Abstract
It is well established that a high-fat diet (HFD) can lead to overweight and ultimately to obesity, as well as promoting low-grade chronic inflammation associated with increased levels of such mediators as TNF-α, IL-1, and IL-6. Bone marrow mesenchymal stem cells (MSCs), which are involved in hematopoietic niches and microenvironments, can be affected by these cytokines, resulting in induction of NF-κB and inhibition of PPAR-γ. Because this phenomenon could ultimately lead to suppression of bone marrow adipogenesis, we set out to investigate the effect of an HFD on the expression of PPAR-γ and NF-κB, as well as the production of IL-1, IL-6, and TNF-α in MSCs. Two-month-old male Wistar rats were fed a HFD diet and evaluated by means of leukograms and myelograms along with blood total cholesterol, triglyceride, and C-reactive protein levels. MSCs were isolated, and PPAR-γ and NF-κB were quantified, as well as IL-1, IL-6, and TNF-α production. Animals that were fed a HFD showed higher levels of blood total cholesterol, triglycerides, and C-reactive protein with leukocytosis and bone marrow hyperplasia. MSCs from HFD animals showed increased production of IL-1, IL-6, and TNF-α and increased NF-κB and reduced PPAR-γ expression. Therefore, ingestion of an HFD induces alterations in MSCs that may influence modulation of hematopoiesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
It is well established that the excessive consumption of a high-fat diet (HFD) leads to overweight and ultimately to obesity, as well as promoting low-grade chronic inflammation, which is deeply tied to the pathogenesis of metabolic syndrome and other chronic diseases [1, 2]. Low-grade inflammatory states are commonly associated with increased levels of certain biomarkers, mainly pro-inflammatory cytokines, such as TNF-α, IL-1, and IL-6, which can have direct or indirect effects on hematopoiesis [1, 3–5].
Hematopoiesis is a complex process that leads to the continuous production of blood cells and is highly regulated and influenced by various stimuli. The production of these cells depends on the hematopoietic stem cell and a bone marrow microenvironment that is suitable for survival, proliferation, and differentiation to occur in an organized manner [6, 7].
The bone marrow microenvironment is formed mainly by mesenchymal stem cells (MSCs), which can support hematopoiesis and differentiate along multiple mesenchymal lineages, such as osteoblasts, adipocytes, and chondrocytes. MSCs express transcription factors that regulate this process of differentiation, including osteogenic factors, such as RUNX2 and osterix, adipogenic factors, such as CCAAT-enhancer-binding protein α and proliferator-activated receptor γ (PPARγ), and the chondrogenic factor SOX-9 [8]. RUNX2 represses adipogenesis, while PPARγ both downregulates RUNX2 expression and also binds to the RUNX2 protein to inhibit transactivation of osteogenic promoters [9, 10].
MSCs are involved in stabilizing microenvironments and forming niches for hematopoietic cells, while osteoblastic cells within the endosteal region play a role in controlling the number of hematopoietic stem cells [11–13]. Adipocytes, conversely, suppress hematopoiesis under homeostatic conditions and particularly under stressed conditions [14]. It should be noted that while pro-inflammatory cytokines, such as IL-1, IL-6, and TNF-α, usually inhibit bone marrow adipogenesis, when bone marrow adipocytes act as negative regulators of the hematopoietic microenviroment, these cytokines can, in fact, act as inducers of hematopoiesis in the bone marrow microenvironment [14–16]. Suppression of adipogenesis is mediated by the inhibition of the transcription factor PPAR-γ, which is a key inducer of adipogenesis. Additionally, other intracellular signal transducers can be activated, including NF-κB, which is also able to suppress the function of PPARγ effectively [16, 17].
NF-κB is a key component of inducible expression pathways and may play a role in stem cell cytokine production. Inhibition of PPAR-γ induces NF-κB and promotes inflammatory responses by enhancing the transcription of various inflammatory cytokines, adhesion molecules, and chemokines [18, 19]. Our aims in this study were to examine the role of NF-κB and PPAR-γ in MSCs from an obese rat model and to assess the capability of these cells to produce IL-1, IL-6, and TNF-α.
