alone compared with COS7 cells which expressed mouse PAR4 as well as PAR3 [10]. Moreover, Mao et al. [41] revealed that PAR3 knockout (PAR3−/−) mouse platelets had enhanced intracellular Ca2+ mobilization and platelet activation in response to plasmin in comparison with wild-type platelets [41]. These investigations indicate that PAR3 can affect PAR4 signaling more than heightening PAR4 activation. The consensus finding is that PAR3 adversely regulates PAR4-mediated Gq signaling via the down-regulation of Ca2+ mobilization instead of influencing the downstream signaling of the G12/13 pathway [42].
PAR4 β-arrestin signaling
β-arrestins are a group of cytoplasmic proteins that were initially characterized due to their role of associating with agonist-activated G protein-coupled receptors (GPCRs) [43], inducing their internalization and desensitization [44]. Current research suggests that β-arrestins play excess roles in GPCR signaling, by acting as scaffolds for signaling complex recruitment to the receptor, and can lead to enhanced activation of G protein-coupled pathways [43, 45]. One of the arrestin-mediated pathways is the PI3K-induced activation of the Ser-Thr kinase, Akt [46, 47]. As the data display, arrestins have been considered to have a vital role localizing PI3K to GPCR complexes by collaborating with Src family kinases (SFKs) in fibroblasts, colorectal cells, and gastric carcinoma cells [48–50]. Thrombin-induced Akt phosphorylation associated with the activation of Gi as well as Gq-/Gi-dependent signaling to Akt requires RAS activation, whereas Gq-dependent Akt activation requires arrestin-2 [51]. In platelets, thrombin-mediated Akt phosphorylation trends to decrease by about 90 % when exposed to inhibitors for the Gi-coupled ADP receptor, P2Y12, and is prevented completely by inhibitors of PKC [37, 52].
Akt activation by thrombin is completely reliant on the PKC-induced release of ADP. However, the level of Akt phosphorylation induced by ADP is low. That is to say, the activation of P2Y12 is required, but not sufficient, for maximal Akt stimulation by PAR4 agonists or thrombin. Compared with the effect of specific G protein-subunits on thrombin with ADP-inducted signal pathway in mouse platelets, it can be seen that Gi2 is required solely for ADP signaling, while Gq is necessary for thrombin or ADP to induce Akt phosphorylation, specifically. The above facts suggest that there are some factors, not just ADP alone, that induce a secondary role of PAR4 stimulation. Moreover, new research has shown that PAR4 is involved in inducing Akt phosphorylation in platelets with P2Y12 knock-out [53]. To sum up, these studies manifest that the activation process of Akt stimulated by thrombin receptors versus P2Y12 is diverse, but synergistic to some degree. Besides, Akt phosphorylation partly relies on arrestin-2 in the formation of complexes with PI3Ks [51]. PAR4 agonist-induced Akt phosphorylation is arrestin-2-dependent, whereas Akt phosphorylation stimulated by ADP is not. Similarly, PAR4 agonist-induced fibrinogen binding is also arrestin-dependent, while fibrinogen binding induced by ADP is not. The involvement of arrestin-2 in platelet aggregation by PAR4 has been investigated by arrestin-2 knock-out mice, which have a mild defect in thrombus formation, suggesting that arrestin-2 might contribute to platelet function in vivo [54].
THE MAIN FACTORS CONNECTED WITH PAR4 PARTICIPATING IN INFLAMMATION
Tissue Factor
Tissue factor (TF) is a transmembrane glycoprotein that combines with the serine protease activated factor VII (FVIIa) to start the coagulation pathway. Two major forms of TF may exist: cell-bound form and the plasma or soluble form. The cell-bound form has been thought to take part in most of the known biological processes, but it is noteworthy that soluble forms of TF may participate in coagulation or hemostasis [55] and tissue inflammation [56]. Soluble tissue factor (sTF), when injected into mouse joints, is considered to cause inflammatory arthritis [57, 58]. In one regard, inflammatory response stimulates the coagulation cascade and is often seen as a prethrombotic state, but, on the contrary, coagulation can also start and perpetuate the inflammatory response. The factors related to the above phenomenon include TF, fibrin, thrombin, and PARs. TF-induced coagulation is attributed to fibrin formation and also evokes inflammatory responses through the activation of downstream coagulation proteases such as thrombin and FVIIa on PAR4. A recent study showed that injecting recombinant murine sTF into the mouse footpad leads to footpad swelling and an acute inflammatory response of extravascular tissues. This action is mainly regulated by the well-known pathway of coagulation activation, through thrombin and fibrin formation, as inflammatory responses were effectually attenuated by regulation of the thrombin inhibitor hirudin and an FVIIa inhibitor. The depletion of fibrinogen also blocked inflammatory responses in this model. Busso et al. [59] testified that fibrin formation was necessary to link coagulation and inflammatory responses. To verify whether PAR4 activation could also exert its effect, the mice that were deficient for the individual PARs and only PAR4-deficient mice were tested, which showed that these mice were entirely protected from sTF-induced inflammatory responses [59]. This is in contrast with glomerulonephritis and arthritis, which require an immune stimulus, where the activation of PAR1 and PAR2 seems to play a role [60, 61].
Bradykinin B2 Receptor
Bradykinin is a major inflammatory peptide that is formed at sites of injury and is known to activate sensory nociceptors, inducing a sensation of pain [62]. The inflammatory effects of activated PAR4 rely on the kallikrein-kinin system, which is based on the fact that AYPGKF-NH2-initiated edema could be abrogated by regulation of the bradykinin B2 receptor antagonist, HOE140 [20, 25]. Russell et al. [26] demonstrated that PAR4 is intricately linked to the B2 receptor with regard to both its inflammatory and nociceptive effects. The mechanisms of action of PAR4 in triggering joint inflammatory response and pain appear to be involved with the kallikrein-kinin system. The bradykinin antagonist HOE140 blocked edema, hyperemia, and painful responses to AYPGKF-NH2, which was consistent with the results of a previous research suggesting that PAR4-regulated edema could be blocked by pretreatment with a bradykinin B2 antagonist [25]. PAR4 is present on the surface of leukocytes, endothelial cells, and vascular smooth muscle cells [19], which are stimulated by PAR4-activating peptides to release kallikreins. The kallikreins released then cleave kininogens to generate active kinins, which eventually link to bradykinin receptors, leading to vasodilatation and enhanced vascular permeability. Actually, bradykinin is known to be vasoactive in knee joints, in which it leads to synovial vasodilatation and protein extravasation [63–65]. The effect of the kallikrein-kinin system on enhancing joint pain is also verified by other researches showing that bradykinin evokes peripheral sensitization of knee joint afferent nerves, resulting in increased pain sensation [66, 67]. Other PARs such as PAR1 and PAR2 cause painful and inflammatory responses by inducing the secondary release of proinflammatory neuropeptides from sensory neurons and by stimulating connective tissue mast cells [68–71]. On the contrary, however, the inflammatory response of PAR4 is not neurogenically driven and does not involve mast cell degranulation [24].
