Abstract
Elaeocarpus petiolatus is known to exert active oxygen scavenging, anti-aging, and whitening actions. However, the biological effects of E. petiolatus on inflammation and the underlying mechanisms are yet to be established. In the present study, we investigated the anti-inflammatory effects of the ethanol extract from E. petiolatus (EPE) bark in murine Raw264.7 macrophages stimulated with lipopolysaccharide (LPS). EPE inhibited the production of PGE2, TNF-α, and IL-1β in a dose-dependent manner in Raw264.7 cells stimulated with LPS. The decrease in PGE2 production was correlated with reduced COX-2 expression. Furthermore, EPE suppressed the phosphorylation of extracellular signal-related kinases (ERK), c-Jun N-terminal kinase (JNK), and p38 as well as translocation of the NF-κB p65 subunit from the cytosol to nucleus. Our results suggest that EPE exerts anti-inflammatory activity through inhibition of inflammatory mediators, such as PGE2, TNF-α, and IL-1β, and downregulation of COX-2 via suppression of NF-κB translocation and phosphorylation of ERK, JNK, and p38 in LPS-stimulated Raw264.7 cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Elaeocarpus is a genus of tropical and subtropical evergreen trees and shrubs that includes approximately 350 species widely distributed in tropical and subtropical regions from Madagascar in the west through India, Southeast Asia, southern China, Japan, Australia, New Zealand, Fiji, and Hawaii in the east [1]. The islands of Borneo and New Guinea have the greatest concentration of Elaeocarpus species [2].
Previously, Osumi and Sakaida in 2003 reported that a skincare preparation comprising an extract from plants of the genus Elaeocarpus in the Elaeocarpaceae family, such as Elaeocarpus sphaericus, Elaeocarpus serratus, Elaeocarpus petiolatus, or Elaeocarpus floribundus, exerts active oxygen scavenging, hyaluronidase inhibitory, elastase inhibitory, collagenase inhibitory, and tyrosinase inhibitory actions, in addition to high safety and excellent anti-aging and whitening properties.
Lipopolysaccharide (LPS) stimulates the production of inflammatory mediators, such as prostaglandin (PGE2), tumor necrosis factor-α (TNF-α), and interleukins [3]. Overproduction of inflammatory mediators by activated macrophages is associated with the pathophysiology of many inflammatory diseases, including cardiovascular disease, cancer, and rheumatoid arthritis [4, 5]. PGE2, a key inflammatory mediator produced following the sequential oxidation of arachidonic acid, dihomo gamma linolenic acid, or eicosapentaenoic acid by cyclooxygenases (COX-1 and COX-2) and terminal prostaglandin synthases, stimulates cytokine generation [6] and vasodilation, and mediates fever and pain [7]. These prostaglandin levels are regulated by expression of inducible COX-2 in inflammation [8].
Production of proinflammatory mediators and cytokines by LPS depends on inducible gene expression mediated by the activation of different transcription factors, such as nuclear factor kappa B (NF-κB) and mitogen-activated protein kinase (MAPKs) [9–11]. NF-κB plays critical roles in the regulation of cell survival genes and coordination of the expression of proinflammatory mediators and cytokines, including COX-2, TNF-α, and IL-1β [12]. MAPK proteins, such as extracellular signal-related kinases (ERK), p38 MAPK, and c-Jun N-terminal kinase (JNK), are activated by LPS in macrophages and other cell types [3, 13]. Accordingly, NF-κB and MAPKs have been investigated as potential targets for anti-inflammatory drug candidates. Some effective plant-derived medicines have been found to suppress the production of proinflammatory cytokines and PGE2 in macrophages [14]. Data obtained from our screening program designed to identify plants with anti-inflammatory potential showed that the ethanol extract of E. petiolatus (EPE) inhibits PGE2 production. In the present study, we investigated the biological effects of EPE on LPS-induced inflammation of Raw264.7 cells and its underlying mechanisms of action.
To establish the anti-inflammatory actions of EPE in macrophage cells under LPS exposure and the related mechanisms, we specifically investigated its influence on COX-2 expression, translocation of NF-κB, and activation of MAPK pathways.