MATERIALS AND METHODS
Animals and Treatments
Two-month-old male Wistar rats (initial weight, 298 ± 27 g) were obtained from the Faculty of Pharmaceutical Sciences at the University of São Paulo. Rats were placed in plastic cages (two to three rats per cage) in an atmosphere of 55 ± 10 % relative humidity at 22 ± 2 °C with a 12-h light/dark cycle. Rats were given free access to food and water. Body mass and dietary intake were recorded three times a week. The study was approved by the Ethics Committee on Animal Experimentation of the Faculty of Pharmaceutical Sciences at the University of São Paulo according to the guidelines of the Brazilian College on Animal Experimentation.
After acclimatization for 10 days with a semipurified diet based on the American Institute of Nutrition’s recommendations for the adult rodent (AIN-93M) [20], rats were randomly assigned into two groups: the HFD group and the control (CON) group. For 12 weeks, the CON group (n = 8) received the AIN-93M diet (total energy: 75.8 % carbohydrates, 9.3 % fat, and 14.9 % protein), while the HFD group (n = 8) received an AIN-93M-based diet that was enriched with lard (total energy: 24.2 % carbohydrates, 60.9 % fat, and 14.9 % protein). A pilot study determined that rats from the HFD group consumed approximately 30 % less food than rats from the CON group. However, given the higher energy density of the HFD (5.55 kcal/g) compared to the CON diet (3.99 kcal/g), the daily energy intake did not differ between the groups. Insufficient intake of micro- and macronutrients by the HFD group rats, which was caused by the lower consumption rate, could significantly affect the outcomes of the study. Therefore, to ensure comparable intakes of micro- and macronutrients between the groups, diet ingredients (except for starch and lard) were normalized according to their energy densities, as shown in Table 1. Additionally, because HFD feed is highly susceptible to oxidation, its tert-butylhydroquinone content was increased [21].
Blood and Adipose Tissue Mass
Animals were anesthetized with xylazine chlorohydrate (Rompum®, 10 mg/kg, Bayer S.A., São Paulo, SP, Brazil) and ketamine chlorhydrate (Ketamina®, 100 mg/kg, Cristália Ltda., Itapira, SP, Brazil), and whole blood samples were collected in tubes with or without the anticoagulant ethylenediaminetetraacetic acid (EDTA, 1 mg/mL, Sigma Chemical Company, St. Louis, MO, USA). Blood samples collected with EDTA were used to perform a leukogram (Horiba ABX Diagnostics, Montpellier, France). Differential leukocyte counts were performed on blood smears stained with the standard May–Grunwald and Giemsa solutions (Sigma Chemical Co., St. Louis, MO, USA) [22]. Samples collected without anticoagulant were separated, and total cholesterol and triglyceride levels were quantified using standard methods. Quantification of the leptin and C-reactive protein levels in the serum was performed by the Luminex-based bead array method LINCOplex simultaneous multi-analyte detection system (Linco Research Inc., St. Charles, MO, USA) according to the manufacturer’s instructions. After euthanasia, adipose tissue was collected, and the periepididymal and retroperitoneal fat pads were isolated and weighed.
Bone Marrow Cellularity and Mesenchymal Stem Cell Isolation
Femurs were removed under aseptic conditions, and bone marrow cells were flushed using Dulbecco’s Modified Eagle’s Medium (DMEM) (Vitrocell, Campinas, SP, Brazil) supplemented with 10 % fetal calf serum (Vitrocell, Campinas, SP, Brazil). Cells were washed by adding complete media, centrifuging for 5 min at 300 rpm at 24 °C, and removing the supernatant.
Myelogram counts were performed by counting cells using a Neubauer chamber (Herka, Berlin, Germany), and differential cell counts were performed on smears stained with the standard May–Grünwald–Giemsa solutions (Sigma Chemical Company, St. Louis, MO, USA).
The bone marrow cell pellet was resuspended and cultured in 75-cm2 culture flasks with complete media at 37 °C with 5 % CO2 in air. MSCs preferentially attached to the polystyrene surface. After 48 h, non-adherent cells in suspension were discarded. Fresh complete media was added and replaced every 3 or 4 days thereafter. Cells were confirmed to be MSCs by checking for cell surface markers CD 271+, CD34−, CD45−, and CD90+. Cultures were passaged when they reached 90 % confluency by detaching them with 0.25 % trypsin–EDTA (GIBCO Invitrogen, Carlsbad, CA) and replating them in culture flasks. Cells were utilized for experimentation between passages 3 and 4.