ERK/MAPK
PAR4-AP evokes the overexpression of CGRP via activation of the ERK1/2 signaling pathway, and PAR4 activation notably enhances the levels of CGRP messenger RNA (mRNA) and protein in DRG neurons in the presence of AYPGKF-NH2 both in vivo and in vitro [72]. Remarkably, this overexpression is significantly attenuated after inhibiting ERK1/2 phosphorylation. The activation of PAR4 is involved in the administration of CGRP expression in primary sensory neurons via activation of the ERK1/2 signaling pathway. In addition, the activation of PAR4 increases the number of CGRP, PAR4, or p-ERK1/2 immunopositive neurons in DRGs in the presence of AYPGKF-NH2 both in vivo and in vitro, characterized by small- and medium-sized painful neuronal cells [18, 73].
A previous research showed that harmful stimulation enhanced the level of p-ERK1/2 expression simultaneously in the cytoplasm and nucleus of DRG neurons [74]. PAR4 activation increases p-ERK1/2 staining in the cytoplasm and nuclei of DRG neurons with AYPGKF-NH2 treatment. The enhanced p-ERK1/2 staining in cytoplasm and nuclei represents cellular redistribution of p-ERK1/2 in DRG neurons after the activation of PAR4. However, nuclear translocation of ERK1/2 and an increase of p-ERK1/2 in the nucleus lead to numerous cell effects involving proliferation and gene transcription [75, 76]. Therefore, it is possible that the translocation of p-ERK1/2 to the nucleus induced by active PAR4 has a close relationship to CGRP gene transcription in DRG neurons [77, 78]. It is a closely relevant between the up-expression of cytoplasmic p-ERK1/2 in DRG neurons and harmful stimulation [74, 79].
Membrane depolarization and Ca2+ influx induced by harmful stimulation would result in ERK1/2 activation [80]. After phosphorylation, p-ERK1/2 is quickly localized from the cytosol into the nucleus, in which it phosphorylates variety of substrates, e.g., transcription factors [81–83]. The redistribution above is considered to be essential for the effective phosphorylation of transcription factors to mediate levels of mRNA [75, 76]. A rapid and continuing activation of ERK1/2 induced by PAR4 evokes activation of the transcriptional regulation factor cAMP-response element binding protein (CREB) which in turn causes gene expression [84–86]. Activation of p-ERK1/2 also induces CREB-initiated transcription and overexpression of CGRP mRNA in DRG neurons [77, 78]. It is connective between the activation of ERK and the expression of CGRP in sensory neurons [79, 87]. Harmful stimulation causes the rapid phosphorylation of ERK in sensory neurons that conduces to the facilitation of pain sensations and is often used as an instant marker for the excitation of spinal neurons. An intense harmful peripheral or C-fiber electrical stimulation triggers many p-ERK-positive neurons [88]. A recent study showed that harmful stimulation of the rat hind paw could evoke p-ERK1/2 activation in the cytoplasm and nucleus in L3–L5 DRG cells according to the time order exposed to stimulation [74], suggesting an immediate translocation of ERK1/2 from the cytoplasm to the nucleus. All of these data indicate that enhanced levels of p-ERK1/2 occur in advance of the increased expression of CGRP.
Accordingly, it is possible that PAR4 leads to activation of the ERK1/2 pathway which connects activation of the transcriptional regulation factor CREB to the production of CGRP. Depending on the activation of PAR4, p-ERK1/2 may be involved in the overexpression of CGRP mRNA through CREB-dependent transcription. Overexpression of CGRP mRNA and protein levels after AYPGKF-NH2 treatment in DRG neurons offers a molecular mechanism for PAR4 in painful and inflammatory responses. PAR4 activation can notably improve the levels of CGRP mRNA and protein in DRG neurons. The function of active PAR4 on CGRP expression seems to be mediated by the p-ERK signaling pathway.
PAR4 IN NOCICEPTION AND PAIN PATHWAYS
Nociception, mediated by sensory receptors on afferent neurons, is the neuronal sensation, transmission, and central procession of noxious stimulation. Usually, more sensitive nociceptors and enhanced pain sensation are expressed in inflammation. PAR4 protein and mRNA are commonly observed in small nociceptive dorsal root ganglion (DRG) neurons, the majority of which are peptidergic and are marked by substance P and calcitonin gene-related peptide (CGRP) [73, 89]. Furthermore, increasing experimental results prove that activated nociception and inflammation induce a rapid increase in protein and mRNA expression of CGRP in DRG neurons [90–92]. The expression of CGRP in DRG neurons plays a vital role in regulating neurogenic inflammation and pain [72, 93]. PAR4 has been recognized to be up-regulated in DRG neurons during nociceptor activation and inflammation pain [94, 95]. The PAR4 agonist does not evoke a Ca2+ signal in DRG neurons, but reduces the Ca2+ signal of DRG neurons, meaning that activated PAR4 can attenuate the nociceptive pathway in DRG neurons. Previous studies have suggested that, unlike PAR1 and PAR2, edema induced by PAR4 is not reliant on a neurogenic signal relating to capsaicin-sensitive neurons [24], but is reliant on the kallikrein-kinin system activation [23, 25]. Asfaha et al. [18] identified a novel mechanism for the regulation of pain transduction, which demonstrated that PAR4 had an inhibitory role on pain and nociception. The finding that PAR4 exists in sensory neurons and that KCl-induced calcium mobilization in those neurons can be inhibited by a PAR4 agonist means that the activation of PAR4 has a direct effect on sensory nerves by inhibiting the transmission of nociceptive signal. The fact that PAR4 agonists directly activate DRG neurons mediates ascending nociceptive transduction, which is similar to that of opioid receptors, leading to abrogating nociception in DRG neurons.
