Abstract
Clinical studies have reported associations between MMP-8 genotypes and clinical outcomes without exploring underlying mechanisms. This study aims to understand the influence of the rs1940475 SNP on downstream chemokine and cytokine response in human endotoxemia. Rs1940475 was genotyped in 44 healthy Caucasian males, who were challenged with an intravenous bolus of 2 ng/kg lipopolysaccharide (LPS). Plasma levels of tumor necrosis factor (TNF), interleukin (IL)-6, IL-8, and macrophage inflammatory protein (MIP)-1α were measured at baseline and 2, 4, 6, and 24 h after LPS infusion with high-sensitivity enzyme immunoassays. Peak TNF levels at 2 h after LPS infusion were significantly higher in subjects with AA genotype compared to subjects with AG or GG genotypes (185 pg/mL [IQR, 154–234] vs. 94 pg/mL [IQR, 65–125] vs. 107 pg/mL [IQR, 80–241], respectively; p = 0.03 between groups). Peak IL-6 levels were trend-wise higher in subjects with AA genotype compared to those with AG or GG genotypes (566 pg/mL [IQR, 294–644] vs. 278 pg/mL [IQR, 184–539] and 329 pg/mL [IQR, 240–492], respectively; p = 0.15 between groups). In contrast, peak MIP-1α at 2 h was highest in GG genotype carriers compared to those with AG or AA genotypes (602 pg/mL [IQR, 449–727] vs. 389 pg/mL [IQR, 375–490] and 510 pg/mL [425–813], respectively; p < 0.03 between groups). AA genotype carriers had highest peak TNF and IL-6 levels after LPS challenge, whereas peak MIP-1α levels were highest in GG carriers. This indicates that the rs1940475 SNP modifies the host response to inflammatory stimuli, which may in part explain previously shown associations with clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Neutrophils (PMN) are crucial for clearing microbial pathogens [1]. Among many other proteins, PMNs produce matrix metalloproteinase (MMP)-8, a neutrophil collagenase, which is pivotal for initiation and consequent resolution of inflammation, presumably by altering chemotactic gradients [1]. In general, a lack of MMP-8 has been associated with increased neutrophil counts at inflammatory sites [2, 3].
Macrophage inflammatory protein (MIP)-1 α, also known as chemokine ligand 3 (CCL3), is a potent pro-inflammatory chemokine that is produced by macrophages in response to various stimuli including endotoxin. CCL3 propagates inflammation by further recruitment and activation of PMNs. Data from different experimental models, including a murine acute lung injury model, suggest that soluble as well as membrane bound MMP-8 degrades MIP-1α and therefore mitigates inflammation, resulting in improved survival [4]. In turn, genetically deleting MIP 1-α in MMP-8 knockout mice also reduced lung inflammation and mortality, thus suggesting an important role for an “MMP-8/MIP-1α axis” in acute inflammation [4].
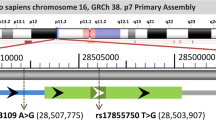
Human studies to date have largely reported associations between MMP-8 plasma levels or MMP-8 genotypes and clinical outcomes, without exploring underlying mechanisms [5–7]. For example, preliminary analysis of the GenIMS study showed that the MMP-8 non-synonymous single-nucleotide polymorphism (SNP) rs1940475 was associated with 90-day mortality in patients with community-acquired pneumonia (CAP), and the presence of the A allele was associated with better survival [8]. The rs1940475 SNP causes a point mutation in the pro-domain of MMP-8. This results in an amino acid substitution of glutamic acid for lysine at position 87, thereby rendering it less amenable to activation, which results in functional suppression [9]. As such, its ability to function as a negative feedback regulator in inflammation is impaired, leading to an over-recruitment of PMNs which may lead to tissue and organ damage.
To better understand the role of MMP-8 in human inflammation, we investigated the influence of the rs1940475 SNP (K87E) on downstream chemokine and cytokine processing in human endotoxemia. The human endotoxemia model is a well-established model, in which a defined inflammatory stimulus allows to study the pathogenesis and potential treatments for systemic inflammation [10]. We hypothesized that subjects homozygous for the allele (A) would have lower peak MIP-1α levels compared to subjects with mutated alleles (G).
MATERIALS AND METHODS
Study Participants
The Medical University of Vienna Ethics Committee approved the study protocol, and all participants gave written informed consent prior to enrolment. We obtained complete data and mRNA samples from 44 healthy Caucasian males. Determination of health status included a medical history, physical examination, laboratory testing, and virus and standard drug screening. Exclusion criteria were regular or recent intake of medications, including over-the-counter medications as well as clinically relevant abnormal findings detected in the screening examinations.
