Abstract
The purpose of this study is to investigate the anti-inflammatory effect of thalidomide (Thd) on H1N1-induced acute lung injury in mice. BALB/C mice were infected intranasally with influenza A virus (H1N1) and then treated with Thd at a dose of 100 or 200 mg/kg/day for 7 days. Weight loss and survival of mice were monitored for 14 days after virus challenge, and the serum and lung tissues were collected at 4 days for histological and biochemical analysis. The results showed that Thd significantly improved the survival rate, reduced the infiltration of inflammatory cells and cytokine (e.g., IL-6, TNF-α) and chemokine (e.g., RANTES, IP-10) levels, and inhibited activated p-NFκB p65 in infected mice. These findings suggested that Thd may attenuate H1N1-induced pulmonary injury and thus may find use in the treatment of viral diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Influenza viruses may cause acute respiratory disease with significant morbidity and mortality each year. In 2009, a novel influenza A (H1N1) virus emerged in Mexico and then spread rapidly worldwide, leading the World Health Organization to declare a phase-6 pandemic alert [1]. It has been well documented that the pathogenicity of influenza virus is associated with the expression of cytokines/chemokines [2]. They may be particularly important in the pathological development of viral infection, as the production of cytokines by infected cells seems to be a prerequisite for the initiation of an immune response to control viral replication, and a cytokine storm contributes to severe post-infection complications. A better knowledge of the inflammatory response to influenza A virus infection may help to control the occurrence of complications and to reduce the associated tissue damage [3]. For this reason, anti-inflammatory agents have been considered to be important constituents of anti-influenza treatment strategies.
Thalidomide (α-N-phthalimidoglutarimide), a glutamic acid derivative initially developed as a sedative, was withdrawn from the market due to its teratogenic effects. However, a number of clinical and experimental studies have demonstrated that thalidomide and its analogs are effective in the treatment of a wide variety of diseases [4], including erythema nodosum leprosum, multiple myeloma, rheumatoid arthritis, Crohn's disease, prostate cancer, and lupus erythematosus [5]. It also showed that interleukins-6 (IL-6), IL-10, and tumor necrosis factor-alpha (TNF-α) were significantly higher in patients with influenza H1N1 than in healthy controls [6]. Thalidomide has been reintroduced into clinical practice as an anti-inflammatory and anti-cancer agent in recent years, and it can be a potent inhibitor of TNF-α, IL-1β, 6, 12, and granulocyte macrophage-colony stimulating factor (GM-CSF) [7].
In line with the hypothesis that an effective treatment for H1N1-induced lung injury should have considerable anti-inflammatory and anti-viral effects, thalidomide may be of particular benefit for fatal viral pneumonia. In this study, we aim to examine whether thalidomide has a protective effect on H1N1-induced lung injury in mice and to investigate the mechanism underlying its therapeutic effect on pulmonary inflammation.
MATERIALS AND METHODS
Animals and Chemicals
Male BALB/C mice of about 16–18 g were purchased from Shanghai SLACCAS Laboratory Animal Co., Ltd. (Shanghai, China), thalidomide from Changzhou Pharmaceutical Co., Ltd. (Lot number: 12042232; Jiangsu, China), and ribavirin bulk pharmaceutical chemicals from Zhaoqing Pharmaceutical Co., Ltd. (Guangdong, China), respectively. All experimental protocols were approved by the Animal Experiment Committee of Fudan University (Approval No. 2009001901364).
Virus
A mouse-adapted strain of influenza virus A/FM/1/47 (H1N1) supplied by Shanghai Center for Disease Control & Prevention (Shanghai, China) was stored in aliquots at −70 °C, and a fresh aliquot was thawed for each experiment.
