Abstract
This study aimed to investigate the effects of paeoniflorin, the main active ingredient of the medicinal plant Paeonia lactiflora Pall., on the permeability of endothelial cells induced by lipopolysaccharide (LPS) and the underlying mechanisms. Human umbilical vein endothelial cells (HUVECs) were stimulated by LPS. Extravasated FITC-dextran reflecting permeability was assessed by multimode microplate reader, and the migration of bis-carboxyethyl-carboxyfluorescein acetoxy-methyl-labeled human acute monocytic leukemia cell line and leukemia cell line cells through HUVECs were analyzed by fluorescence microscopy. The phosphorylations of phosphatidylinositol 3-kinase (PI3K)/Akt, protein kinase C (PKC), and cofilin in HUVECs were assessed by western blotting, and the F-actin level was detected by laser scanning confocal microscopy. After LPS stimulation, inflammatory endothelial cells exhibited significantly increased permeability. Paeoniflorin (10, 30, and 100 μM) inhibited dextran extravasation and leukocyte migration through HUVECs induced by LPS in a concentration-dependent manner. Moreover, paeoniflorin was able to suppress the phosphorylations of PI3K/Akt, PKC, and cofilin, as well as F-actin reorganization in HUVECs induced by LPS. These findings revealed that paeoniflorin partly blocked LPS-induced endothelium permeability, supporting a new explanation for its anti-inflammatory effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The dry roots of Paeonia lactiflora Pall. have long been used in oriental medicine for analgesia and nourishment of the blood and liver. Accumulative data show that P. lactiflora roots possess multiple physiological benefits, including immunoregulation, improvement of learning and memory, and anti-inflammatory effects. Paeoniflorin, a monoterpene glycoside isolated from the roots, has been identified as the main active ingredient responsible for the biological activities [1]. Our previous work showed that the anti-inflammatory action of paeoniflorin was related to the prevention of adhesion between inflammatory endothelial cells and leukocytes by downregulating the expression of adhesion molecules [2]. The candidacy of paeoniflorin as an anti-inflammatory agent prompts better understanding of the downstream pathways responsible for paeoniflorin-associated anti-inflammatory activity.
Under physiological conditions, endothelial cells interconnect to form a selective semipermeable membrane that serves as a barrier between blood and tissue and is responsible for the exchange of fluid and macromolecules on both sides of the vessel wall. Inflammatory stimulation results in damage and dysfunction of the endothelial cell junction, leading to increased vascular permeability, plasma macromolecules, leukocyte infiltration, and even edema or inflammatory injury. Endothelial cells shrink with a widened gap to allow large molecules or blood cells to pass through the endothelial cell layer [3]. In this process, the actin cytoskeleton fulfills this essential function to provide a strong and dynamic intracellular scaffold that organizes integral membrane proteins and responds to environmental cues to orchestrate appropriate cell shape [4]. The association between F-actin and the actin-binding proteins vinculin, talin, α-actinin, zyxin, tensin, and filamin forms cytoplasmic focal adhesion plaques that consecutively bind to the short cytoplasmic domain of the transmembrane integrin receptor [5]. In non-activated confluent endothelial cells, focal adhesion plaques and related cytoskeleton binding proteins are arranged around the cell periphery and appear as punctate structures [6]. Intimate interactions between the actin cytoskeleton and integrins and extracellular matrix also contribute to endothelial barrier integrity [7].
Here, we found that paeoniflorin suppressed the migration of human acute monocytic leukemia cell line (THP-1) and leukemia cell line (HL-60) cells through human umbilical vein endothelial cells (HUVECs) as well as extensive permeability induced by lipopolysaccharide (LPS). To elucidate the anti-inflammatory mechanisms of paeoniflorin, its effects on the qualitative (structural) changes of the cytoskeleton and downstream effectors were investigated.