The experimental procedures of our LPS infusion studies have been described in detail elsewhere [11]. Briefly, volunteers reported to the study ward at 8:00 a.m. after an overnight fast and received an intravenous bolus of 2 ng/kg LPS (National Reference Endotoxin, Escherichia coli, CC-RE-Lot 2; National Institutes of Health, Bethesda, MD, USA). Throughout the entire study period, participants were confined to bed rest, and vital parameters, i.e., electrocardiogram (ECG), heart rate, oxygen saturation, and blood pressure were continuously monitored.
MMP-8 Genotype Analysis
Based on our preliminary findings in patients with CAP, [8] we selected the non-synonymous SNP 259A > G (rs1940475 in the National Center for Biotechnology Single Nucleotide Polymorphism database, http://www.ncbi.nlm.nih.gov/SNP) for analysis. All blood samples were immediately processed to avoid storage-induced changes in mRNA levels. After isolating total RNA with an RNeasy minikit (Qiagen, Valencia, CA, USA), mRNA was directly transcribed into cDNA, using a TaqMan reverse transcription reagents kit (Applied Biosystems, Foster City, CA, USA), and stored at −80 °C until analysis. Consequently, cDNA samples were genotyped on an ABI 7700 Prism using a commercially available SNP assay (TaqMan MMP-8 assay, Applied Biosystems) and analyzed with Sequence Detection System software (Ver. 1.7, Applied Biosystems).
Blood Sampling and Analysis
Blood samples were collected into ethylenediaminetetraacetic acid (EDTA) anti-coagulated tubes before LPS infusion and 2, 4, 6, and 24 h after LPS infusion. All samples were immediately centrifuged at 2,000 × g at 4 °C for 15 min and then stored at −80 °C until batch analysis.
Plasma levels of tumor necrosis factor (TNF), interleukin (IL)-6, IL-8, and MIP-1α were analyzed with high-sensitivity enzyme immunoassays (all R&D-Systems, Oxon, UK) [12]. Plasma concentrations of thrombin-anti-thrombin complexes (TAT) and fibrin split products (F1 + 2) were measured with immunoassays (Enzygnost TAT micro and Enzygnost F1 + 2 micro, both Dade Behring, Marburg, Germany) as described previously [13–15].
Differential blood counts were measured with an automatic cell counter (Sysmex, Milton Keynes, UK) [16].
Data Analysis
Data are expressed as medians and inter-quartile ranges (IQR). After repeated measures ANOVA, we applied nonparametric statistics for robustness. We used the Kruskal–Wallis ANOVA for all statistical comparisons between groups, and the Mann–Whitney U test for individual comparisons. Based on a study by Kumpf et al., [17] we estimated a sample size of 40 sufficient to demonstrate 40 % different peak MIP-1a levels between subjects homozygous for the A and G alleles, respectively. A p value of <0.05 was considered statistically significant. All statistical calculations were performed with statistical software (Stata 12.1, College Station, TX, USA).
RESULTS
MMP-8 Genotype Distribution and Subject Characteristics
Of the 44 subjects genotyped, 9 (20.5 %) had the AA genotype, 9 (20.5 %) had the GG genotype, and the remaining 26 (59 %) had the AG genotype and thus were in Hardy–Weinberg equilibrium (p = 0.23). All participating subjects were healthy male nonsmokers, with a median age of 25.5 years (IQR, 23 to 30 years) and a median BMI of 23.4 kg/m2 (IQR, 21.8 to 24.2 kg/m2), without any differences between different genotype carriers (Table 1).
Vital Parameters
LPS infusion induced a transient increase in heart rate and a transient decrease in mean arterial blood pressure (MAP; all p < 0.05 versus time), as previously described in this model [11]. Interestingly, subjects homozygous for the A allele showed the largest decrease in MAP at 4 h compared to the other groups (69, 79, and 81 mmHg, respectively, p = 0.04). LPS infusion also induced a transient increase in body temperature that reached its maximum after 4 h. Subjects homozygous for the A allele had the largest increase in body temperature (37.8 vs. 37.3 °C and 37.3 °C, p = 0.02)
MMP-8 Genotypes and Plasma Cytokine and Chemokine Levels
LPS infusion transiently increased plasma concentrations of TNF, IL-6, IL-8, and MIP-1α (all p < 0.05 vs. time), which returned to baseline after 24 h.
