Abstract
Salivary, serum matrix metalloproteinase-8 (MMP-8), tissue inhibitor of matrix metalloproteinases-1 (TIMP-1), neutrophil elastase (NE), and myeloperoxidase (MPO) levels were investigated in generalized chronic periodontitis (GCP), generalized aggressive periodontitis (GAgP), and healthy groups. Whole-mouth clinical periodontal measurements were recorded. Salivary, serum concentrations of MMP-8, MPO, TIMP-1, and NE were determined by immunofluorometric assay or ELISA in 18 patients with GCP, 23 patients with GAgP, 18 individuals with healthy periodontium. Patients in the GAgP group were younger than the other groups (p < 0.05). The study groups were similar in gender, smoking status. Plaque index was higher in GCP than GAgP group (p < 0.05). Biochemical data were similar in periodontitis groups. Salivary, serum MPO, and salivary NE concentrations were higher; TIMP-1 concentrations were lower in the periodontitis groups than the controls (p < 0.05). The present data support a close relationship between salivary, serum protease content and clinical periodontal parameters in patients with generalized periodontitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Periodontitis is a multifactorial disease where interplay of microbiologic, genetic, immunologic, and environmental/behavioural risk factors decides the onset, course, and severity. Proteolytic activities related with inflammation participate in collagen degradation observed in periodontitis. Chronic periodontitis (CP) is related to polybacterial infection, and the tissue destruction appears to result from a complex interaction between pathogenic bacteria and the host immune system. Generalized aggressive periodontitis (GAgP) is a rapidly progressive disease that affects otherwise healthy individuals and results in rapid loss of attachment and bone destruction, which may lead to edentulism early in life [1]. Therefore, despite its relatively low prevalence, GAgP has important social implications [2, 3].
Periodontal tissues are infiltrated mainly by neutrophilic granulocytes and polymorphonuclear neutrophils (PMN), which play an important role in the development of inflammatory injury. Matrix metalloproteinases (MMPs) represent a structurally related but genetically distinct superfamily of proteases acting not only in physiological development and tissue remodelling but also in pathological tissue destruction [4]. MMPs can also process bioactive non-matrix substrates such as cytokines, chemokines, growth factors, and immune modulators thereby mediating anti-inflammatory and pro-inflammatory processes [5, 6]. Upon bacterial insult, triggered leukocytes migrate to the site of inflammation and release MMP-8 and MMP-9, which are activated locally [5]. Tissue inhibitors of MMPs (TIMPs) regulate the activities of these enzymes, and TIMP-1 is more effective on interstitial collagenases [7]. An imbalance between MMPs and TIMPs results in the pathological tissue destruction observed in periodontitis [8, 9].
Neutrophil elastase (NE) is one of the most destructive enzymes with the capability of degrading almost all extracellular matrix components as well as plasma proteins and activating proMMPs and inactivating TIMP-1 [5, 10]. A high concentration of NE is stored in azurophilic granules of PMNs, providing an important step in host defence. When activated, NE can be released rapidly into the extracellular space and cause local tissue damage [11]. Endogenous proteinase inhibitors are important to protect tissues from unregulated proteolysis. Conjugating with protease inhibitors rapidly inactivates NE in circulation. Azurophilic granules of PMNs also contain the enzyme myeloperoxidase (MPO) that can generate reactive oxygen species including hypochlorous acid. MPO is released into the extracellular environment following neutrophil stimulation and/or degranulation [12]. MPO can oxidatively activate MMP-8 and MMP-9 and inactivate TIMP-1 [5]. Thus, MPO and NE can potentiate the destructive MMP cascades.
CP and AgP differ in age of onset and prognosis. Despite these differences, the two principal forms of periodontitis cannot be distinguished on the basis of histopathological features [13] or microbiological colonization profiles [14]. AgP has been suggested to be related with a hyper-responsive systemic profile also associated with genetic susceptibility [15]. It is hypothesized that MMPs and neutrophil degranulation products in serum and saliva may differentiate GAgP and GCP from each other and also from clinically healthy periodontium. With this background, the present study is undertaken to comparatively evaluate the serum and saliva concentrations of MMP-8, TIMP-1, NE, and MPO in patient groups of GAgP or GCP as well as healthy controls.