MATERIALS AND METHODS
Reagents
Paeoniflorin (98 % purity) was obtained from Nanjing Institute for Drug Control (Nanjing, China). Human acute promyelocytic HL-60, THP-1, and HUVECs were purchased from ATCC (VA, USA). RPMI medium 1640 (1640), penicillin, and streptomycin were purchased from Gibco BRL (Grand Island, NY, USA). New-born calf serum (NBCS) was purchased from PAA Laboratories (Linz, Austria). Dexamethasone (DEX) was purchased from Zhejiang Xianju Pharmaceutical Co. Ltd., (Zhejiang, Taizhou China). Bis-carboxyethyl-carboxyfluorescein acetoxy-methyl (BCECF-AM) was purchased from Beyotime Bio-tech (Nantong, China). Twenty-four-well Transwell inserts (5.0-μm pores) were purchased from Millipore (Billerica, USA). Glass-bottom dishes (35 mm) were purchased from Shengyou Bio-Tech (Hangzhou, China). FITC-phalloidin was purchased from Enzo Life Science (NY, USA). FITC-dextran, LPS (Escherichia coli 026:B6), Tween 20, bovine serum albumin, sodium dodecyl sulfate (SDS), dithiothreitol, and phenylmethylsulfonyl fluoride were purchased from Sigma Chemical (St. Louis, MO, USA). Anti-protein kinase C (PKC)α, anti-phosphorylated PKCα/βII, anti-PKCθ, anti-phospho PKCθ, anti-PKCδ, anti-phospho PKCδ, anti-PKCζ, anti-phospho PKCζ, anti-cofilin, anti-phospho cofilin, anti-phosphatidylinositol 3-kinase (PI3K), anti-phospho PI3K, anti-Akt, and anti-phospho Akt antibodies were purchased from Bioworld (GA, USA). GADPH antibody and the peroxidase-conjugated secondary antibodies were purchased from Keygen Biotech Co., Ltd. (Nanjing, China). The other chemicals and reagents used were of analytical grade.
Cell Cultures
HUVECs and HL-60 and THP-1 cells were cultured with RPMI-1640 medium supplemented with 10 % (v/v) NBCS, 100 units/ml penicillin, and 100 μg/ml streptomycin at 37 °C in a humidified atmosphere with 5 % CO2. The medium was changed every 2 days until 80–90 % confluence was achieved. All of the experiments were performed using cells within 20 passages.
HUVEC Monolayer Permeability Assay
HUVECs were plated in 24-well Transwell inserts and cultured to confluence. The upper and lower compartments were replaced with medium, paeoniflorin (10, 30, and 100 μM), and DEX (10 μM) for 24 h, respectively. Lipopolysaccharide (10 μg/ml) was added at the same time for stimulation for 24 h. FITC-dextran was added to the upper compartments and allowed to migrate for 1 h at 37 °C. The medium in the lower compartments was collected and analyzed in a multimode microplate reader (Varioskan Flash, USA) using 547 and 572 nm as the excitation and emission wavelengths, respectively.
Migration of THP-1 and HL-60 cells
HUVECs were plated in 24-well Transwell units and cultured to confluence. The upper and lower compartments were replaced by medium, paeoniflorin (10, 30, and 100 μM), and DEX (10 μM), respectively. Lipopolysaccharide (10 μg/ml) was simultaneously added for stimulation for 24 h. For the THP-1 cell migration assay, BCECF-AM-labeled THP-1 cells (8 × 107 cells/ml; 100 μl) were added to the upper compartments and allowed to migrate for 5 h. For the HL-60 cell migration assay, BCECF-AM-labeled HL-60 cells (8 × 107 cells/ml; 100 μl) were added to the upper compartments and allowed to migrate for 5 h. Cell migration was measured by counting the number of leukocytes in the lower compartments a fluorescence microscopy (Olympus, IX51, Japan).
Immunofluorescence Assay of F-actin in HUVECs
The HUVECs were plated in glass-bottom 35-mm dishes and cultured to confluence. The HUVECs were incubated with paeoniflorin (10, 30, and 100 μM), DEX (10 μM), and medium for 24 h. Lipopolysaccharide (10 μg/ml) was simultaneously added to stimulate for 24 h. After incubation, the HUVECs were fixed in 4 % paraformaldehyde solution for 10 min and permeabilized with 0.1 % Triton X-100 for 5 min. They were then incubated with FITC-phalloidin for 30 min at room temperature in the dark to stain F-actin. Fluorescence was detected by a laser scanning confocal microscopy (Leica, TCS SP2, Germany) using 488 and 525 nm as the excitation and emission wavelengths, respectively.