MATERIALS AND METHODS
Materials
Lipopolysaccharide (LPS), concanavalin A (Con A), and dimethyl sulfoxide (DMSO) were purchased from Sigma (St Louis, MO). 3-(4, 5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) was obtained from Amresco (Solon, OH). Antibodies specific for COX-2, β-actin, and MAPKs (ERK, p38, JNK) were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). We obtained p-p38 and pJNK from Assay Designs (Ann Arbor, MI), and pIκB-α, pERK, and IκB-α from Cell Signaling Technology (Danvers, MA).
Preparation of the E. petiolatus Ethanol Extract
E. petiolatus (Jack) Wall. ex Steud. was collected in chang bing du ying, China, in 2008. The ethanol extract from barks of E. petiolatus (FBM004-030) was obtained from International Biological Material Research Center in Korea Research Institute of Bioscience and Biotechnology, Daejeon, Korea. Stock solution (20 mg/ml) of the extract was prepared in DMSO and stored at −20°C before use.
Cell Culture
RAW 264.7 mouse macrophage cells purchased from the American Tissue Culture Center (Rockville, MD) were cultured in Dulbecco’s modified Eagle’s medium containing 10% fetal bovine serum and maintained at 37°C in a humidified atmosphere containing 5% CO2. After adhesion of Raw264.7 cells for 4 h, various concentrations of EPE were added.
Cell Viability Assay
Cell proliferation was evaluated using the MTT assay involving mitochondria-dependent reduction of MTT to formazan. Briefly, 10 μl of 5 mg/ml MTT solution was added to the supernatant and incubated for 4 h at 37°C. Media were discarded, followed by the addition of DMSO. The optical density of formazan was measured at 570 nm using a microplate reader (Benchmark, Bio-Rad Laboratories, Hercules, CA). Absorbance of formazan formed by untreated cells was taken as 100%.
PGE2 Assay
PGE2 synthesis was assessed using a commercially available PGE2 enzyme immunometric assay kit (Cayman Co., Ann Arbor, MI). Diluted standard/sample was pipetted into a 96-well plate pre-coated with a goat polyclonal anti-mouse IgG after LPS (1 μg/ml) stimulation for 24 h. Aliquots of a PGE2 monoclonal antibody and PGE2 acetylcholine esterase conjugate were added to each well and allowed to incubate at room temperature for 16 h. Wells were washed five times with wash buffer containing 0.05% Tween-20, followed by the addition of 200 μl of Ellman’s reagent containing acetylthiocholine and 5,5′-dithio-bis-(2-nitrobenzoic acid). After 60 min, absorbance was measured at 405 nm with a microplate reader.
Reverse Transcription-PCR Analysis
Raw264.7 cells (5 × 106 cells) were incubated for 6 h with or without various concentrations of EPE and LPS (1 μg/ml). After washing twice with PBS, total RNA was isolated from the cell pellet using TRIzol (Invitrogen, Carlsbad, CA). The total amount of RNA was determined by absorbance at 260 nm. RNA (1 μg) was reverse-transcribed into cDNA using AccuPower RT PreMix and oligo(dT)18 primer (Bioneer, Daejeon, Korea). PCR samples contained 20 μl of the reaction mixture comprising 30 mM KCl, 1.5 mM MgCl2, 0.25 mM dNTP, 1.0 U of Top DNA polymerase (Bioneer, Daejeon, Korea), and primers in 10 mM Tris–HCl (pH 8.3). The sense and antisense primers were 5′-GAA GTC TTT GGT CTG GTG CCT G-3′ and 5′-GTC TGC TGG TTT GGA ATA GTT GC-3′ for COX-2, 5′-GGA GCG ACT TGT GGA TTG TC-3′ and 5′-GTG AGG GCT TGG CTG AGT GAG-3′ for iNOS, and 5′-AGG CTG TGC TGT CCC TGT ATG C-3′ and 5′-ACC CAA GAA GGA AGG CTG GAA A-3′ for β-actin, respectively. The PCR amplification was performed under the following conditions: 30 cycles of denaturation at 94°C for 45 s, annealing at 56°C (iNOS and β-actin) or 57°C (COX-2) for 45 s, and extension at 72°C for 1 min using an automated DNA thermal cycler (Palm cycler Corbett Research, Sydney, Australia). Amplified products were run on a 1.5% agarose gel and visualized by ethidium bromide staining.