MATERIALS AND METHODS
Study Population
A total of 59 Caucasian individuals from those patients seeking dental treatment at the School of Dentistry, Ege University were included in the present study. Systemically healthy 18 patients with GCP (10 males and 8 females; age range 42 to 61 years), 23 patients with GAgP (10 males and 13 females; age range between 30 and 45 years), and 18 individuals with clinically healthy periodontium (11 males and 7 females; age range 26 to 63 years) were recruited for the study between September 2011 and August 2012. The study was approved by the Ethics Committee of Ege University, School of Medicine and conducted in full accordance with ethical principles, including the World Medical Association’s Declaration of Helsinki, as revised in 2000. The aims and methods of the study were explained, and written informed consent was received from each individual before enrolment in the study. Detailed medical and dental histories were obtained. A standardized questionnaire was used to clarify the smoking status of the individuals, but smokers were not excluded. Patients who smoke ≥10 cigarettes/day for >5 years were classified as current smokers and those who had quit smoking at least 6 months prior to enrolment in the study were regarded as the former smokers [16]. Non-smokers did not have history of smoking at all. Individuals with known medical disorders, such as diabetes mellitus or immunological disorders and those who had received antibiotic or periodontal treatment in the last 6 months were excluded from the study. GCP patients were diagnosed in accordance with the clinical criteria stated in the consensus report of the World Workshop in Periodontitis [17]. The diagnosis of GCP was assigned if the individual had ≥4 teeth in each jaw with a probing depth (PD) of ≥5 mm, clinical attachment level (CAL) of ≥4 mm, and ≥50 % alveolar bone loss at least in two quadrants. The extent and severity of alveolar bone loss was assessed by radiographs. These individuals also had bleeding on probing (BOP) at >80 % of the proximal sites. Individuals were assigned to the GAgP group, if they were otherwise healthy, had at least six permanent teeth, including incisors and/or the first molars, with at least one site with PD and CAL ≥5 mm and six teeth other than the first molars and incisors with similar PD and CAL measurements, familial aggregation (all individuals were asked if they had any family member with current or history of severe periodontal disease) and exhibit rapid destruction of periodontal attachment and bone. Periodontally healthy individuals in the control group had no BOP, no clinical/radiographic sign of alveolar bone loss (i.e., a distance of <3 mm between the cemento-enamel junction (CEJ) and bone crest at >95 % of the proximal tooth sites).
Saliva and Serum Sampling
The method described by Navazesh [18] was used for saliva sampling. Whole saliva samples were obtained simply by expectorating into polypropylene tubes before clinical periodontal measurements or any periodontal intervention and in the morning following an overnight fast during which subjects were requested not to drink (except water) or chew gum. The saliva samples were clarified by centrifugation (800 g) for 10 min at room temperature, and 500 μL amounts were placed in clean polypropylene tubes. Five millilitres of venous blood were taken from the antecubital vein by a standard venipuncture method and serum was separated from blood by centrifugation at 1,500 g for 10 min. All saliva and serum samples were frozen and stored at −40 °C until the sample collection period was completed and thawed immediately before assays.
Determination of Periodontal Status
After collection of biofluid samples, the clinical periodontal parameters including PD, CAL, BOP (+/−), and plaque index (PI) [19] were assessed at six sites/tooth (mesiobuccal, mid-buccal, distobuccal, mesiolingual, mid-lingual, and distolingual locations) excluding the third molars using a periodontal probe (Williams, Hu-Friedy, Chicago, IL, USA). CAL was assessed from the CEJ to the base of the probable pocket. (BOP (deemed positive if it occurred within 15 s after periodontal probing). All measurements were performed by two precalibrated examiners (PG and NN) using a Williams periodontal probe, and serum samples were obtained before initiation of any periodontal intervention. Inter-examiner and intra-examiner calibration was analysed using the Kappa-Cohen test. The initial intra-examiner kappa values were 0.96 (PD) and 0.86 (CAL) for PG and 0.93 (PD) and 0.79 (CAL) for NN. The inter-examiner values were 0.92 (PD) and 0.75 (CAL).