Western Blotting
HUVECs (4 × 105 cells) were cultured for 24 h and incubated with serum-free 1640 medium for 2 h to allow the cells to achieve quiescence. They were pretreated with paeoniflorin (10, 30, and 100 μM), DEX (10 μM), and medium and stimulated by LPS (10 μg/ml) for appropriate lengths of time in the different protein assays. The HUVECs were then washed twice with ice-cold phosphate-buffered saline (pH 7.2), and proteins were extracted with lysis buffer (50 mM Tris–HCl, 150 mM NaCl, 0.02 % NaN3, 1 % NP40) for 30 min on ice. The cytosol and nuclear extracts were harvested after centrifugation at 12,000 rpm at 4 °C for 10 min. The protein concentration was determined using the Bradford assay. The samples were fractionated on 10 % SDS-polyacrylamide gel electrophoresis and transferred to polyvinylidene fluoride membranes. The membranes were blocked for 1 h at room temperature with 5 % nonfat milk in PBS-Tween 20 (0.1 %) and then incubated with different antibodies. The membrane was incubated with electrochemiluminescence reagent for 2–10 min and exposed to X-ray film. The semiquantification of protein expressions was performed by the software image pro plus applied for densitometry analysis.
Statistical Analysis
All of the data are expressed as mean ± S.D. Statistical significance was evaluated using one-way analysis of variance followed by the Dunnett's test. Values of p less than 0.05 were considered statistically significant.
RESULTS
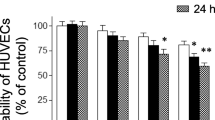
Paeoniflorin Inhibited FITC-dextran Extravasation Induced by LPS in HUVECs
Endothelial structural alternations, impairment or loss of adherence junction, and cell contraction are considered the main reasons for the hyperpermeability of the endothelium following various insults, such as inflammatory stimuli. We investigated the effect of paeoniflorin on the permeability of LPS-stimulated HUVECs by assaying the extravasation of dextran. As shown in Fig. 1, LPS stimulation for 24 h significantly increased dextran extravasation in HUVECs. Paeoniflorin (10, 30, and 100 μM) inhibited extravasation. The inhibitory percentage at a concentration of 100 μM was 35.7 %. The positive control dexamethasone (10 μM) also significantly inhibited extravasation by 52.2 %.
Effects of paeoniflorin and dexamethasone (DEX) on the permeability of LPS-stimulated HUVECs. HUVECs were treated with LPS and paeoniflorin (10, 30, and 100 μM) or DEX (10 μM) for 24 h. The extravasated FITC-dextran was collected and analyzed by a multimode microplate reader. The data are expressed as mean ± S.D. n = 4. The double number sign indicates p < 0.01, vs. normal; single asterisk indicates p < 0.05, double asterisks indicate p < 0.01, vs. LPS group.
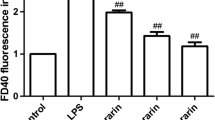
Paeoniflorin Reduced the Migration of Leukocytes in LPS-stimulated HUVECs
Increased endothelium permeability by inflammatory stimuli should facilitate the migration of leukocytes between endothelial cells. As expected, LPS stimulation for 24 h led to a significant increase in the migration of the THP-1 and HL-60 leukocytes through HUVECs. For THP-1 cell migration, paeoniflorin (100 μM) and DEX (10 μM) showed inhibitory percentages of 34.5 and 40.2 %, respectively (Fig. 2a). For HL-60 cell migration, paeoniflorin (100 μM) and DEX (10 μM) showed inhibitory percentages of 36.2 and 42.1 %, respectively (Fig. 2b). These findings were consistent with the results from the dextran extravasation assay.
Effects of paeoniflorin and dexamethasone (DEX) on the migration of leukocytes in LPS-stimulated HUVECs. HUVECs were treated with LPS and paeoniflorin (10, 30, and 100 μM) or DEX (10 μM) for 24 h. The migrated THP-1 and HL-60 cells were measured by counting the number of leukocytes in the lower compartments by a fluorescence microscopy. The data are expressed as mean ± S.D. n = 4. The double number sign indicates p < 0.01, vs. normal; single asterisk indicates p < 0.05, double asterisks indicate p < 0.01, vs. LPS group.