Previous research has shown that injecting thrombin results in an analgesic effect under the condition of a mechanical stimulus, but hyperalgesia responds to a thermal stimulus, while selective PAR1 activation leading to analgesia under the action of both mechanical and thermal stimulus [96]. Similarly, the injection of a PAR4 agonist evokes analgesia in rat paw in the presence of both stimuli. With regard to the hyperpathia of thrombin in response to thermal stimulus, thrombin might work through a receptor different to PAR1 or PAR4, and/or might come into effect independently of its catalytic site [97–99]. In the joint, the activation of PAR4 on non-neuronal cells causes the release of tissue kallikreins secreted by multiple cell types [100]. This, in turn, results in the production of bradykinin, which can then enhance the sensitivity of knee joint primary afferents. The mechanism of action of PAR4 in triggering joint inflammatory reaction and pain appears to include the kallikrein-kinin system, as the bradykinin antagonist HOE140 weakens edema, hyperemia, and painful responses to AYPGKF-NH2 [20]. A previous finding that PAR4-dependent paw edema could be attenuated by pretreatment with a bradykinin B2 antagonist also manifested the similar conclusion [25]. Auge et al. [101] proved that PAR4 has an effect on the termination of primary afferent nerves in the mouse colon, suggesting that PAR4 activation had a direct effect on these afferent nerves.
PAR4 SIGNALING IN THE GASTROINTESTINAL INFLAMMATION
It has been confirmed that PAR4 participates in modulation of the motility of rat duodenum [102] or pig gall bladder [103]. However, Hollenberg et al. [2] indicated that PAR4 agonists evoke contraction of gastric longitudinal smooth muscle and nitric oxide-dependent relaxation of vascular smooth muscle. PAR4 is also moderately expressed in the human colon [104]. Furthermore, Auge et al. [101] proved that the colonic delivery of PAR4 agonists in mice reduces basal visceral pain and moderates visceral hypersensitivity triggered by PAR2. It was also demonstrated that PAR4 was detected in sensory neurons protruding from the colon and was co-expressed with PAR2 as well as TRPV4. PAR4 attenuates calcium mobilization evoked by PAR2 and TRPV4, while the use of PAR4 agonists alone did not cause any change in the free intracellular calcium mobilization in sensory neuron cells in vitro. A higher dose of the PAR4 agonist increased the visceral sensitivity to colorectal distension and was found to trigger a small increase in macroscopic damage scores and myeloperoxidase activity, indicating the existence of an inflammatory response. These observations are in accordance with the previous studies of a differential effect of PAR4 agonists on the development of inflammatory reaction and hyperalgesia, which suggest that PAR4 agonists may perform double pro- or anti-nociceptive roles in the somatic and visceral domains according to the dose used [105]. Mule et al. [106] have demonstrated that PAR4 is expressed in rat colon, the activation of which triggers contraction of the intestinal longitudinal smooth muscle. They found that PAR4 activation evoked contractile effects in rat colonic longitudinal muscle via treating with TTX, a neuronal transduction blocker, to evaluate the function of neuronal transmission in the induced effects, and it indicated that a neurogenic component was relevant to the PAR4 agonist-induced effects. PAR4 activation can trigger acetylcholine release via an action potential-dependent neuromechanism. Besides, NK1 and NK2 receptor antagonists, when mediated independently or in combination, reduce contraction because of PAR4 activation, indicating the involvement of these receptors in the functions induced by AYPGKF-NH2. The existence of these receptors mediating contraction in the rat colon has been previously proven by histochemistry and functional researches [107–109]. This functional mechanism may support a proinflammatory role for PAR4, which could conduces motility disturbances observed at the time of intestinal trauma and inflammation [106].
PAR4 AS MEDIATORS IN BRAIN MICROGLIAL INFLAMMATION
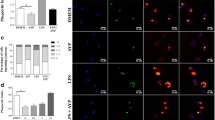
In the central nervous system (CNS), microglia are the major immune effector cells and reactive microgliosis has been implicated in the pathogenesis of a broad range of CNS disorders. These include not only infectious CNS diseases but also acute CNS injuries such as traumatic brain injury (TBI) [110], spinal cord injury [111], stroke, and brain ischemia [112]. In addition, microgliosis is also intimately involved in several chronic neurodegenerative disorders such as Alzheimer’s disease (AD) and amyotrophic lateral sclerosis (ALS) [113, 114]. Regarding the molecular mechanisms underlying thrombin-induced microglial activation, studies have suggested that PAR1 is not involved in the activation of microglia, using parameters such as inducible nitric-acid synthase [115]. However, Suo et al. [116] demonstrated that murine microglial cells constitutively express PAR4 at both the protein and mRNA levels. Functionally, a PAR4-specific agonist peptide mimics the thrombin-induced TNF-α production both in vitro and in vivo. The ineffectiveness of the scrambled PAR4AP on TNF-α induction confirms the specificity of the PAR4-AP effect. The inhibition of the effects of both thrombin and PAR4-AP on TNF-α induction following down-regulation of PAR4 with PAR4-specific antisense oligonucleotide further demonstrates the critical role of PAR4 in thrombin and PAR4-AP-induced TNF-α production. Therefore, PAR4 is at least one of the receptors that mediates the thrombin-induced TNF-α production in both mouse and rat microglia.
Experiments confirmed that PAR4 activation in microglial cells indeed induced a fourfold and twofold, rather than zero, increase of PAR4 binding to GRK5 and GRK2, respectively. This indicates that microglial PAR4, unlike fibroblastic PAR4, may be under the loose control of GRKs [111]. Besides the critically involved cellular thrombin receptors, Suo et al. [116] also revealed that, compared with PAR1, the PAR4 signaling pathway in microglia featured prolonged Ca2+ increase and p44/42 MAPK activation as well as subsequent NF-κB activation. This may explain why PAR1 primarily contributes to promoting microglial proliferation while PAR4 is fully engaged in activating microglia and inducing cytokine (i.e., TNF-α) production. These results are consistent with previously reported thrombin signaling in microglia [115, 117, 118], while adding more detailed features and clearer identification of upstream mediators.
CONCLUSION
PAR4-induced cell signaling remains a puzzle for most cell types. PAR4 activation regulates calcium signaling while PAR4-mediated NO release is independent of a Ca2+ mechanism in endothelial cells [96, 119]. In cardiomyocytes, PAR4 activation causes a certain amount of increased phospholipase C (PLC) and extracellular signal-regulated kinase (ERK) [120]. Furthermore, PAR4 evokes the strong activation of a non-receptor Src tyrosine kinase-p38-mitogen-activated protein kinase (MAPK) cascade in cardiomyocytes [121]. The studies discussed testify a main role of PAR4 signaling in critical pathways that induce regenerative processes and inflammation. These pathways have been demonstrated by the application of specific PAR4 agonist peptides in animal models with appropriate controls in PAR4-deficient animals, as demonstrated by the identification of a selective inhibitory antibody that blocks pathological PAR4 signaling in inflammation mouse models; however, the proteases concerned have not been well studied in vivo. PAR4 seems to be expressed and able to inhibit Ca2+ signaling in all sizes of neurons. Possible direct interactions of PAR with L-, N-, or P/Q-type voltage-gated Ca2+ pathways could explain the anti-nociceptive effects of PAR4 activation and its inhibitory effects against depolarization-induced Ca2+ signaling. Despite a direct inhibitory action of PAR4 activation on primary afferents explaining its analgesic effects, one cannot exclude the possibility that PAR4 might also exert indirect effects on other cell types [101]. To sum up, although the distribution, activation, and biological effects of PAR4 have been realized to a certain extent, deeper exploration of PAR4-mediated pathogenesis is still needed. Previous data suggest that PAR4 activated by thrombin, trypsin, tryptase, and so on play a pivotal role in pathological processes, defining that the crucial protease pathway associated with PAR4 signaling has underlying therapeutic value.