MMP-8 Analysis by Immunofluorometric Assay
MMP-8 levels in the saliva and serum samples were determined by a time-resolved immunofluorometric assay (IFMA) as described previously [20, 21]. The monoclonal MMP-8 specific antibodies 8708 and 8706 (Medix Biochemica Oy Ab, Kauniainen, Finland) were used as a catching and tracer antibody, respectively. The tracer antibody was labelled using europium chelate. The assay buffer contained 20 mM Tris–HCl (pH 7.5), 0.5 M NaCl, 5 mM CaCl2, 50 μM ZnCl2, 0.5 % bovine serum albumin, 0.05 % sodium azide, and 20 mg/L diethyhlenetriaminepentaacetic acid (DTPA). Samples were diluted in assay buffer and incubated for 1 h, followed by incubation for 1 h with the tracer antibody. Enhancement solution was added, and after 5 min, fluorescence was measured using a fluoremeter (1234 Delfia Research Fluoremeter, Wallac, Turku, Finland). The specificity of the monoclonal antibodies [20] against MMP-8 was the same as that of polyclonal MMP-8 antibodies [20–22]. MMP-8 concentrations in biofluid samples were expressed as nanograms per millitres. MMP-8/TIMP-1 ratios were calculated as described previously [21, 22].
TIMP-1, MPO, and NE Analysis by Enzyme-Linked Immunosorbent Assay
TIMP-1 analyses were carried out by enzyme-linked immunosorbent assay (ELISA) as described earlier [23]. TIMP-1 (Duoset ELISA Development Systems, R&D Systems, Minneapolis, USA), MPO (Immunodiagnostic AG, Bensheim, Germany), and NE (Bender MedSystems mbH, Vienna, Austria) concentrations were determined using commercially available ELISA kits. All samples were analysed in duplicate. As stated by the manufacturer, the present TIMP-1 ELISAs detect the active form, pro-form, complexed form, and fragmented form of the studied TIMP-1. The secondary antibody in each kit was conjugated with horseradish peroxidase, and tetramethyl benzidine was used as a substrate [23]. The saliva and serum concentrations of the proteins were expressed as nanograms per millitres.
Statistical Analysis
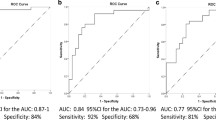
With a power of 80 % and α = 0.05, a minimum number of 17 participants was required for the comparisons. Numerical variables were tested by Shapiro-Wilk test to validate whether they are normally distributed. BOP was evaluated dichotomously as present or absent and then the full-mouth percentage was calculated for each person. PI was recorded in terms of scores at six sites of each tooth present and means and medians were calculated for each person. BOP, PI, PD, and CAL values and biochemical data were compared between the study groups by Kruskal-Wallis test with Dunn’s multiple comparisons test. The distribution of gender and smoking between groups were tested using chi-square test. Possible correlations between the biochemical variables and clinical periodontal measurements were computed by the Spearmen rho rank test. All tests were performed at α = 0.05 significance level. All the statistical calculations were performed using a statistical software package (GraphPad Prism version 6.00c for Mac OS X, GraphPad Software, La Jolla, CA, USA).
RESULTS
Clinical Periodontal Analyses
Demographic characteristics and clinical periodontal measurements are presented in Table 1. The GAgP group was significantly younger than the GCP and control groups (p < 0.0001 and p = 0.0014, respectively). There were no significant differences between the study groups in terms of sex distribution or smoking status. Clinical periodontal measurements were similar in the periodontitis groups, apart from the significantly higher plaque score in the GCP group than the GAgP group (p = 0.015). The control group revealed significantly lower values in all clinical periodontal parameters than the periodontitis groups (p < 0.05).