Paeoniflorin Suppressed Cytoskeletal Protein Actin Expression in LPS-stimulated HUVECs
The vascular barrier can be altered by specific factors that act on endothelial cells, including tight junctions, adherens junctions, Ca2+, matrix, and actins. F-actin rearrangement and the subsequent endothelial cell contraction should lead to an increase in endothelium permeability. To determine the expression of F-actin, HUVECs were stimulated by LPS. After 24 h, F-actin expression significantly increased, with disordered stress fibers and contracted cells. Paeoniflorin (30, 100 μM) and dexamethasone (10 μM) obviously decreased the expression of F-actin; the inhibitory percentages were 28.3 %, 55.6 % and 68 %, respectively. Paeoniflorin (30, 100 μM) almost restored stress fiber and cell morphology, and dexamethasone (10 μM) had a slight effect on cell morphology (Fig. 3a, b).
Effects of paeoniflorin and dexamethasone (DEX) on F-actin expression in LPS-stimulated HUVECs. HUVECs were treated with LPS and paeoniflorin (10, 30, and 100 μM) or DEX (10 μM) for 24 h, and then incubated with FITC-phalloidin for 30 min. Fluorescence was detected by laser scanning confocal microscopy using 488 and 525 nm as the excitation and emission wavelengths, respectively. Bar = 20 μm. ×650. The data are expressed as mean ± S.D. n = 3. The double number sign indicates p < 0.01, vs. normal; single asterisk indicates p < 0.05, double asterisks indicate p < 0.01, vs. LPS group.
Paeoniflorin Repressed p-Cofilin Expression in LPS-Stimulated HUVECs
As an important cytoskeleton-associated protein, cofilin has been proved to contribute to actin depolymerization and stress fiber disruption. For the higher expression of p-cofilin in HUVECs, the optimal stimulation time of LPS (10 μg/ml) was 3 h (Fig. 4a, b). Paeoniflorin inhibited p-cofilin protein expression in a concentration-dependent manner, and the inhibitory percentages at concentrations of 30 and 100 μM were 16.3 and 33.3 %, respectively. No significant change was observed in the total cofilin levels. The inhibitory percentage of DEX (10 μM) was 52.7 % (Fig. 4c).
Effects of paeoniflorin and dexamethasone (DEX) on the expression of cofilin proteins in LPS-stimulated HUVECs. a Time-course analysis of cofilin protein expression in LPS-stimulated HUVECs. b After treatment with paeoniflorin (10, 30, and 100 μM) or DEX (10 μM) for 24 h, the levels of cofilin proteins were measured by Western blot. GADPH was used as the internal control. The data are expressed as mean ± SD. n = 3. The double number sign indicates p < 0.01, vs. normal; single asterisk indicates p < 0.05, double asterisks indicate p < 0.01, vs. LPS group.
Paeoniflorin Inhibited PKC Isoforms Phosphorylation in LPS-stimulated HUVECs
The activation of PKC results in the high permeability of vascular vessels by contracting endothelial cells and weakening cell connections. Stimulation with LPS (10 μg/ml) for 20 min resulted in apparent phosphorylation of PKCα, PKCδ, PKCθ, and PKCζ in HUVECs. Paeoniflorin had almost no effect on non-phosphorylated PKCα, PKCδ, PKCθ, and PKCζ and phosphorylated PKCδ and only slightly inhibited the phosphorylation of PKCθ. While for the phosphorylations of PKCα and PKCζ, paeoniflorin exhibited concentration-dependent inhibition. The inhibitory percentages at 30 and 100 μM reached 44.5 and 48.2 %, respectively. In contrast, DEX was able to inhibit the phosphorylation of four isoforms of PKC at 10 μM (Fig. 5a, b).
Effects of paeoniflorin and dexamethasone (DEX) on the expression of PKC proteins in LPS-stimulated HUVECs. HUVECs were incubated with paeoniflorin (10, 30, and 100 μM) or DEX (10 μM) for 24 h and treated with LPS (10 μg/ml) for 20 min. The levels of PKCα, PKCθ, PKCδ, and PKCζ proteins were measured by Western blot. GADPH was used as the internal control. The data are expressed as mean ± SD. n = 3. The double number sign indicates p < 0.01, vs. normal; double asterisks indicate p < 0.01, vs. LPS group.