References
Vu, T.-K.H., D.T. Hung, V.I. Wheaton, and S.R. Coughlin. 1991. Molecular cloning of a functional thrombin receptor reveals a novel proteolytic mechanism of receptor activation. Cell 64: 1057–1068.
Hollenberg, M.D., M. Saifeddine, B. Al-Ani, and Y. Gui. 1999. Proteinase-activated receptor 4 (PAR4): Action of PAR4-activating peptides in vascular and gastric tissue and lack of cross-reactivity with PAR1 and PAR2. Canadian Journal of Physiology and Pharmacology 77: 458–464.
Coughlin, S.R. 2000. Thrombin signalling and protease-activated receptors. Nature 407: 258–264.
Steinhoff, M., J. Buddenkotte, V. Shpacovitch, A. Rattenholl, C. Moormann, N. Vergnolle, T.A. Luger, and M.D. Hollenberg. 2005. Proteinase-activated receptors: Transducers of proteinase-mediated signaling in inflammation and immune response. Endocrine Reviews 26: 1–43.
Ramachandran, R., and M. Hollenberg. 2008. Proteinases and signalling: Pathophysiological and therapeutic implications via PARs and more. British Journal of Pharmacology 153: S263–S282.
Macfarlane, S.R., M.J. Seatter, T. Kanke, G.D. Hunter, and R. Plevin. 2001. Proteinase-activated receptors. Pharmacological Reviews 53: 245–282.
Ossovskaya, V.S., and N.W. Bunnett. 2004. Protease-activated receptors: Contribution to physiology and disease. Physiological Reviews 84: 579–621.
Kahn, M.L., Y.-W. Zheng, W. Huang, V. Bigornia, D. Zeng, S. Moff, R.V. Farese, C. Tam, and S.R. Coughlin. 1998. A dual thrombin receptor system for platelet activation. Nature 394: 690–694.
Kahn, M.L., M. Nakanishi-Matsui, M.J. Shapiro, H. Ishihara, and S.R. Coughlin. 1999. Protease-activated receptors 1 and 4 mediate activation of human platelets by thrombin. Journal of Clinical Investigation 103: 879–887.
Nakanishi-Matsui, M., Y.-W. Zheng, D.J. Sulciner, E.J. Weiss, M.J. Ludeman, and S.R. Coughlin. 2000. PAR3 is a cofactor for PAR4 activation by thrombin. Nature 404: 609–613.
McLaughlin, J.N., M.M. Patterson, and A.B. Malik. 2007. Protease-activated receptor-3 (PAR3) regulates PAR1 signaling by receptor dimerization. Proceedings of the National Academy of Sciences 104: 5662–5667.
Riewald, M., R.J. Petrovan, A. Donner, B.M. Mueller, and W. Ruf. 2002. Activation of endothelial cell protease activated receptor 1 by the protein C pathway. Science 296: 1880–1882.
Riewald, M., V.V. Kravchenko, R.J. Petrovan, P.J. O’Brien, L.F. Brass, R.J. Ulevitch, and W. Ruf. 2001. Gene induction by coagulation factor Xa is mediated by activation of protease-activated receptor 1. Blood 97: 3109–3116.
Boire, A., L. Covic, A. Agarwal, S. Jacques, S. Sherifi, and A. Kuliopulos. 2005. PAR1 is a matrix metalloprotease-1 receptor that promotes invasion and tumorigenesis of breast cancer cells. Cell 120: 303–313.
Lourbakos, A., Y. Yuan, A.L. Jenkins, J. Travis, P. Andrade-Gordon, R. Santulli, J. Potempa, and R.N. Pike. 2001. Activation of protease-activated receptors by gingipains fromPorphyromonas gingivalis leads to platelet aggregation: a new trait in microbial pathogenicity. Blood 97: 3790–3797.
Cocks, T.M., and J.D. Moffatt. 2000. Protease-activated receptors: Sentries for inflammation? Trends in Pharmacological Sciences 21: 103–108.
Sambrano, G.R., E.J. Weiss, Y.-W. Zheng, W. Huang, and S.R. Coughlin. 2001. Role of thrombin signalling in platelets in haemostasis and thrombosis. Nature 413: 74–78.
Asfaha, S., N. Cenac, S. Houle, C. Altier, M. Papez, C. Nguyen, M. Steinhoff, K. Chapman, G. Zamponi, and N. Vergnolle. 2007. Protease‐activated receptor‐4: a novel mechanism of inflammatory pain modulation. British Journal of Pharmacology 150: 176–185.
Vergnolle, N., C.K. Derian, M.R. D’Andrea, M. Steinhoff, and P. Andrade-Gordon. 2002. Characterization of thrombin-induced leukocyte rolling and adherence: a potential proinflammatory role for proteinase-activated receptor-4. The Journal of Immunology 169: 1467–1473.
McDougall, J.J., C. Zhang, L. Cellars, E. Joubert, C.M. Dixon, and N. Vergnolle. 2009. Triggering of proteinase‐activated receptor 4 leads to joint pain and inflammation in mice. Arthritis and Rheumatism 60: 728–737.
Kawabata, A., R. Kuroda, N. Kuroki, H. Nishikawa, and K. Kawai. 2000. Dual modulation by thrombin of the motility of rat oesophageal muscularis mucosae via two distinct protease‐activated receptors (PARs): a novel role for PAR‐4 as opposed to PAR‐1. British Journal of Pharmacology 131: 578–584.
Bretschneider, E., R. Kaufmann, M. Braun, G. Nowak, E. Glusa, and K. Schrör. 2001. Evidence for functionally active protease‐activated receptor‐4 (PAR‐4) in human vascular smooth muscle cells. British Journal of Pharmacology 132: 1441–1446.
Kataoka, H., J.R. Hamilton, D.D. McKemy, E. Camerer, Y.-W. Zheng, A. Cheng, C. Griffin, and S.R. Coughlin. 2003. Protease-activated receptors 1 and 4 mediate thrombin signaling in endothelial cells. Blood 102: 3224–3231.