Biochemical Analyses
The results of biochemical analyses in saliva samples are outlined in Table 2. Salivary concentrations of MPO and NE and the ratio of MMP-8/TIMP-1 were higher, and salivary TIMP-1 concentration was lower in the periodontitis groups than the control group (p = 0.002, p = 0.001, p < 0.001, and p < 0.001, respectively). NE levels were higher in the GAgP and all the other data were higher in the CGP, but none of the differences reached the level of significance (p > 0.05).
The results of biochemical analyses in serum samples are outlined in Table 3. There were no significant differences between the study groups in serum concentrations of MMP-8, TIMP-1, or NE (p > 0.05). The periodontitis groups exhibited higher serum concentrations of MPO than the control group (p < 0.013).
In the GCP group, Spearman correlation analysis revealed significant positive correlations between salivary MMP-8 concentration and PD, PI, and BOP values (p = 0.007, p = 0.005, p = 0.049, respectively) (Table 4). Salivary MPO concentration correlated with PI and BOP values in the GCP group (p = 0.001, p = 0.02, respectively). Serum TIMP-1 concentration correlated with PD in the GCP group (p = 0.046) (Table 4). There were no other significant correlations between biochemical data in serum samples and clinical periodontal measurements.
Salivary MMP-8 concentration correlated with age in the GAgP group (p = 0.01) (Table 5). BOP correlated with salivary MPO concentration (p = 0.042). There were no other significant correlations between salivary biochemical data and clinical periodontal parameters in the GAgP group (p > 0.05). Serum analyses in the GAgP group revealed significant positive correlations between PI and MMP-8 and MPO (p = 0.022 and p = 0.012, respectively) (Table 5). There were no other significant correlations between serum biochemical data and clinical periodontal parameters.
In the healthy control group, there were significant positive correlations between age and salivary MPO concentration (p = 0.033), between PI and salivary NE concentration (p < 0.042) (Table 6). Finally, PI correlated with serum TIMP-1 concentration (p < 0.008) (Table 6).
DISCUSSION
In the present cross-sectional study, serum and saliva concentrations of MMP-8, MPO, NE, and TIMP-1 were analysed in patients with GCP or GAgP and healthy individuals. The two periodontitis groups were very similar in terms of demographic and clinical periodontal parameters apart from the older age and higher plaque scores in the GCP group. None of the biochemical parameters analysed in serum or saliva revealed statistically significant differences between the two periodontitis groups. Several correlations were found between biochemical data and clinical periodontal parameters in the study groups.
MMP-8 is considered to be a key mediator of the irreversible tissue destruction associated with periodontitis [4, 5]. Neutrophils are major cellular sources of MMP-8, and a large and persistent neutrophil influx is a hallmark of inflammatory periodontal diseases [4]. Additionally, MMP-8 expression by several non-PMN-lineage cells found in the periodontium can be induced by pro-inflammatory cytokines such as interleukin-1beta (IL-1β) and tumour necrosis factor-alpha (TNF-α) [20, 24]. Furthermore, specific bacterial proteinases present in microbial dental plaque can activate the PMN-type MMP-8 [4]. Pathogens in microbial dental plaque are capable of stimulating host cells to increase their MMP release, which is considered as one of the indirect mechanisms of tissue destruction seen in periodontitis [25]. Putative pathogens differ in aggressive and chronic periodontitis, which is likely to affect the dominant MMPs acting in each disease entity. Cairo et al. [26] comparatively evaluated serum levels of pro-inflammatory and regulatory cytokines such as ILs and C-reactive protein (CRP) in patients with either AgP or CP and failed to find any significant differences. Wohlfeil et al. [27] also compared serum levels of inflammatory mediators, elastase, and CRP between patients with AgP or CP and reported significantly higher elastase and CRP levels in AgP group. In a pilot study, Duarte et al. [28] compared serum levels of various pro-inflammatory cytokines among GCP, GAgP, and healthy controls. The authors reported significantly higher serum concentration of TNF-α in GAgP than GCP, whereas all other biochemical data were similar. The present findings indicate similar salivary and serum levels of MMP-8 in patients with GAgP and GCP. This finding may be explained by the similarity in clinical parameters of periodontitis in the two periodontitis groups. On the other hand, the literature indicates no consistency in the reported data so far.