Bone Marrow Mesenchymal Stem Cell Culture and IL-1, IL-6, and TNF-α Quantification
MSCs were isolated as described above and cells at passage 3 were cultured in DMEM medium (Vitrocell, Campinas, SP, Brazil) supplemented with 10 % fetal calf serum at a concentration of 1 × 106 cells/mL. These cells were incubated at 37 °C in a humidified atmosphere of 5 % CO2 for 24 h. Supernatants were subsequently collected for IL-1, IL-6, and TNF-α quantification, which was performed using the Luminex-based bead array method LINCOplex simultaneous multi-analyte detection system (Linco Research Inc., St. Charles, MO, USA) according to the manufacturer’s instructions. The entire procedure was executed under aseptic conditions, and all of the materials were previously sterilized and were pyrogen-free.
Western Blot Analysis
To determine the protein levels of PPAR-γ, NF-κB, and RUNX2, MSCs were isolated and washed three times with sterile, cold PBS and were lysed with RIPA buffer (0.1 % SDS, 1 % Igepal CA-630, 1 % sodium deoxycholate, 10 mM Tris-HCL, pH 7.5, 150 mM NaCl, and 0.5 mM EDTA) in the presence of a protease and phosphatase inhibitor cocktail (Sigma-Aldrich Corp., St. Louis, MO, USA). After centrifugation at 14,000 rpm and 4 °C for 15 min, the supernatant was collected, mixed with 5X Laemmli buffer (1 M Tris-HCl, pH 6.8, 10 % 2-mercaptoethanol, 10 % SDS, 50 % glycerol, and 0.01 % bromophenol blue) and boiled for 5 min. The protein content of cell homogenates was determined using a BCA Protein Assay kit (Pierce Biotechnology, Inc., Rockford, IL, USA), and equal amounts of protein (30 μg per well) were separated on 7.5 % SDS-polyacrylamide mini gels and transferred to Immobilon polyvinylidene difluoride membranes (Millipore Corporation, Billerica, MA, USA). After overnight incubation with the appropriate primary antibodies (1:1,000), including PPAR-γ (cat no. sc7196, Santa Cruz Biotechnology, Santa Cruz, CA, USA), NF-κB p65 (cat no. 146751, eBioscince, San Diego, CA, USA.), phosphorylated NF-κB (cat no. sc33039, Santa Cruz Biotechnology, Santa Cruz, CA, USA), and RUNX2 (cat no. Ab81357-100, Abcam Inc, MA, USA), the membranes were washed three times and incubated for 1 h with a secondary antibody conjugated to horseradish peroxidase (cat no. DC03L, Calbiochem, San Diego, CA, USA). After three washes with TBST, the immunoreactive bands were visualized using the ECL detection system (Amersham ECL™ Advance Western Blotting Detection Kit, Piscataway, NJ, USA). To standardize and quantify the immunoblots, a digital detection system (IMAGE QUANTTM 400 version 1.0.0, Amersham Biosciences, Pittsburgh, PA, USA) was used. The results were expressed in relation to the intensity of β-actin (1:40,000 for anti-β-actin, Cell Signaling Technology, Inc., Beverly, MA, USA) and as a percentage of the control value.
Statistics
Dependent variables were normally distributed. Results were subjected to statistical analysis (Student’s t test) using the computer software GraphPad Prism® (GraphPad Prism version 5.03 for Windows; GraphPad Software, San Diego, CA, USA), and data are expressed as the mean values with their standard deviations. Differences were considered statistically significant when the p value was ≤0.05.
RESULTS
Diet, Body Weight, Periepididymal and Retroperitoneal Adipose Tissue Mass, Serum Cholesterol, Triglycerides, Leptin, and C-Reactive Protein Quantification; Leukogram; and Myelogram
Rats maintained on the HFD reduced their food consumption up to 30 % but had a significant increase in lipid consumption, which resulted in increased body weight and a significant increase in the periepididymal and retroperitoneal adipose tissue mass. Blood total cholesterol, triglyceride, leptin, and C-reactive protein levels were significantly increased in the animals from the HFD group compared to the CON group (Table 2).
The animals in the HFD group presented with leukocytosis and neutrophilia (p ≤ 0.05) when compared to the CON group; the number of lymphocytes and monocytes did not show difference (Table 2). Additionally, the HFD group presented hyperplastic bone marrow with an increase in the number of granulocytic cells (p ≤ 0.05) when compared to the CON group (Table 2).