Hollenberg, M.D., M. Saifeddine, S. Sandhu, S. Houle, and N. Vergnolle. 2004. Proteinase‐activated receptor‐4: Evaluation of tethered ligand‐derived peptides as probes for receptor function and as inflammatory agonists in vivo. British Journal of Pharmacology 143: 443–454.
Houle, S., M.D. Papez, M. Ferazzini, M.D. Hollenberg, and N. Vergnolle. 2005. Neutrophils and the kallikrein–kinin system in proteinase‐activated receptor 4‐mediated inflammation in rodents. British Journal of Pharmacology 146: 670–678.
Russell, F.A., Veldhoen, V.E., Tchitchkan, D., and McDougall, J.J. 2009. Proteinase-activated receptor-4 (PAR4) activation leads to sensitization of rat joint primary afferents via a bradykinin B2 receptor-dependent mechanism. Receptor.
Leger, A.J., S.L. Jacques, J. Badar, N.C. Kaneider, C.K. Derian, P. Andrade-Gordon, L. Covic, and A. Kuliopulos. 2006. Blocking the protease-activated receptor 1–4 heterodimer in platelet-mediated thrombosis. Circulation 113: 1244–1254.
Nieman, M.T. 2008. Protease-activated receptor 4 uses anionic residues to interact with α-thrombin in the absence or presence of protease-activated receptor 1†. Biochemistry 47: 13279–13286.
Holinstat, M., B. Voss, M.L. Bilodeau, J.N. McLaughlin, J. Cleator, and H.E. Hamm. 2006. PAR4, but not PAR1, signals human platelet aggregation via Ca2+ mobilization and synergistic P2Y12 receptor activation. Journal of Biological Chemistry 281: 26665–26674.
Voss, B., J.N. McLaughlin, M. Holinstat, R. Zent, and H.E. Hamm. 2007. PAR1, but not PAR4, activates human platelets through a Gi/o/phosphoinositide-3 kinase signaling axis. Molecular Pharmacology 71: 1399–1406.
Knut, F., H. Linda, G. Peter, N. Martina, L.L. Tomas, and G. Magnus. 2011. Protease-activated receptor 1 (PAR1) signalling desensitization is counteracted via PAR4 signalling in human platelets. Biochemical Journal 436: 469–480.
Arora, P., T.K. Ricks, and J. Trejo. 2007. Protease-activated receptor signalling, endocytic sorting and dysregulation in cancer. Journal of Cell Science 120: 921–928.
Covic, L., A.L. Gresser, and A. Kuliopulos. 2000. Biphasic kinetics of activation and signaling for PAR1 and PAR4 thrombin receptors in platelets. Biochemistry 39: 5458–5467.
Faruqi, T.R., E.J. Weiss, M.J. Shapiro, W. Huang, and S.R. Coughlin. 2000. Structure-function analysis of protease-activated receptor 4 tethered ligand peptides determinants of specificity and utility in assays of receptor function. Journal of Biological Chemistry 275: 19728–19734.
Hung, D.T., T. Vu, N.A. Nelken, and S.R. Coughlin. 1992. Thrombin-induced events in non-platelet cells are mediated by the unique proteolytic mechanism established for the cloned platelet thrombin receptor. The Journal of Cell Biology 116: 827–832.
Paul, B.Z., J. Jin, and S.P. Kunapuli. 1999. Molecular mechanism of thromboxane A2-induced platelet aggregation ESSENTIAL ROLE FOR P2T AC and α2ARECEPTORS. Journal of Biological Chemistry 274: 29108–29114.
Kim, S., C. Foster, A. Lecchi, T.M. Quinton, D.M. Prosser, J. Jin, M. Cattaneo, and S.P. Kunapuli. 2002. Protease-activated receptors 1 and 4 do not stimulate Gi signaling pathways in the absence of secreted ADP and cause human platelet aggregation independently of Gisignaling. Blood 99: 3629–3636.
Kim, S., J. Jin, and S.P. Kunapuli. 2006. Relative contribution of G-protein-coupled pathways to protease-activated receptor-mediated Akt phosphorylation in platelets. Blood 107: 947–954.
Jantzen, H.-M., D.S. Milstone, L. Gousset, P.B. Conley, and R.M. Mortensen. 2001. Impaired activation of murine platelets lacking Gαi2. Journal of Clinical Investigation 108: 477–483.
Weiss, E.J., J.R. Hamilton, K.E. Lease, and S.R. Coughlin. 2002. Protection against thrombosis in mice lacking PAR3. Blood 100: 3240–3244.
Mao, Y., J. Jin, J.L. Daniel, and S.P. Kunapuli. 2009. Regulation of plasmin-induced protease-activated receptor 4 activation in platelets. Platelets 20: 191–198.
Arachiche, A., M. de la Fuente, and M.T. Nieman. 2013. Calcium mobilization and protein kinase C activation downstream of protease activated receptor 4 (PAR4) is negatively regulated by PAR3 in mouse platelets. PloS One 8: e55740.
DeWire, S.M., S. Ahn, R.J. Lefkowitz, and S.K. Shenoy. 2007. β-arrestins and cell signaling. Annual Review of Physiology 69: 483–510.
Reiter, E., and R.J. Lefkowitz. 2006. GRKs and β-arrestins: Roles in receptor silencing, trafficking and signaling. Trends in Endocrinology and Metabolism 17: 159–165.
Luttrell, L., S. Ferguson, Y. Daaka, W. Miller, S. Maudsley, G. Della Rocca, F.-T. Lin, H. Kawakatsu, K. Owada, and D. Luttrell. 1999. β-Arrestin-dependent formation of β2 adrenergic receptor-Src protein kinase complexes. Science 283: 655–661.
Yang, M., R. He, J. Benovic, and R. Ye. 2009. beta-Arrestin1 interacts with the G-protein subunits beta1gamma2 and promotes beta1gamma2-dependent Akt signalling for NF-kappaB activation. Biochemical Journal 417: 287–296.
Lodeiro, M., M. Theodoropoulou, M. Pardo, F.F. Casanueva, and J.P. Camiña. 2009. c-Src regulates Akt signaling in response to ghrelin via β-arrestin signaling-independent and-dependent mechanisms. PLoS One 4: e4686.
Goel, R., P.J. Phillips-Mason, D.M. Raben, and J.J. Baldassare. 2002. α-Thrombin induces rapid and sustained Akt phosphorylation by β-arrestin1-dependent and-independent mechanisms, and only the sustained Akt phosphorylation is essential for G1 phase progression. Journal of Biological Chemistry 277: 18640–18648.