Increased MMP-8 expression is associated with remodelling of extracellular matrix components and the basement membrane components, including collagen destruction in the periodontal tissues and other tissues [9, 29–31]. Furthermore, physiological MMP-8 levels have been shown to exert protective and anti-inflammatory properties in alveolar bone loss during periodontal infection by Porphyromonas gingivalis, and MMP-8 deficiency in knockout mice alters the response to serum cholesterol and triglycerides participating to the early development of atherosclerosis [6].
MPO is an antimicrobial enzyme of PMNs released to the extracellular environment following neutrophil stimulation [12]. Recently, data from our group indicated significant increases in serum concentrations of MPO in smoker patients with chronic periodontitis, although the clinical periodontal measurements did not differ from those of the non-smoker counterparts [25]. This increase in serum MPO concentration may be regarded as an indicator of increased risk for local and systemic inflammation such as periodontal tissue destruction or an early sign of atherosclerosis. The salivary MPO and MMP-8 levels were similar in the present study groups; however, Meschiari et al. [32] demonstrated higher salivary MPO activity and MMP-8 levels in patients with periodontitis before the start of non-surgical periodontal treatment. Moreover, Meschiari et al. [32] reported similar serum MPO activity in periodontitis patients and healthy controls. In contrast, the present study revealed higher levels in the periodontitis groups. This discrepancy between the two studies could be attributed to the differences between demographic variables and site characteristics. The present findings do not provide a differentiating serum or saliva concentration for GAgP or GCP.
NE, which is a serine protease, can also accelerate MMP cascades by activating latent proMMPs and inactivating TIMP-1 [5]. NE was suggested to be involved in the degradation of non-collagenous protein-covered collagen fibrils in the early destructive stages of periodontal diseases [32]. Recently, Wohlfeil et al. [33] investigated serum levels of NE in 40 systemically and periodontally healthy individuals comparing males with females. They reported that serum NE correlated positively with PD even in subjects with clinically healthy periodontium and negatively with BOP. The authors reported no significant difference between the study groups (males versus females). In a recent study by our group [25], we compared smoker patients with chronic periodontitis and clinically healthy individuals with non-smoker counterparts, where we found that serum NE concentrations of smoker patients with CP were significantly higher than those of non-smokers. The present GAgP and GCP groups were similar in smoker/non-smoker ratios and also in clinical parameters. These similarities may have resulted in similar serum and saliva NE concentrations.
Significant differences in the investigated biomarker levels between patients with periodontitis and periodontally healthy individuals have been documented in previous studies [34–36]. The present study confirmed the previous findings as the healthy control group revealed significantly lower biochemical data than the two periodontitis groups, but failed to detect a differentiating biomarker for GCP and GAgP, which has become a major debate in recent years.
As a conclusion, the present findings of similar serum and salivary levels of MMP-8, MPO, NE, and TIMP-1 in patients with GCP and GAgP do not provide support for the variation in proteolytic enzyme profile in the two periodontitis types. Further studies are warranted to address microbiological parameters. Other biomarker analyses may also help to better understand the differences between the occurrences of GAgP and GCP.
References
Armitage, G.C. 2004. Periodontal diagnoses and classification of periodontal diseases. Periodontology 2000 34: 9–21.
Albandar, J.M., and E.M. Tinoco. 2002. Global epidemiology of periodontal diseases in children and young persons. Periodontology 2000 29: 153–176.
Demmer, R.T., and P.N. Papapanou. 2010. Epidemiologic patterns of chronic and aggressive periodontitis. Periodontology 2000 53: 28–44.
Sorsa, T., L. Tjaderhane, and T. Salo. 2004. Matrix metalloproteinases (MMPs) in oral diseases. Oral Diseases 10: 311–318.
Sorsa, T., L. Tjaderhane, Y.T. Konttinen, et al. 2006. Matrix metalloproteinases: Contribution to pathogenesis and treatment of periodontal inflammation. Annals of Medicine 38: 306–321.