Immunoblot Analysis
Cells (5 × 105 cells/ml) were harvested and washed twice with ice-cold PBS. Nuclear and cytoplasmic fractions were prepared using NE-PER nuclear and cytoplasmic extraction reagents (Pierce, Rockford, IL), according to the manufacturer’s instructions. Total cell lysates were prepared using lysis buffer (Sigma, St Louis, MO). Protein concentrations were measured using a Bradford assay kit (Bio-Rad, Hercules, CA). The protein equivalents of samples were separated using 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to polyvinylidene fluoride (PVDF) membranes. Membranes were blocked with 5% skim milk in TBST, probed with antibodies against COX-2, ERK, JNK, p38, and β-actin overnight at 4°C, and exposed to horseradish peroxidase (HRP)-conjugated secondary antibodies for 1 h. Antibody-specific proteins were visualized using an enhanced chemiluminescence detection system (Amersham Pharmacia Biotech, Uppsala, Sweden).
Immunocytochemistry Analysis
Raw264.7 cells were preincubated with EPE for 1 h on Permanox plastic chamber slides, and subsequently treated with LPS (1 μg/ml) for 16 h (COX-2) or 1 h (p65). Cells were fixed with ethanol for 30 min at 4°C. Slides were washed three times with PBS and blocked with 3% BSA in PBS for 30 min, followed by overnight incubation at 4°C with an antibody to COX-2 (rabbit polyclonal IgG). For p65 staining, chamber slides were incubated with anti-NF-κB p65 subunit (rabbit polyclonal IgG, Assay Designs) antibodies. Slides were washed three times each with PBS and incubated with anti-rabbit Texas Red-conjugated secondary antibody (Santa Cruz Biotechnology, Santa Cruz, CA) for 2 h at room temperature. Next, slides were washed with PBS and mounted using ProLong Gold Antifade reagent containing 4′,6-diamidino-2-phenylindole (DAPI) (Invitrogen Co., Carlsbad, CA) to highlight cell nuclei. Intensity changes were visualized under a confocal laser scanning microscope (LSM510m, Carl Zeiss, Stuttgart, Germany).
Cytokine Assays in Raw264.7 Cells
The inhibitory effects of extracts on TNF-α and IL-1β production were measured with an enzyme-linked immunosorbent assay (ELISA) kit (Biosource International Co., Camarillo, CA) in supernatant fractions collected from EPE-treated cells. Samples were analyzed according to the manufacturer’s protocols.
Cytokine Assays in Splenocytes
BALB/c mice were sacrificed at 6–8 weeks and the spleens aseptically removed. Splenocytes were mechanically dissociated with two needles. Red blood cells (RBC) were lysed with RBC lysis buffer (Sigma Chemical, St Louis, MO) at 37°C for 10 min. After washing with PBS, cells were cultured for 4 h in RPMI 1640 containing 10% fetal bovine serum, 25 mM HEPES, 2 mM glutamine, 100 U/ml penicillin, and 100 μg/ml streptomycin (GibcoBRL, NY, USA). Splenocytes were plated onto 96-well plates at a density of 1 × 106 cells/ml and treated with different concentrations of EPE for 1 h. Following incubation with 1 μg/ml of ConA (Sigma, St Louis, MO) for a further 3 days, IL-4 and IL-13 concentrations in the supernatant were measured using ELISA kits (R&D Systems, Minneapolis, MN) for mouse cytokines, according to the manufacturer’s protocols.
Statistics
Data are expressed as means ± standard errors (SEM). Results were obtained from at least three independent experiments performed in triplicate. Statistical significance was determined using a two-tailed Student’s t test for independent means. P values of 0.05 or less were considered statistically significant.
RESULTS
EPE Inhibits PGE2 Production by Suppressing COX-2 Expression in LPS-Induced Raw264.7 Cells
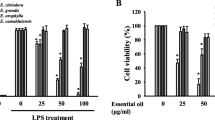
To determine whether EPE affects COX-2 expression induced by LPS, the PGE2 concentrations in culture media and COX-2 expression were examined in Raw264.7 cells stimulated with LPS. Incubation of Raw264.7 cells with LPS for 24 h resulted in a 38-fold increase in the PGE2 level. Notably, EPE (50 μg/ml) inhibited PGE2 release by 39.0 ± 8.2% (Fig. 1a), but had no effects on cell viability (Fig. 1b).