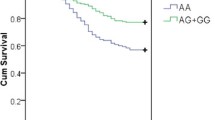
Plasma TNF levels peaked 2 h after LPS infusion (106 pg/mL; IQR, 75–210 pg/mL). Subjects homozygous for the A allele had significantly higher peak values compared to those with GG or AG genotypes (185 pg/mL [IQR, 154–234] vs. 107 pg/mL [IQR, 80–241] and 94 pg/mL [IQR, 65–125, respectively; p = 0.03). The remaining time course did not differ between genotypes (Fig. 1).
Peak IL-6 values were observed 2 h after LPS infusion (329 pg/mL; IQR, 216 to 541 pg/mL]. Subjects homozygous for the A allele had trend-wise higher peak values compared to those with GG or AG genotypes (566 pg/mL [IQR, 294–644] vs. 329 pg/mL [IQR, 240–492] and 278 pg/mL [IQR, 184–593], p = 0.15; Fig. 1).
Baseline MIP-1α levels did not differ between the three genotypes (Table 1). Peak MIP-1α plasma levels were measured 2 h after LPS infusion (439 pg/mL; IQR, 376–614). In contrast to TNF and IL-6 values, subjects homozygous for the mutant G allele had the highest peak levels compared to subjects with AA or AG genotypes (602 pg/mL [IQR, 449–727] vs. 510 pg/mL [IQR, 425–813] and 389 pg/mL [IQR, 375–490], p = 0.03). The remaining time course was similar between genotypes (Fig. 1). Peak IL-8 values were detectable 2 h after LPS infusion (222 pg/mL; IQR, 167–486) but did not differ between genotypes.
MMP-8 Genotypes and Coagulation Activation
As expected, [13] LPS infusion was associated with a potent activation of the coagulation system as reflected by increases in the plasma concentrations of thrombin–anti-thrombin complexes and prothrombin fragments F1+2, both peaking after 4 h (54.5 pmol/L [IQR, 28.2–111.8] and 1,130 μg/L [IQR, 668–1,918], respectively, both p < 0.05 vs. time). This LPS-induced coagulant response did not differ between different genotypes.
MMP-8 Genotypes and Neutrophil Counts
As expected, neutrophil counts increased about threefold compared to baseline levels (p < 0.05 vs. time) after LPS infusion. Nadir levels were reached 1.5 h after LPS infusion (2.0 G/L [IQR, 1.7–3.4]), whereas peak levels were observed 6 h after LPS infusion (9.2 G/L [IQR, 8.2–11.8]). Subjects homozygous for the A allele displayed a lesser drop in neutrophils at 1.5 h compared to subjects with AG or GG genotypes (3.7 G/L [IQR, 2.3–4.6] vs. 1.9 G/L [IQR, 1.6–2.7] and 1.8 G/L [IQR, 1.4–3.3], p = 0.07 between groups). Similarly, subjects with the AA genotype had trend-wise higher peak neutrophil levels at 6 h compared to AG and GG individuals, respectively (12.2 G/L [IQR, 8.6–12.7] vs. 9.1 G/L [IQR, 7.2–11.1] and 9.2 G/L [IQR, 8.3–11.6]); p = 0.09 between groups).
DISCUSSION
Data from MMP-8 knockout animals suggest that MMP-8 assists in early PMN recruitment and elimination of chemotactic gradients. For example, acute lung inflammation (ALI) is less pronounced in MMP-8 wild-type mice compared to knockout mice due to inactivation MIP 1-α [4]. Compared to knockout animals, MMP-8 wild-type (WT) mice had higher levels of PMN membrane bound MMP, which is likely to be the key bioactive form of the enzyme. In turn, MMP-8 inactivated MIP 1-α, and genetically deleting MIP 1-α in MMP-8 knockout mice decreased the increased lung inflammation and mortality, thus emphasizing a possible role for a “MMP-8/MIP-1α axis” in acute inflammation.
Our understanding of MMP-8 in human inflammation and infection is less clear, in part due to the fact that we cannot selectively silence the MMP-8 gene. Studies to date have largely reported associations between MMP-8 plasma levels and/or MMP-8 genotypes and clinical outcomes without elaborating the underlying mechanisms. Most of these studies report a similar trend, i.e., higher MMP-8 levels are associated with worse clinical disease. For instance, MMP-8 is not only strongly associated with acute inflammatory states in humans such as ARDS [18] but also states with chronic inflammation and neutrophilia such as cystic fibrosis, rheumatoid arthritis, periodontal, and chronic skin diseases [19–22]. For example, MMP-8 levels correlated well with C-reactive protein (CRP) levels in a study of patients with ARDS [23]. Alternatively, several functional MMP-8 single-nucleotide polymorphisms (SNPs) have been linked to clinical outcomes as well. For instance, our preliminary analysis from the GenIMS study showed that the rs1940475 genotype was associated with 90-day mortality in patients with CAP, and patients homozygous for the A allele had the best outcomes [8].