Kuula, H., T. Salo, E. Pirilä, et al. 2009. Local and systemic responses in matrix metalloproteinase 8-deficient mice during Porphyromonas gingivalis-induced periodontitis. Infection and Immunity 77: 850–859.
Howard, E.W., E.C. Bullen, and M.J. Banda. 1991. Preferential inhibition of 72- and 92-kDa gelatinases by tissue inhibitor of metalloproteinasees-2. Journal of Biological Chemistry 266: 13070–13075.
Aiba, T., N. Akeno, T. Kawane, H. Okamoto, and N. Horiuchi. 1996. Matrix metalloproteinases-1 and -8 and TIMP-1 mRNA levels in normal and diseased human gingivae. European Journal of Oral Sciences 104: 562–569.
Bıyıkoğlu, B., N. Buduneli, L. Kardeşler, K. Aksu, M. Pitkala, and T. Sorsa. 2009. Gingival crevicular fluid matrix metalloproteinase-8, -13 and tissue inhibitor of matrix metalloproteinase-1 levels in rheumatoid arthritis patients with inflammatory periodontal disease. Journal of Periodontology 80: 1307–1316.
Geraghty, P., M.P. Rogan, C.M. Greene, et al. 2007. Neutrophil elastase up-regulates cathepsin B and matrix metalloproteinase-2 expression. Journal of Immunology 178: 5871–5878.
Kawabata, K., T. Hagio, and S. Matsuoka. 2002. The role of neutrophil elastase in acute lung injury. European Journal of Pharmacology 451: 1–10.
Buchmann, R., A. Hasilik, M.E. Nunn, T.E. Van Dyke, and D.E. Lange. 2002. PMN responses in chronic periodontal disease: Evaluation by gingival crevicular fluid enzymes and elastase-alpha-1-proteinase inhibitor complex. Journal of Clinical Periodontology 29: 563–572.
Smith, M., G.J. Seymour, and M.P. Cullinan. 2010. Histopathological features of chronic and aggressive periodontitis. Periodontology 2000 53: 45–54.
Armitage, G.C. 2010. Comparison of the microbiological features of chronic and aggressive periodontitis. Periodontology 2000 53: 70–88.
Nibali, L., M. Parkar, P. Brett, J. Knight, M.S. Tonetti, and G.S. Griffiths. 2006. NADPH oxidase (CYBA) and FcgR polymorphisms as risk factors for aggressive periodontitis: A case–control association study. Journal of Clinical Periodontology 33: 529–539.
Erley, K.J., G.D. Swiec, R. Herold, F.C. Bisch, and M.E. Peacock. 2006. Gingival recession treatment with connective tissue grafts in smokers and non-smokers. Journal of Periodontology 77: 1148–1155.
Armitage, G.C. 1999. Development of a classification system for periodontal diseases and conditions. Annals of Periodontology 4: 1–6.
Navazesh, M. 1993. Methods for collecting saliva. Annals of the New York Academy of Sciences 694: 72–77.
Quigley, G., and J. Hein. 1962. Comparative cleansing efficiency of manual and power brushing. Journal of the American Dental Association 65: 26–29.
Hanemaaijer, R., T. Sorsa, Y.T. Konttinen, et al. 1997. Matrix metalloproteinase-8 is expressed in rheumatoid synovial fibroblasts and endothelial cells. Regulation by tumor necrosis factor-alpha and doxycycline. Journal of Biological Chemistry 272: 31504–31509.
Tuomainen, A.M., K. Nyyssonen, J.A. Laukkanen, et al. 2007. Serum matrix metalloproteinase-8 concentrations are associated with cardiovascular outcome in men. Arteriosclerosis, Thrombosis, and Vascular Biology 27: 2722–2728.
Lauhio, A., T. Salo, Y. Ding, Y.T. Konttinen, D. Nordström, H. Tschesche, J. Lähdevirta, L.M. Golub, and T. Sorsa. 1994. In vivo inhibition of human neutrophil collagenase (MMP-8) activity during long-term combination therapy of doxycycline and non-steroidal anti-inflammatory drugs (NSAID) in acute reactive arthritis. Clinical and Experimental Immunology 98: 21–28.