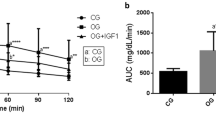
In Vitro Determination of MSC Production of IL-1, IL-6, and TNF-α
IL-1, IL-6, and TNF-α production by MSCs was measured in sample supernatants after 24 h of culture. IL-1, IL-6, and TNF-α concentrations from the HFD group were significantly higher (p ≤ 0.05) than in the CON group (Fig. 1).
In vitro production of IL-1, IL-6, and TNF-α by bone marrow mesenchymal stem cells of the control group (CON) and the high-fat diet group (HFD). The results are expressed as the mean ± SD of the levels of IL-1, IL-6, and TNF-α in the supernatant of a 24-h bonemarrowmesenchymal stem cell culture using a final concentration of 1×106 cells/mL of cells from that the of the control (CON; n = 6) and high-fat diet (HFD; n = 6) groups. Asterisk indicates that there was a significant difference between the CON and HFD groups (p ≤ 0.05).
Western Blots (NF-κB and Phosphorylated NF-κB, PPAR-γ, and RUNX2)
The evaluation of the expression of total NF-κB as well as phosphorylated NF-κB in MSCs was significantly higher in the HFD group (p ≤ 0.05) compared to the CON group. MSCs showed a significantly decreased PPAR-γ expression (p ≤ 0.05) in the HFD group compared to the CON group and an increased RUNX2 expression (p ≤ 0.05) in the HFD group in comparison to the CON group (Fig. 2).
Western blots (NF-κB, phosphorylated NF-κB, PPAR-γ, and RUNX2). Results expressed as mean plus standard deviation (n = 6) of total and phosphorylated NF-κB, PPAR-γ, and RUNX2 protein expression in mesenchymal stem cells from control (CON) and high-fat diet group (HFD). After densitometric quantification, results for total and phosphorylated NF-κB, PPAR-γ, and RUNX2 protein expression were normalized to β-actin values. Asterisk indicates a significant difference between the control group (CON) and high-fat diet group (HFD) (p ≤ 0.05).
DISCUSSION
HFD is a widely used model for the study of obesity and metabolic syndrome in rodents [ 23–25 ]. The main advantages of this model lie in its physiological properties and in its similarity to human disease etiology [23, 24]. However, the contribution of HFD models to understanding obesity and the metabolic syndrome has limitations, due to the frequent use of unbalanced composition of diets resulting from low nutrient density and addition of non-purified ingredients [25]. In the current study, dietary constituents were carefully matched to diet energy density with the goal of providing a more precise assessment. Since diet ingredients were adjusted for nutrient density, and no signs of hyperphagia were observed, groups did not differ with respect to the intake of protein, fiber, or micronutrients. This fact is of major importance, given that the marginal intake of some nutrients could have affected the studied outcomes, either directly or indirectly [26, 27].
Studies have shown an association between HFD and an increase in body fat and total cholesterol and triglyceride levels [25, 28], as well as elevated white blood cell counts [29, 30]. In our study, we observed that the consumption of a HFD resulted in increased body weight with a significant increase in adiposity as evaluated by fat depots, as well as higher blood levels of total cholesterol, triglycerides, leptin, and C-reactive protein. Furthermore, we observed leukocytosis and a higher number of bone marrow cells and, more specifically, polymorphonuclear granulocytes.
Obesity can be considered a state of low-grade inflammation associated with increased levels of leptin and other mediators, mainly pro-inflammatory cytokines. TNF-α was identified as the first molecular link between inflammation and obesity [31]. TNF-α is overexpressed not only in adipose tissue, albeit at extremely low circulating levels, but also in other tissues [31, 32]. Adipose tissue can also secrete several cytokines, such as TNF-α, IL-1, IL-6, adiponectin, and leptin, which can have both direct and indirect effects on hematopoietic cells [1, 3–5].
NF-κB is regarded as a primary regulator of acute and chronic inflammatory responses. Also, NF-κB is a key component of inducible expression pathways and may play a role in stem cell cytokine production [33]. Inflammatory signaling is primarily mediated by the NF-κB pathway, which can lead to increased expression of cytokines and such growth factors as IL-6, TNF-α, and VEGF in MSCs. These cytokines and growth factors are implicated in the dynamic production of mediators of cell–stromal communication, which are important in hematopoiesis [34]. Our results show that MSCs from HFD animals have more capability to produce IL-1, IL-6, and TNF-α in vitro compared to cells from animals fed a CON diet. Consistent with these data is an increase of total and phosphorylated NF-κB expression. Furthermore, our data showed that the increase in NF-κB expression was associated with a reduction in PPAR-γ expression.