In this study, we show that subjects with the A allele had higher peak TNF and IL-6 levels after LPS challenge than those homozygous for the G allele, whereas MIP-1 α levels were higher in subjects homozygous for the G allele. In addition, subjects with the A allele also showed a stronger clinical response to LPS infusion in terms of drop in MAP and increase in body temperature. As clinical studies have shown a higher pro-inflammatory response to be associated with poorer survival [24], our findings of higher peak TNF and IL-6 levels in AA homozygous individuals are not consistent with higher survival rates in our preliminary analysis of AA homozygous individuals with CAP [8]. Conversely, patients homozygous for the G allele had the highest peak MIP-1 alpha levels. MIP-1α usually parallels TNF and IL-6 response in a TNF independent way [25]. Bronchoalveolar fluid levels of MIP-1 α were inversely correlated with lung compliance in a small human cohort of ARDS patients but not associated with outcomes. These preliminary findings warrant further study in larger cohorts.
Our study has several limitations. First, although we calculated a sample size of 40 to be sufficient to detect a 40 % difference in peak MIP-1α levels between AA and GG genotypes, our study was not adequately powered to assess any differences beyond that; hence, all additional analyses must be viewed as exploratory. Second, while our results suggest an association between peak plasma cytokine levels and MMP-8 genotypes and thus a role for MMP-8 in cytokine regulation, we do not have insight how this affects downstream cell trafficking to actual sites of infection. Hence, additional studies using alternative compartmental models such as inhaled LPS will be helpful to better understand the role of MMP-8 in ALI and pneumonia. Third, we did not measure MMP-8 levels in our healthy volunteers. Fourth, our study was conducted in healthy male volunteers, and thus, our results may not apply to females. Currently, the exact link between MMP-8 genotypes and plasma levels/activity levels is not well understood. While some studies report a clear dose–response relationship between MMP-8 genotypes and activity levels, we failed to show a significant association in ex vivo incubation experiments (unpublished data). However, our preliminary data suggest that the rs1940475 SNP results in a conformational change of the active site, which makes the enzyme less amenable to activation [9]. This needs to be verified in further studies.
In conclusion, subjects homozygous for the ancestral A allele had a stronger pro-inflammatory response to LPS compared to other genotypes, whereas peak MIP-1α levels were highest in subjects homozygous for the G allele. These findings indicate that the rs1940475 SNP modifies the host response to inflammatory stimuli, which may in part explain previously shown associations with clinical outcomes.
References
Tester, A.M., J.H. Cox, A.R. Connor, et al. 2007. LPS responsiveness and neutrophil chemotaxis in vivo require PMN MMP-8 activity. PLoS One 2: e312.
Owen, C.A., Z. Hu, C. Lopez-Otin, and S.D. Shapiro. 2004. Membrane-bound matrix metalloproteinase-8 on activated polymorphonuclear cells is a potent, tissue inhibitor of metalloproteinase-resistant collagenase and serpinase. Journal of Immunology 172: 7791–7803.
Balbin, M., A. Fueyo, A.M. Tester, et al. 2003. Loss of collagenase-2 confers increased skin tumor susceptibility to male mice. Nature Genetics 35: 252–257.
Quintero, P.A., M.D. Knolle, L.F. Cala, Y. Zhuang, and C.A. Owen. 2010. Matrix metalloproteinase-8 inactivates macrophage inflammatory protein-1 alpha to reduce acute lung inflammation and injury in mice. Journal of Immunology 184: 1575–1588.
Kader, A.K., L. Shao, C.P. Dinney, et al. 2006. Matrix metalloproteinase polymorphisms and bladder cancer risk. Cancer Research 66: 11644–11648.
Decock, J., W. Hendrickx, U. Vanleeuw, et al. 2008. Plasma MMP1 and MMP8 expression in breast cancer: protective role of MMP8 against lymph node metastasis. BMC Cancer 8: 77.
Wang, H., S. Parry, G. Macones, et al. 2004. Functionally significant SNP MMP8 promoter haplotypes and preterm premature rupture of membranes (PPROM). Human Molecular Genetics 13: 2659–2669.
Rella JM, Kaynar AM, Yende S, et al. Matrix Metalloproteinase (MMP)-8 polymorphism is associated with mortality in patients with community-acquired pneumonia (CAP). Intensive Care Med. 2009:90.