Differential effects of EPE on LPS-induced PGE2 in Raw264.7 cells. a PGE2 EIA assay; cells were preincubated with EPE for 1 h, followed by treatment with LPS (1 μg/ml) for 24 h. The supernatant was collected and the PGE2 level measured as described in “MATERIALS AND METHODS.” “Basal” represents the amount of PGE2 produced from cells not treated with LPS. $ P < 0.005, significant difference from untreated cells and # P < 0.05, significant difference from LPS-treated cells. b Cell viability; effects of EPE on cell growth were determined using the MTT assay. $ P < 0.005 significant difference from untreated cells.
Preincubation of cells with EPE prevented COX-2 protein (Fig. 2a) and mRNA (Fig. 2b) expression in a dose-dependent manner. To further examine the expression of COX-2 protein in cell, immunocytometric analysis was performed. As shown as Fig. 2c, treatment with LPS resulted in a marked increase of COX-2 protein levels, which was inhibited upon pretreatment with EPE (50 μg/ml). Our results suggest that EPE inhibits the release of PGE2 via suppression of COX-2 mRNA and protein expression.
Differential effects of EPE on LPS-induced COX-2 expression in Raw264.7 cells. a Cells were preincubated with EPE for 1 h and treated with LPS (1 μg/ml) for 16 h. The COX-2 protein level was determined with the immunoblot assay. b Cells were preincubated with EPE for 1 h, followed by treatment with LPS (1 μg/ml) for 6 h. COX-2 gene expression was determined using reverse transcription-PCR as described in “MATERIALS AND METHODS.” Densitometric data are normalized by β-actin and presented as the relative ratio of COX-2 levels in only LPS-treated cells. Values are expressed as the mean ± SEM of three independent experiments each performed in triplicate. *p < 0.05. c Immunocytochemistry analysis of COX-2 expression was performed as described in “MATERIALS AND METHODS” (magnification, ×400). Control: DMSO (0.1%), LPS: LPS only (1 μg/ml), LPS + EPE: EPE (50 μg/ml) and LPS treatment.
EPE Suppresses Phosphorylation of MAPK Molecules in LPS-Induced Raw264.7 Cells
To examine the specific cell signaling pathway involved in EPE-mediated COX-2 suppression, we measured the phosphorylation level of MAPK in EPE-treated Raw264.7 cells via Western blotting using anti-phospho-MAPK and anti-MAPK antibodies. As shown as Fig. 3, LPS induced phosphorylation of ERK, p38, and JNK, which was reduced in a dose-dependent manner upon pretreatment with EPE. These results imply that EPE inhibits LPS-induced COX-2 expression by suppressing the MAPK signaling pathway.
Differential effects of EPE on phosphorylation of ERK, p38, and JNK in LPS-stimulated Raw264.7 cells. Cells were preincubated with EPE for 1 h, followed by stimulation with LPS for 15 min. Total cell lysates were prepared using lysis buffer (Sigma, St Louis, MO). Protein concentrations were measured using the Bradford assay kit (Bio-Rad, Hercules, CA). Similar amounts of protein were separated by 10% SDS-PAGE, and transferred to PVDF membranes. Membranes were probed with antibodies against ERK, JNK, p38, and β-actin overnight at 4°C, and exposed to HRP-conjugated secondary antibodies for 1 h. Antibody-specific proteins were visualized using an enhanced chemiluminescence detection system. One of similar results is represented and relative ratio is also indicated, normalizing to total ERK, p38 or JNK signal. Values are expressed as the mean ± SEM of three independent experiments each performed in triplicate. $ P < 0.05, significant difference from unstimulated cells; # P < 0.05 and + P < 0.005, significant difference from LPS-treated cells.