Cytokines, such as IL-1 and TNF-α, are dependent on NF-κB activation and have the capacity to inhibit adipocyte differentiation in MSCs by antagonizing PPAR-γ, a key inducer of adipogenesis, suggesting that these cytokines may be physiologically important for MSCs lineage commitment [16]. Additionally, PPAR-γ is a ligand-activated transcription factor having anti-inflammatory properties that play an important role in regulating NF-κB-induced inflammation [35]. PPAR-γ plays a role in diverse biological processes, including cell proliferation, glucose homeostasis, lipid metabolism, and inflammation [36]. PPAR-γ and its activators are known as important modulators of NF-κB, thus exhibiting anti-inflammatory effects [35] that can ultimately alter the expression of pro-inflammatory genes, such as IL-1, IL-6, or TNF-α [19].
Because PPAR-γ is a key regulator of adipogenesis, suppression of PPAR-γ function may inhibit adipogenesis and consequently shift bone marrow differentiation towards osteoblastogenesis [37]. This effect was reflected in our findings as an increase in levels of RUNX2, an osteogenic transcription factor, in MSCs from the HFD group. Suzawa et al. [16] demonstrated the ability of TNF-α/IL-1 to activate the TAK1/TAB1/NIK (NF-κB-inducible kinase) signaling cascade that blocks PPAR-γ DNA binding trough physical association with NF-κB. Suppression of PPAR-γ function may inhibit adipogenesis and consequently shift cell fate commitment more to osteoblasts than adipocytes in bone marrow. In agreement with these data, we observe increased levels of leptin in HFD animals compared to control animals. Leptin has been shown to have an anabolic effect in a human marrow stromal cell line, indicating that leptin can promote differentiation into an osteoblastic phenotype [38, 39].
Our results lead us to speculate that MSCs from HFD animals are in an inflammatory state compared to control animals and that this state may be brought on by an increase of pro-inflammatory cytokines such as IL-1, IL-6, and TNF-α as well as the NF-κB expression to the detriment of PPAR-γ expression. Additionally, a reduction of PPAR-γ expression in MSCs could decrease their ability to differentiate into adipocytes, thus increasing osteoblastic differentiation. This, in turn, could be partly responsible for niche alterations that affect hematopoietic cell numbers [40], as is indicated by an increase in total bone marrow cellularity associated to peripheral leukocytosis in our model.
To summarize, chronic consumption of a HFD can affect hematopoiesis in general and MSCs in particular by promoting an inflammatory state and influencing modulation of the hematopoietic system.
References
Gainsford, T., T.A. Willson, D. Metcalf, E. Handman, C. McFarlane, A. Ng, N.A. Nicola, W.S. Alexander, and D.J. Hilton. 1996. Leptin can induce proliferation, differentiation, and functional activation of hemopoietic cells. Proceedings of the National Academy of Sciences USA 93: 14564–14568.
Choi, K.D., M. Vodyanik, and I.I. Slukvin. 2011. Hematopoietic differentiation and production of mature myeloid cells from human pluripotent stem cells. Nature Protocols 6: 296–313.
Fantuzzi, G., and R. Faggioni. 2000. Leptin in the regulation of immunity, inflammation, and hematopoiesis. Journal of Leukocyte Biology 68: 437–446.
Schäffler, A., J. Schölmerich, and B. Salzberger. 2007. Adipose tissue as an immunological organ: Toll-like receptors, C1q/TNFs and CTRPs. Trends in Immunology 28: 393–399.
Laharrague, P., J.M. Oppert, P. Brousset, J.P. Charlet, A. Campfield, A.M. Fontanilles, B. Guy-Grand, J.X. Corberand, L. Pénicaud, and L. Casteilla. 2000. High concentration of leptin stimulates myeloid differentiation from human bone marrow CD34+ progenitors: potential involvement in leukocytosis of obese subjects. International Journal of Obesity and Related Metabolic Disorders 24: 1212–1216.
Ogawa, M. 1993. Differentiation and proliferation of hematopoietic stem cells. Blood 81: 2844–2853.
Fuchs, E., T. Tumbar, and G. Guasch. 2004. Socializing with the neighbors: stem cells and their niche. Cell 116: 769–778.