McLaughlin J, Rella J, Bakan A, et al. Impact of pro-domain stability of matrix metalloproteinase-8 on the outcome of sepsis. Crit Care 2011:P278.
Pernerstorfer, T., R. Schmid, C. Bieglmayer, H.G. Eichler, S. Kapiotis, and B. Jilma. 1999. Acetaminophen has greater antipyretic efficacy than aspirin in endotoxemia: a randomized, double-blind, placebo-controlled trial. Clinical pharmacology and therapeutics. 66: 51–57.
Mayr, F.B., A. Spiel, J. Leitner, et al. 2005. Effects of carbon monoxide inhalation during experimental endotoxemia in humans. American Journal of Respiratory and Critical Care Medicine 171: 354–360.
Derhaschnig, U., D. Bergmair, C. Marsik, I. Schlifke, J. Wijdenes, and B. Jilma. 2004. Effect of interleukin-6 blockade on tissue factor-induced coagulation in human endotoxemia. Critical Care Medicine 32: 1136–1140.
Mayr, F.B., A.O. Spiel, J.M. Leitner, et al. 2009. Racial differences in endotoxin-induced tissue factor-triggered coagulation. Journal of Thrombosis and Haemostasis 7: 634–640.
Mayr, F.B., A.O. Spiel, J.M. Leitner, et al. 2008. Duffy antigen modifies the chemokine response in human endotoxemia. Critical Care Medicine 36: 159–165.
Leitner, J.M., C. Firbas, F.B. Mayr, R.A. Reiter, B. Steinlechner, and B. Jilma. 2006. Recombinant human antithrombin inhibits thrombin formation and interleukin 6 release in human endotoxemia. Clinical pharmacology and therapeutics. 79: 23–34.
Ruzicka, K., M. Veitl, R. Thalhammer-Scherrer, and I. Schwarzinger. 2001. The new hematology analyzer Sysmex XE-2100: performance evaluation of a novel white blood cell differential technology. Archives of Pathology & Laboratory Medicine 125: 391–396.
Kumpf, O., E.J. Giamarellos-Bourboulis, A. Koch, et al. 2010. Influence of genetic variations in TLR4 and TIRAP/Mal on the course of sepsis and pneumonia and cytokine release: an observational study in three cohorts. Critical Care 14: R103.
Fligiel, S.E., T. Standiford, H.M. Fligiel, et al. 2006. Matrix metalloproteinases and matrix metalloproteinase inhibitors in acute lung injury. Human pathology. 37: 422–430.
Ratjen, F., C.M. Hartog, K. Paul, J. Wermelt, and J. Braun. 2002. Matrix metalloproteases in BAL fluid of patients with cystic fibrosis and their modulation by treatment with dornase alpha. Thorax 57: 930–934.
Hanemaaijer, R., T. Sorsa, Y.T. Konttinen, et al. 1997. Matrix metalloproteinase-8 is expressed in rheumatoid synovial fibroblasts and endothelial cells. Regulation by tumor necrosis factor-alpha and doxycycline. The Journal of biological chemistry. 272: 31504–31509.
Maatta, M., O. Kari, T. Tervahartiala, et al. 2008. Elevated expression and activation of matrix metalloproteinase 8 in tear fluid in atopic blepharoconjunctivitis. Cornea 27: 297–301.
Nwomeh, B.C., H.X. Liang, I.K. Cohen, and D.R. Yager. 1999. MMP-8 is the predominant collagenase in healing wounds and nonhealing ulcers. The Journal of surgical research. 81: 189–195.
Schaaf, B., C. Liebau, V. Kurowski, D. Droemann, and K. Dalhoff. 2008. Hospital acquired pneumonia with high-risk bacteria is associated with increased pulmonary matrix metalloproteinase activity. BMC pulmonary medicine. 8: 12.
Kellum, J.A., L. Kong, M.P. Fink, et al. 2007. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Archives of internal medicine. 167: 1655–1663.
O’Grady, N.P., M. Tropea, H.L. Preas 2nd, et al. 1999. Detection of macrophage inflammatory protein (MIP)-1alpha and MIP-1beta during experimental endotoxemia and human sepsis. Journal of Infectious Diseases 179: 136–141.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rella, J.M., Jilma, B., Fabry, A. et al. MMP-8 Genotypes Influence the Inflammatory Response in Human Endotoxemia. Inflammation 37, 451–456 (2014). https://doi.org/10.1007/s10753-013-9758-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-013-9758-0