EPE Blocks the Degradation of IκB-α and NF-κB Activation in LPS-Induced Raw264.7 Cells
To determine the effects of EPE on activation and translocation of the p65 subunit of NF-κB, we examined IκB-α and NF-κB activation using immunoblot analysis. PARP or β-actin was used as an internal control and for confirmation of no contamination during extraction of nuclear or cytosolic fraction. After LPS stimulation, we observed p65 accumulation in the nucleus. However, the p65 level in the nuclear fraction was significantly reduced by pretreatment with EPE, compared with that in the presence of LPS only. Moreover, phosphorylation and degradation of IκB-α were dose-dependently reduced by EPE (Fig. 4a).
Differential effects of EPE on activation of IκB-α and translocation of p65 in LPS-stimulated Raw264.7 cells. a Cells were treated with EPE for 1 h, followed by stimulation with LPS for 10 min. Equal amounts of protein were analyzed using specific antibodies for IκB-α and p65. Values are expressed as the mean ± SEM of three independent experiments each performed in triplicate. $ P < 0.05 significant difference from unstimulated cells; # P < 0.05 and *P < 0.005, significant difference from LPS-treated cells. b Raw264.7 cells were pretreated with different concentrations of EPE for 1 h and stimulated with LPS (1 μg/mL) for another 1 h. Cells were fixed, permeabilized, and incubated with a specific antibody for NF-κB (p65), followed by Texas Red-conjugated anti-rabbit Ig (red). Nuclei of the corresponding cells were visualized using DAPI staining (magnification, ×400). Control: DMSO (0.1%), LPS: LPS only (1 μg/ml), LPS + EPE: EPE (50 μg/ml) and LPS treatment.
To establish the effect of EPE on p65 translocation to the nucleus, we performed further immunocytochemical analysis. As shown in Fig. 4b, p65 was mainly localized to the cytosol in control cells. However, after LPS treatment, the majority of intracellular p65 translocated from the cytoplasm to the nucleus, as evident from strong NF-κB p65 nuclear staining. Pretreatment with EPE resulted in weaker intensity of p65 staining in the nucleus. Based on these results, we suggest that EPE exerts inhibitory action on LPS-induced translocation of p65 via suppressing phosphorylation of IκB-α.
EPE Inhibits Proinflammatory Cytokine Production in LPS-Induced Raw264.7 Cells
To determine the effects of EPE on release of cytokines, we investigated the TNF-α and IL-1β levels using a specific ELISA kit. As shown in Fig. 5, incubation of Raw264.7 cells with LPS for 24 h induced an increase in the TNF-α (419.84 ± 1.70 pg/ml) and IL-1β (68.83 ± 6.40 pg/ml) levels. Pretreatment with EPE (50 μg/ml) resulted in significant inhibition of TNF-α (by 59.9 ± 6.4%) and IL-1β (by 51.7 ± 4.7%) production.
Differential effects of EPE on TNF-α and IL-1β production in LPS-stimulated Raw264.7 cells. Cells were pretreated with EPE for 1 h and stimulated with LPS (1 μg/ml) for another 24 h. Cytokine levels in the supernatant were measured with the ELISA. Data are presented as means ± SEM from three independent experiments. $ P < 0.005, significant difference from unstimulated cells; # P < 0.05 and *P < 0.005, significant difference from LPS-treated cells.
EPE Inhibits IL-4 and IL-13 Cytokine Production in ConA-Induced Splenocytes
To examine the effects of EPE on production of cytokines (IL-4 and IL-13), the cytokine levels in splenocytes were investigated using an ELISA kit. As shown as Fig. 6, ConA treatment markedly enhanced the production of IL-4 (446.56 ± 13.99 pg/ml) and IL-13 (345.00 ± 2.83 pg/ml) in splenocytes. The IL-4 and IL-13 levels in Raw264.7 cells pretreated with 50 μg/ml EPE were markedly suppressed by 96.77 ± 0.28% and 85.47 ± 11.85%, respectively.
Differential effects of EPE on IL-4 and IL-13 production in ConA-stimulated splenocytes. Splenocytes were plated onto 96-well plates and treated with different concentrations of EPE for 1 h. After the addition of 1 μg/ml of concanavalin A for a further 3 days, concentrations of IL-4 and IL-13 from the supernatant fractions were measured using ELISA kits (R&D systems). Data are presented as mean values of three experiments ± SEM. $ P < 0.005, significant difference from untreated cells; # P < 0.05 and *P < 0.005, significant difference from ConA-treated cells.