Paeoniflorin Regulated PI3K/Akt Pathway in LPS-Stimulated HUVECs
The PI3K/Akt signal transduction pathway also plays an important role in the cell cytoskeleton, permeability, migration, proliferation, and apoptosis. Lipopolysaccharide (10 μg/ml) stimulation for 20 min resulted in evident phosphorylations of PI3K and Akt in HUVECs (Fig. 6a). Paeoniflorin (10, 30, and 100 μM) only slightly inhibited the phosphorylation of PI3K but suppressed the phosphorylation of Akt in a concentration-dependent manner. It had no significant effect on the protein expression of PI3K and Akt. Dexamethasone apparently inhibited the phosphorylations of PI3K and Akt at 10 μM (Fig. 6b, c).
Effects of paeoniflorin and dexamethasone (DEX) on LPS-stimulated activation of PI3K/Akt signaling pathways in HUVECs. a Time-course analysis of phosphorylation of PI3K and Akt in LPS-stimulated HUVECs. b After treatment with paeoniflorin (10, 30, and 100 μM) or DEX (10 μM) for 24 h, PI3K, Akt, p-PI3K, and p-Akt were analyzed by Western blot using specific antibodies. GADPH was used as the internal control. The data are expressed as mean ± S.D. n = 3. The double number sign indicates p < 0.01, vs. normal; single asterisks indicate p < 0.05, double asterisks indicate p < 0.01, vs. LPS group.
DISCUSSION
The vascular endothelium that connects the intima of the blood vessels regulates a variety of functions. The maintenance by the endothelium of a semipermeable barrier is very important for controlling the passage of macromolecules and fluid between the blood and interstitial space. If this barrier loses function, tissue inflammation may occur [8]. Leukocytes and macromolecules will enter into inflamed tissues after the permeability of the endothelium changes [9]. Lipopolysaccharide, an important mediator which originates from the cell wall of gram-negative bacteria, substantially enlarges endothelial permeability. The extravasation of the macromolecule dextran and leukocyte migration obviously increased. Paeoniflorin and dexamethasone significantly prevented the extravasation of dextran and leukocyte migration, suggesting that inhibition of endothelial permeability is an important contributor to the anti-inflammatory action of paeoniflorin.
When the endothelium is triggered by certain stimuli, disorganization of the actin filaments can occur, and increased permeability appears [10]. Herein, we go on observing the structural change of actin when enhanced permeability occurs. As we know, actin has two forms: monomer (G-actin) and polymer (F-actin) [11]. ADF/cofilin, as an actin-depolymerizing protein, binds to G-actin, then depolymerizes G-actin from F-actin, in turn, mediates actin depolymerization and stress fiber disruption [12, 13], thereby allowing cells to contract, generate protrusions, and divide [14, 15]. In the present study, LPS treatment led to increased F-actin expression, disordered stress fibers, and endothelial cell contraction. Paeoniflorin reduced the expression of F-actin and normalized the arrangement of stress fibers as well as cell morphology. Dexamethasone only reduced the expression of F-actin and slightly normalized the arrangement of stress fibers and cell morphology. F-actin downregulation induced by paeoniflorin might contribute to a reduction of the high permeability of endothelial cells.
Once phosphated, ADF/cofilin becomes inactive, losing the filament-severing and monomer- binding activities, thereby promoting actin polymerization, cell perameability, and cell migration [16]. In the present study, LPS stimulation substantially phosphorylated cofilin in HUVECs. Paeoniflorin reversed the expression of phosphorylated cofilin in a concentration-dependent manner. The findings suggest that the inhibition of cofilin phosphorylation may contribute to the ability of paeoniflorin to down-regulate F-actin expression.