Rosen, E.D., and O.A. MacDougald. 2006. Adipocyte differentiation from the inside out. Nature Reviews Molecular Cell Biology 7: 885–896.
Ichida, F., R. Nishimura, K. Hata, T. Matsubara, F. Ikeda, K. Hisada, H. Yatani, X. Cao, T. Komori, A. Yamaguchi, and T. Yoneda. 2004. Reciprocal roles of MSX2 in regulation of osteoblast and adipocyte differentiation. The Journal of Biological Chemistry 279: 34015–34022.
Jeon, M.J., J.A. Kim, S.H. Kwon, S.W. Kim, K.S. Park, S.W. Park, S.Y. Kim, and C.S. Shin. 2003. Activation of peroxisome proliferator-activated receptor-y inhibits the Runx2-mediated transcription of osteocalcin in osteoblasts. The Journal of Biological Chemistry 278: 23270–23277.
Arai, F., A. Hirao, M. Ohmura, H. Sato, S. Matsuoka, K. Takubo, K. Ito, G.Y. Koh, and T. Suda. 2004. Tie2/angiopoietin-1 signaling regulates hematopoietic stem cell quiescence in the bone marrow niche. Cell 118: 149–161.
Calvi, L.M., G.B. Adams, K.W. Weibrecht, J.M. Weber, D.P. Olson, M.C. Knight, R.P. Martin, E. Schipani, P. Divieti, F.R. Bringhurst, L.A. Milner, H.M. Kronenberg, and D.T. Scadden. 2003. Osteoblastic cells regulate the haematopoietic stem cell niche. Nature 425: 841–846.
Zhang, J., C. Niu, L. Ye, H. Huang, X. He, W.G. Tong, J. Ross, J. Haug, T. Johnson, J.Q. Feng, S. Harris, L.M. Wiedemann, Y. Mishina, and L. Li. 2003. Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425: 836–841.
Naveiras, O., V. Nardi, P.L. Wenzel, P.V. Hauschka, F. Fahey, and G.Q. Daley. 2009. Bone-marrow adipocytes as negative regulators of the haematopoietic microenvironment. Nature 460: 259–263.
Takada, I., A.P. Kouzmenko, and S. Kato. 2010. PPAR-gamma Signaling Crosstalk in Mesenchymal Stem Cells. PPAR Research. doi:10.1155/2010/341671.
Suzawa, M., I. Takada, J. Yanagisawa, F. Ohtake, S. Ogawa, T. Yamauchi, T. Kadowaki, Y. Takeuchi, H. Shibuya, Y. Gotoh, K. Matsumoto, and S. Kato. 2003. Cytokines suppress adipogenesis and PPAR-gamma function through the TAK1/TAB1/NIK cascade. Nature Cell Biology 5: 224–230.
Wan, Y. 2010. PPARγ in bone homeostasis. Trends in Endocrinology and Metabolism 21: 722–728.
Takada, I., M. Suzawa, and S. Kato. 2005. Nuclear receptors as targets for drug development: crosstalk between peroxisome proliferator-activated receptor gamma and cytokines in bone marrow-derived mesenchymal stem cells. Journal of Pharmacological Sciences 97: 184–189.
Kelly, D., J.I. Campbell, T.P. King, G. Grant, E.A. Jansson, A.G. Coutts, S. Pettersson, and S. Conway. 2004. Commensal anaerobic gut bacteria attenuate inflammation by regulating nuclear-cytoplasmic shuttling of PPAR-gamma and RelA. Nature Immunology 5: 104–112.
Reeves, P.G., F.H. Nielsen, and G.C. Fahey Jr. 1993. AIN-93 purified diets for laboratory rodents: final report of the American Institute of Nutrition ad hoc writing committee on the reformulation of the AIN-76A rodent diet. Journal of Nutrition 123: 1939–1951.
Pang, J., Y. Choi, and T. Park. 2008. Ilex paraguariensis extract ameliorates obesity induced by high-fat diet: potential role of AMPK in the visceral adipose tissue. Archives of Biochemistry and Biophysics 476: 178–185.
Dacie, J.V., and S.M. Lewis. 1995. Practical haematology, 57–58. Edinburgh: Churchill Livingstone.
Buettner, R., J. Scholmerich, and L.C. Bollheimer. 2007. High-fat diets: Modeling the metabolic disorders of human obesity in rodents. Obesity 15: 798–808.