DISCUSSION
In the present study, we demonstrate that EPE suppresses PGE2 production in LPS-stimulated Raw 264.7 cells in a dose-dependent manner but has no effect on cell viability. Macrophages play an important role in different immunopathological phenomena during inflammation, fever, and septic shock. Primary macrophages (Raw264.7 cells) and cancerous macrophage-like (J774) cells induced by LPS are regarded as a useful in vitro model for evaluating the potency of anti-inflammatory drugs and exploring their mechanisms of action [15]. Inflammation is related to the overproduction of inflammatory mediators (PGE2 and NO) and proinflammatory cytokines (TNF-α and IL-1β) and is caused to the unbalance of Th1 type cytokines (IL-1 and IL-6) and Th2 type cytokines (IL-4 and IL-13). Th1 type cytokines was detected in LPS-treated macrophages, and Th2 type cytokines was released in ConA-treated splenocytes. PGE2 is generated by activated inducible cyclooxygenase (COX)-2 [16–18].
The inhibitory effects of EPE against COX-2 expression (Fig. 2) and PGE2 production (Fig. 1a) suggest that anti-inflammatory activity is exerted via reduction of cytokines (Figs. 5 and 6), based on the knowledge that COX-2 expression coincides with PGE2 secretion in the pathogenesis of various inflammatory diseases. Several groups have recently demonstrated that the effects of plant extracts on the expression of inflammation-related genes [19–21] are strongly related to inhibitory effects on COX-2 protein expression in LPS-stimulated macrophages.
COX-2 expression is regulated at both the transcriptional and post-transcriptional levels [22, 23], and the specific signaling pathways involved are dependent on the stimulus type [22]. Induction of COX-2 has been shown to require activation of the ERK signaling pathway [24], while other researchers have demonstrated that constitutively active MEKK1 induces COX-2 expression by activating the SEK1/MKK4-p38 kinase pathway [25]. The c-Jun N-terminal kinases (JNKs), known as stress-activated protein kinases (SAPKs), are also associated with induction of COX-2 [19]. Here, we have shown that EPE inhibits LPS-induced COX-2 expression via suppressing ERK, p38, and JNK phosphorylation (Fig. 3).
NF-κB, a known pleiotropic regulator of several genes involved in immune and inflammatory responses, is activated in macrophages by various stimuli, including LPS and TNF- α [26]. Our data showed that EPE is involved in downregulation of the NF-κB signaling pathway in LPS-stimulated Raw264.7 cells, in support of our hypothesis. Various stimuli trigger signaling pathways that induce phosphorylation, ubiquitination, and subsequent degradation of IκB proteins, resulting in translocation of NF-κB from the cytoplasm to nucleus and binding to its motif [12, 26, 27]. However, in the cytoplasm of unstimulated cells, the IκB family of proteins prevents translocation of NF-κB to the nucleus by masking its nuclear localization sequence. Here, we found that EPE inhibits the translocation of NF-κB via dephosphorylation of IκB-α (Fig. 4).
LPS-stimulated NF-κB activation is a cellular event mainly managed by surface receptors, such as Toll-like receptor (TLR), and several cytosolic adapters, such as MyD88 [28–30]. TLR-MyD88 modulates NF-κB activation via several signal transducers associated with the function of the IKK complex and MEKK [31, 32]. The possible involvement of TLR-mediated signaling, including IKK complex and MEKKs, or other proteins requiring for LPS-TLR binding, such as MD-2, CD14, or LBP, in EPE-mediated inhibition of NF-κB activation should be further investigated.
In summary, we demonstrate that EPE inhibits the PGE2 production in LPS-stimulated Raw264.7 cells by blocking the phosphorylation of ERK, JNK, p38 kinase, and IκB-α and translocation of NF-κB which positively regulates transcription of TNF, IL-1β, and COX-2. In view of these findings, we propose that EPE is a useful potential anti-inflammatory agent. Further studies are required to identify the active compounds within the extract.