Buchanan, F.G., D.L. Gorden, P. Matta, Q. Shi, L.M. Matrisian, and R.N. DuBois. 2006. Role of β-arrestin 1 in the metastatic progression of colorectal cancer. Proceedings of the National Academy of Sciences of the United States of America 103: 1492–1497.
Álvarez, C.J., M. Lodeiro, M. Theodoropoulou, J.P. Camiña, F.F. Casanueva, and Y. Pazos. 2009. Obestatin stimulates Akt signalling in gastric cancer cells through β-arrestin-mediated epidermal growth factor receptor transactivation. Endocrine-Related Cancer 16: 599–611.
Goel, R., P.J. Phillips-Mason, A. Gardner, D.M. Raben, and J.J. Baldassare. 2004. α-Thrombin-mediated phosphatidylinositol 3-kinase activation through release of Gβγ dimers from Gαq and Gαi2. Journal of Biological Chemistry 279: 6701–6710.
Li, D., S. August, and D.S. Woulfe. 2008. GSK3β is a negative regulator of platelet function and thrombosis. Blood 111: 3522–3530.
Xiang, B., G. Zhang, J. Liu, A.J. Morris, S.S. Smyth, T.K. Gartner, and Z. Li. 2010. A Gi‐independent mechanism mediating Akt phosphorylation in platelets. Journal of Thrombosis and Haemostasis 8: 2032–2041.
Li, D., L. D’Angelo, M. Chavez, and D.S. Woulfe. 2011. Arrestin-2 differentially regulates PAR4 and ADP receptor signaling in platelets. Journal of Biological Chemistry 286: 3805–3814.
Szotowski, B., S. Antoniak, W. Poller, H.-P. Schultheiss, and U. Rauch. 2005. Procoagulant soluble tissue factor is released from endothelial cells in response to inflammatory cytokines. Circulation Research 96: 1233–1239.
Sommeijer, D., H. Hansen, R. Van Oerle, K. Hamulyak, A. Van Zanten, E. Meesters, H. Spronk, and H. Ten Cate. 2006. Soluble tissue factor is a candidate marker for progression of microvascular disease in patients with type 2 diabetes. Journal of Thrombosis and Haemostasis 4: 574–580.
Bokarewa, M., J. Morrissey, and A. Tarkowski. 2002. Intra-articular tissue factor/factor VII complex induces chronic arthritis. Inflammation Research 51: 471–477.
Bokarewa, M.I., J.H. Morrissey, and A. Tarkowski. 2002. Tissue factor as a proinflammatory agent. Arthritis Research 4: 190–195.
Busso, N., V. Chobaz-Péclat, J. Hamilton, P. Spee, N. Wagtmann, and A. So. 2008. Essential role of platelet activation via protease activated receptor 4 in tissue factor-initiated inflammation. Arthritis Research and Therapy 10: R42.
Yang, Y.H., P. Hall, C.B. Little, A.J. Fosang, G. Milenkovski, L. Santos, J. Xue, P. Tipping, and E.F. Morand. 2005. Reduction of arthritis severity in protease‐activated receptor–deficient mice. Arthritis and Rheumatism 52: 1325–1332.
Cunningham, M.A., E. Rondeau, X. Chen, S.R. Coughlin, S.R. Holdsworth, and P.G. Tipping. 2000. Protease-activated receptor 1 mediates thrombin-dependent, cell-mediated renal inflammation in crescentic glomerulonephritis. The Journal of Experimental Medicine 191: 455–462.
Steranka, L.R., D.C. Manning, C.J. DeHaas, J.W. Ferkany, S.A. Borosky, J.R. Connor, R.J. Vavrek, J.M. Stewart, and S.H. Snyder. 1988. Bradykinin as a pain mediator: Receptors are localized to sensory neurons, and antagonists have analgesic actions. Proceedings of the National Academy of Sciences 85: 3245–3249.
Bignold, L., and A. Lykke. 1975. Increased vascular permeability induced in synovialis of the rat by histamine, serotonin and bradykinin. Experientia 31: 671–672.
Dick, W., D. Grennan, and I. Zeitlin. 1976. Studies on the relative effects of prostaglandins, bradykinin, 5‐hydroxytryptamine and histamine on the synovial microcirculation in dogs. British Journal of Pharmacology 56: 313–316.
Cruwys, S., B. Kidd, P. Mapp, D. Walsh, and D. Blake. 1992. The effects of calcitonin gene‐related peptide on formation of intra‐articular oedema by inflammatory mediators. British Journal of Pharmacology 107: 116–119.
Kanaka, R., H.-G. Schaible, and R. Schmidt. 1985. Activation of fine articular afferent units by bradykinin. Brain Research 327: 81–90.
Neugebauer, V., H.-G. Schaible, and R. Schmidt. 1989. Sensitization of articular afferents to mechanical stimuli by bradykinin. Pflügers Archiv 415: 330–335.
Vergnolle, N., M.D. Hollenberg, K.A. Sharkey, and J.L. Wallace. 1999. Characterization of the inflammatory response to proteinase‐activated receptor‐2 (par2)‐activating peptides in the rat paw. British Journal of Pharmacology 127: 1083–1090.
Steinhoff, M., N. Vergnolle, S. Young, M. Tognetto, S. Amadesi, H. Ennes, M. Trevisani, M. Hollenberg, J. Wallace, and G. Caughey. 2000. Agonists of proteinase-activated receptor 2 induce inflammation by a neurogenic mechanism. Nature Medicine 6: 151–158.
de Garavilla, L., N. Vergnolle, S.H. Young, H. Ennes, M. Steinhoff, V.S. Ossovskaya, M.R. D’Andrea, E.A. Mayer, J.L. Wallace, and M.D. Hollenberg. 2001. Agonists of proteinase‐activated receptor 1 induce plasma extravasation by a neurogenic mechanism. British Journal of Pharmacology 133: 975–987.
D’Andrea, M.R., M.R. Saban, N.-B. Nguyen, P. Andrade-Gordon, and R. Saban. 2003. Expression of protease-activated receptor-1,-2,-3, and-4 in control and experimentally inflamed mouse bladder. The American Journal of Pathology 162: 907–923.
Wang, Z., D. Chen, Z. Zhang, R. Zhang, S. An, and L. Yu. 2013. Protease‐activated receptor 4 activation increases the expression of calcitonin gene‐related peptide mRNA and protein in dorsal root ganglion neurons. Journal of Neuroscience Research 91: 1551–1562.
Vellani, V., A.M. Kinsey, M. Prandini, S.C. Hechtfischer, P. Reeh, P.C. Magherini, C. Giacomoni, and P.A. McNaughton. 2010. Protease activated receptors 1 and 4 sensitize TRPV1 in nociceptive neurones. Molecular Pain 6: 61.