Main Reagents
Mouse TNF-α; interferon (IFN)-α; IL-6; IL-10; regulated on activation normal T cell expressed and secreted factor (RANTES); interferon-inducible protein-10 (IP-10); monocyte chemot actic protein-1 (MCP-1); and macrophage inflammatory protein-1α (MIP-1α) ELISA kit (Abcam, England) were supplied by Jinma Laboratory Equipment Co., Ltd. (Lot number: 201303; Shanghai, China) and monoclonal antibody of p-NF-κB p65(Ser 276) by Santa Cruz Biotechnology, Inc. (Santa Cruz, CA, USA), respectively.
Survival Experiments
Mice were randomly divided into five groups of 12 mice each and infected intranasally with influenza virus A/FM/1/47 H1N1 under isoflurane anesthesia at a 10 × LD50 (median lethal dose) dose in a volume of 30 μL per mouse. The treatment was initiated 2 h after virus challenge. Mice were gavaged once daily for 7 days with saline solution (normal control group), distilled water (virus control group), Thd administered intragastrically at a dose of 100 mg/kg/day (Thd100 group) or 200 mg/kg/day (Thd200 group), or ribavirin at a dose of 100 mg/kg/day (Rib group). Weight loss and survival of mice were monitored for 14 days after virus challenge.
Lung Injury Experiments
Mice were randomly divided into five groups of eight mice each. All mice were infected with influenza virus as described above, then treated intragastrically with thalidomide and ribavirin daily for 4 days, and then sacrificed by euthanasia at 4 days to harvest lung tissues. The tissues were weighted, the left lobes were suspended in PBS-buffered formalin for pathological observation, and the rest was stored at −70 °C for the analysis of cytokine/chemokine.
Histological Examination
Histological examination of the lung tissues from each group was performed to evaluate the severity of H1N1-induced lung injury. Tissue specimens were fixed in PBS-buffered formalin for 24 h, embedded in paraffin, sliced into 5-μm-thick sections, and stained with hematoxylin and eosin for pathological observation.
Assay for Pulmonary Viral Titer
Viral load was presented as hemagglutinin (HA) titer as in a previous study [8]. Each lung was homogenized to a 10 % (w/v) suspension with PBS, and the homogenates were serially diluted twofold. Homogenate dilution of 50 μL was added to each well of V-bottom microplate, and then 50 μL of 1 % suspension of chicken red blood cells in PBS was added. The suspensions were mixed and incubated at room temperature for 30 min. The final dilution of homogenate that agglutinated red blood cells was considered the end point of titration, and the HA titer was calculated.
Measurement of Inflammatory Cytokines and Chemokines
Anti-mouse IFN-α, TNF-α, IL-6, RANTES, IL-1, IP-10, MCP-1, and MIP-1α antibodies were used to coat the 96-well filtration plates (Abcam). Lung homogenates were prepared at a concentration of 100 mg tissue/ml PBS and then centrifuged for assay using specific sandwich ELISA kits according to the manufacturer’s instructions.
Immunohistochemical Analysis
Four-μm-thick, formalin-fixed, paraffin-embedded tissues were immunostained using the streptavidin-biotin-horseradish peroxidase method. The deparaffinized sections were rehydrated through a graded series of alcohol and then microwaved in EDTA antigen retrieval buffer (pH 8.0) at 97 °C for 12 min to unmask antigen epitopes. The sections were treated with 3 % hydrogen peroxide methanol solution for 10 min to block endogenous peroxidase and then incubated with 100 μl serum for 30 min at 37 °C. The serum was removed, and the sections were incubated with primary antibody p-NFκB p65 dilution overnight at 4 °C and then with ready-to-use HRP-labeled secondary antibody at 37 °C for 30 min each. The tissues were stained in DAB (3’3-diaminobenzidine) substrate and then counterstained with hematoxylin, dehydrated, and mounted.
Statistical Analyses
All statistical analyses were performed using GraphPad Prism for Windows, version 6.0. Gehan-Breslow-Wilcoxon test was used for comparisons of survival data and Mann-Whitney test for other comparisons. For all analyses, P ≤ 0.05 was considered to be statistically significant.