REFERENCES
Wu, Z.Y., P.H. Raven, and D.Y. Hong. 2007. Flora of China. Beijing/St. Louis: Science Press/Missouri Botanical Garden Press.
Coode, M.J.E. 2001. Elaeocarpus in New Guinea—new taxa in the Debruynii subgroup of the Monocera group. Contributions to the Flora of Mt Jaya, V. Kew Bulletin, United Kingdom.
Guha, M., and N. Mackman. 2001. LPS induction of gene expression in human monocytes. Cellular Signalling 13: 85–94.
Turini, M.E., and R.N. DuBois. 2002. Cyclooxygenase-2: a therapeutic target. Annual Reviews Medicine 53: 35–57.
Rocca, B., and G.A. FitzGerald. 2002. Cyclooxygenases and prostaglandins: shaping up the immune response. International Immunopharmacology 2: 603–630.
Williams, J.A., and E. Shacter. 1997. Regulation of macrophage cytokine production by prostaglandin E2. Distinct roles of cyclooxygenase-1 and -2. The Journal of Biological Chemistry 272: 25693–25699.
Vane, J.R. 1976. Prostaglandins as mediators of inflammation. Advances in Prostaglandin and Thromboxane Research 2: 791–801.
Vane, J.R., J.A. Mitchell, I. Appleton, A. Tomlinson, D. Bishop-Bailey, J. Croxtall, and D.A. Willoughby. 1994. Inducible isoforms of cyclooxygenase and nitric-oxide synthase in inflammation. Proceedings of the National Academy of Sciences of the United States of America 91: 2046–2050.
Johnson, G.L., and R. Lapadat. 2002. Mitogen-activated protein kinase pathways mediated by ERK, JNK, and p38 protein kinases. Science 298: 1911–1912.
Kim, Y.H., S.H. Lee, J.Y. Lee, S.W. Choi, J.W. Park, and T.K. Kwon. 2004. Triptolide inhibits murine-inducible nitric oxide synthase expression by down-regulating lipopolysaccharide-induced activity of nuclear factor-kappa B and c-Jun NH2-terminal kinase. European Journal of Pharmacology 494: 1–9.
Olsson, S., and R. Sundler. 2006. The role of lipid rafts in LPS-induced signaling in a macrophage cell line. Molecular Immunology 43: 607–612.
Baeuerle, P.A., and D. Baltimore. 1996. NF-kappa B: ten years after. Cell 87: 13–20.
Vanden Berghe, W., S. Plaisance, E. Boone, K. De Bosscher, M.L. Schmitz, W. Fiers, and G. Haegeman. 1998. p38 and extracellular signal-regulated kinase mitogen-activated protein kinase pathways are required for nuclear factor-kappaB p65 transactivation mediated by tumor necrosis factor. The Journal of Biological Chemistry 273: 3285–3290.
Genovese, M.C. 2005. Biologic therapies in clinical development for the treatment of rheumatoid arthritis. Journal of Clinical Rheumatology 11: S45–S54.
Kobori, M., M. Yoshida, M. Ohnishi-Kameyama, and H. Shinmoto. 2007. Ergosterol peroxide from an edible mushroom suppresses inflammatory responses in RAW264.7 macrophages and growth of HT29 colon adenocarcinoma cells. British Journal of Pharmacology 150: 209–219.
Qureshi, N., S.N. Vogel, C. Van Way 3rd, C.J. Papasian, A.A. Qureshi, and D.C. Morrison. 2005. The proteasome: a central regulator of inflammation and macrophage function. Immunologic Research 31: 243–260.
Malyshev, I.Y., and A. Shnyra. 2003. Controlled modulation of inflammatory, stress and apoptotic responses in macrophages. Current Drug Targets. Immune, Endocrine and Metabolic Disorders 3: 1–22.
Jiang, Q., I. Elson-Schwab, C. Courtemanche, and B.N. Ames. 2000. gamma-tocopherol and its major metabolite, in contrast to alpha-tocopherol, inhibit cyclooxygenase activity in macrophages and epithelial cells. Proceedings of the National Academy of Sciences of the United States of America 97: 11494–11499.