The cytoskeleton proteins of endothelial cells, which are important substrates of PKC, play roles in maintaining cell morphology, cell adhesion, and cell connections. PKC is an important protein kinase and an intracellular signaling molecule that can bind to many protein substrates. The activation of PKC results in the high permeability of vascular vessels by contracting endothelial cells and weakening cell connections [17]. The function and tissue distribution of PKC isoforms are specific. The isoforms in endothelia include PKCα, PKCβ, PKCδ, PKCε, PKCζ, and PKCθ [18, 19], but which one is preferentially related to endothelium permeability is still unknow. PKCθ has been shown to be related to the cytoskeletal endothelium protein [20]. The expression of cofilin-1 induced by hyperglycemia in endothelial cells occurred through PKCζ activation [21]. In the present study, LPS significantly induced the phosphorylation of PKCα, PKCδ, PKCθ, and PKCζ. Paeoniflorin inhibited the phosphorylations of PKCα and PKCζ in a concentration-dependent manner but only slightly affected the phosphorylation of PKCθ and exhibited almost no effect on PKCδ. The inhibition of cofilin phosphorylation by paeoniflorin might be accounted for the downregulation of PKCα and PKCζ activation.
Besides PKC, the PI3K/Akt pathway also plays an important role in cell cytoskeleton maintenance and permeability [22]. The lipid products of PI3K serve as second messengers by binding to and activating different cellular target proteins, such as Akt. Activated Akt is released into the cytoplasm or nucleus from the membrane and then phosphorylates the substrate with serine/threonine residues to exert its biological effects. The PI3K/Akt pathway can be activated by numerous stimuli, including LPS, cytokines, and growth factors. Interestingly, the activation of PKC isoforms is also related to the PI3K/Akt pathway. PKCα has been shown to contribute to Akt activation [23], and PI3K has been linked to PKCζ activation [24]. In the present study, LPS stimulation led to significant phosphorylation of PI3K and Akt. Paeoniflorin inhibited phosphorylation in a concentration-dependent manner, suggesting that it prevented the permeability of the endothelium likely by downregulating the activation of the PI3K/Akt signaling pathway.
In conclusion, the findings of the present study indicate that paeoniflorin prevented LPS-induced endothelium permeability, a crucial step in the inflammatory response. The underlying mechanisms may involve the expression of F-actin and phosphorylation of PI3K/Akt, PKC, and cofilin in endothelial cells.
References
Fang, S., W. Zhu, Y. Zhang, Y. Shu, and P. Liu. 2012. Paeoniflorin modulates multidrug resistance of a human gastric cancer cell line via the inhibition of NF-Κb activation. Molecular Medicine Report 5: 351–356.
Xu, H., X.H. Gao, J. Song, F.Y. Wang, Z. Xu, D. Lu, X.X. Xu, Y.F. Xia, and Y. Dai. 2010. Peoniflorin prevents the adhesion between inflammatory endothelial cells and leukocytes through inhibiting the activation of MAPKs and NF-κB. Drug Development Research 71: 275–284.
Vandenbroucke, E., D. Mehta, R. Minshall, and A.B. Malik. 2008. Regulation of endothelial junctional permeability. Annals of the New York Academy of Sciences 1123: 134–145.
Prasain, N., and T. Stevens. 2009. The actin cytoskeleton in endothelial cell phenotypes. Microvascular Research 77: 53–63.
Geiger, B., A. Bershadsky, R. Pankov, and K.M. Yamada. 2001. Transmembrane crosstalk between the extracellular matrix-cytoskeleton crosstalk. Nature Reviews Molecular Cell Biology 2: 793–805.
Patterson, C.E., and H. Lum. 2001. Update on pulmonary edema: the role and regulation of endothelial barrier function. Endothelium-New York 8: 75–105.
Curtis, T.M., P.J. McKeown-Longo, P.A. Vincent, S.M. Homan, E.M. Wheatley, and T.M. Saba. 1995. Fibronectin attenuates increased endothelial monolayer permeability after RGD peptide, anti-alpha 5 beta 1, or TNF-alpha exposure. The American Journal of Physiology 269: L248–L260.
Dolly, M., and B.M. Asrar. 2006. Signaling mechanisms regulating endothelial permeability. Physiological Reviews 86: 279–367.
Bogatcheva, N.V., and A.D. Verin. 2008. The role of cytoskeleton in the regulation of vascular endothelial barrier function. Microvascular Research 76: 202–207.
Lai, C.H., K.H. Kuo, and J.M. Leo. 2005. Critical role of actin in modulating BBB permeability. Brain Research Reviews 50: 7–13.