RESULTS
Survival Rate
BALB/C mice showed signs of piloerection, lethargy, weight loss, and reduced food intake 3 days after infection with H1N1 virus, and some of them died from 7 to 11 days. Figure 1 showed that no mice survived in the virus control group (0/12), whereas the survival rate at 14 days was 25 % (3/12), 41.7 % (5/12), and 83.3 %(10/12) for the Thd100, Thd200, and Rib group, respectively, which were significantly higher than the virus control group.
Effect of Thd on the survival rate of influenza virus-infected mice. Mice were infected intranasally with influenza virus at a 10 × LD50 dose and then treated with saline solution (normal control group), distilled water (virus control group), Thd at a dose of 100 (Thd100 group) or 200 mg/kg/day (Thd200 group), or ribavirin at a dose of 100 mg/kg/day (Rib group). Survival of mice was monitored daily for 14 days after viral infection, and the survival rate was calculated.
Pulmonary Damage
The main pathological damage observed in mice infected with influenza virus was viral interstitial pneumonia that occurred 4 days after virus inoculation. The lung/body index in virus control mice was increased, indicating that influenza A (H1N1) infection caused swelling of the lung tissues and weight loss. In microcosmic view, most infected mice showed severe infiltration of monocytes and lymphocytes, thickened alveolar walls, and exudation of inflammatory cells into the alveolar space. Thd markedly ameliorated the pathological injury induced by H1N1 in a dose-dependent manner, as it was found that Thd at 200 mg/kg/day significantly decreased the number of influenza-related focal lesions and lung consolidation (Fig. 2) and lung/body index (Fig. 3) as well as the infiltration of monocytes and lymphocytes.
Pulmonary histopathological change in influenza virus-infected mice on day 4 after infection. a Normal control mice (×100); b virus control mice (200×); c, d Thd-treated mice (100 and 200 mg/kg/day) (×200); e Rib-treated mice (100 mg/kg/day) (×200). On day 4 after infection, mice showed pathological damages of acute viral pneumonia. b Showed severe infiltration of monocytes and lymphocytes and thickened alveolar walls. After treatment with Thd or Rib, infiltration of monocytes and lymphocytes was significantly suppressed (c, d, e).
Effect of Thd on the lung/body index of influenza virus-infected mice. Mice infected with 10 × LD50 influenza virus were sacrificed to calculate the lung/body index (lung weight/body weight) on day 4 post-infection. Each bar represents mean ± SD of eight mice. *P < 0.05, ***P < 0.001 compared with the virus control group.
HA Titers of Pulmonary Tissue
HA is the predominant surface glycoprotein of influenza virus, and its expression is positively correlated with copies of influenza virus. Figure 4 showed that HA titers in the lungs were significantly higher in virus control mice than in normal control mice (P < 0.01) and those mice treated with Thd at a dose of either 100 or 200 mg/kg/day.
Inhibitory effect of Thd on the pulmonary HA titer of influenza virus-infected mice. Each bar represents mean ± SD of eight mice. Mice infected with influenza H1N1 virus were treated intragastrically with Thd or Rib and then sacrificed by euthanasia 4 days later. Lungs were homogenized in PBS, and the homogenates were serially diluted twofold, and HA test was conducted. HA titers were expressed as the maximum dilution that caused complete agglutination. *P < 0.05, **P < 0.001 compared with the virus control group.
Cytokine/Chemokine Levels in Lungs
Influenza virus infection is known to induce a strong inflammatory reaction, hallmarked by the production of cytokines and chemokines. Lungs were collected at 4 days after infection for the measurement of cytokines/chemokines. It showed in Figs. 5 and 6 that Thd at a dose of 200 mg/kg/day significantly inhibited the production of TNF-α, IL-6, RANTES IFN-a, and IP-10 and that the concentrations of IL-1, MCP-1, and MIP-1α were slightly but not significantly lower in Thd-treated mice. Quantitative analysis showed that Thd reduced cytokines in a dose-dependent manner and inhibited excessive cytokines/chemokines released by innate immune cells.