Kwon, O.K., M.Y. Lee, J.E. Yuk, S.R. Oh, Y.W. Chin, H.K. Lee, and K.S. Ahn. Anti-inflammatory effects of methanol extracts of the root of Lilium lancifolium on LPS-stimulated Raw264.7 cells. Journal of Ethnopharmacology 130:28–34.
Lii, C.K., H.W. Chen, W.T. Yun, and K.L. Liu. 2009. Suppressive effects of wild bitter gourd (Momordica charantia Linn. var. abbreviata ser.) fruit extracts on inflammatory responses in RAW264.7 macrophages. Journal of Ethnopharmacology 122: 227–233.
Sheeba, M.S., and V.V. Asha. 2009. Cardiospermum halicacabum ethanol extract inhibits LPS induced COX-2, TNF-alpha and iNOS expression, which is mediated by NF-kappaB regulation, in RAW264.7 cells. Journal of Ethnopharmacology 124: 39–44.
Mestre, J.R., K. Subbaramaiah, P.G. Sacks, S.P. Schantz, T. Tanabe, H. Inoue, and A.J. Dannenberg. 1997. Retinoids suppress phorbol ester-mediated induction of cyclooxygenase-2. Cancer Research 57: 1081–1085.
Dean, J.L., M. Brook, A.R. Clark, and J. Saklatvala. 1999. p38 mitogen-activated protein kinase regulates cyclooxygenase-2 mRNA stability and transcription in lipopolysaccharide-treated human monocytes. The Journal of Biological Chemistry 274: 264–269.
Xie, W., and H.R. Herschman. 1996. Transcriptional regulation of prostaglandin synthase 2 gene expression by platelet-derived growth factor and serum. The Journal of Biological Chemistry 271: 31742–31748.
Guan, Z., S.Y. Buckman, A.P. Pentland, D.J. Templeton, and A.R. Morrison. 1998. Induction of cyclooxygenase-2 by the activated MEKK1 --> SEK1/MKK4 --> p38 mitogen-activated protein kinase pathway. The Journal of Biological Chemistry 273: 12901–12908.
Rajapakse, N., M.M. Kim, E. Mendis, and S.K. Kim. 2008. Inhibition of inducible nitric oxide synthase and cyclooxygenase-2 in lipopolysaccharide-stimulated RAW264.7 cells by carboxybutyrylated glucosamine takes place via down-regulation of mitogen-activated protein kinase-mediated nuclear factor-kappaB signaling. Immunology 123: 348–357.
Kretz-Remy, C., P. Mehlen, M.E. Mirault, and A.P. Arrigo. 1996. Inhibition of I kappa B-alpha phosphorylation and degradation and subsequent NF-kappa B activation by glutathione peroxidase overexpression. The Journal of Cell Biology 133: 1083–1093.
Palaniyar, N., J. Nadesalingam, and K.B. Reid. 2002. Pulmonary innate immune proteins and receptors that interact with gram-positive bacterial ligands. Immunobiology 205: 575–594.
Kawai, T., O. Adachi, T. Ogawa, K. Takeda, and S. Akira. 1999. Unresponsiveness of MyD88-deficient mice to endotoxin. Immunity 11: 115–122.
Takeda, K., T. Kaisho, and S. Akira. 2003. Toll-like receptors. Annual Review of Immunology 21: 335–376.
Hayden, M.S., and S. Ghosh. 2004. Signaling to NF-kappa B. Genes & Development 18: 2195–2224.
Huang, Q., J. Yang, Y. Lin, C. Walker, J. Cheng, Z.G. Liu, and B. Su. 2004. Differential regulation of interleukin 1 receptor and Toll-like receptor signaling by MEKK3. Nature Immunology 5: 98–103.
ACKNOWLEDGMENTS
This work was supported by grants from the Construction of Foreign Plant Extract Library funded by the Ministry of Science and Technology (FGS1010924) and KRIBB Research Initiative Program (KGS2241012) of the Republic of Korea.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kwon, OK., Ahn, KS., Park, JW. et al. Ethanol Extract of Elaeocarpus petiolatus Inhibits Lipopolysaccharide-Induced Inflammation in Macrophage Cells. Inflammation 35, 535–544 (2012). https://doi.org/10.1007/s10753-011-9343-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-011-9343-3