Donnerer, J., and I. Liebmann. 2011. Phosphorylation of ERK1/2 in dorsal root ganglia following sequential mustard oil and thermal stimulation of the rat hind paw. Pharmacology 89: 7–12.
Brunet, A., D. Roux, P. Lenormand, S. Dowd, S. Keyse, and J. Pouysségur. 1999. Nuclear translocation of p42/p44 mitogen‐activated protein kinase is required for growth factor‐induced gene expression and cell cycle entry. The EMBO Journal 18: 664–674.
Hochholdinger, F., G. Baier, A. Nogalo, B. Bauer, H.H. Grunicke, and F. Überall. 1999. Novel membrane-targeted ERK1 and ERK2 chimeras which act as dominant negative, isotype-specific mitogen-activated protein kinase inhibitors of Ras-Raf-mediated transcriptional activation of c-fos in NIH 3T3 cells. Molecular and Cellular Biology 19: 8052–8065.
Lanigan, T.M., and A.F. Russo. 1997. Binding of upstream stimulatory factor and a cell-specific activator to the calcitonin/calcitonin gene-related peptide enhancer. Journal of Biological Chemistry 272: 18316–18324.
Nakanishi, M., K. Hata, T. Nagayama, T. Sakurai, T. Nishisho, H. Wakabayashi, T. Hiraga, S. Ebisu, and T. Yoneda. 2010. Acid activation of Trpv1 leads to an up-regulation of calcitonin gene-related peptide expression in dorsal root ganglion neurons via the CaMK-CREB cascade: a potential mechanism of inflammatory pain. Molecular Biology of the Cell 21: 2568–2577.
Tajti, J., A. Kuris, L. Vécsei, C.-B. Xu, and L. Edvinsson. 2011. Organ culture of the trigeminal ganglion induces enhanced expression of calcitonin gene-related peptide via activation of extracellular signal-regulated protein kinase 1/2. Cephalalgia 31: 95–105.
Hetman, M., and A. Gozdz. 2004. Role of extracellular signal regulated kinases 1 and 2 in neuronal survival. European Journal of Biochemistry 271: 2050–2055.
Chen, R., C. Sarnecki, and J. Blenis. 1992. Nuclear localization and regulation of erk-and rsk-encoded protein kinases. Molecular and Cellular Biology 12: 915–927.
Ritchie, E., M. Saka, C. Mackenzie, R. Drummond, C. Wheeler‐Jones, T. Kanke, and R. Plevin. 2007. Cytokine upregulation of proteinase‐activated‐receptors 2 and 4 expression mediated by p38 MAP kinase and inhibitory kappa B kinase β in human endothelial cells. British Journal of Pharmacology 150: 1044–1054.
Ma, C., K.A. Bower, G. Chen, X. Shi, Z.-J. Ke, and J. Luo. 2008. Interaction between ERK and GSK3β mediates basic fibroblast growth factor-induced apoptosis in SK-N-MC neuroblastoma cells. Journal of Biological Chemistry 283: 9248–9256.
De Sousa, L.P., B.S. Brasil, B.M. Silva, M.H. Freitas, S.V. Nogueira, P.C. Ferreira, E.G. Kroon, and C.A. Bonjardim. 2005. Plasminogen/plasmin regulates c-fos and egr-1 expression via the MEK/ERK pathway. Biochemical and Biophysical Research Communications 329: 237–245.
Versteeg, H., K. Borensztajn, M. Kerver, W. Ruf, P. Reitsma, C. Spek, and M. Peppelenbosch. 2008. TF: FVIIa‐specific activation of CREB upregulates proapoptotic proteins via protease‐activated receptor‐2. Journal of Thrombosis and Haemostasis 6: 1550–1557.
Wang, H., S. Wen, N.W. Bunnett, R. Leduc, M.D. Hollenberg, and W.K. MacNaughton. 2008. Proteinase-activated receptor-2 induces cyclooxygenase-2 expression through β-catenin and cyclic AMP-response element-binding protein. Journal of Biological Chemistry 283: 809–815.
Lei, L., X. Yuan, S. Wang, F. Zhang, Y. Han, Q. Ning, G. Luo, and S. Lu. 2012. Mitogen-activated protein kinase pathways are involved in the upregulation of calcitonin gene-related peptide of rat trigeminal ganglion after organ culture. Journal of Molecular Neuroscience 48: 53–65.
Ji, R.-R., H. Baba, G.J. Brenner, and C.J. Woolf. 1999. Nociceptive-specific activation of ERK in spinal neurons contributes to pain hypersensitivity. Nature Neuroscience 2: 1114–1119.
Zhu, W.-J., H. Yamanaka, K. Obata, Y. Dai, K. Kobayashi, T. Kozai, A. Tokunaga, and K. Noguchi. 2005. Expression of mRNA for four subtypes of the proteinase-activated receptor in rat dorsal root ganglia. Brain Research 1041: 205–211.
Bulling, D.G., D. Kelly, S. Bond, D.S. McQueen, and J.R. Seckl. 2001. Adjuvant‐induced joint inflammation causes very rapid transcription of β‐preprotachykinin and α‐CGRP genes in innervating sensory ganglia. Journal of Neurochemistry 77: 372–382.
Ambalavanar, R., M. Moritani, A. Moutanni, P. Gangula, C. Yallampalli, and D. Dessem. 2006. Deep tissue inflammation upregulates neuropeptides and evokes nociceptive behaviors which are modulated by a neuropeptide antagonist. Pain 120: 53–68.
Xu, X., P. Wang, X. Zou, D. Li, L. Fang, and Q. Lin. 2009. Increases in transient receptor potential vanilloid‐1 mRNA and protein in primary afferent neurons stimulated by protein kinase C and their possible role in neurogenic inflammation. Journal of Neuroscience Research 87: 482–494.
Benemei, S., P. Nicoletti, J.G. Capone, and P. Geppetti. 2009. CGRP receptors in the control of pain and inflammation. Current Opinion in Pharmacology 9: 9–14.
Dattilio, A., and M.A. Vizzard. 2005. Up-regulation of protease activated receptors in bladder after cyclophosphamide induced cystitis and colocalization with capsaicin receptor (VR1) in bladder nerve fibers. The Journal of Urology 173: 635–639.
Chen, D., Z. Wang, Z. Zhang, R. Zhang, and L. Yu. 2013. Capsaicin up-regulates protease-activated receptor-4 mRNA and protein in primary cultured dorsal root ganglion neurons. Cellular and Molecular Neurobiology 33: 337–346.