Rautelin, H.I., A.M. Oksanen, L.I. Veijola, et al. 2009. Enhanced systemic matrix metalloproteinase response in Helicobacter pylori gastritis. Annals of Medicine 41: 208–215.
Cole, A.A., S. Chubinskaya, B. Schumacher, et al. 1996. Chondrocyte matrix metalloproteinase-8. Human articular chondrocytes express neutrophil collagenase. Journal of Biological Chemistry 271: 11023–11026.
Ozcaka, O., N. Bicakci, P. Pussinen, T. Sorsa, T. Kose, and N. Buduneli. 2011. Smoking and matrix metalloproteinases, neutrophil elastase and myeloperoxidase in chronic periodontitis. Oral Diseases 17: 68–76.
Cairo, F., M. Nieri, A.M. Gori, et al. 2010. Markers of systemic inflammation in periodontal patients: Chronic versus aggressive periodontitis. An exploratory cross-sectional study. European Journal of Oral Implantology 3: 147–153.
Wohlfeil, M., S. Scharf, Y. Siegelin, et al. 2012. Increased systemic elastase and C-reactive protein in aggressive periodontitis. Clinical Oral Investigations 16: 1199–1207.
Duarte, P.M., M. da Rocha, E. Sampaio, et al. 2010. Serum levels of cytokines in subjects with generalized chronic and aggressive periodontitis before and after non-surgical periodontal therapy: A pilot study. Journal of Periodontology 81: 1056–1063.
Sorsa, T., P. Mäntylä, H. Rönkä, et al. 1999. Scientific basis of matrix metalloproteinase-8 specific chair-side test for monitoring periodontal and peri-implant health and disease. Annals of the New York Academy of Sciences 878: 130–140.
Said, S., H. Mohd, L. Sander, H. Ronka, T. Sorsa, and D.F. Kinane. 1999. GCF levels of MMP-3 and MMP-8 following placement of bioresorbable membranes. Journal of Clinical Periodontology 26: 757–763.
Meschiari, C.A., A.M. Marcaccini, B.C. Santos Moura, L.R. Zuardi, J.E. Tanus-Santos, and R.F. Gerlach. 2013. Salivary MMPs, TIMPs, and MPO levels in periodontal disease patients and controls. Clinica Chimica Acta 421: 140–146.
Ujiie, Y., S. Oida, K. Gomi, T. Arai, and M. Fukae. 2007. Neutrophil elastase is involved in the initial destruction of human periodontal ligament. Journalof Periodontal Research 42: 325–330.
Wohlfeil, M., J. Wehner, B. Schacher, G.M. Oremek, H. Sauer-Eppel, and P. Eickholz. 2009. Degree of gingivitis correlates to systemic inflammation markers. Clinica Chimica Acta 401: 105–109.
Buduneli, N., S. Vardar, G. Atilla, T. Sorsa, H. Luoto, and H. Baylas. 2002. Ginvival crevicular fluid matrix metalloproteinase-8 levels following adjunctive use of meloxicam and initial phase of periodontal therapy. Journal of Periodontology 73: 103–109.
Rathnayake, N., S. Akerman, B. Klinge, N. Lundegren, H. Jansson, Y. Tryselius, T. Sorsa, and A. Gustafsson. 2013. Salivary biomarkers of oral health—A cross-sectional study. Journal of Clinical Periodontology 40: 140–147.
Gursoy, U.K., E. Könönen, S. Huumonen, T. Tervahartiala, P.J. Pussinen, A.L. Suominen, and T. Sorsa. 2013. Salivary type I collagen degradation end-products and related matrix metalloproteinases in periodontitis. Journal of Clinical Periodontology 40: 18–25.
Source of Funding
This study has been funded solely by the institutions of the authors.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nizam, N., Gümüş, P., Pitkänen, J. et al. Serum and Salivary Matrix Metalloproteinases, Neutrophil Elastase, Myeloperoxidase in Patients with Chronic or Aggressive Periodontitis. Inflammation 37, 1771–1778 (2014). https://doi.org/10.1007/s10753-014-9907-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-014-9907-0