Cytokine expression (IFN-α, TNF-α, IL-6, IL-1) in mice following the treatment of Thd at 4 days after infection. Cytokines in lung homogenates and serum were determined using ELISA, and the results represent the mean of eight mice. *P < 0.05, **P < 0.01, ***P < 0.001 as compared with the virus control group.
Chemokine (RANTES, MCP-1, MIP-1α, and IP-10) expression in mice following the treatment of Thd at 4 days after infection. Chemokines in lung homogenates and serum were determined using ELISA, and the results represent the mean of eight mice. *P < 0.05, **P < 0.01 as compared with the virus control group.
P-NFκBp65 Activity
The staining obtained with p-NF-κB antibody was assessed. A difference in staining intensity was observed between the non-infected and infected cell area and linked to the presence of inflammation. Figure 7 showed that H1N1 infection significantly up-regulated p-NF-κB activity in the virus control mice, but their expression could be inhibited by Thd at a dose of 200 mg/kg/day.
Immunohistochemical expression of p-NFκBp65 in lungs of H1N1 influenza virus-infected mice. The superior lobe of right lung was evaluated by immunohistochemistry using anti-p-NFκB p65 on day 4. a Normal control mice (×100); b viral control mice 4 (×200); c, d Thd-treated mice (100 or 200 mg/kg/day) (200×); e Rib-treated mice (100 mg/kg/day) (×200). On day 4, the infected mice showed strong expressions of p-NFκBp65 in the infiltrated area of monocytes and lymphocytes. However, NF-kappaB expression was weak after the treatment with Thd or Rib.
DISCUSSION
The aim of the present study was to assess the effects of Thd on H1N1-induced pulmonary injury in mice. The results showed that Thd inhibited the replication of H1N1 and thus suppressed the induced pulmonary inflammation. The association between inflammation and lung injury has been well established, then the anti-inflammatory activity of Thd was assessed in mice infected with lethal influenza virus. The results showed that Thd significantly suppressed the expression of cytokines and chemokines released by epithelial and inflammatory cells and correlated with activated NFκBp65 signal pathway.
Immune response is a double-edged sword. It presents a powerful barrier against viruses and can target virus-infected cells. However, excessive inflammation due to overabundant production of proinflammatory cytokines and lung inflammatory infiltrates is considered an important factor in disease pathogenesis [9, 10]. Therefore, suppression of cytokine/chemokine production appears to be a viable approach to control severe inflammatory complications induced by influenza virus. IFN-α as an anti-viral protein can activate inflammatory cells and stimulate expression of multiple cytokines/chemokines. IL-6 expression and TNF-α secretion are directly linked to host morbidity and pulmonary injury. Chemokines, such as RANTES and IP-10 produced by epithelial cells, have been reported to favor the recruitment of monocytes in response to the influenza A virus infection. RANTES may contribute to inflammatory cell infiltration in the airway during viral infection, while IP-10 mediates the inflammatory response by further recruitment of circulating leukocytes into the inflamed tissues [11]. These conclusions have been supported clinically and experimentally, which showed that a number of mediators, including IL-6, IL-10, IP-10, IFN-α, and TNF-α, were significantly elevated in severely infected patients, indicating that these mediators contributed to the increased morbidity in these patients [12]. It has been demonstrated that monoclonal antibody against IP-10 ameliorates the H1N1-induced acute lung injury [13].
In the process of cytokine storm, NFκB is a critical regulator of the immediate early pathogen response, playing an important role in promoting inflammation and viral gene expression [14, 15]. Activation of NF-κB leads to the up-regulation of a variety of anti-viral genes, it is thus commonly regarded as a major regulator of the innate immune defense to infection [16]. We found that Thd had no anti-viral activity in vitro (data no shown), but it could inhibit the expression of viral protein HA in the lungs of mice. However, an uncontrolled immune response may cause more damage to host cells than the replication of the virus would. Thus, the anti-viral efficiency in vivo may be due to the suppression of cytokines/chemokines.