Lee, S.H., and R. Dominguez. 2010. Regulation of actin cytoskeleton dynamics in cells. Molecules and Cells 29: 311–325.
Gohla, A., and G.M. Bokoch. 2002. 14-3-3 regulates actin dynamics by stabilizing phosphorylated cofilin. Current Biology 12: 1704–1710.
Dreiza, C.M., C.M. Brophy, P. Komalavilas, E.J. Furnish, L. Joshi, M.A. Pallero, J.E. Murphy-Ullrich, M. von Rechenberg, Y.S. Ho, B. Richardson, N. Xu, Y. Zhen, J.M. Peltier, and A. Panitch. 2005. Transducible heat shock protein 20 (HSP20) phosphopeptide alters cytoskeletal dynamics. The FASEB Journal 19: 261–263.
Ghosh, M., X. Song, G. Mouneimne, M. Sidani, D.S. Lawrence, and J.S. Condeelis. 2004. Cofilin promotes actin polymerization and defines the direction of cell motility. Science 304: 743–746.
Maciver, S.K., and P.J. Hussey. 2002. The ADF/cofilin family: actin-remodeling proteins. Genome Biology 3: 3007.1–3007.12.
Bamburg, J.R., A. McGough, and S. Ono. 1999. Putting a new twist on actin: ADF/cofilins modulate actin dynamics. Trends in Cell Biology 9: 364–370.
Li, S., Q.B. He, and K.S. Zhou. 2003. The research of vascular permeability between Protein kinase C and endothelial cytoskeletal protein. Journal Chinese of Microcirculation 7: 184–190.
Mattila, P., M.L. Majuri, S. Tiisala, and R. Renkonen. 1994. Expression of six protein kinase C isotypes in endothelial cells. Life Sciences 55: 1253–1260.
Haller, H., W. Ziegler, C. Lindschau, and F.C. Luft. 1996. Endothelial cell tyrosine kinase receptor and G protein-coupled receptor activation involves distinct protein kinase C isoforms. Arteriosclerosis, Thrombosis, and Vascular Biology 16: 678–686.
Tang, S., K.G. Morgan, C. Parker, and J.A. Ware. 1997. Requirement for protein kinase C theta for cell cycle progression and formation of actin stress fibers and filopodia in vascular endothelial cells. Journal of Biological Chemistry 272: 28704–28711.
Liu, Y.M., Y.F. Wang, F.J. Wang, J. Deng, D.H. Wu, H. Su, Y.M. Zhang, N. Wang, D.L. Zhang, and J.P. Ouyang. 2008. The expression of cofilin-1 via PKC pathway induced by hyperglycemia in endothelial cells. The FASEB Journal 22: 964.
Katso, R., K. Okkenhaug, K. Ahmadi, S. White, J. Timms, and M.D. Waterfield. 2001. Cellular function of phosphoinositide 3-kinases: implications for development, homeostasis, and cancer. Annual Review of Cell and Developmental Biology 17: 615–675.
Partovian, C., and M. Simons. 2004. Regulation of protein kinase B/Akt activity and Ser473 phosphorylation by protein kinase Calpha in endothelial cells. Cell Communication and Signaling 16: 951–957.
Minshall, R.D., E.E. Vandenbroucke, M. Holinstat, A.T. Place, C. Tiruppathi, S.M. Vogel, G.P. van Nieuw Amerongen, D. Mehta, and A.B. Malik. 2010. Role of protein kinase Cζ in thrombin-induced RhoA activation and interendothelial gap formation of human dermal microvessel endothelial cell monolayers. Microvascular Research 80: 240–249.
Acknowledgments
This work was funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions and Program for Changjiang Scholars and Innovative Research Team in University (IRT1193).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Huan Xu and Jie Song equally contributed to this paper.
Rights and permissions
About this article
Cite this article
Xu, H., Song, J., Gao, X. et al. Paeoniflorin Attenuates Lipopolysaccharide-Induced Permeability of Endothelial Cells: Involvements of F-Actin Expression and Phosphorylations of PI3K/Akt and PKC. Inflammation 36, 216–225 (2013). https://doi.org/10.1007/s10753-012-9537-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-012-9537-3