Asfaha, S., V. Brussee, K. Chapman, D.W. Zochodne, and N. Vergnolle. 2002. Proteinase‐activated receptor‐1 agonists attenuate nociception in response to noxious stimuli. British Journal of Pharmacology 135: 1101–1106.
Bar-Shavit, R., A. Kahn, G.D. Wilner, and J.W. Fenton. 1983. Monocyte chemotaxis: Stimulation by specific exosite region in thrombin. Science 220: 728–731.
Bar-Shavit, R., and G.D. Wilner. 1986. Biologic activities of nonenzymatic thrombin: Elucidation of a macrophage interactive domain. Seminars in Thrombosis and Hemostasis 12: 244–249.
Herbert, J., E. Dupuy, M. Laplace, J. Zini, S.R. Bar, and G. Tobelem. 1994. Thrombin induces endothelial cell growth via both a proteolytic and a non-proteolytic pathway. Biochemical Journal 303: 227–231.
Kaplan, A.P., K. Joseph, and M. Silverberg. 2002. Pathways for bradykinin formation and inflammatory disease. Journal of Allergy and Clinical Immunology 109: 195–209.
Auge, C., D. Balz‐hara, M. Steinhoff, N. Vergnolle, and N. Cenac. 2009. Protease‐activated receptor‐4 (PAR4): a role as inhibitor of visceral pain and hypersensitivity. Neurogastroenterology and Motility 21: 1189–e1107.
Kawabata, A., R. Kuroda, H. Nishikawa, and K. Kawai. 1999. Modulation by protease‐activated receptors of the rat duodenal motility in vitro: Possible mechanisms underlying the evoked contraction and relaxation. British Journal of Pharmacology 128: 865–872.
Tognetto, M., M. Trevisani, B. Maggiore, G. Navarra, A. Turini, R. Guerrini, N.W. Bunnett, P. Geppetti, and S. Harrison. 2000. Evidence that PAR‐1 and PAR‐2 mediate prostanoid‐dependent contraction in isolated guinea‐pig gallbladder. British Journal of Pharmacology 131: 689–694.
Xu, W.-f., H. Andersen, T.E. Whitmore, S.R. Presnell, D.P. Yee, A. Ching, T. Gilbert, E.W. Davie, and D.C. Foster. 1998. Cloning and characterization of human protease-activated receptor 4. Proceedings of the National Academy of Sciences 95: 6642–6646.
Bradesi, S. 2009. PAR4: a new role in the modulation of visceral nociception. Neurogastroenterology and Motility 21: 1129–1132.
Mule, F., R. Pizzuti, A. Capparelli, and N. Vergnolle. 2004. Evidence for the presence of functional protease activated receptor 4 (PAR4) in the rat colon. Gut 53: 229–234.
Maggi, C.A. 1995. Tachykinins and calcitonin gene-related peptide (CGRP) as co-transmitters released from peripheral endings of sensory nerves. Progress in Neurobiology 45: 1–98.
Grady, E.F., P. Baluk, S. Böhm, P.D. Gamp, H. Wong, D.G. Payan, J. Ansel, A.L. Portbury, J.B. Furness, and D.M. McDonald. 1996. Characterization of antisera specific to NK1, NK2, and NK3 neurokinin receptors and their utilization to localize receptors in the rat gastrointestinal tract. The Journal of Neuroscience 16: 6975–6986.
Serio, R., F. Mule, F. Bonvissuto, and A. Postorino. 1998. Tachykinins mediate noncholinergic excitatory neural responses in the circular muscle of rat proximal colon. Canadian Journal of Physiology and Pharmacology 76: 684–689.
Csuka, E., V.H. Hans, E. Ammann, O. Trentz, T. Kossmann, and M.C. Morganti-Kossmann. 2000. Cell activation and inflammatory response following traumatic axonal injury in the rat. Neuroreport 11: 2587–2590.
Popovich, P.G. 2000. Immunological regulation of neuronal degeneration and regeneration in the injured spinal cord. Progress in Brain Research 128: 43.
Stoll, G., S. Jander, and M. Schroeter. 1998. Inflammation and glial responses in ischemic brain lesions. Progress in Neurobiology 56: 149–171.
Benveniste, E.N. 1997. Role of macrophages/microglia in multiple sclerosis and experimental allergic encephalomyelitis. Journal of Molecular Medicine 75: 165–173.
McGeer, E.G., and P.L. McGeer. 1998. The importance of inflammatory mechanisms in Alzheimer disease. Experimental Gerontology 33: 371–378.
Ryu, J., H. Pyo, I. Jou, and E. Joe. 2000. Thrombin induces NO release from cultured rat microglia via protein kinase C, mitogen-activated protein kinase, and NF-κB. Journal of Biological Chemistry 275: 29955–29959.
Suo, Z., M. Wu, B.A. Citron, C. Gao, and B.W. Festoff. 2003. Persistent protease-activated receptor 4 signaling mediates thrombin-induced microglial activation. Journal of Biological Chemistry 278: 31177–31183.
Möller, T., U.K. Hanisch, and B.R. Ransom. 2000. Thrombin‐induced activation of cultured rodent microglia. Journal of Neurochemistry 75: 1539–1547.
Suo, Z., M. Wu, S. Ameenuddin, H.E. Anderson, J.E. Zoloty, B.A. Citron, P. Andrade‐Gordon, and B.W. Festoff. 2002. Participation of protease‐activated receptor‐1 in thrombin‐induced microglial activation. Journal of Neurochemistry 80: 655–666.
Hirano, K., N. Nomoto, M. Hirano, F. Momota, A. Hanada, and H. Kanaide. 2007. Distinct Ca2+ requirement for NO production between proteinase-activated receptor 1 and 4 (PAR1 and PAR4) in vascular endothelial cells. Journal of Pharmacology and Experimental Therapeutics 322: 668–677.
Steinberg, S.F. 2005. The cardiovascular actions of protease-activated receptors. Molecular Pharmacology 67: 2–11.
Sabri, A., J. Guo, H. Elouardighi, A.L. Darrow, P. Andrade-Gordon, and S.F. Steinberg. 2003. Mechanisms of Protease-activated Receptor-4 Actions in Cardiomyocytes ROLE OF Src TYROSINE KINASE. Journal of Biological Chemistry 278: 11714–11720.
Author information
Authors and Affiliations
Corresponding author
Additional information
Qiang Fu and Jing Cheng are co-first authors; they contributed equally to the work.
Rights and permissions
About this article
Cite this article
Fu, Q., Cheng, J., Gao, Y. et al. Protease-Activated Receptor 4: A Critical Participator in Inflammatory Response. Inflammation 38, 886–895 (2015). https://doi.org/10.1007/s10753-014-9999-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-014-9999-6