Thd, once withdrawn from the market because of teratogenicity, now has returned with a boom as an anti-cancer and immunomodulatory drug. However, its mode of action in various infections (i.e., pneumonia, tuberculosis, HIV infection, etc.) and related inflammatory conditions has not been well understood yet [17]. In this study, we examined its therapeutic effect on H1N1-induced pneumonia; the results clearly demonstrated that Thd had a potent anti-viral effect against influenza virus, leading to an improved survival rate, attenuation of lung damage, reduction of virus HA titers in the lungs of infected mice, and attenuation of cytokine network after viral infection. However, it remains largely unknown how Thd affects immune cells and whether it affects the acquired immune response and has a protective effect on the other subtypes of influenza virus strains.
Thd has been used in the treatment of pulmonary fibrosis, tumor, and rheumatism because of its potent immunomodulatory properties. Viral pneumonia induced by influenza virus was characteristic of inflammatory cell infiltration in lung tissue. In our study, Thd has been shown to decrease pulmonary inflammation and to suppress specific pathway by blocking the production of the proinflammatory mediators. Modulation of the immune response reduces infection-induced lung pathology, which could be important when new influenza variants arise, particularly prior to the production of new vaccine stocks. Anti-inflammation drug may offer an alternative and complementary tool for the therapy of fatal influenza virus infection.
In summary, Thd has a protective effect on H1N1-infected mice by inhibiting the production of interferons, cytokines and chemokines. The anti-viral activity of Thd is a subsequent effect of anti-inflammation. We envisage that the use of Thd, in combination with anti-viral strategies, may be effective tools against morbidity and mortality induced by seasonal and pandemic strains of influenza A virus.
References
Martinez-Hernandez, F., D.E. Jimenez-Gonzalez, A. Martinez-Flores, G. Villalobos-Castillejos, G. Vaughan, S. Kawa-karasik, A. Flisser, P. Maravilla, and M. Romero-Valdovinos. 2010. What happened after the initial global spread of pandemic human influenza virus a (h1n1)? A population genetics approach. Virology Journal 7: 196.
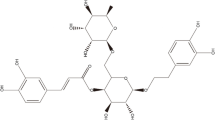
Yang, F., W.L. Zhou, A.L. Liu, H.L. Qin, S.M. Lee, Y.T. Wang, and G.H. Du. 2012. The protective effect of 3-deoxysappanchalcone on in vitro influenza virus-induced apoptosis and inflammation. Planta Medica 78: 968–973.
Julkunen, I., K. Melen, M. Nyqvist, J. Pirhonen, T. Sareneva, and S. Matikainen. 2000. Inflammatory responses in influenza a virus infection. Vaccine 19(suppl 1): s32–s37.
Amirshahrokhi, K. 2013. Anti-inflammatory effect of thalidomide in paraquat-induced pulmonary injury in mice. International Immunopharmacology 17: 210–215.
Martinez-Ocana, J., A. Olivo-diaz, T. Salazar-Dominguez, J. Reyes-Gordillo, C. Tapia-Aquino, F. Martinez-Hernandez, M.E. Manjarrez, M. Antonio-Martinez, A. Contreras-Molina, R. Figueroa-Moreno, R. Valdez-Vazquez, S. Kawa-Karasik, P. Rodriguez-Zulueta, A. Flisser, P. Maravilla, and M. Romero-Valdovinos. 2013. Plasma cytokine levels and cytokine gene polymorphisms in Mexican patients during the influenza pandemic a(H1N1)pdm09. Journal of Clinical Virology 58: 108–113.