Buettner, R., K.G. Parhofer, M. Woenckhaus, C.E. Wrede, L.A. Kunz-Schughart, J. Schölmerich, and L.C. Bollheimer. 2006. Defining high-fat-diet rat models: metabolic and molecular effects of different fat types. Journal of Molecular Endocrinology 36: 485–501.
Hariri, N., and L. Thibault. 2010. High-fat diet-induced obesity in animal models. Nutrition Research Reviews 23: 270–299.
Cohen-Lahav, M., S. Shany, D. Tobvin, C. Chaimovitz, and A. Douvdevani. 2006. Vitamin D decreases NF kappa B activity by increasing I kappa B alpha levels. Nephrology, Dialysis, Transplantation 21: 889–897.
Wintergerst, E.S., S. Maggini, and D.H. Hornig. 2007. Contribution of selected vitamins and trace elements to immune function. Annals of Nutrition and Metabolism 51: 301–323.
Ghibaudi, L., J. Cook, C. Farley, M. van Heek, and J.J. Hwa. 2002. Fat intake affects adiposity, comorbidity factors, and energy metabolism of Sprague-Dawley rats. Obesity Research 10: 956–963.
Pratley, R.E., C. Wilson, and C. Bogardus. 1995. Relation of the white blood cell count to obesity and insulin resistance: effect of race and gender. Obesity Research 3: 563–571.
Dixon, J.B., and P.E. O’Brien. 2006. Obesity and the white blood cell count: Changes with sustained weight loss. Obesity Surgery 16: 251–257.
Hotamisligil, G.S., P. Arner, J.F. Caro, R.L. Atkinson, and B.M. Spiegelman. 1995. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. The Journal of Clinical Investigation 95: 2409–2415.
Saghizadeh, M., J.M. Ong, W.T. Garvey, R.R. Henry, and P.A. Kern. 1996. The expression of TNF alpha by human muscle. Relationship to insulin resistance. The Journal of Clinical Investigation 97: 1111–1116.
Crisostomo, P.R., Y. Wang, T.A. Markel, M. Wang, T. Lahm, and D.R. Meldrum. 2008. Human mesenchymal stem cells stimulated by TNF-alpha, LPS, or hypoxia produce growth factors by an NF kappa B- but not JNK-dependent mechanism. American Journal of Physiology. Cell Physiology 294: C675–C682.
Hideshima, T., C. Mitsiades, G. Tonon, P.G. Richardson, and K.C. Anderson. 2007. Understanding multiple myeloma pathogenesis in the bone marrow to identify new therapeutic targets. Nature Reviews. Cancer 7: 585–598.
Ricote, M., and C.K. Glass. 2007. PPARs and molecular mechanisms of transrepression. Biochimica et Biophysica Acta 1771: 926–935.
Kota, B.P., T.H. Huang, and B.D. Roufogalis. 2005. An overview on biological mechanisms of PPARs. Pharmacological Research 51: 85–94.
Takada, I., M. Suzawa, K. Matsumoto, and S. Kato. 2007. Suppression of PPAR transactivation switches cell fate of bone marrow stem cells from adipocytes into osteoblasts. Annals of the New York Academy of Sciences 1116: 182–195.
Gordeladze, J.O., C.A. Drevon, U. Syversen, and J.E. Reseland. 2002. Leptin stimulates human osteoblastic cell proliferation, de novo collagen synthesis, and mineralization: Impact on differentiation markers, apoptosis, and osteoclastic signaling. Journal of Cellular Biochemistry 85: 825–836.
Thomas, T., F. Gori, S. Khosla, M.D. Jensen, B. Burguera, and B.L. Riggs. 1999. Leptin acts on human marrow stromal cells to enhance differentiation to osteoblasts and to inhibit differentiation to adipocytes. Endocrinology 140: 1630–1638.
Yin, T., and L. Li. 2006. The stem cell niches in bone. The Journal of Clinical Investigation 116: 1195–1201.
Acknowledgments
This investigation was supported by grants from the Fundação de Amparo a Pesquisa do Estado de São Paulo.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cortez, M., Carmo, L.S., Rogero, M.M. et al. A High-Fat Diet Increases IL-1, IL-6, and TNF-α Production by Increasing NF-κB and Attenuating PPAR-γ Expression in Bone Marrow Mesenchymal Stem Cells. Inflammation 36, 379–386 (2013). https://doi.org/10.1007/s10753-012-9557-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-012-9557-z