Desanctis, J.B., M. Mijares, A. Suarez, R. Compagnone, J. Garmendia, D. Moreno, and M. Salazar-Bookaman. 2010. Pharmacological properties of thalidomide and its analogues. Recent Patents on Inflammation & Allergy Drug Discovery 4: 144–148.
Zhou, S., F. Wang, H. Tze-Chen, J.M. Wu, and E. Wu. 2013. Thalidomide-a notorious sedative to a wonder anticancer drug. Current Medicinal Chemistry 20: 4102–4108.
Wang, J.X., J.Y. Zhou, Q.W. Yang, Y. Chen, X. Li, Y.A. Piao, and H.Y. Li. 2008. An improved embryonated chicken egg model for the evaluation of antiviral drugs against influenza a virus. Journal of Virological Methods 153: 218–222.
Cheung, C.Y., L.L. Poon, A.S. Lau, W. Luk, Y.L. Lau, K.F. Shortridge, S. Gordon, Y. Guan, and J.S. Peiris. 2002. Induction of proinflammatory cytokines in human macrophages by influenza a (h5n1) viruses: a mechanism for the unusual severity of human disease? Lancet 360: 1831–1837.
Humphreys, I.R., G. Walzl, L. Edwards, A. Rae, S. Hill, and T. Hussell. 2003. A critical role for OX40 in T cell-mediated immunopathology during lung viral infection. Journal of Experimental Medicine 198: 1237–1242.
Matsukura, S., F. Kokubu, H. Kubo, T. Tomita, H. Tokunaga, M. Kadokura, T. Yamamoto, Y. Kuroiwa, T. Ohno, H. Suzaki, and M. Adachi. 1998. Expression of RANTES by normal airway epithelial cells after influenza virus A infection. American Journal of Respiratory Cell and Molecular Biology 18: 255–264.
Bradley-Stewart, A., L. Jolly, W. Adamson, R. Gunson, C. Frew-Gillespie, K. Templeton, C. Aitken, W. Carman, S. Cameron, and C. Mcsharry. 2013. Cytokine responses in patients with mild or severe influenza A (H1N1)pdm09. Journal of Clinical Virology 58: 100–107.
Wang, W., P. Yang, Y. Zhong, Z. Zhao, L. Xing, Y. Zhao, Z. Zou, Y. Zhang, C. Li, T. Li, C. Wang, Z. Wang, X. Yu, B. Cao, X. Gao, J.M. Penninger, X. Wang, and C. Jiang. 2013. Monoclonal antibody against CXCL-10/IP-10 ameliorates influenza A (H1N1) virus induced acute lung injury. Cell Research 23: 577–580.
Bernasconi, D., C. Amici, S. La Frazia, A. Ianaro, and M.G. Santoro. 2005. The IkappaB kinase is a key factor in triggering influenza a virus-induced inflammatory cytokine production in airway epithelial cells. Journal of Biological Chemistry 280: 24127–24134.
Flory, E., M. Kunz, C. Scheller, C. Jassoy, R. Stauber, U.R. Rapp, and S. Ludwig. 2000. Influenza virus-induced NF-kappaB-dependent gene expression is mediated by overexpression of viral proteins and involves oxidative radicals and activation of IkappaB kinase. Journal of Biological Chemistry 275: 8307–8314.
Ludwig, S., and O. Planz. 2008. Influenza viruses and the NF-kappaB signaling pathway—towards a novel concept of antiviral therapy. Biological Chemistry 389: 1307–1312.
Kumar, V., and S. Chhibber. 2011. Thalidomide: an old drug with new action. Journal of Chemotherapy 23: 326–334.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant No. 81173173).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhu, H., Shi, X., Ju, D. et al. Anti-Inflammatory Effect of Thalidomide on H1N1 Influenza Virus-Induced Pulmonary Injury in Mice. Inflammation 37, 2091–2098 (2014). https://doi.org/10.1007/s10753-014-9943-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-014-9943-9